Abstract
Background
Despite interventions to improve the nutrition of grocery store purchases, also referred to as at home (AH) foods, by SNAP participants, little is known about what proportion of participants’ intake is from AH foods and how the dietary quality of AH food compares to participants’ away-from-home (AFH) food. While recent research indicates SNAP participants have slightly worse dietary quality than income-eligible nonparticipants, it is unknown if this is attributable to AH or AFH consumption.
Objective
The objective of this study is to examine differences in self-reported dietary intake by food source for SNAP participants compared to income-eligible non-participants using 2011–2014 data from the National Health and Nutrition Examination Survey (NHANES).
Design
This study included data from the National Health and Nutrition Examination Survey (NHANES), a cross-sectional, nationally representative survey of the US population.
Study participants
This study included 2,523 adults with low incomes (≤130% Federal Poverty Limit) in NHANES (2011–2014).
Main outcome measures
Self-reported intake of calories, solid fats, added sugars, and servings of non-starchy vegetables, whole fruits, and whole grains, was assessed by food source in SNAP participants and income-eligible nonparticipants.
Statistical analysis
Multivariate linear regression was used for each outcome, controlling for relevant sociodemographic characteristics. Data was stratified by food source, including grocery stores, sit-down restaurants, and fast food.
Results
SNAP participants had a higher intake of solid fats and added sugar (SoFAS) from AH foods than nonparticipants. Added sugar from AH food accounted for 15.3% of total calories consumed by SNAP participants, compared to 11.8% for nonparticipants. SNAP participants consumed fewer calories from sit-down restaurants, but both groups consumed similar calories from fast food. Consumption of non-starchy vegetables, whole fruits and whole grains were low for both groups.
Conclusions
SNAP participants had poorer diet quality from AH food than did nonparticipants. Future research should focus on interventions to improve the healthfulness of grocery store purchases as a mechanism to improve dietary quality of SNAP participants.
Five keywords: Supplemental Nutrition Assistance Program, low-income, diet quality, at-home, away-from-home
Introduction
Poor diet has been associated with a higher incidence of obesity and chronic disease1 and there is evidence that Americans with lower incomes disproportionately suffer from obesity and nutrition-related health problems.1,2 As the largest federal food assistance program,3 the Supplemental Nutrition Assistance Program (SNAP) has the potential to improve the nutrition of Americans with lower incomes and subsequently reduce health disparities in this vulnerable population. Although research on the quality of SNAP participants’ diet has yielded mixed results,4,5 both a recent systematic review and USDA report show that SNAP participants tend to have less healthy diets as measured by the Healthy Eating Index.6,7
One major unanswered question is whether SNAP dietary quality varies by where food is obtained. Specifically, few studies8,9 evaluate the dietary quality of food from away from home (AFH) sources, such as fast food and sit-down restaurants, and at-home (AH) food sources, such as grocery stores, for SNAP participants. SNAP can only improve the dietary quality of AH food since benefits can only be spent at grocery stores. Although it is established that SNAP participants are less likely than nonparticipants to eat AFH food 10–12 and that an increase in SNAP benefits increases money spent on AH food,10,13 more money spent on groceries may not result in more nutritious purchases if foods are chosen for shelf-life stability or convenience.14,15 While those who consume more AH food tend to have healthier diets,16,17 it is unknown if this is true among SNAP participants. Furthermore, it is important to assess dietary trends in the context of a rapidly changing food supply,5 evolving food preferences, updated dietary guidelines and rising trends in consuming AFH food.18
The objective of this study is to examine differences in self-reported dietary intake by food source for SNAP participants compared to income-eligible non-participants using 2011–2014 data from the National Health and Nutrition Examination Survey (NHANES).
Methods and Data
Study Design and Population
The present analysis included 2,523 adults with lower incomes 20 to 64 years of age from the 2011–2012 and 2013–2014 waves of the National Health and Nutrition Examination Survey (NHANES). NHANES is a representative, cross-sectional study of the non-institutionalized US population using a stratified, four-stage probability sampling design. Oversampling is carried out for certain subgroups, including Hispanics, non-Hispanic Blacks, and persons with lower income. Data collection includes demographic and health interviews as well as 24-hour dietary recalls.19 This study was deemed exempt from IRB approval by the University of North Carolina Office of Human Research Ethics, as it does not constitute human subjects research as defined under federal regulations [45 CFR 46.102 (d of f) and 21 CFR 56.102 (c)(e)(l)].
