Abstract
Background
Ischaemic heart disease (IHD) is a major barrier to sustainable human development, but its health burden and geographic distribution among provinces of China remain unclear. This study aimed to estimate IHD burden in provinces of China, and attributable to risk factors from 1990 to 2015.
Methods
Data were collected from the Global Burden of Disease 2015 Study, which evaluated IHD burden and attributable risk factors using deaths and disability-adjusted life years (DALYs). Statistical models including cause of death ensemble modelling, Bayesian meta-regression analysis, and comparative risk assessment approaches were applied to reduce bias and produce comprehensive results of IHD deaths, DALYs and attributable risks. The 95% uncertainty intervals (UIs) were calculated and reported for mortality and DALYs.
Results
The age-standardised death rate per 100,000 people increased by 13.3% from 101.3 (95%UI: 95.3–107.5) to 114.8 (95%UI: 109.8–120.1) from 1990 to 2015 in China, whereas the age-standardised DALY rate declined 3.9% to 1760.2 per 100,000 people (95%UI: 1671.6–1864.3). In 2015, the age-standardised death rate per 100,000 people was the highest in Heilongjiang (187.4, 95%UI: 161.6–217.5) and the lowest in Shanghai (44.2, 95%UI: 37.0–53.1), and the age-standardised DALY rate per 100,000 people was the highest in Xinjiang (3040.8, 95%UI: 2488.8–3735.4) and the lowest in Shanghai (524.4, 95%UI: 434.7–638.4). Geographically, the age-standardised death and DALY rates for southern provinces were lower than northern provinces, especially in southeastern coastal provinces. 95.3% of the IHD burden in China was attributable to environmental, behavioural and metabolic risk factors. The five leading IHD risks in 2015 were high systolic blood pressure, high total cholesterol, diet high in sodium, diet low in whole grains, and smoking.
Conclusions
Population growth and ageing has led to a steady increase in the IHD burden. Regional disparities in IHD burden were observed in provinces of China. The distribution characteristics of IHD burden provide guidance for decision makers to formulate targeted preventive policies and interventions.
Electronic supplementary material
The online version of this article (10.1186/s12872-018-0761-0) contains supplementary material, which is available to authorized users.
Keywords: Ischaemic heart disease, Mortality, Disability-adjusted life years, Risk factors
Background
Cardiovascular diseases (CVDs), which accounted for one-third of global deaths in 2015, are recognised as a major barrier to sustainable human development [1, 2]. Of all CVDs, ischaemic heart disease (IHD) is one of the leading causes of mortality and disease burden worldwide [3], resulting in approximately 8.9 million deaths and 164.0 million disability-adjusted life years (DALYs) globally in 2015 [4–6]. A number of risk factors have been found to be associated with IHD such as hypertension, high total cholesterol, diet high in sodium, and smoking [7–9]. Additionally, mortality from IHD has decreased in developed countries in the past three decades [10] but has increased continuously in many low- and middle- income countries [11–14].
China, one of the largest developing countries in the world, has undergone rapid health transition in the past decades under the background of economic growth and social change. The prevalence and mortality of non-communicable diseases (NCDs), including IHD, has been rising rapidly in China [15]. Therefore, the Chinese Government has implemented the Plan of Healthy China 2030 in response to the Sustainable Development Goals (target 3.4.1) by the United Nations to reduce premature mortality from major NCDs [16, 17]. Furthermore, IHD is one of the major health threats to Chinese people and was the second leading causes of mortality next to stroke in 2013 [18]. However, IHD burden and its geographic distribution among provinces of China remain unclear due to the lack of comparable data. The Global Burden of Diseases, Injuries, and Risk Factors 2015 Study (GBD 2015) estimated health lost from fatal and non-fatal outcomes by integrating all available data on incidence, prevalence, and mortality to produce accurate, consistent, transparent, and up-to-date estimates for global, regions, nations, and subnational regions for some countries [2, 19]. In this study, we aimed to estimate the disease burden of IHD on mortality and DALYs in various provinces of China, as well as DALYs attributed to IHD risk factors, by using the data from the GBD 2015 study.
Methods
Data sources
Data for this study were obtained from the GBD 2015 study, which estimated the burden of 315 diseases and injuries, 2619 unique sequelae, and 79 risk factors in 195 countries worldwide from 1990 to 2015 [4–7]. Original data from three main data sources including the Disease Surveillance Points (DSPs), the Maternal and Child Surveillance System, and the Chinese Center for Disease Control and Prevention (CDC) Cause of Death Reporting System were adapted by the GBD 2015 collaborators to estimate outcomes of IHD in China. IHD cases were identified using the World Health Organization clinical criteria and the 10th revision of the International Classification of Diseases and Injuries (ICD-10) discharge diagnosis codes (codes I20-I25).
Mortality, disability-adjusted life years and risk factors
The general methodological approaches of GBD 2015 and the specific methodology used to study IHD in China have been described elsewhere [4–7]. We used mortality and DALYs to measure the burden caused by IHD. DALYs from IHD consisted of two parts, years of life lost (YLLs) that quantifies life loss caused by premature mortality from fatal IHD and years lived with disability (YLDs) that evaluates health loss from living with non-fatal IHD sequelae such as non-fatal myocardial infarction, angina, and ischaemic heart failure [6, 20]. Cause of Death Ensemble modelling (CODEm) was the principal method adapted to estimate fatal IHD mortality and YLLs [4]. Prevalence for non-fatal IHD sequelae was estimated using Bayesian meta-regression analysis using the DisMod-MR 2.1 software, and its disability weight was evaluated by population-based health surveys and an open web-based survey [5, 21]. We computed DALYs via the summation of YLLs and YLDs [5]. Comparative risk assessment (CRA) approaches were used to evaluate the number of excess DALYs from IHD observed in a given year that can be attributed to past exposure to a risk factor [7]. We used the revised GBD 2015 global population age standard to determine all the age-standardised death and DALY rates.
Uncertainty interval
For each estimated rate and number of deaths and DALYs, we reported its 95% uncertainty interval (UI), which was estimated by taking 1000 samples from the posterior distribution of each quantity and using the 25th and 975th-ordered draws of the uncertainty distribution [4–7].
Results
Mortality
The IHD death rate per 100,000 people in China increased significantly from 52.2 (95%UI: 49.2–55.6) in 1990 to 105.6 (95%UI: 101.0–110.8) in 2015. A total of 1461.2 thousand IHD deaths (95%UI: 1396.8–1532.9) occurred in 2015 in China compared to 6,03.1 thousand in 1990. IHD deaths accounted for 15.5% of all deaths in 2015, ranking only next to stroke (20.1%), with a sharp increase from 6.8% in 1990. Nevertheless, the age-standardised death rate only increased slightly in both males (19.5%) and females (4.5%) from 1990 to 2015. Of all IHD deaths in 2015, 58.0% were in males and 66.4% were in those aged 70+ years.
