Abstract
The incidence of large cell neuroendocrine carcinoma (LCNEC) of the lung is rare, and the treatment methods and prognosis for such patients are still subjects of debate. We report a case of a 78-year-old male LCNEC patient for whom stereotactic body radiation therapy was performed. A four-dimensional computed tomography scan was used for simulation, and radiotherapy was planned using the volumetrically modulated arc technique. A total of 55 Gy was delivered in five daily fractions. The treatment was safely completed, and the patient did not report any discomfort. The only side-effect was an intermittent cough. Currently, the patient has received 18 months of outpatient follow-up care with no evidence of disease. In conclusion, stereotactic body radiation therapy can be a valuable treatment option for early stage LCNEC.
Keywords: lung, large cell, neuroendocrine carcinoma, stereotactic ablative radiotherapy, radiation therapy
Introduction
Large cell neuroendocrine carcinoma (LCNEC) of the lung is a very rare lung cancer, with a rate of ~1% of all lung cancer patients.1,2 Although the histological features of LCNEC are similar to those of small cell lung cancer (SCLC), the biological features of LCNEC are more similar to those of non-small-cell lung cancer (NSCLC).3 There are no established treatment guidelines for LCNEC.3 However, if possible, surgery for early stage LCNEC is recommended because it is not only possible to make a final diagnosis but it can also be an important basis for planning the patient’s treatment after surgery.4 If surgery cannot be performed, stereotactic body radiation therapy (SBRT) may serve as a useful alternative treatment for early stage NSCLC.5–7 However, SBRT is not yet established as an appropriate treatment for early stage SCLC.8 Here, we report the case of a patient with stage IA LCNEC for whom SBRT was performed after refusal of surgical resection. The patient is currently under outpatient follow-up care with no evidence of disease 18 months after SBRT completion.
Case report
The patient was a 78-year-old man with a smoking history of 50 pack-years. He had a 25-year history of type II diabetes mellitus and benign prostate hypertrophy, and there was a history of several hospitalizations due to hypoglycemic shock from unregulated type II diabetes mellitus and pneumonia. At the age of 12, he lost his right arm at the time of the Korean War. The patient gave written informed consent for publication of his case details and images. The study was approved by the Institutional Review Board of Soonchunhyang University Cheonan Hospital (approval no SCHCA 2018-05-052).
The patient underwent chest X-ray in March 2017 for a routine medical examination. A consolidative ground glass opacity was observed in the left upper lobe. Chest computed tomography (CT) with contrast enhancement revealed an ~2.6-cm-sized lung mass without any lymph node enlargement (Figure 1). Percutaneous needle biopsy confirmed that the mass was an LCNEC. Immunohistochemical analysis showed positivity for CK7 and CD56 and focal positivity for chromogranin A, TTF-1, and P63. Synaptophysin was weakly positive, and napsin-A, P40, and ALK were negative. EGFR mutation in exons 18, 19, 20, and 21 was not found, and ALK gene translocation was negative.
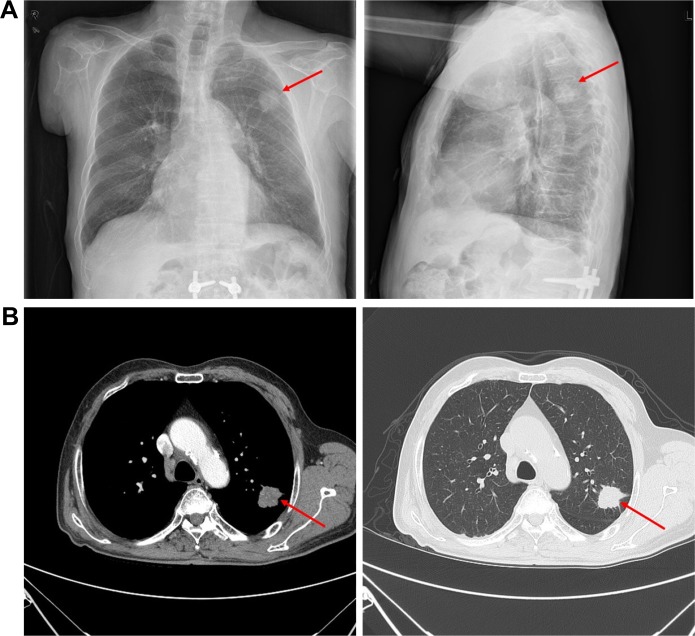
Figure 1.
