Abstract
A 73-year-old man underwent bilateral spinal decompression of L4/5 for severe spinal canal stenosis, requiring minimal analgesia and providing immediate relief. Two days post-operatively, he presented with new onset bilateral leg pain and difficulty mobilising. MRI demonstrated spinal epidural lipomatosis (SEL), which was not present pre-operatively, at L5/S1. Further surgery was performed with decompression of L5/S1 through removal of epidural fat. At both 3 weeks and 5 months follow-up clinics, the patient was asymptomatic. To our knowledge, this is the first case of acute spinal epidural lipomatosis directly following spinal surgery. It is important to recognise SEL as a complication following spinal surgical intervention, due to the potential development of significant neurological consequences.
Keywords: radiology, orthopaedic and trauma surgery
Background
Spinal epidural lipomatosis (SEL) refers to an excessive accumulation of fat within the epidural space. It is a well-recognised but rare disease, with an incidence of 0.6% in patients undergoing dedicated spinal MRI for any indication.1 Excessive systemic exogenous steroid use accounts for 55% of cases.2 Other causes include obesity and Cushing’s syndrome, due to excessive endogenous steroid production.2 3 Epidural steroid injection causing SEL has also been reported.3 4 Typically, SEL occurs in the lumbar region and results in thecal sac compression. Although usually asymptomatic, SEL can cause spinal nerve compression symptoms such as incontinence, leg pain, weakness and numbness.2 Our case describes SEL 3 days following spinal decompression surgery. We have found no previously reported cases of acute adjacent SEL following lumbar spine surgery in the literature to date.
Case presentation
A 73-year-old man presented with spinal claudication and bilateral leg pain. MRI of the lumbar spine demonstrated severe spinal canal stenosis at L4/5. His medical history included prostate cancer, which was treated in 2010 and was in remission at the time of surgery. He underwent bilateral spinal canal decompression. Initial recovery was excellent with relief of symptoms and early discharge. Two days post-operatively, he developed difficulty in mobilisation and bilateral leg pain. He was pain-free at rest but suffered significant bilateral leg discomfort on walking. On examination, he was walking with a crouch gait and there was bruising at the surgical site, but no obvious active bleeding. He had no neurological deficit, including no incontinence, saddle anaesthesia or leg weakness at rest. A clinical diagnosis of epidural haematoma was initially considered as it is a previously recognised cause of compressive spinal symptoms following spinal surgery.5 6 Subsequently, MRI demonstrated excess epidural fat in the spinal canal, causing tight spinal canal stenosis and compressing the cauda equina, at the L5/S1 level. A provisional diagnosis of SEL was made. The following day, repeat surgery to remove the swollen fat from the spinal canal was performed and the diagnosis of SEL was confirmed.
Investigations
At initial presentation, the pre-operative MRI spine demonstrated tight spinal canal stenosis at L4/5 (figure 1). There was no evidence of SEL on pre-operative MRI (figure 2) at L5/S1. Repeat MRI spine 3 days following initial decompression surgery showed prominent epidural fat, severely compressing the cauda equina at L5/S1 (figure 3). Typical MRI features of stage III spinal epidural lipomatosis were demonstrated, with thecal sac compression creating a ‘Y’ sign appearance on transverse images at the level of L5/S1.
Figure 1.
Axial T2-weighted MRI scan of the lumbar spine before nerve root decompression. Image demonstrates tight spinal canal stenosis at L4/5.
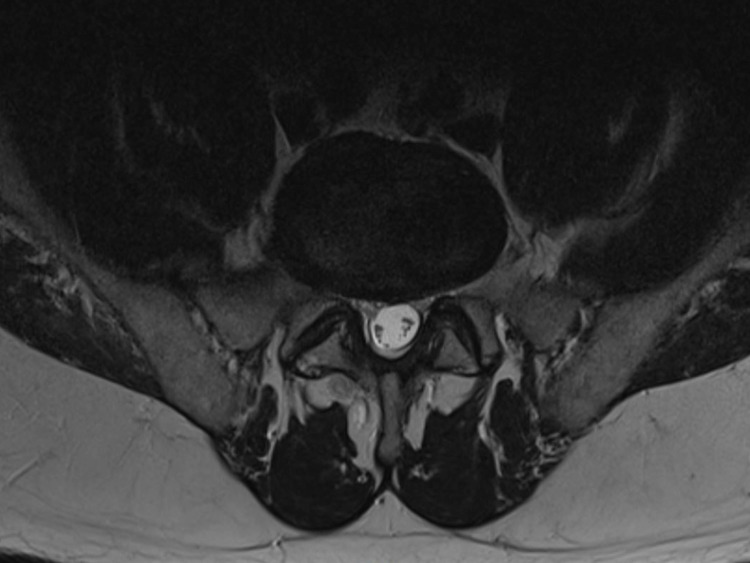
Figure 2.