The study population was limited to individuals meeting the gross income eligibility requirement to qualify for SNAP, defined as a family income ≤ 130% of the federal poverty level (FPL).20 Sensitivity analyses were conducted by expanding the population to those at 200% of the FPL for two reasons. First, higher income households can receive benefits based on broadened net income and asset testing, which increased SNAP enrollment following the 2008 recession.21 Second, since eligibility is transitory over the course of the year, particularly among adults in low-wage jobs, some families may have been eligible for SNAP at the time of the survey despite having an annual income higher than the 130% FPL threshold.3,22–24 In the sensitivity analyses, only the association between SNAP participation and per consumer consumption of calories from restaurants was affected and found to no longer be significant.
SNAP Exposure
SNAP participants were identified using the NHANES Food Security Questionnaire,25 and were considered SNAP beneficiaries if they reported receiving SNAP benefits in the past 30 days. Individuals with reported incomes ≤130% of the FPL but not currently receiving SNAP benefits were considered “income-eligible nonparticipants,” (hereafter referred to as nonparticipants). Although it is common in the literature to define SNAP participation as having received benefits in the past 12 months,26,27 the present study assumes individuals would only alter their intake behavior while they were currently receiving SNAP benefits. When SNAP participation was instead defined as receipt of benefits within the past 12 months at 130% of the FPL, only the association of SNAP participation and the consumption of solid fats from grocery store foods was affected. While the association was no longer significant, there was little substantive difference in amount of solid fat consumed. An additional sensitivity analysis defined SNAP participation as the receipt of benefits in the past 30 days but nonparticipants only included those income-eligible individuals who had not used SNAP in the past 12 months. Individuals who used SNAP within the past 12 months but not the past 30 days were excluded from the study sample.28 This change did not affect associations between SNAP status and nutrient outcomes.
Dietary data
Details of the NHANES method of collecting dietary intake data have been described elsewhere.29 In brief, self-reported dietary data are collected via a 24h recall during an in-person interview using USDA’s Automated Multiple Pass method.30 The analytic sample includes only the first day of two days of dietary intake data, as recommended for the examination of population means.31 Waves of NHANES were combined to ensure sufficient sample size (2011–2012 with 2013–2014). Caloric data was sources from the USDA’s Food and Nutrient Database for Dietary Studies (FNDDS)32 while solid fats, added sugars, servings of fruit and vegetables and ounce equivalents of whole grains were sourced from the USDA’s Food Patterns Equivalents Database (FPED)33 for the corresponding survey cycles.
Dietary outcomes included calories, solid fats, added sugars, servings of non-starchy vegetables, servings of whole fruits and ounce equivalents of whole grains. Following the 2015–2020 Dietary Guidelines for Americans, solid fats and added sugars (SoFAS) are the two macronutrients Americans should limit in their diet,34 whereas non-starchy vegetables, whole fruits and whole grains are recommended and represent the majority of MyPlate.1 Participants reported where each food and beverage consumed was obtained. These food sources were categorized as 1) grocery store (store, convenience store, and store with no additional information), 2) sit-down restaurant (restaurant with water/waitress, restaurant with no additional information, bar/tavern/lounge and cafeteria not at school), 3) fast food restaurant (restaurant fast food/pizza, street vendor and sport, recreation or entertainment facility) and 4) other sources (including soup kitchens, community food programs, meals on wheels, vending machines, common coffee pot, mail order purchases, home garden or hunting, fundraiser sales, gifts and other). Study participants missing source information for at least one food item were excluded from analysis (n=30).
