Abstract
Background:
Sugar-sweetened beverages (SSB) are considered a risk factor for obesity.
Objective:
The objective of the current study was to investigate associations between the predictors of beverage and energy intakes and mean adequacy ratios (MARs), and the outcome of body mass index (BMI) z-scores, in a birth cohort using longitudinal models.
Design:
Longitudinal analyses of secondary data.
Participants/setting:
Participants in the Iowa Fluoride (IFS) and Iowa Bone Development Studies with two beverage intake questionnaires completed between ages 2–4.7 or 5–8.5 years or one questionnaire between ages 9–10.5, 11–12.5, 13–14.5, or 15–17 years (n=720); two food and beverage diaries completed between ages 2–4.7 or 5–8.5 years or completion of the Block’s Kids’ Food Frequency Questionnaires at age 11, 13, 15 or 17 years (n=623); and anthropometric measures at the corresponding age 5, 9, 11, 13, 15 or 17 year exam(s).
Predictors:
Mean daily 100% juice, milk, SSB, water/SFB, and energy intakes and MARs averaged over ages 2–4.7, 5–8.5, 9–10.5, 11–12.5, 13–14.5, or 15–17 years.
Outcome:
BMI z-score.
Statistical Analyses:
Linear mixed models were fit for each beverage, energy and MAR variable, with the beverage, energy or MAR variable as the predictor and BMI z-score as the outcome. Beverage models were adjusted for energy and MAR and baseline socioeconomic status (SES).
Results:
SSB intake adjusted for energy intake, MAR and baseline SES was associated with BMI z-score; each additional 8 oz SSB consumed/day throughout childhood and adolescence increased the BMI z-score an average 0.050 units (Confidence Interval {CI}: 0.022, 0.079; P=0.001). Adjusted water/SFB intake (0.026 units; CI: 0.006, 0.046; P=0.013) was modestly associated with BMI z-score, while 100% juice (−0.001 units; CI: −0.059, 0.057; P=0.97) and milk (0.022 units; CI: −0.007, 0.052; P=0.13) intakes were not associated with BMI z-scores.
Conclusions:
Higher SSB intakes were associated with increased BMI z-scores throughout childhood and adolescence in IFS participants. Public health initiatives targeting SSB consumption during childhood and adolescence remain relevant.
Keywords: Beverage, sugar-sweetened beverages, energy, BMI z-score
Introduction:
Childhood obesity is a risk factor for adult obesity, type 2 diabetes mellitus and cardiovascular disease. The prevalence of obesity has remained relatively stable since 1999–2000 among children aged 2–11 years, and has increased among children aged 12–19 years.1,2,3 In 2015–16, 18.5% of United States (U.S.) children and adolescents were considered obese.2 The prevalence of both obesity (body mass index [BMI] ≥ 30) and severe obesity (BMI ≥ 40) among U.S. adults has gradually increased since 2007–8; 39.6% and 7.7% of adults were considered obese and severely obese, respectively, in 2015–16.2 According to Buscot et al.,4 obese children who remained obese as adults had mean BMIs 2.0–3.4 units higher at age 6 years than their peers who were not obese in adulthood, while non-obese children who became obese adults had slightly higher mean BMIs at age 6 than their peers who did not become obese as adults. Obesity is difficult to treat, and an improved understanding of risk factors for obesity development during childhood could be important as a foundation for improved preventive strategies.
Obesity is recognized as a disease of energy imbalance, with energy and macronutrient intakes, individual food and beverage intakes, and dietary behaviors being investigated as risk factors. Recent attention has focused on added sugars, particularly in liquid form. Sugar-sweetened beverages (SSBs) are defined as beverages containing added sugars, and examples include carbonated soda-pops, fruit drinks, energy drinks, sports drinks, sweetened waters and coffees and teas with added sugars.5 The literature linking SSBs to obesity is mostly observational in nature, and several systematic reviews have been inconclusive.6–8 Luger et al.8 conducted a systematic review of recent prospective cohort studies and four randomized controlled trials. They concluded that the majority of recent studies support a positive association between SSBs and weight, BMI or BMI z-score in both children and adults, while older studies were inconclusive.
Marshall et al.9 recently investigated adolescent (i.e., age 13 to 17 year) beverage patterns and age 17 year anthropometric measures in a cohort followed longitudinally from birth (n=369). Beverage patterns were identified through cluster analysis with clusters named for the dominant beverage intake within the cluster. Mean age 17 year BMIs were higher for members of the milk cluster (by 2.4 units), SSB cluster (3.2 units), water/sugar-free beverage (SFB) cluster (3.5 units) and neutral (no dominant beverage) cluster (2.2 units) compared to members of the 100% juice cluster (all Ps<0.05).9 The objective of the current study was to investigate longitudinal associations between beverage and energy intakes and mean adequacy ratios (MARs) and BMI z-scores in this cohort.
Materials and Methods:
Data Collection:
Secondary analyses were conducted on data collected as part of the Iowa Fluoride Study (IFS) and Iowa Bone Development Study (IBDS, a substudy of the IFS), which investigated relationships among fluoride exposures, dietary intakes, oral health and bone health.9–15 IFS questionnaires queried family demographic information at birth (1992–1995) and in 2007. Participant beverage intakes were collected at 3–6 month intervals following birth, while energy intakes were collected at 3–6 month intervals from birth through age 8.5 years, and at most every other year after age 9. Weight and height were measured at clinic visits when participants were approximately ages 5, 9, 11, 13, 15, and 17 years.
All components of the IFS and IBDS were approved by the University of Iowa’s Institutional Review Board. Written informed consent was obtained from mothers at recruitment and from parents at clinic visits, while written assent was obtained from children beginning at age 13 years.
Socioeconomic status (SES):
Household income and mother’s educational attainment at baseline were used to identify three categories of SES. Low SES was defined by a household income <$30,000 and a maternal educational level below a 4-year college degree. Moderate SES was defined as having a household income of $30,000-$49,999 and a participant’s mother without a graduate/professional degree or household income <$30,000 and a participant’s mother with at least a 4-year college degree. High SES was defined as a household income ≥$50,000 regardless of maternal educational level, or household income ≥$30,000 and a participant’s mother with a graduate or professional degree.