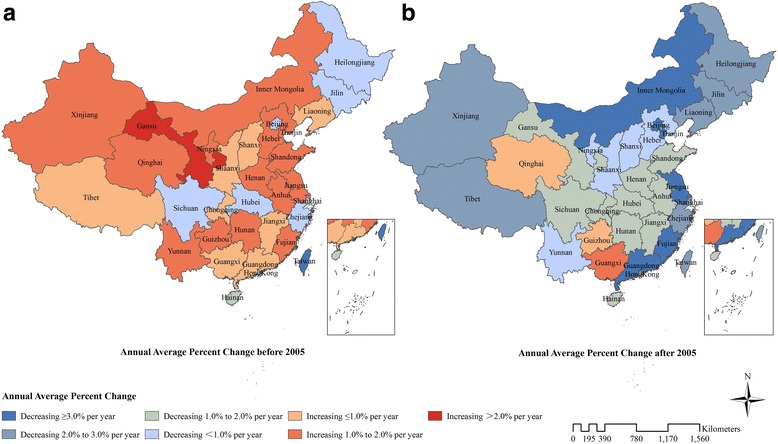
Table 1 provides the number of deaths and age-standardised death rates from IHD in various provinces of China from 1990 to 2015. In 2015, Shandong had the greatest number of IHD deaths at 146.4 thousand (95%UI: 123.6–171.5), and Heilongjiang had the highest age-standardised death rate at 187.4 per 100,000 people (95%UI: 161.6–217.5) followed by Jilin and Xinjiang. The lowest age-standardised death rate occurred in Shanghai with 44.2 per 100,000 people (95%UI: 37.0–53.1) followed by Zhejiang and Hong Kong. Age-standardised death rates for southern provinces were lower than northern provinces, especially in southeastern coastal provinces such as Shanghai, Zhejiang, Hong Kong, Jiangsu, and Fujian (Fig. 1a). Age-standardised death rates for 22 provinces increased while the remaining 11 provinces decreased between 1990 and 2015; the highest increases occurred in Qinghai (54.0%), Shandong, and Hunan, and the largest declines were observed in Macao (− 52.3%), Hong Kong, and Beijing.
Table 1.
Number of deaths and age-standardised death rates from ischaemic heart disease with percent change, 1990–2015, in provinces of China
| Locations | Number of deaths (thousand) | Age-standardized death rate per 100,000 people | ||||
|---|---|---|---|---|---|---|
| 1990 | 2015 | % change | 1990 | 2015 | % change | |
| China | 603.1 (568.0–642.2) |
1461.2 (1396.8–1532.9) |
142.3 | 101.3 (95.3–107.5) |
114.8 (109.8–120.1) |
13.3 |
| Anhui | 22.8 (18.4–28.7) |
65.2 (55.3–76.8) |
186.0 | 86.6 (69.9–106.1) |
107.8 (91.7–126.1) |
24.4 |
| Beijing | 7.5 (6.0–9.2) |
16.9 (14.6–19.7) |
125.7 | 116.7 (94.9–141.2) |
86.5 (74.7–100.6) |
−25.9 |
| Chongqing | 6.5 (5.2–8.1) |
28.3 (22.0–34.7) |
332.3 | 73.2 (58.9–89.8) |
87.3 (69.1–105.8) |
19.3 |
| Fujian | 11.0 (8.9–13.6) |
22.7 (18.5–27.1) |
105.9 | 78.0 (64.0–94.8) |
70.7 (57.7–84.1) |
−9.4 |
| Gansu | 7.8 (6.2–9.6) |
23.3 (19.0–27.9) |
197.0 | 87.8 (71.3–105.5) |
117.3 (97.6–138.2) |
33.6 |
| Guangdong | 30.4 (24.1–37.5) |
79.7 (69.2–92.2) |
162.3 | 94.9 (75.8–116.1) |
97.7 (85.0–112.7) |
2.9 |
| Guangxi | 21.7 (17.5–26.9) |
61.1 (50.6–72.8) |
181.6 | 98.6 (79.4–121.7) |
136.3 (113.4–161.7) |
38.3 |
| Guizhou | 12.7 (10.1–16.0) |
34.5 (27.1–43.7) |
172.1 | 87.7 (70.3–109.8) |
114.6 (91.0–143.0) |
30.7 |
| Hainan | 4.0 (3.2–4.9) |
7.5 (6.0–9.3) |
88.2 | 120.2 (98.6–145.4) |
91.5 (72.7–113.2) |
−23.9 |
| Hebei | 38.4 (30.0–48.5) |
92.7 (77.1–111.7) |
141.6 | 114.3 (90.3–141.6) |
143.5 (120.8–169.7) |
25.5 |
| Heilongjiang | 28.2 (21.9–35.3) |
66.7 (56.3–78.7) |
136.4 | 198.0 (158.3–242.3) |
187.4 (161.6–217.5) |
−5.4 |
| Henan | 55.1 (44.0–67.2) |
121.7 (101.2–146.6) |
120.8 | 119.8 (96.2–144.7) |
152.4 (127.7–181.4) |
27.2 |
| Hong Kong Special Administrative Region of China | 4.2 (3.9–4.7) |
7.4 (6.6–8.7) |
78.6 | 91.7 (85.5–103.6) |
58.3 (52.1–67.7) |
−36.4 |
| Hubei | 27.5 (22.1–33.9) |
58.4 (49.1–69.1) |
112.5 | 106.5 (86.8–129.6) |
111.4 (94.8–131.3) |
4.6 |
| Hunan | 31.1 (24.6–38.6) |
93.5 (79.5–110.2) |
201.0 | 99.4 (79.8–121.7) |
139.2 (118.1–163.3) |
40.0 |
| Inner Mongolia | 13.7 (10.8–17.4) |
32.3 (26.7–38.5) |
136.5 | 157.0 (127.8–193.9) |
158.7 (134.1–184.1) |
1.1 |
| Jiangsu | 23.5 (18.5–29.7) |
55.7 (47.1–65.2) |
137.0 | 59.5 (47.3–74.7) |
63.4 (53.8–74.2) |
6.5 |
| Jiangxi | 17.1 (13.6–21.3) |
38.2 (31.8–45.3) |
123.4 | 101.6 (81.5–124.5) |
106.4 (89.3–124.9) |
4.8 |
| Jilin | 22.3 (17.7–28.0) |
45.4 (36.5–56.8) |
103.3 | 201.9 (165.0–248.9) |
182.0 (148.4–223.1) |
−9.9 |
| Liaoning | 28.1 (22.3–34.6) |
66.0 (56.7–77.2) |
134.8 | 129.6 (104.3–156.8) |
135.7 (117.6–157.1) |
4.7 |
| Macao Special Administrative Region of China | 0.41 (0.36–0.46) |
0.43 (0.34–0.54) |
6.0 | 174.0 (153.2–194.4) |
83.1 (64.7–103.2) |
−52.3 |
| Ningxia | 2.0 (1.5–2.4) |
7.2 (5.6–9.1) |
266.0 | 122.0 (97.7–148.7) |
166.8 (133.8–206.2) |
36.7 |
| Qinghai | 1.8 (1.4–2.2) |
6.6 (5.1–8.5) |
278.8 | 114.6 (91.5–141.6) |
176.5 (140.2–218.6) |
54.0 |
| Shaanxi | 17.1 (13.7–21.2) |
47.3 (36.0–58.8) |
177.5 | 113.0 (91.8–138.0) |
151.9 (119.6–184.4) |
34.5 |
| Shandong | 50.3 (41.0–61.2) |
146.4 (123.6–171.5) |
191.0 | 103.8 (84.0–125.1) |
145.9 (123.6–170.4) |
40.6 |
| Shanghai | 5.9 (4.7–7.1) |
13.1 (11.0–15.7) |
123.2 | 57.6 (46.3–69.2) |
44.2 (37.0–53.1) |
−23.3 |
| Shanxi | 16.6 (13.2–20.8) |
41.0 (31.4–51.5) |
146.5 | 114.9 (92.9–141.9) |
137.4 (108.5–168.8) |
19.6 |
| Sichuan | 47.7 (38.6–59.5) |
65.4 (51.9–80.8) |
37.0 | 88.1 (72.2–108.4) |
75.4 (60.3–92.4) |
−14.4 |
| Tianjin | 6.8 (5.5–8.5) |
16.8 (14.2–19.6) |
145.5 | 126.4 (103.3–153.2) |
134.8 (115.6–155.4) |
6.7 |
| Tibet | 1.4 (1.1–1.9) |
2.3 (1.8–2.8) |
61.0 | 138.6 (107.7–185.2) |
135.6 (110.3–168.7) |
−2.1 |
| Xinjiang | 10.9 (8.6–13.8) |
27.1 (22.2–33.2) |
148.0 | 169.5 (137.3–211.1) |
178.4 (148.5–214.2) |
5.2 |
| Yunnan | 14.7 (11.7–18.5) |
44.6 (37.1–54.3) |
202.9 | 86.0 (68.6–107.2) |
118.2 (99.2–142.2) |
37.4 |
| Zhejiang | 14.0 (11.3–17.1) |
26.0 (21.3–31.2) |
85.6 | 57.1 (46.5–68.9) |
45.0 (37.0–53.8) |
−21.2 |
Fig. 1.