Covariate data
Covariate data was collected from the interviewer-administered Demographic,35,36 Food Security25,37 and Occupation questionnaires.38,39 Multivariate regression included covariates for sex, age (continuous, including quadratic term), race/ethnicity (Mexican-American, Non-Hispanic White, Non-Hispanic Black (referent), Other), marital status (married/living with partner or other), poverty income ratio (family income as a percentage of the federal poverty level, continuous), employment (yes/no), education (less than high school (referent), high school/GED, some college or college graduate or above), participation in the Special Supplemental Nutrition Program for Women, Infants and Children (recipient in the past 12 months or not), whether the dietary recall was for food consumed on the weekend (defined as Friday, Saturday or Sunday) and year (2011–2012 or 2013–2014). Complete case analysis was used (missing covariate data: n=2).
Statistical Analysis
All analyses used the NHANES dietary day 1 sample weights to derive nationally representative estimates. Due to pooling data from 2011–2014, these weights were recalculated to account for the probability of being sampled over four years instead of two.40 Proportions testing and t-tests were used to compare the sociodemographic characteristics of SNAP participants and nonparticipants in the study sample.
Ordinary least squares (OLS) linear regression models controlling for covariates were used to examine the association between SNAP status and nutrient intake for each of the four food source categories. The use of OLS models follows similar research examining the association between SNAP status and dietary quality.9,22,27,41,42 For primary analysis, the average nutrient intake per food source was estimated across the pooled sample population. Since few individuals consume food from all four food sources in one 24-hour dietary recall, a secondary per consumer analysis was conducted in which the average nutrient and food intakes per source were estimated only among those who consumed at least one food item from that source. In the first per capita analysis, SoFAS were calculated as a percent of total energy intake across all food sources, whereas in the second per consumer analysis, SoFAS were calculated as a percentage of total energy intake from a given food source. In both analyses, a Wald test for the interaction between SNAP participation and survey year was found to be statistically insignificant; therefore, pooling data from 2011–2014 was not found to violate the assumption of homogeneity in the association between SNAP participation and nutrient intake within this time period. In addition, a sensitivity analysis was conducted to evaluate whether results were robust to outliers. Exclusion of the top one percent of consumers of each dietary outcome did not alter significant associations.
Statistical analyses were performed using STATA 14.2.43 Estimates were generated using STATA’s svy command to adjust for NHANES complex survey design. Variance estimates were calculated using Taylor Series Linearization methods as recommended by the National Center for Health Statistics.44 This method generates linear approximations for the nonlinear estimates resulting from NHANES’ complex sampling design and uses the STATA vce(unconditional) option on estimation commands. Significant differences in nutrient intakes were identified with Wald tests using STATA margins and contrast post-estimation commands to compare participant groups. All hypothesis testing was two-sided with a significance level of p< 0.025 to adjust for multiple comparisons.
Results
Means and Proportions, unadjusted for covariates
Of the 2,523 adults included in the sample period, 1,191 (47.2%) reported current participation in SNAP (Table 1). SNAP participants were more likely to be women, identify as non-Hispanic Black and receive WIC benefits. Although the sample was restricted to individuals with a family income below 130% FPL, participants were still found to have a lower poverty income ratio than nonparticipants. Participants were also less likely to be employed or have a college degree. SNAP participants reported consuming a greater percentage of daily total calories from grocery stores than did nonparticipants (Table 2), which was true for both average consumption of grocery store food (per capita, p=0.01) as well as when the sample was restricted to only those individuals who consumed any food from grocery stores (per consumer, p=0.004). On average, SNAP participants were less likely to eat at sit-down restaurants (per capita, p=0.001). SNAP participants also consumed a lower proportion of their total calories from sit-down restaurants even when the sample was restricted to restaurant consumers (per consumer, p=0.036). In addition, the per consumer sample sizes in Table 2 indicate the extent of self-reported nonconsumption by food source and by dietary outcome.
Table 1.