Beverage intakes:
Beverage frequency questionnaires, validated using 3 day food and beverage diaries, queried frequency and quantity of beverage consumption during the previous week.12,13 Prior to age 9, beverage questionnaires queried flavored and unflavored milk, ready-to-drink 100% juice and juice drinks, soda pop, reconstituted powdered beverages and water. After age 9, 100% juice and juice drinks were queried separately, and sports drinks, coffee and alcoholic beverages were also queried. Beverages were collapsed into four categories: 100% juice, milk, sugar-sweetened beverages (SSBs), and water and other sugar-free beverages (water/SFBs). SFBs were combined with water given their similar energy concentrations and the observation that subjects consumed very small quantities of SFBs during the ages studied. Mean daily beverage intakes were calculated for each subject from all available questionnaires over the time periods preceding clinic exams (i.e., 2–4.7, 5–8.5, 9–10.5, 11–12.5, 13–14.5 and 15–17 years). Within-subject averages were used as time-varying covariates in linear mixed models.
Energy intakes and MARs:
Energy intakes and MARs were obtained from 3 day food and beverage diaries completed at 3–6 month intervals prior to age 8.5 years.15 Entries from food and beverage diaries were coded and verified by registered dietitians to create a Food and Beverage Table. A Nutrient Table was created from nutrient data obtained from the United States Department of Agriculture (USDA),16 the Minnesota Nutrient Database17 and manufacturers’ data. A relational database18 was used to link the Food and Beverage Table with the Nutrient Table for calculation of energy and nutrient intakes. MARs, a measure of overall diet quality, were calculated from nutrient adequacy ratios (NARs) for protein, 9 vitamins (vitamin A, vitamin C, thiamin, riboflavin, niacin, folate, vitamin B-6, vitamin D, and vitamin E), and 5 minerals (calcium, iron, magnesium, phosphorous and zinc).14 NARs were truncated at one when calculating the MAR to prevent an excess intake of one nutrient from compensating for low intakes of other nutrients. Mean daily energy intakes and MARs were averaged from all available 3-day diaries for ages 2–4.7 and 5–8.5 years. Energy intakes and MARs were obtained from Block’s Kids’ Food Frequency Questionnaires19 completed for the previous week at 11, 13, 15 and 17 years.
Anthropometric measures:
Weight and height were measured at clinic visits with participants wearing lightweight clothing and without shoes. Weight was measured using a standard physician’s scale; height was measured using a stadiometer. Body mass indices (kg/m2) were calculated from weight and height measures. BMI z-scores were calculated from the Centers for Disease Control and Prevention (CDC) standards using a SAS macro provided by the CDC.20 BMI z-scores were used instead of BMI in order to better accommodate comparisons over time, and properly account for extreme values.21
Participants:
Mothers were recruited at the time of their infants’ births (1992–1995) for participation in the ongoing IFS. Inclusion in the beverage, energy or MAR analysis required explanatory variables and an outcome measurement for at least one time point. Inclusion in the beverage intake analyses (n=720) required completion of at least two questionnaires between ages 2–4.7 or 5–8.5, or completion of at least one questionnaire between ages 9–10.5, 11–12.5, 13–14.5, or 15–17 years, and anthropometric measures at the corresponding age 5, 9, 11, 13, 15 or 17 year exam(s), respectively. For the energy intake or MAR analyses (n=623), inclusion required completion of at least two food and beverage diaries between ages 2–4.7 or 5–8.5 years or completion of the Block’s Kids’ Food Frequency Questionnaires at age 11, 13, 15 or 17 years, and anthropometric measures at the corresponding age 5, 9, 11, 13, 15, or 17 year exam(s), respectively.
Statistical Analyses:
At each age for which anthropometric data were collected, a two sample t-test was used to identify differences in mean BMI z-scores between males and females. Longitudinal analyses were conducted to identify associations between the predictors of beverage intakes, energy intakes or MARs, and the outcome of mean BMI z-scores. After visually confirming via scatterplots that a linear relationship between each beverage, energy or MAR variables and BMI z-score was appropriate, a linear mixed model was fit for each beverage, energy and MAR variable under study, with the beverage, energy and MAR variable as the predictor of interest and BMI z-score as the outcome. Linear mixed models allow for participants to be included in the model if they have full data available (beverage intake, energy intake or MAR and BMI z-score) for at least one time point. The models were formulated using a participant-specific random intercept and slope, and fit by applying maximum likelihood estimation using PROC MIXED in SAS.22
Associations between beverage intakes and BMI z-scores throughout childhood and adolescence were investigated. All participants and all available time points were included in a single model examining the effect of beverage intake on mean BMI z-score, to optimize statistical power given the available data.
In the initial set of models, variables representing intakes of particular beverage types, energy or MAR and age at BMI measurement were used as predictors of BMI z-score in a linear mixed model to determine if intake of each beverage type was associated with a difference in mean BMI z-score over time. For each beverage type, four additional models were fit. The first contained an indicator for sex and an interaction between beverage intake and sex in order to determine if the associations between beverage intakes and BMI z-scores differed between males and females. The second did not contain an indicator for sex or interaction terms, but adjusted for energy intake and baseline SES. The third adjusted for energy intake, MAR, and baseline SES. The fourth adjusted for energy intake, MAR, and baseline SES, and included an interaction term between beverage intake and an indicator for whether the outcome (and corresponding dietary intake) was at or before age 9, or after age 9. The interaction was considered in order to determine if the effect of 8oz of beverage intake on mean BMI z-score differed between these two age ranges due to differences in beverage intake questionnaires over time and/or physiological differences between children (prior to age 9) and pre-teens/adolescents (after age 9).
Finally, a single composite model, which adjusted for energy intake, MAR and baseline SES, and included beverage intakes from all four beverage categories, was fit to assess the effect of beverage intake on mean BMI z-score after adjusting for intakes of all other beverages.
The effect of beverage intake on mean BMI z-score for a particular model was summarized, while the fixed effect estimates for the intercept, age at BMI measurement, energy intake, MAR, baseline SES, and the interaction term were omitted for clarity of interpretation.
Results:
Participants were about half female (51%) and mostly non-Hispanic white (94%). Forty-five percent of mothers had a 4-year college degree at baseline, while 50% of mothers had a college degree in 2007. Nineteen percent and 67% of households had an annual income > $60,000 at baseline and in 2007, respectively. At baseline, 25% of participants belonged to the low, 38% of participants belonged to the middle, and 38% of participants belonged to the high SES category.
Median (25th, 75th percentile) daily beverage intakes are presented in Table 1. Milk intakes remained relatively stable across ages. Water/SFB and SSB intakes gradually increased with age, while 100% juice intakes declined between 2–4.7 years and 9–10.5 years. Median (25th, 75th percentile) daily energy intakes and MARs are presented in Table 2. Variability in energy intakes increased with age. The median energy intake peaked around 13–14.5 years for males and 9 – 10.5 years for females. The median MARs were relatively stable through age 9–10.5 and declined slightly thereafter.