Age-standardised death rate (a) and age-standardised DALY rate (b) from ischaemic heart disease for both sexes combined in 2015 in China. DALYs = disability-adjusted life years
YLLs and YLDs
In 2015, YLLs from IHD was 24,407.2 thousand person years (95%UI: 23,041.1–25,809.1), which increased by 84.6% from 13,221.8 thousand (95%UI: 12,382.0–14,098.7) in 1990. However, the age-standardised YLL rate per 100,000 people decreased 4.3% from 1761.1 (95%UI: 1656.4–1877.2) in 1990 to 1671.9 (95%UI: 1585.1–1763.4) in 2015 (Table 2). Among all provinces, Xinjiang had the highest age-standardised YLL rate at 2956.7 (95%UI: 2403.7–3659.6) in 2015, and the lowest occurred in Shanghai at 427.6 (95%UI: 346.8–536.0). Age-standardised YLL rates for 20 provinces decreased whereas the remaining 13 provinces increased from 1990 to 2015; Macao showed the most rapid decline while Qinghai experienced the most rapid increase.
Table 2.
Age-standardised YLL and YLD rates and YLLs/YLDs ratios for ischaemic heart disease in 1990 and 2015 in provinces of China
| Province | Age-standardized YLL rate per 100,000 people | Age-standardized YLD rate per 100,000 people | YLL/YLD ratio 1990 | YLL/YLD ratio 2015 | ||||
|---|---|---|---|---|---|---|---|---|
| 1990 | 2015 | % change | 1990 | 2015 | % change | |||
| China | 1761.1 (1656.4–1877.2) |
1671.9 (1585.1–1763.4) |
−4.3 | 71.3 (47.9–97.7) |
88.3 (59.4–120.9) |
23.8 | 25.2 | 18.0 |
| Anhui | 1426.7 (1137.0–1795.5) |
1505.4 (1249.9–1812.1) |
5.5 | 70.9 (48.1–97.7) |
87.5 (58.4–120.7) |
23.5 | 19.8 | 16.4 |
| Beijing | 1849.3 (1477.0–2306.9) |
1040.6 (873.1–1251.1) |
−43.7 | 90.4 (61.4–124.2) |
111.3 (76.0–153.9) |
23.0 | 20.3 | 8.9 |
| Chongqing | 1216.8 (968.3–1527.6) |
1215.7 (925.1–1533.8) |
−0.1 | 63.7 (42.3–88.3) |
79.2 (52.9–110.1) |
24.4 | 18.7 | 14.5 |
| Fujian | 1307.5 (1054.8–1636.3) |
925.6 (738.6–1128.8) |
− 29.2 | 68.6 (46.4–94.4) |
84.2 (56.7–115.8) |
22.8 | 19.0 | 10.3 |
| Gansu | 1565.7 (1239.1–1908.2) |
1755.2 (1422.3–2120.7) |
12.1 | 64.7 (43.4–88.8) |
80.4 (54.3–110.5) |
24.3 | 24.6 | 20.3 |
| Guangdong | 1611.02 (1259.93–2005.35) |
1272.8 (1087.1–1502.2) |
−21.0 | 74.2 (50.4–102.4) |
91.3 (61.7–125.6) |
23.2 | 22.1 | 13.2 |
| Guangxi | 1719.6 (1377.1–2179.6) |
2152.1 (1748.0–2640.7) |
25.2 | 68.2 (46.0–94.0) |
83.9 (56.8–115.8) |
23.1 | 25.5 | 25.1 |
| Guizhou | 1510.6 (1197.1–1917.9) |
1845.2 (1434.4–2379.7) |
22.2 | 61.7 (41.3–85.7) |
76.9 (51.3–106.5) |
24.6 | 24.2 | 23.0 |
| Hainan | 1957.9 (1559.9–2444.0) |
1315.4 (1006.4–1708.9) |
−32.8 | 67.3 (45.2–93.1) |
83.1 (56.2–114.9) |
23.4 | 28.6 | 15.5 |
| Hebei | 2065.0 (1598.0–2632.7) |
2255.2 (1846.2–2780.1) |
9.2 | 73.2 (49.8–100.8) |
90.0 (60.4–124.5) |
22.9 | 29.4 | 23.9 |
| Heilongjiang | 3606.6 (2791.8–4496.9) |
2761.8 (2291.2–3302.4) |
−23.4 | 80.2 (54.6–109.3) |
98.2 (67.1–133.4) |
22.4 | 49.7 | 26.1 |
| Henan | 2173.8 (1734.0–2676.7) |
2324.5 (1903.3–2855.6) |
6.9 | 75.6 (50.8–104.0) |
93.1 (63.6–127.8) |
23.1 | 30.2 | 24.0 |
| Hong Kong Special Administrative Region of China | 1298.6 (1228.1–1434.1) |
699.7 (624.8–794.3) |
−46.1 | 71.2 (48.1–99.1) |
86.3 (57.2–119.3) |
21.2 | 17.7 | 8.5 |
| Hubei | 1840.91 (1471.74–2290.86) |
1577.4 (1308.6–1890.7) |
−14.3 | 68.7 (46.3–94.5) |
84.6 (57.0–116.4) |
23.1 | 26.9 | 17.1 |
| Hunan | 1733.0 (1364.6–2157.8) |
2004.2 (1664.3–2402.9) |
15.7 | 65.3 (43.5–89.9) |
80.2 (53.7–112.1) |
22.9 | 26.6 | 23.8 |
| Inner Mongolia | 2829.3 (2252.6–3587.8) |
2371.5 (1935.4–2863.1) |
−16.2 | 78.7 (53.5–108.4) |
96.3 (64.9–132.2) |
22.2 | 38.6 | 23.3 |
| Jiangsu | 928.2 (724.2–1179.2) |
787.0 (653.1–944.7) |
− 15.2 | 71.8 (47.8–98.3) |
88.3 (59.7–121.3) |
23.0 | 12.6 | 8.3 |
| Jiangxi | 1703.8 (1351.9–2135.7) |
1482.1 (1206.5–1773.0) |
−13.0 | 67.5 (45.4–92.5) |
82.8 (55.9–113.3) |
22.8 | 25.0 | 16.5 |
| Jilin | 3586.3 (2839.1–4495.1) |
2654.5 (2088.9–3408.8) |
− 26.0 | 80.4 (54.4–110.8) |
97.9 (67.1–135.1) |
21.8 | 47.4 | 25.0 |
| Liaoning | 2236.8 (1763.7–2773.4) |
1875.8 (1578.9–2236.1) |
−16.1 | 84.9 (57.9–115.7) |
103.8 (70.2–142.9) |
22.2 | 27.6 | 16.7 |