Sociodemographic and average dietary intake characteristics for SNAPa-eligible adults, NHANESb 2011–2014c
| SNAP | non-SNAP | |
|---|---|---|
| n | 1191 | 1332 |
| Missing datad | 14 | 18 |
| Sociodemographic data | ||
| Female | 56.5% | 50.3%* |
| Age, mean ± SE | 39.1 ± 0.6 | 37.7 ± 1.6 |
| Poverty Income Ratio, mean ± SE | .66 ±.02 | .84 ±.03*** |
| Married/Living with partner | 41.5% | 49.9% |
| Employed | 40.2% | 57.0%*** |
| WICe recipient | 4.8% | 1.1%*** |
| Race/Ethnicity | ||
| Mexican-American | 12.9% | 17.5% |
| Non-Hispanic White | 45.8% | 52.1% |
| Non-Hispanic Black | 24.7% | 12.7%*** |
| Other/Multi-racial | 16.7% | 17.7% |
| Education | ||
| Less than High School | 34.8% | 25.1%* |
| High School/GEDf | 31.9% | 23.4%* |
| Some college | 29.0% | 36.8%* |
| College graduate or above | 4.3% | 14.7%*** |
| Dietary Data | ||
| Daily calories, mean ± SE | 2298 ± 47 | 2276 ± 57 |
| % 24-hour recalls conducted on a weekend day, Fri – Sun | 41.3 % | 38.7% |
SNAP=Supplemental Nutrition Assistance Program
NHANES=National Health and Nutrition Examination Survey
Data are for adults aged 20–64 years with an income at or below 130% of the Federal Poverty Limit from NHANES 2011–2012 and 2013–2014. The sample sizes represent complete case analysis. Data are weighted and nationally representative, but are not adjusted.
Number of individuals excluded from Table 1 statistics and statistical analysis either due to missing covariate data or missing food source information for at least one calorie-containing food item
WIC=Special Supplemental Nutrition Program for Women, Infants and Children
GED=General Education Diploma
Means/proportions are different between SNAP participants and non-participants at p<0.05
p<0.001
Table 2.
Per capita and per consumer average dietary intake characteristics, by SNAPa participation status (mean ± SE)b
| Per capitac mean | n | % nd | Per consumere mean | |
|---|---|---|---|---|
| Percentage of total daily energy intake derived from each food source | ||||
|
| ||||
| SNAP participants | ||||
| Grocery Store | 72.5 ± 1.5 | 1,162 | 97.6% | 74.2 ± 1.3 |
| Sit-down Restaurant | 4.0 ± 0.6 | 155 | 13.0% | 37.5 ± 2.2 |
| Fast Food Restaurant | 16.0 ± 1.2 | 473 | 39.7% | 41.6 ± 1.8 |
| Other Source | 7.6 ± 0.8 | 342 | 28.7% | 25.4 ± 2.0 |
| SNAP non-participants | ||||
| Grocery Store | 65.4 ± 2.9* | 1,304 | 98.0% | 66.8 ± 2.5** |
| Sit-down Restaurant | 10.5 ± 1.7** | 279 | 20.9% | 46.7 ± 3.9* |
| Fast Food Restaurant | 16.1 ± 1.2 | 570 | 42.8% | 39.8 ± 1.3 |
| Other Source | 7.9 ± 0.6 | 463 | 34.8% | 23.3 ± 1.3 |
|
| ||||
| Daily consumption of nutrients and foods | ||||
|
| ||||
| SNAP participants | ||||
| % total energy from solid fats | 14.9 ± 0.5 | 1,171 | 98.3% | 15.1 ± 0.3 |
| % total energy from added sugars | 17.8 ± 0.8 | 1,174 | 98.6% | 18.0 ± 0.8 |
| Servings of non-starchy vegetables | 0.8 ± 0.04 | 998 | 83.8% | 0.9 ± 0.03 |
| Servings of whole fruits | 0.4 ± 0.04 | 450 | 37.8% | 1.1 ± 0.07 |
| Ounce equivalents of whole grains | 0.6 ± 0.04 | 482 | 40.5% | 1.5 ± 0.08 |
| SNAP non-participants | ||||
| % total energy from solid fats | 14.7 ± 0.3 | 1,317 | 98.9% | 14.8 ± 0.3 |
| % total energy from added sugars | 14.9 ± 0.5** | 1,305 | 98.0% | 15.1 ± 0.5** |
| Servings of non-starchy vegetables | 1.1 ± 0.04*** | 1,202 | 90.2% | 1.2 ± 0.05*** |
| Servings of whole fruits | 0.6 ± 0.03*** | 667 | 50.1% | 1.2 ± 0.06 |
| Ounce equivalents of whole grains | 0.7 ± 0.05 | 589 | 44.2% | 1.6 ± 0.08 |
SNAP=Supplemental Nutrition Assistance Program
Results are corrected for National Health and Nutrition Examination Survey (NHANES) complex survey design but are proportions and are unadjusted
Per capita mean consumption is calculated using the full sample of 1,191 SNAP participants and 1,332 non-participants as the denominator for the average.