Pretreatment chest images.
Note: A 2.6-cm-sized left upper lobe mass (red arrows) was observed in chest X-ray (A) and CT (B).
Abbreviation: CT, computed tomography.
Bronchoscopy with endobronchial ultrasound biopsy was performed to determine the mediastinal stage. The 4R and 7 station lymph nodes were negative. 18F-fluorodeoxyglucose positron emission tomography–CT showed no abnormal metabolic activity except for left upper lobe lung cancer (maximum standardized uptake value 12.1) and an incidental parotid Warthin tumor (Figure 2). Lung perfusion scan showed only a few multifocal perfusion defects due to underlying emphysema in both lung fields and no segmental perfusion defect. Finally, the patient was diagnosed with LCNEC T1cN0M0, stage IA, according to the criteria of the American Joint Committee on Cancer, eighth edition.
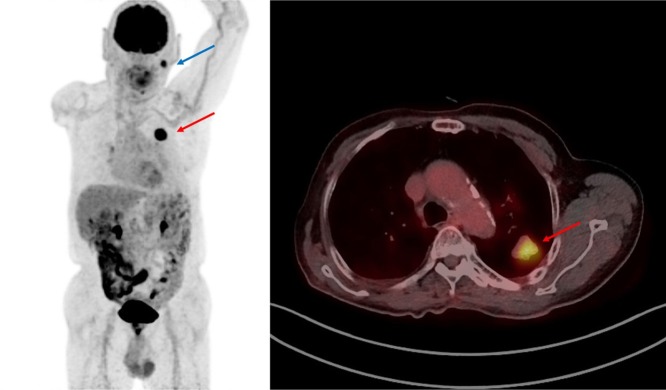
Figure 2.
Pretreatment 18F-fluorodeoxyglucose positron emission tomography/CT images.
Note: There was no lesion with abnormal metabolic activity except for LCNEC (red arrows) in the left upper lobe and a Warthin tumor in the left parotid gland (blue arrow).
Abbreviations: CT, computed tomography; LCNEC, large cell neuroendocrine carcinoma.
Surgery was recommended to the patient, but he was reluctant to undergo surgery. He was also consulted about radiation therapy (RT). SBRT was considered because the tumor was <5 cm in diameter, located peripherally in the lung, and the RT target did not include the regional lymph nodes. Finally, the patient decided to undergo SBRT.
The patient underwent respiration-correlated 4D-CT (Brilliance CT Big Bore; Philips Medical Systems, Cleveland, OH, USA) for simulation. The gross tumor volume was contoured in the mediastinal window setting, and the clinical target volume was expanded by 0.5 cm around the gross tumor volume. The internal target volume was the sum of the clinical target volumes of all ten respiratory phases. The planning target volume was created by adding 0.5-cm isotropic set-up margins all around the internal target volume. The planning target volume was 58.5 mL. The treatment plan was created using the volumetrically modulated arc technique using the Eclipse treatment planning system (Varian Medical Systems, Palo Alto, CA, USA) with 6 MV photons (Figure 3). SBRT employed a NovalisTx system (Varian Medical Systems and BrainLab, Feldkirchen, Germany). The dose was 55 Gy in five daily fractions, and the treatment was continued for 7 days including a weekend.
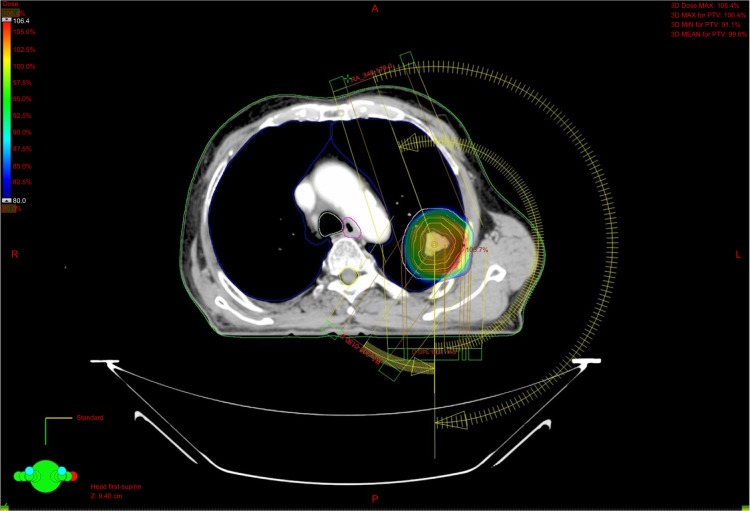
Figure 3.