| Macao Special Administrative Region of China | 2589.3 (2267.0–2883.6) |
988.1 (763.2–1240.8) |
−61.8 | 90.3 (61.2–124.2) |
110.1 (74.7–151.8) |
21.9 | 28.6 | 8.2 |
| Ningxia | 2085.0 (1626.4–2558.8) |
2552.9 (1963.4–3248.2) |
22.4 | 78.5 (53.0–108.3) |
96.5 (65.4–132.3) |
22.9 | 27.7 | 25.3 |
| Qinghai | 2092.9 (1642.2–2671.4) |
2793.5 (2127.3–3591.7) |
33.5 | 63.3 (42.0–87.5) |
79.0 (53.2–109.8) |
24.8 | 34.6 | 33.3 |
| Shaanxi | 1993.6 (1603.5–2489.0) |
2216.3 (1659.0–2795.6) |
11.2 | 72.2 (49.0–99.3) |
89.8 (60.3–124.4) |
24.3 | 28.6 | 22.8 |
| Shandong | 1808.6 (1466.0–2224.1) |
2043.7 (1698.1–2462.8) |
13.0 | 77.0 (52.2–106.2) |
95.0 (64.8–130.1) |
23.4 | 24.1 | 20.3 |
| Shanghai | 802.7 (640.8–982.9) |
427.6 (346.8–536.0) |
−46.7 | 78.5 (53.2–108.0) |
96.8 (65.7–133.2) |
23.3 | 9.7 | 4.1 |
| Shanxi | 2092.7 (1651.9–2621.9) |
2117.0 (1592.1–2701.9) |
1.2 | 75.3 (51.1–104.3) |
92.8 (63.2–126.9) |
23.2 | 29.2 | 21.9 |
| Sichuan | 1468.84 (1184.9–1844.6) |
1092.6 (841.8–1371.1) |
− 25.6 | 60.6 (40.1–83.0) |
75.0 (49.9–103.5) |
23.7 | 23.4 | 13.7 |
| Tianjin | 2205.8 (1759.3–2747.8) |
1780.0 (1492.3–2154.6) |
−18.4 | 90.8 (62.2–125.1) |
112.2 (77.7–153.3) |
23.6 | 25.5 | 15.1 |
| Tibet | 2682.3 (2055.1–3581.9) |
2257.6 (1809.1–2847.6) |
−15.8 | 57.0 (38.1–79.9) |
71.2 (47.2–98.9) |
24.9 | 49.3 | 31.8 |
| Xinjiang | 3177.8 (2481.1–4037.5) |
2956.7 (2403.7–3659.6) |
− 7.0 | 68.0 (45.9–93.0) |
84.0 (56.0–115.7) |
23.5 | 50.0 | 35.0 |
| Yunnan | 1526.2 (1205.6–1927.2) |
1884.4 (1537.7–2325.8) |
23.5 | 63.2 (42.4–87.7) |
78.3 (52.4–109.8) |
23.8 | 24.3 | 23.4 |
| Zhejiang | 864.4 (685.2–1069.9) |
552.3 (446.4–673.8) |
− 36.1 | 68.4 (45.9–94.7) |
83.7 (55.8–114.3) |
22.4 | 12.1 | 6.2 |
YLLs = years of life lost, YLDs = years lived with disability
IHD caused an estimated 1358.0 thousand YLDs (95%UI: 915.7–1870.3) in China in 2015, which was 2.5 times higher than the YLDs in 1990 at 524.6 thousand (95%UI: 352.5–720.2). The age-standardised YLD rate per 100,000 people rose 23.8% from 71.3 (95%UI: 47.9–97.7) to 88.3 (95%UI: 59.4–120.9) (Table 2). All provinces experienced increases in age-standardised YLD rates between 1990 and 2015. In 2015, the highest age-standardised YLD rate appeared in Tianjin, followed by Beijing and Macao, whereas the lowest YLD rate occurred in Tibet.
For IHD, YLLs was much higher than YLDs, as the YLLs/YLDs ratio for IHD was 25.2 in 1990 and reduced to 18.0 in 2015. Although the ratios decreased for all provinces during 1990 to 2015, they remained greater than 10 for most provinces.
DALYs
IHD caused a total of 2576.5 thousand DALYs (95%UI: 2439.1–2737.4) in China in 2015, accounting for 7.5% of total DALYs from all causes, ranking only second to stroke (10.1%). The IHD DALY rate per 100,000 people increased from 1190.7 (95%UI: 1120.9–1268.9) in 1990 to 1862.4 (95%UI: 1763.1–1978.6) in 2015. However, the age-standardised DALY rate showed a 3.9% reduction to 1760.2 (95%UI: 1671.6–1864.3) in 2015.
Table 3 shows the number of DALYs and age-standardised IHD DALY rates for various provinces of China in 1990 and 2015. IHD DALYs for all provinces increased except in Macao. Xinjiang had the highest age-standardised DALY rate at 3040.8 per 100,000 people (95%UI: 2488.8–3735.4) in 2015, followed by Qinghai and Heilongjiang, while Shanghai, Zhejiang and Hong Kong had the lowest rates. Age-standardised DALY rates for southern provinces were lower than northern provinces, especially in southeastern coastal provinces (Fig. 1b). Nineteen provinces showed a downward trend for age-standardised DALY rates with the most rapid decline observed in Macao, Hong Kong, and Beijing. The remaining 14 provinces showed an upward trend, where Qinghai, Guangxi and Yunnan had the fastest growth rate. Before 2005, the age-standardised DALY rates for most provinces increased except in ten provinces including Macao, Hong Kong, Hainan, Shanghai, Sichuan, Zhejiang, Beijing, Hubei, Jilin and Heilongjiang. However, after 2005, the age-standardised DALY rates for the majority of provinces declined except in Guangxi, Qinghai, and Guizhou (Fig. 2and Additional file 1).