Proportion of participants who were consumers. For food source data, food source consumers are defined as those individuals who consumed at least one food item from the food source. For nutrient and food data, consumers are defined as having a nonzero consumption for a given nutrient or food group.
Per consumer mean consumption is calculated using only consumers as the denominator for the average, which is equal to the sample population n in the corresponding row.
Significant difference between SNAP participants and nonparticipants, p<0.05
p<0.01
p<0.001
Adjusted Regression Estimates
SNAP participants and nonparticipants consumed similar total calories, a similar proportion of total calories from solid fat, and similar ounce equivalents of whole grains (Table 3). Compared to nonparticipants, however, SNAP participants consumed a higher proportion of total calories from added sugar (2.7 percentage points greater, p=0.001), 0.3 fewer servings of non-starchy vegetables (p<0.001) and 0.2 fewer servings of whole fruit (p<0.001).
Table 3.
| Per capita | Per consumerd | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Food Source | Grocery Store | Sit-down Restaurant | Fast Food | Other source | Total consumption | Grocery Store | Sit-down Restaurant | Fast Food | Other source | Total consumption |
| Calories | ||||||||||
| SNAP participants | 1762 ± 62 | 65 ± 19 | 354 ± 33 | 183 ± 26f | 2363 ± 55 | 1790 ± 61 | 828 ± 62 | 997 ± 59 | 592 ± 53 | 2363 ± 55 |
| Non-participants | 1581e ± 48 | 216e ± 32 | 371 ± 32 | 184 ± 19 | 2352 ± 40 | 1599e ± 46 | 1029e ± 80 | 1003 ± 54 | 520 ± 40 | 2352 ± 40 |
| Solid Fats (% total energy intake)g | ||||||||||
| SNAP participants | 10.1 ± 0.3 | 0.5 ± 0.1 | 2.8 ± 0.3 | 1.3 ± 0.2 | 14.9 ± 0.4 | 13.5 ± 0.3 | 14.5 ± 1.1g | 19.1 ± 1.3 | 14.9 ± 1.2 | 14.9 ± 0.4 |
| Non-participants | 9.1e ± 0.4 | 1.3e ± 0.2 | 3.0 ± 0.2 | 1.3 ± 0.2 | 14.7 ± 0.4 | 12.9 ± 0.5 | 13.8 ± 0.9 | 20.2 ± 1.0 | 14.1 ± 1.1 | 14.7 ± 0.4 |
| Added Sugars (% total energy intake) | ||||||||||
| SNAP participants | 15.3 ± 0.7 | 0.3 ± 0.1 | 1.8 ± 0.2 | 1.4 ± 0.2 | 18.8 ± 0.7 | 22.7 ± 0.7 | 13.9 ± 1.3 | 11.6 ± 0.8 | 22.6 ± 2.6 | 18.8 ± 0.7 |
| Non-participants | 11.8e ± 0.6 | 1.0 ± 0.2 | 1.8 ± 0.2 | 1.4 ± 0.2 | 16.1e ± 0.7 | 19.5e ± 0.6 | 12.4 ± 1.6 | 13.3 ± 1.1 | 21.7 ± 2.4 | 16.1e ± 0.7 |
| Non-starchy vegetables (servings) | ||||||||||
| SNAP participants | 0.5 ± 0.0 | 0.0 ± 0.0 | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.8 ± 0.0 | 0.6 ± 0.0 | 0.4 ± 0.1 | 0.4 ± 0.0 | 0.2 ± 0.0 | 0.8 ± 0.0 |
| Non-participants | 0.7e ± 0.0 | 0.1e ± 0.0 | 0.2 ± 0.0 | 0.1 ± 0.0 | 1.1e ± 0.1 | 0.7e ± 0.0 | 0.6e ± 0.1 | 0.4 ± 0.0 | 0.2 ± 0.0 | 1.1e ± 0.1 |
| Whole fruits (servings) | ||||||||||
| SNAP participants | 0.3 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.3 ± 0.0 | 0.3 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.1 ± 0.0 | 0.3 ± 0.0 |
| Non-participants | 0.5 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.1 ± 0.0 | 0.5e ± 0.0 | 0.5 ± 0.0 | 0.1 ± 0.0 | 0.0 ± 0.0 | 0.2 ± 0.0 | 0.5e ± 0.0 |
| Whole grains (ounce equivalents) | ||||||||||
| SNAP participants | 0.5 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.6 ± 0.1 | 0.6 ± 0.0 | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.1 ± 0.1 | 0.6 ± 0.1 |
| Non-participants | 0.6 ± 0.1 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.7 ± 0.1 | 0.6 ± 0.1 | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.2 ± 0.1 | 0.7 ± 0.1 |
SNAP=Supplemental Nutrition Assistance Program
NHANES=National Health and Nutrition Examination Survey