Axial T2-weighted MRI scan of the lumbar spine before nerve root decompression at level L5/S1. Image demonstrates no evidence of spinal epidural lipomatosis.
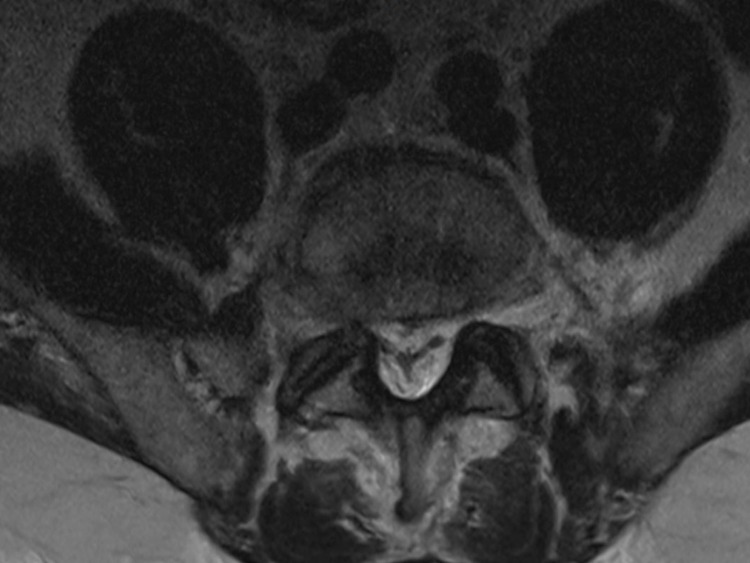
Figure 3.
Axial T2-weighted MRI scan of the lumbar spine post nerve root decompression at level L5/S1. Image demonstrates the characteristic ‘Y’ sign configuration of thecal sac compression due to compression by epidural fat, as first described by Kuhn et al, indicating stage three spinal epidural lipomatosis.10
Differential diagnosis
Epidural haematoma.
Cerebrospinal fluid leak.
Infection and epidural abscess.
Nerve trauma.
Treatment
The SEL was successfully treated with surgical removal of the inflamed, swollen epidural fat from the spinal canal.
Outcome and follow-up
The day following surgery to remove the SEL, the patient was mobilising and the wound was healing well. At 3 weeks and at 5 months follow-up, the patient was asymptomatic of any complications following either the decompression surgery or the surgical removal of excess epidural fat. The SEL was clinically resolved at the last point of contact. No follow-up imaging has therefore been deemed necessary.
Discussion
SEL is an important, but rare condition, which can lead to pain, weakness and in more serious cases, paralysis.2 It is most often diagnosed as an incidental finding on MRI spine.1 Of all patients presenting with spine related symptoms, 1.8% have incidental SEL, with symptoms having been attributed to other pathologies. Risk factors for SEL include excess exogenous or endogenous steroids,2 hypothyroidism and obesity.7 Endogenous steroids may be a result of conditions such as Cushing’s syndrome.2 The patient in this case had none of the known risk factors for SEL. Preoperative MRI spine demonstrated no evidence of SEL; however, it was identified on postoperative MRI spine. No intrathecal steroids were injected as part of the surgery. There were no other compressive causes identified at the L4/5 level on the post-operative imaging. We have not identified any other cases in the literature describing SEL occurring after spinal nerve root decompression.