Table 1:
Median (25th, 75th percentile) daily beverage intakes of Iowa Fluoride Study participants at 2–4.7, 5–8.5, 9–10.5, 11–12.5, 13–14.5 and 15–17 years of age.
| Beverage | Sex | Age (years) | |||||
|---|---|---|---|---|---|---|---|
| 2–4.7 | 5–8.5 | 9–10.5 | 11–12.5 | 13–14.5 | 15–17 | ||
| Males (n) | 317 | 285 | 217 | 250 | 197 | 207 | |
| Females (n) | 333 | 288 | 230 | 270 | 205 | 225 | |
| 100% Juicea (oz) | Males | 7.2 (4.4, 10.7) | 5.6 (3.4, 7.7) | 1.4 (0.0, 3.9) | 1.2 (0.0, 3.4) | 0.9 (0.0, 3.4) | 0.9 (0.0, 3.9) |
| Females | 6.0 (3.7, 9.6) | 4.2 (2.5, 6.6) | 1.3 (0.0, 3.5) | 1.5 (0.0, 3.5) | 1.1 (0.0, 3.1) | 1.0 (0.0, 3.4) | |
| Milk (oz) | Males | 10.9 (7.3, 15.7) | 12.7 (8.9, 17.2) | 11.6 (7.9, 16.1) | 13.3 (8.0, 17.7) | 12.0 (7.2, 19.3) | 11.7 (6.9, 20.9) |
| Females | 10.9 (7.6, 14.1) | 11.9 (8.5, 15.6) | 10.3 (6.4, 15.5) | 11.0 (5.7, 15.7) | 10.2 (5.6, 15.1) | 8.6 (4.6, 15.6) | |
| Sugar-Sweetened Beverages (oz) | Males | 2.7 (1.1, 5.1) | 4.4 (2.7, 7.5) | 9.0 (5.0, 14.0) | 9.7 (6.4, 16.8) | 11.9 (7.0, 18.1) | 12.6 (7.6, 20.9) |
| Females | 2.6 (1.2, 5.1) | 3.2 (1.6, 5.8) | 6.4 (4.0, 10.0) | 7.4 (4.3, 12.0) | 7.3 (4.4, 12.5) | 7.9 (4.0, 14.1) | |
| Water/Other Sugar-Free Beverages (oz) | Males | 4.7 (2.7, 7.6) | 8.9 (5.0, 13.6) | 10.4 (6.9, 18.0) | 13.1 (8.6, 20.6) | 15.6 (10.1, 23.6) | 17.7 (10.7, 30.6) |
| Females | 4.7 (2.8, 7.6) | 8.1 (5.1, 11.7) | 9.1 (6.3, 15.3) | 12.7 (8.0, 19.8) | 14.7 (9.0, 24.2) | 17.3 (10.9, 27.4) | |
Juice drinks are included with 100% juice prior through age 8.5 years.
Table 2:
Median (25th, 75th percentile) energy intakes and mean adequacy ratios (MAR) of Iowa Fluoride Study participants 2–4.7, 5–8.5, 9–10.5, 11–12.5, 13–14.5 and 15–17 years of age.a
| Beverage | Sex | Age (years) | |||||
|---|---|---|---|---|---|---|---|
| 2–4.7 | 5–8.5 | 9–10.5 | 11–12.5 | 13–14.5 | 15–17 | ||
| Males (n) | 231 | 132 | 226 | 230 | 197 | 173 | |
| Females (n) | 230 | 138 | 241 | 239 | 206 | 197 | |
| Energy (kcalb/day) | Males | 1421 (1298, 1631) | 1731 (1565, 1963) | 1724 (1485, 2111) | 1789 (1449, 2229) | 1872 (1555, 2283) | 1772 (1368, 2290) |
| Females | 1299 (1148, 1472) | 1586 (1423, 1754) | 1609 (1301, 1812) | 1517 (1184, 1864) | 1362 (1085, 1724) | 1268 (987, 1594) | |
| MAR | Males | 0.95 (0.93, 0.96) | 0.95 (0.93, 0.97) | 0.94 (0.89, 0.97) | 0.93 (0.87, 0.97) | 0.89 (0.81, 0.94) | 0.87 (0.75, 0.95) |
| Females | 0.94 (0.92, 0.96) | 0.94 (0.92, 0.96) | 0.92 (0.85, 0.95) | 0.89 (0.82, 0.95) | 0.82 (0.71, 0.90) | 0.78 (0.65, 0.88) | |
Modified from Reference 12.
kilocalorie
Mean (standard deviation) anthropometric measures are presented in Table 3. Weights, heights and BMIs generally increased with age. Mean BMI z-scores were slightly higher for males than females at all time points, and the differences were statistically significant at ages 9 and 11 years.
Table 3:
Mean (± SD) anthropometric measures of Iowa Fluoride Study participantsa at approximate ages 5, 9, 11, 13, 15 and 17 years.
| Anthropometric measure | Sex | Age (years) | |||||
|---|---|---|---|---|---|---|---|
| 5 | 9 | 11 | 13 | 15 | 17 | ||
| Males (n) | 317 | 285 | 231 | 267 | 201 | 214 | |
| Females (n) | 334 | 288 | 248 | 277 | 213 | 240 | |
| Weight (kg) | Males | 20.2 ± 3.2 | 35.5 ± 9.6 | 45.4 ± 13.1 | 60.2 ± 17.2 | 70.8 ± 16.2 | 80.5 ± 18.0 |
| Females | 19.7 ± 3.6 | 33.6 ± 8.6 | 44.2 ± 12.2 | 57.0 ± 14.6 | 61.9 ± 14.6 | 66.8 ± 16.5 | |
| Height (cm) | Males | 111.8 ± 5.6 | 137.9 ± 7.3 | 149.1 ± 7.6 | 164.8 ± 9.2 | 175.3 ± 7.8 | 179.3 ± 7.4 |
| Females | 110.9 ± 5.4 | 135.7 ± 6.9 | 148.9 ± 7.4 | 161.2 ± 6.4 | 164.5 ± 6.6 | 165.7 ± 6.7 | |
| BMIb | Males | 16.1 ± 1.8 | 18.5 ± 3.9 | 20.2 ± 4.6 | 22.0 ± 5.1 | 23.0 ± 4.7 | 25.0 ± 5.0 |
| Females | 15.9 ± 1.9 | 18.1 ± 3.6 | 19.7 ± 4.3 | 21.8 ± 5.1 | 22.8 ± 4.9 | 24.3 ± 5.8 | |
| BMI z-scoreb,c | Males | 0.34 ± 1.09 | 0.53 ± 1.06 | 0.59 ± 1.13 | 0.59 ± 1.12 | 0.57 ± 1.04 | 0.62 ± 1.12 |
| Females | 0.28 ± 1.07 | 0.35 ± 1.11 | 0.36 ± 1.13 | 0.46 ± 1.07 | 0.44 ± 0.98 | 0.45 ± 1.01 | |
n=720; 355 male and 365 female.