SBRT plan with volumetric modulated arc technique.
Note: Three arcs were used from 340° to 179° (clockwise and counterclockwise) and from 215° to 180°.
Abbreviation: SBRT, stereotactic body radiation therapy.
The patient was closely followed-up at the outpatient clinic every 1–2 weeks for 2 months and once every 1–3 months thereafter. Follow-up featured physical examination, a complete blood count, a liver function test, and a chest X-ray or CT. A much-reduced small nodule was shown on chest CT 2 months after SBRT. Chest CT 1 year after SBRT demonstrated only irregular consolidation around the treated region, indicating a complete tumor response along with radiation fibrosis (Figure 4).9 During the follow-up period, the patient had no other symptoms except an intermittent cough. The patient remains alive with no evidence of disease 18 months after treatment.
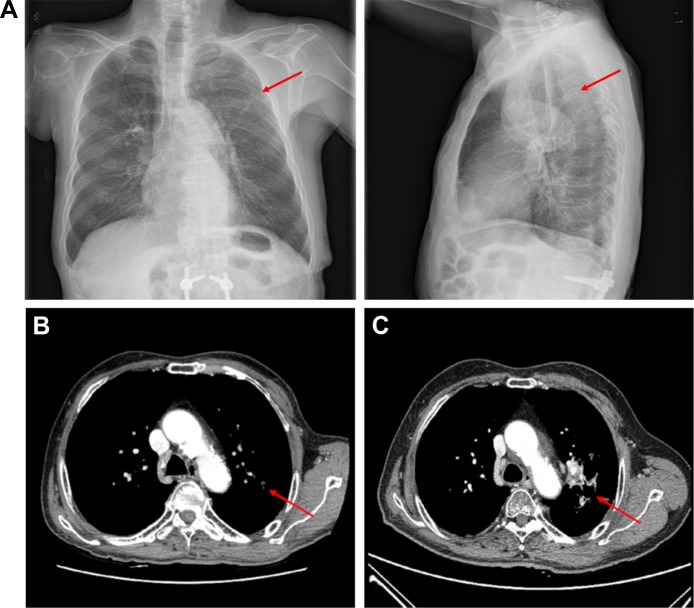
Figure 4.
Posttreatment chest images.
Notes: Chest X-ray (A) and CT (B) 2 months after SBRT revealed a greatly regressed small nodule (red arrows). (C) Chest CT performed 1 year after SBRT evidenced only irregular consolidation around the treated region, indicating a complete tumor response (red arrow) and development of radiation fibrosis.
Abbreviations: CT, computed tomography; SBRT, stereotactic body radiation therapy.
Discussion
LCNEC is very rare and occurs in ~1% of all lung cancers, which is also the case in Korea.2 This tumor is usually found in males, and the median age is 64 years.10 Smoking history greatly influences this tumor. Only limited information on the natural history, clinical course, and optimal management of LCNEC patients is available. LCNEC, together with SCLC, was grouped into neuroendocrine neoplasms in the 2015 WHO classification; however, the National Comprehensive Cancer Network recommends treatment according to the NSCLC guidelines.11 Some studies have suggested that SCLC-based chemotherapy regimens with platinum and etoposide should be used, while others have shown that an NSCLC-based chemotherapy regimen is better.12–14 Surgical resection is recommended for patients with nonmetastatic tumors, reflecting the NSCLC treatment guidelines.4,15
Only a small number of patients with LCNEC have received (conventionally fractionated) RT. Among them, some were treated with postoperative RT alone or concurrent chemoradiotherapy (CCRT) with 50–60 Gy,16,17 or definitive CCRT with 66–70.5 Gy,16 or preoperative RT with 40 Gy.18 Rieber et al16 reported the use of postoperative RT in cases of pathologic N2 disease or incomplete resection after surgery, and definitive CCRT was performed at more advanced stages in inoperable patients. Rieber et al16 also reported 2- and 5-year overall survival rates of 39% and 29%, respectively, in stage III–IV LCNEC. In addition, the 2- and 5-year progression-free survival was 74% and 38%, respectively, in all stages, indicating that RT effectively treats LCNEC. Filosso et al17 reported the use of adjuvant RT without chemotherapy in all patients with more advanced stage than IB after surgery. Filosso et al17 also reported 3- and 5-year overall survival rates of 63% and 35%, respectively. Maeda et al18 reported that 66% of the tumor volume was reduced by using only 40 Gy of CCRT; therefore, preoperative CCRT should be considered a treatment option to facilitate complete resection.