Table 3.
Number of DALYs and age-standardised DALY rates from ischaemic heart disease with percent change, 1990–2015, in provinces of China
| Province | Number of DALY (thousand) | Age-standardized DALY rate per 100,000 people | ||||
|---|---|---|---|---|---|---|
| 1990 | 2015 | % change | 1990 | 2015 | % change | |
| China | 1374.6 (1294.0–1464.9) |
2576.5 (2439.1–2737.4) |
87.4 | 1832.4 (1728.7–1948.7) |
1760.2 (1671.6–1864.3) |
−3.9 |
| Anhui | 520.8 (411.4–661.6) |
1057.5 (878.0–1264.8) |
103.0 | 1497.6 (1207.2–1870.7) |
1592.9 (1331.6–1895.2) |
6.4 |
| Beijing | 159.0 (126.7–201.3) |
266.1 (224.9–320.0) |
67.3 | 1939.7 (1566.7–2398.3) |
1151.9 (982.1–1369.1) |
− 40.6 |
| Chongqing | 143.8 (113.5–181.0) |
462.3 (356.0–581.1) |
221.5 | 1280.5 (1027.7–1588.0) |
1294.9 (1002.3–1615.8) |
1.1 |
| Fujian | 244.5 (195.9–308.2) |
362.5 (292.0–435.5) |
48.3 | 1376.1 (1116.7–1710.6) |
1009.8 (818.3–1206.1) |
−26.6 |
| Gansu | 205.5 (160.8–252.1) |
466.1 (375.0–567.3) |
126.8 | 1630.4 (1309.0–1969.3) |
1835.6 (1494.7–2194.7) |
12.6 |
| Guangdong | 639.6 (501.8–797.2) |
1261.2 (1076.4–1505.2) |
97.2 | 1685.2 (1334.3–2088.1) |
1364.1 (1174.2–1600.6) |
−19.1 |
| Guangxi | 463.9 (368.3–588.2) |
1088.1 (885.8–1329.0) |
134.5 | 1787.8 (1435.2–2241.3) |
2236.0 (1826.4–2717.6) |
25.1 |
| Guizhou | 286.4 (226.2–365.5) |
667.0 (521.9–858.0) |
132.9 | 1572.3 (1259.6–1972.2) |
1922.0 (1513.8–2449.3) |
22.3 |
| Hainan | 79.8 (63.3–101.6) |
123.2 (94.8–159.8) |
54.3 | 2025.2 (1624.4–2519.4) |
1398.5 (1085.1–1796.2) |
−30.9 |
| Hebei | 888.2 (681.8–1137.1) |
1822.5 (1485.1–2261.9) |
105.2 | 2138.2 (1665.4–2702.3) |
2345.2 (1931.9–2865.0) |
9.7 |
| Heilongjiang | 737.4 (559.1–930.4) |
1270.2 (1045.4–1525.8) |
72.2 | 3686.8 (2866.3–4566.4) |
2859.9 (2395.7–3390.3) |
−22.4 |
| Henan | 1269.1 (1006.0–1574.7) |
2242.4 (1832.3–2751.4) |
76.7 | 2249.4 (1800.7–2763.2) |
2417.6 (1998.5–2943.1) |
7.5 |
| Hong Kong Special Administrative Region of China | 69.6 (65.5–76.3) |
90.8 (81.5–102.2) |
30.6 | 1369.7 (1290.2–1505.6) |
786.0 (705.7–881.4) |
−42.6 |
| Hubei | 642.7 (514.3–805.1) |
1034.8 (853.4–1248.9) |
61.0 | 1909.7 (1551.5–2345.8) |
1662.0 (1381.1–1967.2) |
−13.0 |
| Hunan | 706.9 (554.5–878.8) |
1549.0 (1284.5–1859.2) |
119.1 | 1798.3 (1426.3–2218.2) |
2084.4 (1741.6–2484.0) |
15.9 |
| Inner Mongolia | 352.0 (277.0–451.1) |
648.1 (526.2–790.8) |
84.1 | 2908.1 (2332.2–3658.3) |
2467.7 (2026.8–2961.2) |
− 15.1 |
| Jiangsu | 489.5 (384.3–618.0) |
843.0 (710.1–994.9) |
72.2 | 1000.0 (791.4–1250.3) |
875.3 (739.5–1028.2) |
− 12.5 |
| Jiangxi | 378.3 (299.1–477.3) |
656.8 (535.5–790.4) |
73.6 | 1771.3 (1411.3–2196.9) |
1564.9 (1289.6–1858.2) |
−11.7 |
| Jilin | 538.8 (419.2–683.0) |
854.0 (667.2–1114.2) |
58.5 | 3666.7 (2915.4–4577.5) |
2752.4 (2188.9–3502.6) |
−24.9 |
| Liaoning | 637.8 (499.8–798.2) |
1117.1 (943.8–1341.7) |
75.1 | 2321.8 (1845.0–2863.8) |
1979.6 (1681.8–2345.0) |
−14.7 |
| Macao Special Administrative Region of China | 6.7 (5.9–7.5) |
6.6 (5.3–8.3) |
−1.1 | 2679.6 (2355.6–2979.1) |
1098.2 (870.6–1364.4) |
−59.0 |
| Ningxia | 48.6 (36.9–60.3) |
148.4 (113.0–191.0) |
205.3 | 2163.5 (1695.5–2641.8) |
2649.4 (2069.2–3343.4) |
22.5 |
| Qinghai | 48.2 (37.1–62.3) |
138.9 (103.1–182.5) |
187.9 | 2156.2 (1703.9–2737.8) |
2872.5 (2208.7–3675.4) |
33.2 |
| Shaanxi | 418.8 (332.2–525.8) |
899.5 (663.0–1142.5) |
114.8 | 2065.8 (1669.0–2559.3) |
2306.1 (1737.2–2879.4) |
11.6 |
| Shandong | 1114.0 (909.5–1368.5) |
2400.2 (1984.6–2879.7) |
115.5 | 1885.6 (1553.7–2303.5) |
2138.7 (1787.0–2548.1) |
13.4 |
| Shanghai | 108.1 (87.3–131.2) |
161.0 (132.1–196.5) |
49.0 | 881.2 (715.2–1062.1) |
524.4 (434.7–638.4) |
− 40.5 |
| Shanxi | 404.4 (316.4–508.7) |
809.3 (600.2–1047.5) |
100.1 | 2168.0 (1724.6–2701.7) |
2209.8 (1678.3–2811.7) |
1.9 |
| Sichuan | 1057.8 (836.1–1326.3) |
1117.3 (874.9–1389.6) |
5.6 | 1529.5 (1244.9–1902.9) |
1167.6 (923.1–1444.6) |
−23.7 |
| Tianjin | 155.1 (122.5–194.6) |
285.8 (236.6–343.0) |
84.3 | 2296.6 (1845.5–2840.7) |
1912.2 (1605.1–2266.2) |
−16.7 |
| Tibet | 35.3 (26.9–47.0) |
50.2 (40.1–63.9) |
42.4 | 2739.3 (2113.4–3645.6) |
2328.8 (1890.5–2913.8) |
−15.0 |
| Xinjiang | 270.9 (210.0–348.0) |
602.3 (481.9–754.3) |
122.4 | 3245.9 (2557.4–4111.5) |
3040.8 (2488.8–3735.4) |
−6.3 |
| Yunnan | 346.7 (274.6–439.9) |
856.7 (696.1–1062.4) |
147.1 | 1589.4 (1273.6–1993.5) |
1962.7 (1614.1–2407.5) |
23.5 |
| Zhejiang | 278.2 (222.8–342.9) |
406.6 (334.2–489.4) |
46.2 | 932.8 (753.9–1133.3) |
635.9 (524.2–763.4) |
− 31.8 |
DALYs = disability-adjusted life years
Fig. 2.
