Abstract
Ewing sarcoma is a lesion of bone, described in small round cell neoplasm. This tumour resembles primitive neuroectodermal tumour both clinically and histologically. Major difference between these two is that the former arises in the bone and the later in soft tissue. It appears most frequently in males at the age range of of 5–25 years, 80% of which occurs within first two decades of life. Males are more commonly affected than females. Present paper reported with a case report of male patient with 24-year-old showing Ewing’s sarcoma of right maxilla.
Keywords: dentistry and oral medicine, medical education, pathology
Background
James Ewing in 1921 was the first to describe a tumour of undifferentiated cells of long bones, which was radiosensitive.1 Prior to that Arthur Purdy Stout (1918), described a tumour which contain large amount of small round cells in the ulnar nerve, which was known as primitive neuroectodermal tumour (PNET). Numerous investigators believed that both these tumours are having unlike morphological expressions of a single tumour.2 The Ewing’s Sarcoma (EWS) gene shows translocations on an E26 transformation-specific or E-twenty-six (ETS)-type gene, mainly the fli1 gene on chromosome 11 and chromosome 22 are implicated in the vast preponderance of cases.3 Clinical features include localised bone tenderness and a swelling. This disease occurs predominantly in children and young adult aged mostly between 5 and 25 years, however the median age is 13 years. Bones commonly affected are long bones of extremities although skull, pelvic girdle, maxilla and mandible can also be involved. In cases of jaw involvement facial neuralgia and lip paraesthesia has been reported.2 They represent a few of the mainly destructive cancers in that they have a high metastatic budding and are refractory towards conventional radiation and chemotherapy.4 This case report describes a case of Ewing sarcoma which occurs in a 24-year-old male patient who had come with a swelling since 4 years.
Case presentation
A 24-year-old male patient visited the out-patient department with a swelling on the right part of face since 4 years. As stated by the patient he was alright 4 years back when he developed a swelling over the right part of face, which was small in size but enlarged slowly to attain the present dimension. He moreover gave the history of epiphora and epistaxis from the past 1 year. There was no narration of pain in the past. Patient medical and dental history was not contributory. General examination revealed, patient was moderately built, non-anaemic, non-cyanosed and no organomegaly was detected. All the vitals were under normal ranges. Extraoral inspection revealed a solitary pear shaped swelling measuring 7×7 cm on right part of face extending mesiodistally from the nasal bridge to 1–1.5 cm anterior to the tragus (figure 1) and superior-inferiorly from infraorbital margin to 1 cm behind the commissure of mouth (figure 1 (figure 2). The swelling was also present intraorally with respect to 13 and 15 measuring approximately 2×1.5 cm in its greatest dimension, extending from distal surface of 13 to distal aspect of 14. Overlying mucosa was of normal colour. On palpation swelling was hard, with normal temperature, non-fluctuant, non-mobile, non-compressible, absence of translucency and no palpable pulsation was noted. According to the data collected from history and clinical examination, a working diagnosis of cemento-ossifying fibroma was given.
Figure 1.

The extraoral clinical photograph showing an enormous swelling on the right side of the face.
Investigations
On haematological investigation the findings of serum urea, serum creatinine level were 33 and 93 mg/dL, respectively, and haemoglobin level was 13.5 g/dL along with random blood glucose level of 122 mg/dL. The CT scan showed perforation of maxillary and nasal bones (figure 2(figure 3). MRI revealed the extent of tumour into the maxillary sinus (figure 3 (figure 4). The lesion was surgically excised and processed for histopathological evaluation (figure 4Macroscopic evaluation revealed numerous bits of soft and hard tissue which were decalcified and processed. Under scanner view, multiple pieces of tissue with small to large sheets and lobules of compactly packed hyperchromatic tumour cells were evident. Numerous small to large vascular channels were traversing through the sheets (figure 5). The remaining tissue sections show predominantly hypocellular myxoid stroma. The decalcified section showed normal appearing mature trabecular bone. The tumour component consisted of small round cells depicting nuclear hyperchromatism, pleomorphism, nuclear vesiculation, increased nuclear-cytoplasmic ratio and mitotic figures (figure 6). On immunohistochemical analysis with a panel of antibodies, the tumour cells shows strong immune positivity for CD-99 (figure 7) and vimentin; whereas negative for pancytokeratin, epithelial membrane antigen (EMA), cluster of differentiation (CD-31), cluster of designation (CD-34), D2-40, transducin-like enhancer of split-1 (TLE1), myogenin, desmin, synaptophysin, smooth muscle actin and S-100 protein. The overall histopathological features were suggestive of Ewing’s sarcoma after a clinic-pathological correlation.