SBRT is characterized by high-level irradiation with a marked difference in the dose gradients to the tumor and normal tissues, and was associated with significantly improved local control and overall survival (compared with conventional RT) in medically inoperable patients with early stage NSCLC.8,19,20 In addition, SBRT is safe and convenient even for patients with poor lung function caused by smoking or underlying pulmonary disease.8,21 However, SBRT is not yet an established treatment option for early stage SCLC. Only a few experimental case series have used SBRT to this end.8,22 In the LCNEC context, a few SBRT studies on early stage NSCLC patients included cases with LCNEC histology, but the treatment outcomes were not separately described.23 To the best of our knowledge, our present study is the first to report the outcomes of SBRT in an LCNEC patient.
Our patient refused surgery but requested RT. SBRT featured 55 Gy delivered in five fractions. The patient completed treatment without any adverse effects. The patient has been relapse-free for 18 months post SBRT, although further long-term follow-up is required.
Conclusion
We report an early stage LCNEC case treated via SBRT. If surgical resection is not possible in early stage LCNEC patients, SBRT could be a favorable treatment method.
Acknowledgments
This work was supported by the Soonchunhyang University Research Fund.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Derks JL, Hendriks LE, Buikhuisen WA, et al. Clinical features of large cell neuroendocrine carcinoma: a population-based overview. Eur Respir J. 2016;47(2):615–624. doi: 10.1183/13993003.00618-2015. [DOI] [PubMed] [Google Scholar]
- 2.Shin A, Oh CM, Kim BW, Woo H, Won YJ, Lee JS. Lung cancer epidemiology in Korea. Cancer Res Treat. 2017;49(3):616–626. doi: 10.4143/crt.2016.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iyoda A, Makino T, Koezuka S, Otsuka H, Hata Y. Treatment options for patients with large cell neuroendocrine carcinoma of the lung. Gen Thorac Cardiovasc Surg. 2014;62(6):351–356. doi: 10.1007/s11748-014-0379-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Welter S, Aigner C, Roesel C. The role of surgery in high grade neuroendocrine tumours of the lung. J Thorac Dis. 2017;9(Suppl 15):S1474–S1483. doi: 10.21037/jtd.2017.01.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu XJ, Dai WR, Xu Y. Survival outcome after stereotactic body radiation therapy and surgery for early stage non-small cell lung cancer: a meta-analysis. J Invest Surg. 2017:1–8. doi: 10.1080/08941939.2017.1341573. [DOI] [PubMed] [Google Scholar]
- 6.Yeo SG, Kim ES. Efficient approach for determining four-dimensional computed tomography-based internal target volume in stereotactic radiotherapy of lung cancer. Radiat Oncol J. 2013;31(4):247–251. doi: 10.3857/roj.2013.31.4.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang JY, Senan S, Paul MA, et al. Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Oncol. 2015;16(6):630–637. doi: 10.1016/S1470-2045(15)70168-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yeo SG, Kim MJ. Stereotactic body radiation therapy for the treatment of a post-chemotherapy remnant lung mass in extensive-stage small-cell lung cancer: a case report. Exp Ther Med. 2016;12(2):1185–1188. doi: 10.3892/etm.2016.3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang K, Palma DA, IASLC Advanced Radiation Technology Committee Follow-up of patients after stereotactic radiation for lung cancer: a primer for the nonradiation oncologist. J Thorac Oncol. 2015;10(3):412–419. doi: 10.1097/JTO.0000000000000435. [DOI] [PubMed] [Google Scholar]