Body mass index
Mean BMI z-scores differed between males and females at ages 9 and 11 years (P=0.049 and 0.026, respectively, 2-sample t-tests).
For all beverage types, the Bayesian Information Criterion (BIC) was more than three units lower in the unadjusted models than in models with an indicator for sex and an interaction between beverage intake and sex. Models with smaller BIC values are preferred, with two or more units signifying a substantial improvement in complexity-penalized model fit. The P-values for sex and for the interaction between beverage intake and sex were not statistically significant (P>0.05) in any model, and the unadjusted beverage-only models are reported herein (Table 4). SSB intake had the largest effect size of the four beverage types and was significantly associated with BMI z-score in the unadjusted model. Neither 100% juice nor milk intakes were associated with BMI z-scores in unadjusted models, while water/SFB intakes were modestly associated with BMI z-scores. Energy was significantly, but marginally, associated with BMI z-score in an unadjusted model; the estimated effect size for 100 kcal was 0.007 (CI: 0.003–0.012; P<0.001). Similarly, in an unadjusted model, the estimated effect size for 0.1 MAR was 0.027 (CI: 0.005–0.049; P 0.017).
Table 4:
Summary of effects of beverage intakes on mean body mass index (BMI) z-scores adjusted for baseline socioeconomic status (SES), energy intakes and mean adequacy ratios (MARs) during childhood and adolescence in Iowa Fluoride Study participants.a
| Beverage Variable | Estimated Effect (95% CI) of Beverage Intake on mean BMI z-scorea,b | P value | Estimated Effect (95% CI) of Beverage Intake on mean BMI z-score adjusted for energy and baseline SESc,d | P-value | Estimated Effect (95% CI) of Beverage Intake on mean BMI z-score adjusted for energy, MAR and baseline SESc,e | P value |
|---|---|---|---|---|---|---|
| 100% Juicef | −0.027 (−0.076, 0.022) | 0.28 | −0.001 (−0.059, 0.057) | 0.97 | −0.001 (−0.059, 0.057) | 0.97 |
| Milk | 0.014 (−0.013, 0.041) | 0.31 | 0.022 (−0.007, 0.052) | 0.13 | 0.022 (−0.007, 0.052) | 0.13 |
| Sugar-Sweetened Beverages | 0.056 (0.030, 0.083) | <0.001 | 0.050 (0.021, 0.078) | 0.001 | 0.050 (0.022, 0.079) | 0.001 |
| Water/Other Sugar-Free Beverages | 0.023 (0.003, 0.042) | 0.022 | 0.026 (0.006, 0.046) | 0.013 | 0.026 (0.006, 0.046) | 0.013 |
n=719; 355 male, 364 female.
Estimated effect (95% Confidence Interval [CI]) of 8 oz of additional daily beverage intake on mean BMI z-score from unadjusted linear mixed models.
n=623; 309 male, 314 female
Estimated effect (95% CI) of 8 oz of additional daily beverage intake on mean BMI z-score from linear mixed models adjusted for energy intake and baseline SES.
Estimated effect (95% CI) of 8 oz of additional daily beverage intake on mean BMI z-score from linear mixed models adjusted for, energy intake, mean adequacy ratio, and baseline SES.
Juice drinks are included with 100% juice prior through age 8.5 years.
After adjustment for energy intake and baseline SES (Table 4), SSB intake still had the largest effect size among beverage types and remained statistically significant. The adjusted model indicates that each additional 8 oz of SSB/day throughout childhood and adolescence was associated with an expected increase in BMI z-score of 0.050 units (CI: 0.021–0.078). Water/SFB intakes were significantly, but modestly, associated with BMI z-scores in adjusted models. The adjusted model indicates that each additional 8 oz of water/SFB/day throughout childhood and adolescence was associated with an expected increase in BMI z-score of 0.026 units (CI: 0.006–0.046). Neither 100% juice nor milk intakes were significantly associated with BMI z-scores in adjusted models. Model results were very similar following adjustment for energy, MAR and baseline SES (Table 4).
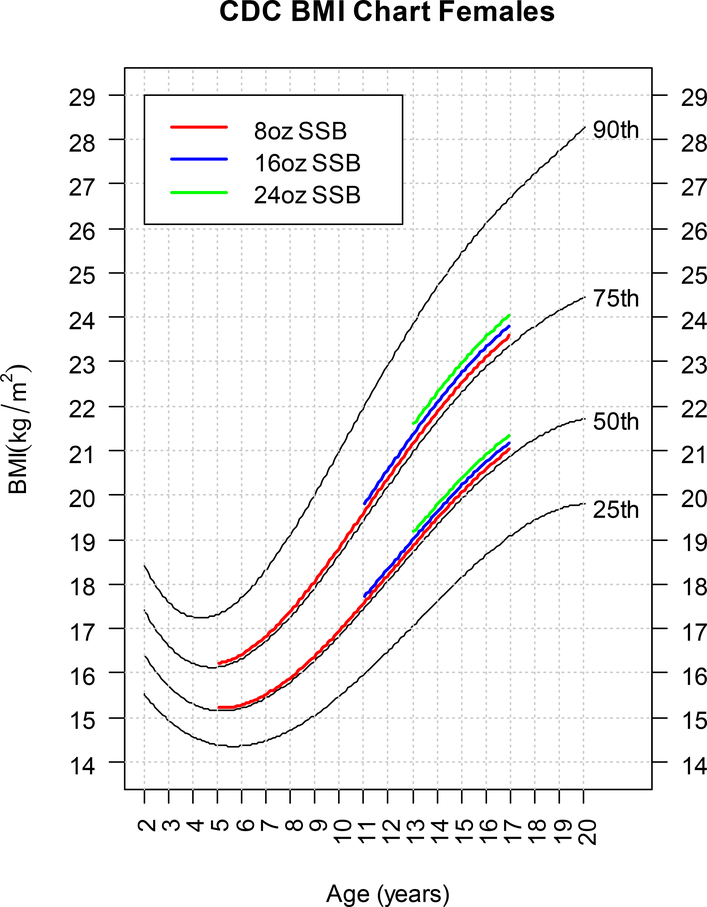
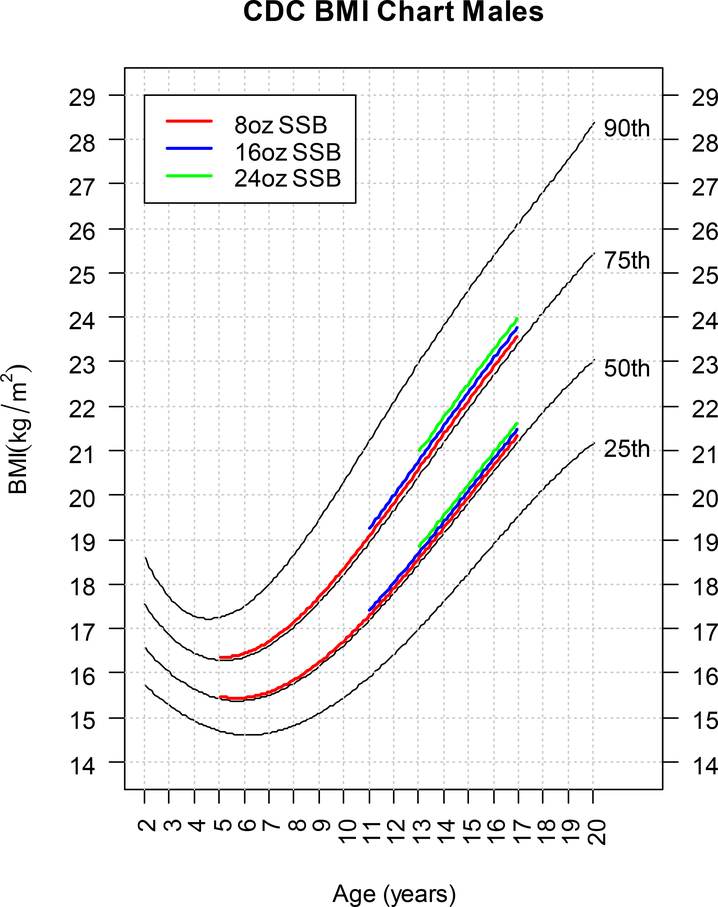
Based on the model adjusted for energy, MAR, and baseline SES, the expected increases in BMI percentile for 8, 16, and 24 oz of SSB intake compared to a child with 0 oz SSB intake at the 50th or 75th BMI percentile are presented graphically in Figures 1 and 2 for females and males, respectively.
Figure 1 –
The expected increase in BMI for 8, 16, and 24 oz of SSB intake relative to 0 oz SSB intake for a female child at the 50th or 75th BMI percentile participating in the Iowa Fluoride Study.