Annual average percent change of age-standardised DALY rates from ischaemic heart disease for both sexes combined in China before 2005 (a) and after 2005 (b). DALYs = disability-adjusted life years
Risk factors
In China, 95.3% of IHD DALYs (24,561.9 thousand, 95%UI: 23,193.9–26,122.8) were attributable to metabolic, environmental, and behavioural risks and their overlaps in 2015 compared to 91.4% of IHD DALYs (12,560.7 thousand, 95%UI: 11,813.6–13,405.6) in 1990. From 1990 to 2015, the proportion of the three metabolic-related risks and overlaps increased while other clusters decreased, including metabolic risks alone, interaction of behavioural and metabolic risks, and interaction of metabolic and environmental risks (Fig. 3). A substantial portion of IHD DALYs was attributable to behavioural-related risks, including behavioural risks alone (7.8%), interaction of behavioural and metabolic risks (51.1%), and interaction of behavioural and metabolic and environmental risks (25.3%).
Fig. 3.

Proportion of DALYs from ischaemic heart disease attributable to metabolic, environmental and behavioural risk factors and their overlaps, for both sexes combined during 1990 to 2015. DALYs = disability-adjusted life years
Figure 4 shows the changes to the 22 leading risk factors for IHD DALYs between 1990 and 2015 in China. In 2015, the five leading IHD risk factors and their DALY rates per 100,000 people were high systolic blood pressure (1080.1, 95%UI: 922.5–1226.9), high total cholesterol (839.4, 95%UI: 685.0–1004.8), diet high in sodium (825.2, 95%UI: 586.6–1081.7), diet low in whole grain (487.3, 95%UI: 302.0–682.2), and smoking (487.0, 95%UI: 395.6–581.0). DALY rates for all risk factors increased between 1990 and 2015 except for household air pollution from solid fuels. The largest increase in the DALY rate occurred for diet low in polyunsaturated fatty acids (283.5%), followed by high body mass index (160.6%) and high systolic blood pressure (128.4%). However, only seven risk factors increased in age-standardised IHD DALY rates, while the remaining 15 risk factors declined. The age-standardised IHD DALY rate for household air pollution from solid fuels showed the greatest decline (50.3%). Six risk factors, including high systolic blood pressure (2nd to 1st), diet low in whole grains (5th to 4th), ambient particulate matter pollution (8th to 7th), high fasting plasma glucose (11th to 8th), high body-mass index (14th to 11th), and diet low in polyunsaturated fatty acids (20th to 19th), increased in rank between 1990 and 2015.
Fig. 4.
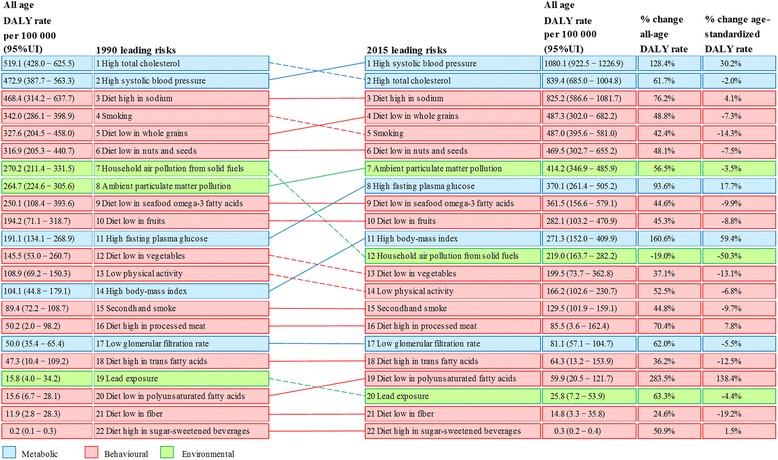
The 22 leading risk factors for DALYs from ischaemic heart disease for both sexes combined in 1990 and 2015 in China. DALYs = disability-adjusted life years
Discussion
Main findings
In this study, we found that the number of deaths and DALYs from IHD have increased significantly in China since 1990, but age-adjusted DALY rate has declined. The IHD burden increased in most provinces before 2005 but declined after 2005. Geographically, the IHD burden in southern provinces were lower than northern provinces, especially in southeastern coastal provinces. Furthermore, 95.3% of the IHD burden in China was attributable to environmental, behavioural and metabolic risk factors. The top five IHD risks were high systolic blood pressure, high total cholesterol, diet high in sodium, diet low in whole grains, and smoking.
Mortality and disability-adjusted life years
IHD was the second leading cause of disease burden in China only after stroke. IHD deaths and DALYs have greatly increased for both sexes since 1990. Moreover, China made the second greatest contribution to global IHD burden after India, accounting for 15.7% of total global IHD DALYs in 2015 [5]. These findings call for comprehensive approaches to prevent and reduce the IHD burden in China.
The IHD death rate and the DALY rate increased greatly, but the age-adjusted death rate and DALY rate showed no obvious increases between 1990 and 2015. These findings were mainly caused by population growth and ageing during this period. YLLs were the main component of IHD burden in China with over 90% of DALYs attributed to YLLs. A global level assessment has shown that YLL rates for CVDs increased with the Socio-demographic Index for countries and regions in the middle of the socio-demographic rankings [4]. Most provinces in China remain in the middle of the socio-demographic rankings despite experiencing an increase in the Socio-demographic Index since 1990 [4]. Evidence has also shown that IHD patients in low- and middle-income countries have less access to affordable and high quality CVD medications [22]. All of these findings imply that, in most provinces of China, economic growth and social development have led to an increase in the life expectancy to allow individuals to survive long enough to develop IHD; however, many of them are not able to access to optimal medical or surgical treatments for IHD. Therefore, both the YLL rate and YLD rate from IHD in China have increased significantly since 1990. However, age-standardised YLL and DALY rates have declined, implying improvements in medical care and social security in China that provided more available and affordable treatments for IHD patients.