Figure 2.

The extraoral superio-inferior viwe of the lesion.
Figure 3.
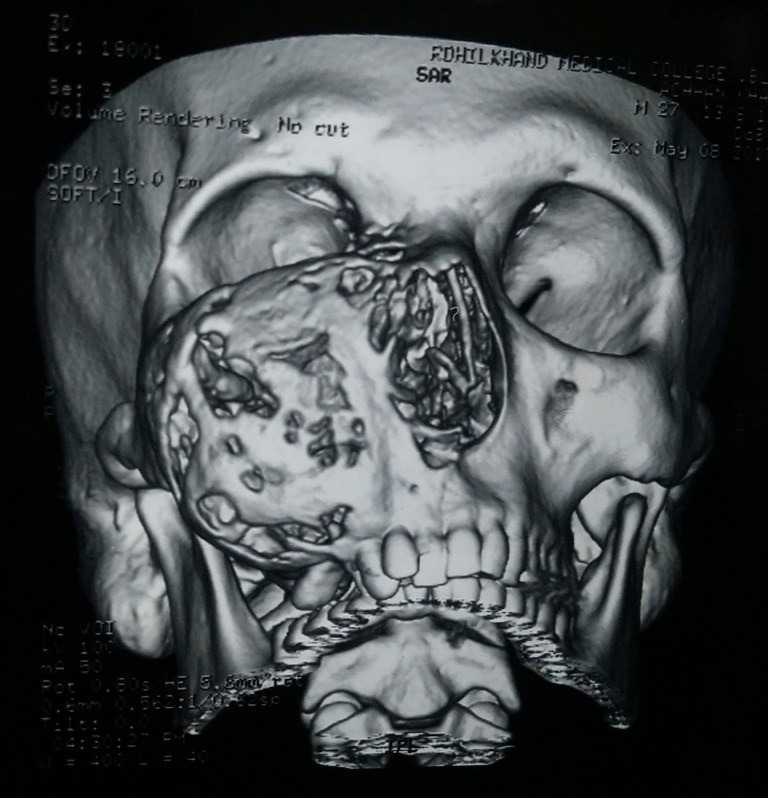
The CT scan showing perforation of maxillary and nasal bones.
Figure 4.
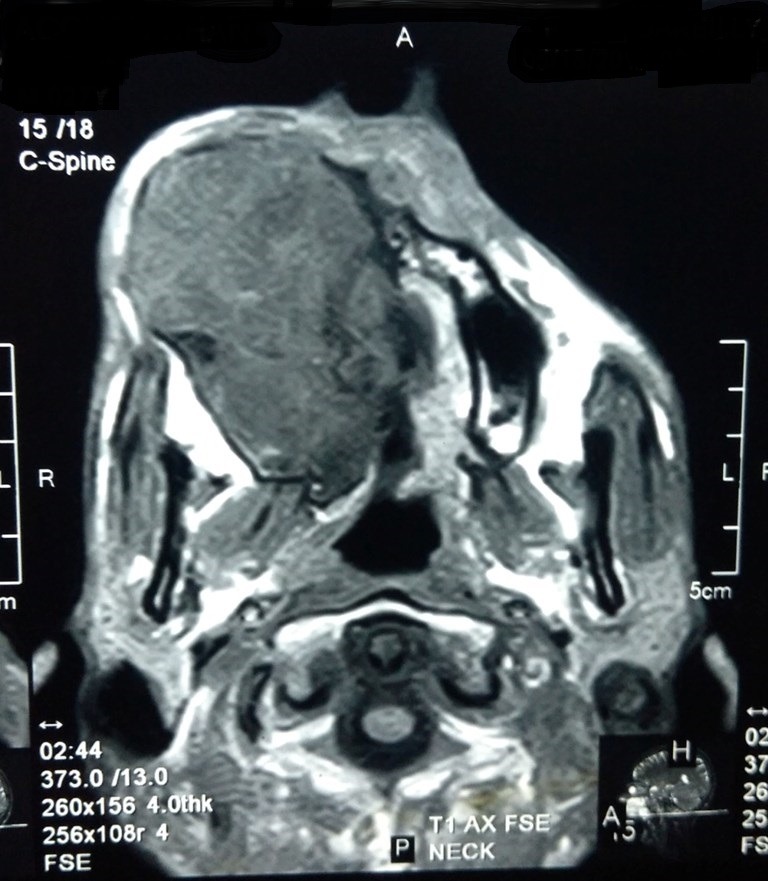
The MRI showed the extension of tumor involving sinus region.