Figure 2 –
The expected increase in BMI for 8, 16, and 24 oz of SSB intake relative to 0 oz SSB intake for a male child at the 50th or 75th BMI percentile participating in the Iowa Fluoride Study.
In Table 5, the fixed effect estimates are presented for the models which adjusted for energy, MAR, and baseline SES, and included the interaction between beverage intake and an indicator for whether the observation was at or before age 9, or after age 9. In the interaction models, the effect of 8oz of beverage intake on mean BMI z-scores at or before age 9 was larger than the effect of 8oz of beverage intake on mean BMI z-score after age 9 for all beverage types except 100% juice. This could be due to the fact that children drink less than adolescents and therefore, 8oz of beverage intake could have a more pronounced effect on the age- and sex-adjusted BMI z-score at earlier ages than later ages. The conclusions from the models with and without the interaction term are arguably similar. 100% Juice and milk are not significantly associated with mean BMI z-score in either age range, whereas SSBs and water/SFBs are significantly associated with mean BMI z-scores, with the association for SSBs being driven primarily by the effect after age 9 and the association for water/SFBs being driven primarily by the effect at or before age 9. While the interaction models help to account for the effect of different questionnaire items before and after age 9 and demonstrate the difference in beverage volume consumed before and after age 9, it is important to note that the interaction term is significant only for the water/SFB model, and the BIC values are at least two units lower in the no interaction models (Table 4) for all beverage types. Therefore, the models without the interaction provide similar conclusions, and better penalized model fit.
Table 5:
Summary of effects of adjusted beverage intakes on mean body mass index (BMI) z-scores before and after age 9 years during childhood and adolescence in Iowa Fluoride Study participants.a,b
| Beverage Variable | Estimated Effect of Beverage Intake on mean BMI z-score prior to age 9 (approx. ages 5 and 9) | P-value | Estimated Effect of Beverage Intake on mean BMI z-score after age 9 (approx. ages 11, 13, 15, and 17) | P value |
|---|---|---|---|---|
| 100% Juicec | −0.026 (−0.107, 0.055) | 0.52 | 0.044 (−0.038, 0.125) | 0.29 |
| Milk | 0.046 (−0.017, 0.109) | 0.15 | 0.020 (−0.011, 0.051) | 0.21 |
| Sugar-Sweetened Beverages | 0.076 (−0.023, 0.175) | 0.13 | 0.048 (0.019, 0.077) | 0.001 |
| Water/Other Sugar-Free Beverages | 0.103 (0.044, 0.162) | <0.001 | 0.023 (0.003, 0.044) | 0.0278 |
n=623; 309 male, 314 female
Estimated effect (95% Confidence Interval [CI]) of 8 oz of additional daily beverage intake on mean BMI z-score from linear mixed models adjusted for energy intake, mean adequacy ratio, and baseline socioeconomic status.
Juice drinks are included with 100% juice prior through age 8.5 years.
Finally, the effect of all beverage intakes were considered in one composite model, with no interaction terms. The fixed effect estimates for each beverage type based on this model are very similar to those presented in Table 4. The effects of 8oz of 100% juice on mean BMI z-score is 0.007 (CI: −0.051, 0.065), the effect of milk is 0.018 (CI: −0.012, 0.048), the effect of SSBs is 0.051 (CI: 0.022, 0.080), and the effect of water/SFBs is 0.023 (CI: 0.002, 0.044). This indicates that changes in the fixed effect of each beverage intake are minimal after adjustment for other beverage intakes.
Discussion:
In the current analyses, the longitudinal associations among beverage intakes, energy intakes, MARs and BMI z-scores were investigated. SSB intakes, but not 100% juice or milk intakes, were associated with a clinically meaningful increase in mean BMI z-scores throughout childhood and adolescence; this association remained clinically meaningful following adjustment for energy intake, MAR and SES. While water/SFB and energy intakes were also associated with BMI z-scores, the effect sizes were relatively small and/or of modest statistical significance, limiting their clinical interpretation. The findings suggest that associations between SSBs and BMI z-scores are not due to the SSBs’ energy content; additional research is necessary to understand the mechanisms.