Differences in the burden of IHD existed between sexes, time periods, and provinces in China. With respect to gender, the IHD burden was higher and increased more rapidly among males than females. Because females are more sensitive to heath information, females are more likely to seek healthcare and have better access to primary prevention compared to males [23]. Regarding time period, the IHD burden in most provinces increased before 2005 but declined afterwards. This transition occurred for multiple reasons. The increase before 2005 was mainly caused by the increase in prevalence of IHD risk factors such as hypertension, dyslipidaemia, and ambient particulate matter pollution [15]. The IHD burden declined after 2005 partly due to the implementation of many important strategies related to tobacco use, diet, physical activities, and harmful use of alcohol to prevent and control NCDs [24–26]. In addition, improvement in IHD treatments and the application of cardiac rehabilitation in recent years have led to great advances in reducing the mortality in IHD patients. Regarding the various provinces, the IHD burden was lower among southern provinces than northern provinces, especially in southeastern coastal provinces. These regional disparities are observed partly due to the differences in exposure to metabolic and behavioural risk factors, environmental qualities, meteorological conditions, and household income levels between different regions. Southeastern coastal provinces experienced a lighter IHD burden, as these provinces have been shown to have lower prevalence of hypertension and high total cholesterol [27–29], a lower smoking rate [30], lower air pollution [31], higher household income [32], warm climate conditions and eating habits similar to the Mediterranean diet or Japanese diet [33].
Risk factors
In 2015, over 90% of IHD DALYs were attributable to risk factors that are controllable through reducing and managing related metabolic, behavioural and environmental risk factors. Behavioural risk factors remained the main source of IHD burden in China, but proportion of DALYs attributable to metabolic risk factors has increased previously since 1990, which should be brought to the forefront.
Over the past 30 years, the economy and society in China have undergone rapid improvement with demographic transitions and lifestyle changes with a large impact on population health. Exposure to metabolic and behavioural risk factors has increased to high levels in recent years. A recent report on CVDs in China showed that 25.2% of Chinese adults (approximately 270 million) suffered from hypertension and 33.6% had high-normal blood pressure, but their knowledge rate, treatment rate and control rate for hypertension were only 46.5%, 41.1%, and 13.8%, respectively [33]. Approximately 10% of Chinese adults had high total cholesterol and 25% had high triacylglycerol. The smoking rate was 27.7% in resident aged 15 years and 52.1% in males. A 14.5 g daily average salt intake in Chinese adults was much higher than 5 g recommended by WHO [34]. Moreover, approximately 9.7% of adults had diabetes, and the overweight and obesity rates for adults were 30% and 11.9%, respectively [33]. These findings imply the immense potential of prevention through comprehensive risk factor modification to reduce the IHD burden in China [35, 36].
Study limitations
Our study has several limitations. First, since data for this study were mainly obtained from the GBD 2015 study, all limitations of the GBD 2015 methods outlined elsewhere also apply here [4–7]. The GBD 2015 study used big data analytic technologies to integrate heterogeneous data and estimate burden of diseases and risk factors. Although many methods and processes were used to reduce bias, including misclassification corrections, redistribution of garbage codes, and noise reduction, it was difficult to thoroughly avoid inaccuracy. Therefore, our results on the IHD burden in provinces of China should be interpreted carefully, as the data we used were estimates. Second, accurate data such as follow-up data on non-fatal IHD outcomes and prevalence of IHD risk factors by provinces are very limited. Due to the insufficiency of provincial data regarding risk factors, our study lacked analysis of regional differences in IHD risk factors, which should be conducted in the future.
Implication for policies
Our findings indicate priorities for comprehensive approaches to reduce the IHD burden in China. First, policies should be created to reduce population exposure to major IHD risk factors such as hypertension preventing and curing, cholesterol lowering, advocating healthy diets such as the Mediterranean diet, smoking cessation, controlling ambient particulate matter pollution, etc. Second, it is essential to monitor and manage individuals at high risk for IHD such as those with high blood pressure, dyslipidaemia, high body mass index and hyperglycaemia, especially in males and the elderly, on the community level. Furthermore, improvement in medical care, IHD treatments and social security will help provide more available, affordable, and high quality treatments for IHD patients. Lastly, health education programmes need to be launched to increase awareness of the importance of controlling IHD and personal preventive strategies among the general population.
Conclusion
Although age-standardised DALY rate from IHD declined from 1990 to 2015 in China, population growth and ageing have led to sharp increases in deaths and DALYs from IHD. Regional disparities in IHD burden were observed among provinces of China. The IHD burden in most southern provinces was lower than that of northern provinces, especially in southeastern coastal provinces. Metabolic, behavioural, and environmental risk factors contributed to the majority of the IHD burden. The characteristics of IHD burden and IHD risk factors provide guidance for decision makers to formulate targeted preventive policies and interventions.
Additional file
ᅟ. (DOCX 18 kb)
Acknowledgements
We wish to thank the Global Burden of Disease Study 2015 collaborators for providing the data.
Funding
This work is supported by the National Natural Science Foundation of China (Grant No. 81773552 and Grant No. 81273179) and the Chinese NSFC International Cooperation and Exchange Program (Grant No. 71661167007).
Availability of data and materials
The raw data of IHD burden on the national level for China were obtained from the GBD Results Tool (http://ghdx.healthdata.org/gbd-results-tool). Data for provinces are nonpublic, which need to be applied to the National CDC of China.
Abbreviations
- 95%UI
95% uncertainty interval
- CVDs
Cardiovascular diseases
- DALYs
Disability-adjusted life years
- GBD 2015
Global burden of disease, injuries, and risk factors 2015 study
- IHD
Ischaemic heart disease
- NCDs
Non-communicable diseases.
- YLDs
Years lived with disability
- YLLs
Years of life lost
Authors’ contributions
CY and GZ contributed to study conception and design. LW and LL collected the data. GZ, LW, and YZ analysed the data. MZ was the expert from the National CDC of China who helped collect the data and confirm the results. All authors were involved in writing the manuscript and provided final approval of the submitted and published versions.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interest
The authors declare that they have no competing interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ganshen Zhang, Email: gszhang1991@163.com.
Chuanhua Yu, Phone: +86-27-6875-9299, Email: YuCHua@whu.edu.cn.
Maigeng Zhou, Email: maigengzhou@126.com.
Lu Wang, Email: ffdw_03@163.com.
Yunquan Zhang, Email: Yun-quanZhang@whu.edu.cn.
Lisha Luo, Email: 13006362970@163.com.