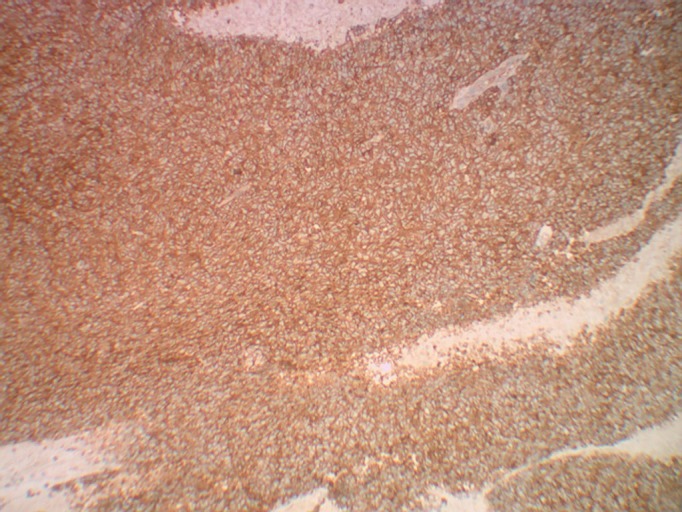
Figure 5.
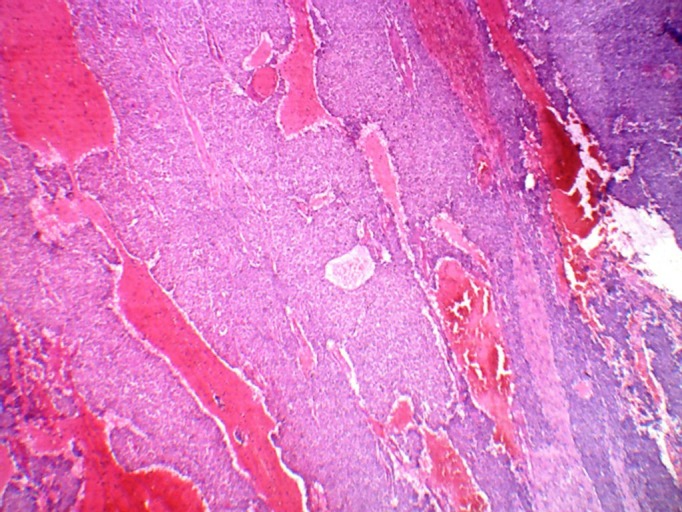
Photomicrograph under low power view showing malignant round cell in scanner. (H&E ×100).
Figure 6.
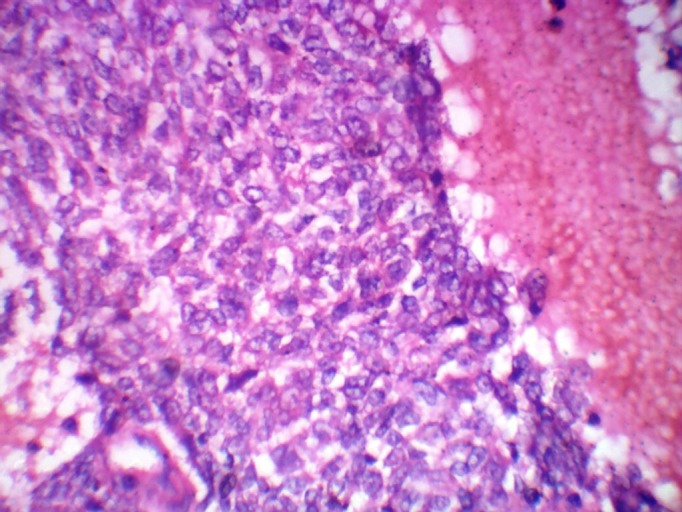
Photomicrograph under higher power view showing nuclear hyperchromatism, pleomorphism, nuclear vesiculation, increased nuclear-cytoplasmic ratio and mitotic figures. (H&E ×400).
Figure 7.
Photomicrograph of immunohistochemical staining with CD99 showing strong positivity.