The results reported herein are consistent with most previous publications investigating associations between SSBs and obesity.23–26 A meta-analysis of prospective studies conducted in children published through March 2013 reported that a child’s mean BMI increased 0.06 (CI 0.02–0.10) units for each additional 12 oz SSBs/day over a 1 year period of time.26 A more recent systematic review of studies published between 2013 and 2015 reported that 15 of 16 prospective studies conducted in children and adolescents found a positive association between SSBs and weight, BMI or % body fat.8 More specifically, Millar et al.27 reported that the mean BMI z-score increased by 0.015 (CI: 0.004, 0.025) units for each additional SSB/day consumed by Australian children aged 4–10 years. Similarly, Zheng et al.28 reported that the mean BMI z-score increased by 0.10 units between 8 and 11.5 years for each additional 100 g/day of energy adjusted SSB consumed by Australian children at age 8 years. However, Zheng et al.28 did not find an association between 1 or more SSB servings/day at age 9 years and BMI change between ages 9 and 21 years in Danish participants of the European Youth Heart study. In the same subjects, 1 or more SSB servings/day at age 15 was associated with BMI change between age 15 and 21 years; this association did not remain after energy adjustment.29 Interestingly, the increase in expected BMI z-score associated with SSB intake in IFS participants was larger than the increase observed with energy intake. Striegel-Moore et al.30 also observed an expected BMI increase associated with 100 g SSB that was greater than that observed with total energy intake.
A recent meta-analyses reported that the mean BMI z-scores increased a mean of 0.087 (CI: 0.008, 0.167) units for each 6–8 oz/day of fruit juice adjusted for energy intake in children aged 1–6 years, but was not associated with juice intake in children aged 7–18 years.31 Hasnain et al.32 reported that 3–9 year old non-Hispanic, white U.S. children in the lower tertile of fruit/vegetable juice intakes tended to have higher skinfolds, waist circumferences and BMIs, but not percent body fats, at 15–17 years than their peers in the highest tertile. While an association between juice intakes and BMI z-scores was not found in the current longitudinal analyses, the impact of early juice intakes on subsequent SSB intakes or anthropometric measures was not investigated. Somneville et al.33 reported that higher juice intakes at 1 year were associated with both higher SSB intakes and BMI z-scores at approximately 3.1 and 7.7 years, suggesting that very early juice intakes might be more important than overall childhood juice intakes for obesity risk.
Previous investigations of associations between milk or dairy intakes and obesity measures have produced mixed results.34 Vogel et al.35 reported that three additional cups of milk or dairy equivalent/day did not influence BMI or percent body fat in healthy or overweight children aged 8–16 years during an 18 month intervention. Marabujo et al.36 did not observe associations between milk or other dairy intakes at age 13 and BMI at age 21 after energy adjustment. In contrast, Beck et al.37 reported that severely obese Latino children tended to consume less total milk than their peers at age 3 years. Similarly, Hasnain et al.32 reported that children in the lower tertile of milk intakes at 3–9 years had significantly higher % body fats and skinfold thicknesses, but not BMIs, at 15–17 years than their peers. De Boer et al.38 reported that having 3 or more servings of milk/day was positively associated with BMI at age 4, but not 5 years.
Investigations of associations between water intakes and obesity measures in adults suggest that total water intake was significantly higher in heavier individuals.39,40 Kant et al. reported that total water intake, but not plain water intake, was positively associated with BMI in U.S. adults.39 Daniels and Popkin41 considered the associations between plain water or beverage alternatives and energy intake or weight status. They reported that replacement of milk, juice or SSBs with water resulted in lower energy intakes and greater weight loss. Most recently, Walton et al.42 reported that the Irish adults in the highest tertile of drinking water consumption had lower mean BMIs when compared to the lowest tertile of consumers, after adjustment for SES, diet quality and energy intake (β coefficient = −0.65 [CI: −1.30, −0.01]). Unfortunately, direct comparisons between the results reported herein and those of other studies are limited by the fact that water was combined with other SFB in the current study. However, the modest association between water/SFB intakes and BMI z-scores in the current participants is consistent with previous reports associating total water with BMI.
Subjects’ median beverage intakes are generally similar to intakes reported by researchers investigating associations between beverage intakes and obesity measures and in national surveys.43–45 However, subjects did report lower median daily SSB intakes (~8 oz) and higher milk intakes (~4 oz) at age 17 years than U.S. children followed by Hasnain et al.32 SSBs provide energy from added sugars; U.S. Dietary Guidelines recommend that added sugar intakes be limited to less than 10% total energy.46 Median juice intakes reported by IFS subjects were higher than current American Academy of Pediatrics recommendations (i.e, 4–6 oz) for ages 2–4.7, but within guidelines for older ages.47 Median milk intakes were less than ChooseMyPlate recommendations at all ages.48
Both strengths and weaknesses must be considered when interpreting the current results. The IFS dataset provides a unique opportunity to longitudinally investigate beverage intakes and BMI z-scores across childhood and adolescence, while adjusting for energy intake and MAR. Earlier prospective studies typically covered either early childhood or adolescent time periods with limited repeated dietary and/or obesity measures.8,26 Additional strengths include a loyal cohort followed for over 17 years. Validated instruments were used to query beverage and dietary intakes at multiple time points throughout life. The longitudinal data allow us to examine beverage and energy intakes, MARs and BMI z-scores over time without concerns regarding a cohort effect. Weaknesses include caregiver-reported (early ages) and self-reported (later ages) beverage and dietary intakes that might not reflect actual intakes. Beverage questionnaires prior to age 9 years combined 100% juice and juice drinks; thus, juice drinks are included with 100% juice for ages 2–4.7 and 5–8.5 years. Inclusion of juice drinks with 100% juice prior to age 9 years could have limited our ability to identify negative associations between 100% juice intakes and BMI z-scores and/or positive associations between SSB intakes and BMI z-scores at early ages. The relatively small and self-selected sample is mostly white, reasonably well-educated and reasonably wealthy, and is not representative of other U.S or international populations.
Conclusion:
The current findings extend earlier research associating higher intakes of SSBs with obesity by investigating the relationship across childhood and adolescence, as well as adjusting for reported energy intakes and MARs. Herein, positive associations between SSBs and BMI z-scores throughout childhood and adolescence were identified. On average, BMI z-scores increased 0.050 units with each additional 8 oz SSB consumed per day. Public health initiatives targeting SSB consumption throughout childhood and adolescence remain relevant.
Research Snapshot:
Research Question:
Is there a longitudinal association between beverage intakes and BMI zscores in a birth cohort followed for 17 years?