Features of SEL on MRI spine include generalised excessive adipose tissue in the extradural space and thecal sac compression. This can cause cauda equina compression, if the SEL is below the conus medullaris, typically located at L1.8 Borré et al classified lumbosacral epidural lipomatosis from grade 0 to III based on 2258 lumbar MRIs. Grade 0 is normal, with ≤40% of the spinal canal width being covered by epidural fat. Grade I reflects 41%–50% coverage of the spinal canal, grade II 51%–74% and grade III ≥75%. All grade III cases were symptomatic from their SEL. The centripetal pressures on the thecal sac exerted by the epidural fat in grade III SEL can lead to a characteristic ‘Y’ sign of the spinal canal on transverse MRI spine.9 10 Spinal MRI of our patient demonstrated the ‘Y’ sign, thus defining his SEL as grade III.
The management of SEL depends on the underlying cause and severity of symptoms.2 A conservative approach may be taken to reduce the risk factors for SEL, for example weight loss interventions or steroid medication dose reduction. Surgery is reserved for cases where conservative management has failed or for more severe clinical symptoms and includes laminectomy or removal of epidural adipose tissue, as in this case.2 7
This case illustrates that high grade SEL should be recognised as a possible complication of spinal decompression surgery and therefore, considered as a differential diagnosis in those presenting post-operatively with lower limb pain and impaired mobility. It was important to make the correct diagnosis in this case as surgery was required. If SEL had been missed, the patient’s symptoms could have progressed and ultimately could have led to lower limb paralysis if the lipomatosis had not been removed.2
Learning points.
Spinal epidural lipomatosis (SEL) should be recognised as a potential rare complication of spinal decompression surgery.
Radiologists should be aware of the clinical and radiological features of SEL in order to recognise the condition following spinal surgery.
Treatment for SEL depends on its aetiology and the severity of symptoms. Surgeons and radiologists should liaise to determine an appropriate management plan depending on imaging and operative potential.
Footnotes
Patient consent for publication: Obtained.
Contributors: DG wrote the manuscript. KW proof-read and edited the manuscript. IH provided patient the information, proof-read and edited the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Theyskens NC, Paulino Pereira NR, Janssen SJ, et al. The prevalence of spinal epidural lipomatosis on magnetic resonance imaging. Spine J 2017;17:969–76. 10.1016/j.spinee.2017.02.010 [DOI] [PubMed] [Google Scholar]
- 2. Fogel GR, Cunningham PY, Esses SI. Spinal epidural lipomatosis: case reports, literature review and meta-analysis. Spine J 2005;5:202–11. 10.1016/j.spinee.2004.05.252 [DOI] [PubMed] [Google Scholar]
- 3. Jaimes R, Rocco AG. Multiple epidural steroid injections and body mass index linked with occurrence of epidural lipomatosis: a case series. BMC Anesthesiol 2014;14:70 10.1186/1471-2253-14-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Choi KC, Kang BU, Lee CD, et al. Rapid progression of spinal epidural lipomatosis. Eur Spine J 2012;21 Suppl 4:408–12. 10.1007/s00586-011-1855-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Uribe J, Moza K, Jimenez O, et al. Delayed postoperative spinal epidural hematomas. Spine J 2003;3:125–9. 10.1016/S1529-9430(02)00535-1 [DOI] [PubMed] [Google Scholar]
- 6. Yi S, Yoon DH, Kim KN, et al. Postoperative spinal epidural hematoma: risk factor and clinical outcome. Yonsei Med J 2006;47:326–32. 10.3349/ymj.2006.47.3.326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fassett DR, Schmidt MH. Spinal epidural lipomatosis: a review of its causes and recommendations for treatment. Neurosurg Focus 2004;16:1–3. 10.3171/foc.2004.16.4.12 [DOI] [PubMed] [Google Scholar]
- 8. Soleiman J, Demaerel P, Rocher S, et al. Magnetic resonance imaging study of the level of termination of the conus medullaris and the thecal sac: influence of age and gender. Spine 2005;30:1875–80. 10.1097/01.brs.0000174116.74775.2e [DOI] [PubMed] [Google Scholar]
- 9. Borré DG, Borré GE, Aude F, et al. Lumbosacral epidural lipomatosis: MRI grading. Eur Radiol 2003;13:1709–21. 10.1007/s00330-002-1716-4 [DOI] [PubMed] [Google Scholar]
- 10. Kuhn MJ, Youssef HT, Swan TL, et al. Lumbar epidural lipomatosis: the “Y” sign of thecal sac compression. Comput Med Imaging Graph 1994;18:367–72. 10.1016/0895-6111(94)90007-8 [DOI] [PubMed] [Google Scholar]