Differential diagnosis
Differential diagnosis was made as osteoma and fibrous dysplasia. Ewing’s sarcoma manifest between 5 and 25 years of age, having median age of occurrence 13 years with a male predilection. Pain and swelling can be earliest clinical signs. Osteoma on the other hand can arise at any age but the mean age of occurrence is between 29.4 and 40.5 years, however it is somewhat more common in young adult and manifests itself as a circumscribed swelling on the jaw producing asymmetry. Moreover, it is a slow growing tumour and seldom patient present with pain. Osteoma of the maxillofacial region shows a predilection for the mandible, especially the ramus and the inferior border below the molars.
With respect to fibrous dysplasia, it clinically manifest in person aged between 3 and 15 years and most cases of it are asymptomatic having equal sex predilection. Various patterns have been recognised including monostotic (70%–80%), polyostotic, craniofacial (10%–25%) and cherubism.
Treatment
Treatment of choice as surgical excision.
Outcome and follow-up
No history of recurrence during 3-month follow-up.
Discussion
Ewing’s sarcoma is a lesion of bony, described underneath the section of small round cell tumours. There is significant clinical and histological similarity of this tumour with that of primitive neuroectodermal tumour (PNET).5 These are regarded as having small, round and quite undifferentiated cells. Because of their undifferentiated or else primal character, its diagnosis becomes difficult. Numerous names including ‘peripheral neuroepithelioma’, ‘Askin tumour’ and PNET are used, often interchangeably.6 The translocation t(11;22)(q24;q12) results in the production of a chimeric gene between EWS and Friend leukemia integration (FLI) member of the ETS family of transcription factors located at 1lq24. The resulting fusion transcript has transforming action which plays a important job in pathogenesis.6
This tumour is most frequently observed in young individuals aged between 4 and 25 years having male predilection.2 The identification of Ewing’s sarcoma is difficult as it requires clinical, radiological and histopathological correlation.7 The study done by Ambros et al, reported that a pseudoautosomal gene was found on the small arms of the Y and X chromosomes, which showed the exact expression of the MIC2 gene, on Ewing’s sarcoma (ES) and peripheral primitive neuroectodermal tumour (pPNET) cells.8 Shek reported a case of Ewing’s sarcoma occurring in small intestine in a 9-year-old patient with abdominal distention.9 Cheung et al, described a case affected with Ewing sarcoma of extraskeletal in origin on the left inguinal region in a 77-year-old woman. They distinguished the tumour from other round cell tumour by showing the lacking of immunoreactivity for epithelial, vascular, lymphoid, neural, neuroendocrine, histiocytic and muscle markers.10
Lam et al reported a case of Primary orbital Ewing’s sarcoma in a 2-year-old boy, who presented with mutual trouble-free proptosis.11 Rafailidis et al described a primary Ewing’s sarcoma of stomach in a 68-year-old man with t(11;22)(q24;q12) gene translocation,12 whereas the present case reported Ewing’s sarcoma in the right maxillary region in a 24-year-old male patient having history of epiphora and epistaxis from the past 1 year. Immunohistochemical analysis with a panel of antibodies, the tumour cells shows strong immune positivity for CD-99 and vimentin; whereas negative for pancytokeratin, EMA, CD-31, CD-34, D2-40, TLE1, myogenin, desmin, synaptophysin, smooth muscle actin and S-100 protein.
Considerable improvements have been prepared in the treatment and survival of children with small round cell tumour. Although diagnostic procedures such as electron microscopy and immunocytochemistry can help in diagnosis, the molecular genetics and cytogenetic abnormalities of the diverse small round cell neoplasm, most of time are detected by fluorescence in situ hybridisation and PCR.13
The present case describes a case of 24-year-old male patient presented with swelling on right side of face, epiphora and epistaxis. However, Mukherjee et al in 201214 described a case of Ewing’s Sarcoma of mandible in a 8-year-old girl who presented with a swelling in mandibular anterior region. Khaliq et al in 201215 reported a case of a 52-year-old healthy woman who presented with a 2-week history of pain in her right posterior thigh that was not relieved by non-steroidal anti-inflammatory medicine and physical therapy. Alasmari et al 16 describes primary Ewing’s sarcoma of kidney in a 15-year-old female patient and Adisesh et al 17 describes a case of 19-year-old young man reported with pain and mild swelling of the upper end of right tibia.
Learning points.
Ewing’s sarcoma is a sarcoma of bone described under round cell tumour.
It arises within bone and often resemble primitive neuroectodermal tumour which is extraosseous.