Key Findings:
Sugar-sweetened beverage (SSB) intakes collected by beverage frequency questionnaires at ages 2 through 17 years were longitudinally associated with BMI z-scores calculated from weight and height measured at ages 5, 9, 11, 13, 15 and 17 years in a birth cohort (n=720). After adjustment for energy intake, mean adequacy ratio and baseline socioeconomic status, each additional 8 oz SSB consumed/day throughout childhood and adolescence increased BMI z-score an average of 0.050 units (P=0.001).
Acknowledgements:
Portions of the results of this study were presented at Nutrition 2018, the American Society for Nutrition’s annual meeting, in Boston, MA on June 9, 2018.
Footnotes
Conflict of Interest: The authors have no conflicts of interest relevant to this article to disclose.
Disclosures:
• National Institutes of Health (R03-DE023784, R01-DE12101, R01-DE09551, UL1-RR024979, UL1-TR000442, UL1-TR001013, M01-RR00059)
• The Roy J. Carver Charitable Trust
• Delta Dental of Iowa Foundation
Clinical Trial Registry number: 199112665.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Teresa A. Marshall, Department of Preventive & CommunityDentistry, College of Dentistry, The University of Iowa, Iowa City, IA USA; Teresa-marshall@uiowa.edu. 319-335-7190..
Alexandra M. Curtis, Department of Biostatistics, College of Public Health, The University of Iowa, Iowa City, IA USA; alexandra-curtis@uiowa.edu; 319-335-7186.
Joseph E. Cavanaugh, Department of Biostatistics, College of Public Health & Department of Statistics and Actuarial Science, College of Liberal Arts and Sciences, The University of Iowa, Iowa City, IA USA; joe-cavanaugh@uiowa.edu; 319-384-1602..
John J. Warren, Department of Preventive & Community Dentistry, College of Dentistry, The University of Iowa, Iowa City, IA USA; johnwarren@uiowa.edu; 319-335-7205..
Steven M. Levy, Department of Preventive & Community Dentistry, College of Dentistry, The University of Iowa, Iowa City, IA USA. Steven-levy@uiowa.edu. 319-335-7185..
References:
- 1.Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruzon-Moran D, Kit BK, Flegal KM. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–14. JAMA. 2016; 315(21):2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016 (Research Letter). JAMA. March 23, 2018; doi: 10.1001/jama.2018.3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skinner AK, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. 2018;141(3):e20173459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buscot MJ, Thomson RJ, Juonala M, Sabin MA, Burgner DP, Lehtimäki T, et al. , BMI trajectories associated with resolution of elevated youth BMI and incident adult obesity. Pediatrics. 2018; 141(1):e20172003. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Get the facts: sugar-sweetened beverages and consumption. Available at: https://www.cdc.gov/nutrition/data-statistics/sugar-sweetened-beverages-intake.html Accessed 7/26/18.
- 6.Scharf RJ, DeBoer MD. Sugar-sweetened beverages and children’s health. Annu Rev Public Health. 2016; 37:273–293. [DOI] [PubMed] [Google Scholar]
- 7.Torre SBD, Keller A, Depeyre JL, Kruseman M. Sugar-sweetened beverages and obesity risk in children and adolescents: a systematic analyses on how methodological quality may influence results. J Acad Nutr Diet. 2016; 116:638–659. [DOI] [PubMed] [Google Scholar]
- 8.Lugar M, Lafontan M, Bes-Rastrollo M, Winzer E, Yumuk V, Farpour-Lambert N. Sugar-sweetened beverages and weight gain in children and adults: a systematic review from 2013 to 2015 and a comparison with previous studies. Obes Facts. 2017; 10:674–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marshall TA, Van Buren JM, Warren JJ, Cavanaugh JE, Levy SM. Beverage consumption patterns at age 13–17 years are associated with weight, height and body mass index at age 17 years. J Acad Nutr Diet. 2017; 117(5):698–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warren JJ, Levy SA, Kanellis MJ. Dental caries in the primary dentition: Assessing prevalence of cavitated and noncavitated lesions. J Public Health Dent. 2002;62(2):109–114. [DOI] [PubMed] [Google Scholar]
- 11.Janz KF, Gilmore JM, Burns TL, Levy SM, Torner JC, Willing MC, Marshall TA. Physical activity augments bone mineral accrual in young children: The IOWA Bone Development study. J Pediatr. 2006; 148(6):793–799. [DOI] [PubMed] [Google Scholar]
- 12.Marshall TA, Eichenberger Gilmore JM, Broffitt B, Levy SM, Stumbo PG. Relative validation of a beverage frequency questionnaire in children ages 6 months through 5 years using 3-day food and beverage diaries. J Am Diet Assoc. 2003; 103(6);714–20. [DOI] [PubMed] [Google Scholar]
- 13.Marshall TA, Eichenberger Gilmore JM, Broffitt B, Stumbo PH, Levy SM. Relative validity of the Iowa Fluoride Study targeted nutrient semi-quantitative questionnaire and the Block Kids’ Food Questionnaire for estimating beverage, calcium and vitamin D intakes by children. J Am Diet Assoc. 2008; 108(3):465–472. [DOI] [PubMed] [Google Scholar]
- 14.Marshall TA, Curtis AM, Cavanaugh JE, Warren JJ, Levy SM. Higher longitudinal milk intakes are associated with increased height in a birth cohort followed for 17 years. J Nutr. 2018; 148(7):1144–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marshall TA, Eichenberger Gilmore JM, Broffitt B, Stumbo PJ, Levy SM. Diet quality in young children is influenced by beverage consumption. J Am Coll Nutr. 2005; 24:65–75. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Department of Agriculture, Agricultural Research Service. 1998. USDA National Nutrient Database for Standard Reference, Release 12. Nutrient Data Laboratory. Available at: www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/nutrient-data-laboratory/docs/sr12-home-page/ Accessed 9/7/18.
- 17.University of Minnesota Nutrition Coordinating Center, Nutrition Data System for Research. Version 4.01. Available at: http://www.ncc.umn.edu/products/ Accessed 9/7/18.
- 18.Microsoft: Downloads Access Relational Database SR 1. Available at: https://www.microsoft.com/en-us/search/result.aspx?q=Access+relational+database+SR+1 Accessed 9–7-18.
- 19.NutritionQuest. Assessment & Analysis Services. Available at: http://nutritionquest.com/assessment/list-of-questionnaires-and-screeners/ Accessed 9/7/18.
- 20.Centers for Disease Control and Prevention. Growth Chart Training: A SAS Program for the 2000 CDC Growth Charts (ages 0-<20 years). U.S. Department of Health and Human Services; Available at: https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessed 4/17/18. [Google Scholar]
- 21.Wang Y and Chen HJ. Uses of percentiles and z-scores in anthropometry In: Preedy VR, ed. Handbook of Anthropometry, Springer; 2012. DOI 10.1007/978-1-4419-1788-1_2. [DOI] [Google Scholar]
- 22.SAS. Analytics Software & Solutions, version 9.4. Available at: https://www.sas.com/en_us/software/sas9.html. Accessed 9/7/18.