References
- 1.Clark H. NCDs: a challenge to sustainable human development. Lancet. 2013;381(9866):510–511. doi: 10.1016/S0140-6736(13)60058-6. [DOI] [PubMed] [Google Scholar]
- 2.Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, Ahmed M, Aksut B, Alam T, Alam K, et al. Global, regional, and National Burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, Casey DC, Charlson FJ, Chen AZ, Coates MM, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kassebaum NJ, Arora M, Barber RM, Bhutta ZA, Brown J, Carter A, Casey DC, Charlson FJ, Coates MM, Coggeshall M, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1603–1658. doi: 10.1016/S0140-6736(16)31460-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, Carter A, Casey DC, Charlson FJ, Chen AZ, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forouzanfar MH, Afshin A, Alexander LT, Anderson HR, Bhutta ZA, Biryukov S, Brauer M, Burnett R, Cercy K, Charlson FJ, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grad C, Zdrenghea D. Heart rate recovery in patients with ischemic heart disease risk factors. Clujul Med. 2014;87(4):220–225. doi: 10.15386/cjmed-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aalami Harandi S, Sarrafzadegan N, Sadeghi M, Talaei M, Dianatkhah M, Oveisgharan S, Pourmoghaddas A, Salehi A, Sedighifard Z. Do Cardiometabolic risk factors relative risks differ for the occurrence of ischemic heart disease and stroke? Res Cardiovasc Med. 2016; 10.5812/cardiovascmed.30619. [DOI] [PMC free article] [PubMed]
- 10.Cooper R, Cutler J, Desvigne-Nickens P, Fortmann SP, Friedman L, Havlik R, Hogelin G, Marler J, McGovern P, Morosco G, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: findings of the national conference on cardiovascular disease prevention. Circulation. 2000;102(25):3137–3147. doi: 10.1161/01.CIR.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. World Heart Federation. World Stroke Organization . Global atlas on cardiovascular disease prevention and control: policies, strategies and interventions. 2011. [Google Scholar]
- 12.Nowbar AN, Howard JP, Finegold JA, Asaria P, Francis DP. 2014 global geographic analysis of mortality from ischemic heart disease by country, age and income: Statistics from World Health Organization and United Nations. Int J Cardiol. 2014;174(2):293–298. doi: 10.1016/j.ijcard.2014.04.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barquera S, Pedroza-Tobías A, Medina C, Hernández-Barrera L, Bibbins-Domingo K, Lozano R, Moran AE. Global overview of the epidemiology of atherosclerotic cardiovascular disease. Arch Med Res. 2015;46(5):328–338. doi: 10.1016/j.arcmed.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Gaziano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol. 2010;35(2):72–115. doi: 10.1016/j.cpcardiol.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, Wan X, Yu S, Jiang Y, Naghavi M, et al. Rapid health transition in China, 1990-2010: findings from the global burden of disease study 2010. Lancet. 2013;381(9882):1987–2015. doi: 10.1016/S0140-6736(13)61097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Health and Family Planning Commission of the People's Republic of China . The plan of healthy China 2030. 2016. [Google Scholar]
- 17.Lim SS, Allen K, Bhutta ZA, Dandona L, Forouzanfar MH, Fullman N, Gething PW, Goldberg EM, Hay SI, Holmberg M, et al. Measuring the health-related sustainable development goals in 188 countries: a baseline analysis from the global burden of disease study 2015. Lancet. 2016;388(10053):1813–1850. doi: 10.1016/S0140-6736(16)31467-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, Li Y, Wang L, Liu Y, Yin P, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the global burden of disease study 2013. Lancet. 2016;387(10015):251–272. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 19.Reddy KS. Global burden of disease study 2015 provides GPS for global health 2030. Lancet. 2016;388(10053):1448–1449. doi: 10.1016/S0140-6736(16)31743-3. [DOI] [PubMed] [Google Scholar]
- 20.Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Flaxman A, Murray CJ, Naghavi M. The global burden of ischemic heart disease in 1990 and 2010: the global burden of disease 2010 study. Circulation. 2014;129(14):1493–1501. doi: 10.1161/CIRCULATIONAHA.113.004046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salomon JA, Haagsma JA, Davis A, de Noordhout CM, Polinder S, Havelaar AH, Cassini A, Devleesschauwer B, Kretzschmar M, Speybroeck N, et al. Disability weights for the global burden of disease 2013 study. Lancet Glob Health. 2015;3(11):e712–e723. doi: 10.1016/S2214-109X(15)00069-8. [DOI] [PubMed] [Google Scholar]
- 22.Wirtz VJ, Kaplan WA, Kwan GF, Laing RO. Access to medications for cardiovascular diseases in low- and middle-income countries. Circulation. 2016;133(21):2076–2085. doi: 10.1161/CIRCULATIONAHA.115.008722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barker-Collo S, Bennett DA, Krishnamurthi RV, Parmar P, Feigin VL, Naghavi M, Forouzanfar MH, Johnson CO, Nguyen G, Mensah GA, et al. Sex differences in stroke incidence, prevalence, mortality and disability-adjusted life years: results from the global burden of disease study 2013. Neuroepidemiology. 2015;45(3):203–214. doi: 10.1159/000441103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization . WHO framework convention on tobacco control. World Health Organization. 2003. [Google Scholar]
- 25.World Health Organization . Global strategy on diet, physical activity and health. World Health Organization. 2004. [Google Scholar]
- 26.World Health Organization . Global strategy to reduce the harmful use of alcohol. World Health Organization. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li D, Lv J, Liu F, Liu P, Yang X, Feng Y, Chen G, Hao M. Hypertension burden and control in mainland China: analysis of nationwide data 2003-2012. Int J Cardiol. 2015;184:637–644. doi: 10.1016/j.ijcard.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 28.Wang J, Zhang L, Wang F, Liu L, Wang H. China National Survey of chronic kidney disease working group. Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens. 2014;27(11):1355–1361. doi: 10.1093/ajh/hpu053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang J, Wang ZQ, Zhao YF, Li YC, Yin P, Liu SW, You JL, Zhou MG. Burden of disease attributed to high total cholesterol in 2013 in China. Zhonghua Yu Fang Yi Xue Za Zhi. 2016; 10.3760/cma.j.issn.0253-9624.2016.09.004. [DOI] [PubMed]
- 30.National Center for Disease Control and Prevention of China. Report on adults tobacco survey in 14 Chinese cities, 2013–2014. http://www.tcrc.org.cn/html/zy/cbw/jc/3192.html. Accessed 20 Aug 2015.
- 31.Ebenstein A, Fan M, Greenstone M, He G, Yin P, Zhou M. Growth, pollution, and life expectancy: China from 1991-2012. American Economic Review: Papers & Proceedings. 2015;105(5):226–231. doi: 10.1257/aer.p20151094. [DOI] [Google Scholar]
- 32.National Bureau of Statistics of the People’s Republic of China, National data. 2017. http://www.stats.gov.cn. Accessed 9 Nov 2017.
- 33.Zhang R, Wang Z, Fei Y, Zhou B, Zheng S, Wang L, Huang L, Jiang S, Liu Z, Jiang J, et al. The difference in nutrient intakes between Chinese and Mediterranean. Japanese and American Diets Nutrients. 2015;7(6):4661–4688. doi: 10.3390/nu7064661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Center for Cardiovascular Diseases of China . Report on cardiovascular diseases in China. 2016. [Google Scholar]
- 35.Xie XX, Zhou WM, Lin F, Li XQ, Zhong WL, Lin SG, Li WY, Chen TH, Ye Y, Hu XJ, et al. Ischemic heart disease deaths, disability-adjusted life years and risk factors in Fujian, China during 1990-2013: data from the global burden of disease study 2013. Int J Cardiol. 2016;214:265–269. doi: 10.1016/j.ijcard.2016.03.236. [DOI] [PubMed] [Google Scholar]
- 36.Turk-Adawi K, Sarrafzadegan N, Fadhil I, Taubert K, Sadeghi M, Wenger NK, Tan NS, Grace SL. Cardiovascular disease in the eastern Mediterranean region: epidemiology and risk factor burden. Nat Rev Cardiol. 2017; 10.1038/nrcardio.2017.138. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ᅟ. (DOCX 18 kb)
Data Availability Statement
The raw data of IHD burden on the national level for China were obtained from the GBD Results Tool (http://ghdx.healthdata.org/gbd-results-tool). Data for provinces are nonpublic, which need to be applied to the National CDC of China.