Oral manifestation includes swelling and ulceration along with generalised symptom like fever and elevated white blood cell.
Footnotes
Patient consent for publication: Obtained.
Contributors: Concepts and design: MA and SS. Intellectual content: SS. Literature search: MA, AM and BSM. Data acquisition and analysis: SS, AM and MA. Manuscript preparation: MA, SS and AM. Manuscript editing and review: AM and BSM.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Desai SS, Jambhekar NA. Pathology of Ewing’s sarcoma/PNET: Current opinion and emerging concepts. Indian J Orthop 2010;44:363–8. 10.4103/0019-5413.69304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rajendran R. Shafer’s textbook of oral pathology. Noida: Elsevier India, 2009. [Google Scholar]
- 3. Bernstein M, Kovar H, Paulussen M, et al. Ewing’s sarcoma family of tumors: current management. Oncologist 2006;11:503–19. 10.1634/theoncologist.11-5-503 [DOI] [PubMed] [Google Scholar]
- 4. Riggi N, Stamenkovic I. The Biology of Ewing sarcoma. Cancer Lett 2007;254:1–10. 10.1016/j.canlet.2006.12.009 [DOI] [PubMed] [Google Scholar]
- 5. Sharma S, Kamala R, Nair D, et al. Round cell tumors: classification and immunohistochemistry. Indian J Med Paediatr Oncol 2017;38:349–53. 10.4103/ijmpo.ijmpo_84_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McManus AP, Gusterson BA, Pinkerton CR, et al. The molecular pathology of small round-cell tumours–relevance to diagnosis, prognosis, and classification. J Pathol 1996;178:116–21. [DOI] [PubMed] [Google Scholar]
- 7. Delattre O, Zucman J, Melot T, et al. The Ewing family of tumors–a subgroup of small-round-cell tumors defined by specific chimeric transcripts. N Engl J Med 1994;331:294–9. 10.1056/NEJM199408043310503 [DOI] [PubMed] [Google Scholar]
- 8. Ambros IM, Ambros PF, Strehl S, et al. MIC2 is a specific marker for Ewing’s sarcoma and peripheral primitive neuroectodermal tumors. Evidence for a common histogenesis of Ewing’s sarcoma and peripheral primitive neuroectodermal tumors from MIC2 expression and specific chromosome aberration. Cancer 1991;67:1886–93. [DOI] [PubMed] [Google Scholar]
- 9. Shek TW, Chan GC, Khong PL, et al. Ewing sarcoma of the small intestine. J Pediatr Hematol Oncol 2001;23:530–2. 10.1097/00043426-200111000-00013 [DOI] [PubMed] [Google Scholar]
- 10. Cheung CC, Kandel RA, Bell RS, et al. Extraskeletal Ewing sarcoma in a 77-year-old woman. Arch Pathol Lab Med 2001;125:1358–60. [DOI] [PubMed] [Google Scholar]
- 11. Lam DS, Li CK, Cheng LL, et al. Primary orbital Ewing’s sarcoma: report of a case and review of the literature. Eye 1999;13:38–42. 10.1038/eye.1999.8 [DOI] [PubMed] [Google Scholar]
- 12. Rafailidis S, Ballas K, Psarras K, et al. Primary Ewing sarcoma of the stomach–a newly described entity. Eur Surg Res 2009;42:17–20. 10.1159/000166166 [DOI] [PubMed] [Google Scholar]
- 13. Khoury JD. Ewing’s sarcoma family of tumors. Expert Review Of Molecular Diagnostics 2010;8:235–42. [DOI] [PubMed] [Google Scholar]
- 14. Mukherjee A, Ray JG, Bhattacharya S, et al. Ewing’s sarcoma of mandible: a case report and review of Indian literature. Contemp Clin Dent 2012;3:494–8. 10.4103/0976-237X.107454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Khaliq W, Bahador MF, Laurence TN, et al. Ewing’s sarcoma: a case report of a 52-year-old woman with recurrent tumor and literature review. Oncol Lett 2012;3:155–8. 10.3892/ol.2011.440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Alasmari F, Albadawe H, Alkhateeb S, et al. Primary Ewing’s sarcoma of the kidney: a case report. Int J Surg Case Rep 2017;41:65–7. 10.1016/j.ijscr.2017.07.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Adisesh A, Neeraja M, Prasad T. Metastatic Ewing sarcoma - a case report . Indian J Orthop 2005;39:127–9. 10.4103/0019-5413.36793 [DOI] [Google Scholar]