- 23.Welsh JA, Wang Y, Figueroa J, Brumme C. Sugar intake by type (added vs. naturally occurring) and physical form (liquid vs. solid) and its varying association with children’s body weight, NHANES 2009–2014. Pediatr Obes. 2018; 13(4); 213–221. [DOI] [PubMed] [Google Scholar]
- 24.Williams RD, Housman JM, Odum M, Rivera AE. Energy drink use linked to high-sugar beverage intake and BMI among teens. Am J Health Behav. 2017; 41(3):259–265. [DOI] [PubMed] [Google Scholar]
- 25.Laverty AA, Magee L, Monteiro CA, Saxena S, Millett C. Sugar and artificially sweetened beverage consumption and adiposity changes: National longitudinal study. Int J Behav Nutr Phys Act. 2015; 12:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analyses. Am J Clin Nutr. 2013; 98: 1084–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Millar L, Rowland B, Nichols M, Swinburn B, Bennett C, Skouteris H, et al. Relationship between raised BMI and sugar sweetened beverage and high fat food consumption among children. Obesity. 2014; 22:E96–E103. [DOI] [PubMed] [Google Scholar]
- 28.Zheng M, Allman-Farinelli M, Heitmann BL, Toelle B, Marks G, Cowell C, Rangan A. Liquid versus solid energy intake in relation to body composition among Australian children. J Hum Nutr Diet. 2015;28(S2):70–79. [DOI] [PubMed] [Google Scholar]
- 29.Zheng M, Rangan A, Olsen NJ, Bo Anderson L, Wedderkopp N, Kristensen P, et al. Sugar-sweetened beverages consumption in relation to changes in body fatness over 6 and 12 years among 9-year-old children: the European Youth Heart Study. Eur J Clin Nutr. 2014;68:77–83. [DOI] [PubMed] [Google Scholar]
- 30.Striegel-Moore RH, Thompson D, Affenito SG, Franko DL, Obarzanek E, Barton BA, Schreiber GB. Daniels SR, Schmidt M, Crawford PB. Correlates of beverage intake in adolescent girls: the National Heart Lung and Blood Institute Growth and Health Study. J Pediatr. 2006; 148:183–187. [DOI] [PubMed] [Google Scholar]
- 31.Auerbach BJ, Wolf FM, Hikida A, Vallila-Buchman P, Littman A, Thompson D, Louden D, Taber DR, Krieger J. Fruit juice and change in BMI: A meta-analyses. Pediatrics. 2017; 139(4):e20162454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hasnain SR, Singer MR, Bradlee ML, Moore LL. Beverage intake in early childhood and change in body fat from preschool to adolescence. Child Obes. 2014; 10(1):42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sonneville KR, Long MW, Rifas-Shiman SL, Kleinman K, Gillman MW, Taveras EM. Juice and water intake in infancy and later beverage intake and adiposity: could juice be a gateway drink? Obesity. 2015; 23:170–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O’Sullivan TA, Bremner AP, Bremer HK, Seares ME, Beilin LJ, Mori TA, Lyons-Wall P, Devine A, Oddy WH. Dairy product consumption, dietary nutrient and energy density and associations with obesity in Australian adolescents. J Hum Nutr Diet. 2015; 28(5)452–464. [DOI] [PubMed] [Google Scholar]
- 35.Vogel KA, Martin BR, McCabe LD, Peacock M, Warden SJ, McCabe GP, Weaver CM. The effect of dairy intake on bone mass and body composition in early pubertal girls and boys: a randomized controlled trial. Am J Clin Nutr. 2017; 105(5):1214–1229. [DOI] [PubMed] [Google Scholar]
- 36.Marabujo T, Ramos E, Lopes C. Dairy products and total calcium intake at 13 years of age and its association with obesity at 21 years of age. Eur J Clin Nutr. January 25, 2018; doi: 10.1038/s41430-017-0082-x. [DOI] [PubMed] [Google Scholar]
- 37.Beck AL, Heyman M, Chao C, Wojcicki J. Full fat milk consumption protects against severe childhood obesity in Latinos. Prev Med Rep. 2017; 23(8):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.DeBoer MD, Agard HE, Scharf RJ. Milk intake, height and body mass index in preschool children. Arch Dis Child. 2015; 100(5):460–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kant AK, Graubard BI, Atchinson EA. Intakes of plain water, moisture in foods and beverages, and total water in the adult U.S. population – nutritional, meal pattern, and body weight correlates: National Health and Nutrition Examination Surveys 1999–2006. Am J Clin Nutr. 2009; 90:655–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rosinger AY, Lawman HG, Akinbami LJ, Ogden CL. The role of obesity in the relation between total water intake and urine osmolality in U.S. adults, 2009–2012. Am J Clin Nutr. 2016; 104:1554–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Daniels MC and Popkin BM. The impact of water intake on energy intake and weight status: a systematic review. Nutr Rev. 2010; 68(9):505–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Walton J, O’Connor L, Flynn A. Cross-sectional association of dietary water intakes and sources, and adiposity: National Adult Nutrition Survey, the Republic of Ireland. Eur J Nutr. March 29, 2018; doi. 10.1007/s00394-018-1635-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Drenowsi A, Rehm CD, Constant F. Water and beverage consumption among children age 4–13y in the United States: Analyses of 2005–2010 NHANES data. Nutr J. 2013; 19;12:85. doi: 10.1186/1475-2891-12-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fulgoni VL and Quann EE. National trends in beverage consumption in children from birth to 5 years: analyses of NHANES across three decades. Nutr J. 2012; 11:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bleich SN, Vercammen KA, Koma JW, Li Z. Trends in beverage consumption among children and adults, 2003–2014. Obesity. 2018; 26:432–441. [DOI] [PubMed] [Google Scholar]
- 46.Dietary Guidelines for Americans 2015–2020. United States Department of Agriculture; Available at: https://health.gov/dietaryguidelines/2015/guidelines/. Accessed 4/17/18. [Google Scholar]
- 47.Heyman MB, Abrams SA, AAP Section on Gastroenterology, Hepatology and Nutrition, AAP Committee on Nutrition. Fruit juice in infants, children and adolescents: current recommendations. Pediatrics. 2017; 139(6):e20170967. [DOI] [PubMed] [Google Scholar]
- 48.MyPlate. United States Department of Agriculture. Available at: http://www.choosemyplate.gov/ Accessed 4/17/18.