- 10.Park MS, Kim KD, Chung JH, et al. Clinical features of pulmonary large cell neuroendocrine carcinoma. Cancer Res Treat. 2003;35(3):245–253. doi: 10.4143/crt.2003.35.3.245. [DOI] [PubMed] [Google Scholar]
- 11.Naidoo J, Santos-Zabala ML, Iyriboz T, et al. Large cell neuroendocrine carcinoma of the lung: clinico-pathologic features, treatment, and outcomes. Clin Lung Cancer. 2016;17(5):e121–e129. doi: 10.1016/j.cllc.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun JM, Ahn MJ, Ahn JS, et al. Chemotherapy for pulmonary large cell neuroendocrine carcinoma: similar to that for small cell lung cancer or non-small cell lung cancer? Lung Cancer. 2012;77(2):365–370. doi: 10.1016/j.lungcan.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 13.Rossi G, Cavazza A, Marchioni A, et al. Role of chemotherapy and the receptor tyrosine kinases KIT, PDGFRalpha, PDGFRbeta, and Met in large-cell neuroendocrine carcinoma of the lung. J Clin Oncol. 2005;23(34):8774–8785. doi: 10.1200/JCO.2005.02.8233. [DOI] [PubMed] [Google Scholar]
- 14.Derks JL, van Suylen RJ, Thunnissen E, et al. Chemotherapy for pulmonary large cell neuroendocrine carcinomas: does the regimen matter? Eur Respir J. 2017;49(6):1601838. doi: 10.1183/13993003.01838-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kujtan L, Muthukumar V, Kennedy KF, Davis JR, Masood A, Subramanian J. The role of systemic therapy in the management of stage I large cell neuroendocrine carcinoma of the lung. J Thorac Oncol. 2018;13(5):707–714. doi: 10.1016/j.jtho.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 16.Rieber J, Schmitt J, Warth A, et al. Outcome and prognostic factors of multimodal therapy for pulmonary large-cell neuroendocrine carcinomas. Eur J Med Res. 2015;20(1):64. doi: 10.1186/s40001-015-0158-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Filosso PL, Ruffini E, Oliaro A, et al. Large-cell neuroendocrine carcinoma of the lung: a clinicopathologic study of eighteen cases and the efficacy of adjuvant treatment with octreotide. J Thorac Cardiovasc Surg. 2005;129(4):819–824. doi: 10.1016/j.jtcvs.2004.05.023. [DOI] [PubMed] [Google Scholar]
- 18.Maeda A, Nakata M, Yasuda K, et al. Unknown primary large cell neuroendocrine carcinoma (LCNEC) in the mediastinum. Gen Thorac Cardiovasc Surg. 2013;61(9):542–545. doi: 10.1007/s11748-012-0157-5. [DOI] [PubMed] [Google Scholar]
- 19.Widder J, Postmus D, Ubbels JF, Wiegman EM, Langendijk JA. Survival and quality of life after stereotactic or 3D-conformal radiotherapy for inoperable early-stage lung cancer. Int J Radiat Oncol Biol Phys. 2011;81(4):e291–e297. doi: 10.1016/j.ijrobp.2011.03.052. [DOI] [PubMed] [Google Scholar]
- 20.Kim K, Lee J, Cho Y, et al. Predictive factors of symptomatic radiation pneumonitis in primary and metastatic lung tumors treated with stereotactic ablative body radiotherapy. Radiat Oncol J. 2017;35(2):163–171. doi: 10.3857/roj.2017.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guckenberger M, Andratschke N, Alheit H, et al. Definition of stereotactic body radiotherapy: principles and practice for the treatment of stage I non-small cell lung cancer. Strahlenther Onkol. 2014;190(1):26–33. doi: 10.1007/s00066-013-0450-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stahl JM, Corso CD, Verma V, et al. Trends in stereotactic body radiation therapy for stage I small cell lung cancer. Lung Cancer. 2017;103:11–16. doi: 10.1016/j.lungcan.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 23.Chang JY, Liu YH, Zhu Z, et al. Stereotactic ablative radiotherapy: a potentially curable approach to early stage multiple primary lung cancer. Cancer. 2013;119(18):3402–3410. doi: 10.1002/cncr.28217. [DOI] [PMC free article] [PubMed] [Google Scholar]