Data are for adults aged 20–64 years with an income at or below 130% of the Federal Poverty Limit from NHANES 2011–2012 and 2013–2014. The sample size for SNAP participants, defined as receipt of benefits in past 30 days, was 1,191 and 1,332 for income-eligible non-participants. Data are nationally representative and results account for complex survey design. Each nutrient outcome was calculated for each category of food source and included in a separate linear regression model. All models were adjusted for year, age (age and age2), sex, marital status, employment, race-ethnicity (Mexican American, non-Hispanic White, non-Hispanic Black (ref), Other), income (poverty income ratio), education (< high school (ref), high school, some college or college graduate or above), weekend consumption and participation in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC).
In addition to restricting the sample to SNAP-eligible adults aged 20–64 years with complete covariate and diet data, subpopulations are further restricted to those people who consumed calories from a given source. Therefore, the subpopulation for “Grocery store” only includes those people who purchased at least one food item from a grocery store (n = 1,162 for SNAP participants) and is different than the subpopulation for “Restaurant” (n=155 for SNAP participants), although there is overlap between the two. For percent intakes, the calories from saturated fat and added sugar (SOFAS) are divided by the total number of calories consumed from that source, in order to calculate the percent of calories from a given source that are attributable to SOFAS. The total population of SNAP-eligible adults ages 20–64 is used for “Total Consumption” for context. Source-specific sample sizes are as follows: among SNAP participants, there were 1,162 grocery store consumers, 155 sit-down restaurant consumers, 473 fast food restaurant consumers and 342 other food source consumers; among nonparticipants, there were 1,304 grocery store consumers, 279 sit-down restaurant consumers, 570 fast food consumers and 463 other food source consumers.
Significant difference between SNAP participants and income-eligible non-participants within the same time period, significant at p<.025; These results are also bolded
Greyed results reflect models which failed an F-test of overall significance with a p-value >0.05. In other words, the model fails to fit the data better than simply using the intercept, or the mean nutrient intake from a given food source, to predict individual outcomes.
Dietary data for solid fats, added sugars, servings and ounce equivalents are from USDA Food Patterns Equivalents Database (FPED) 2011–2012 and 2013–2014. Non-starchy vegetables include dark-green and orange vegetables, tomatoes and other vegetables, and exclude starchy vegetables, potatoes and dry beans and peas. Added sugars are those used as ingredients in processed and prepared foods and do not include naturally occurring sugars. Discretionary solid fats include fats from animal sources or hydrogenated vegetable oils.
Important patterns emerged when average nutrient intake by food source was assessed. SNAP participants consumed 181 more calories from grocery store foods than nonparticipants (p=0.004), despite consuming similar total calories. Consistent with this pattern, SNAP participants consumed more of their daily calories as solid fats and added sugars (SoFAS) derived from grocery store foods compared to nonparticipants (1.0 percentage point higher for solid fats, p=0.018; 3.5 percentage points higher for added sugar, p<0.001). Additional exploratory analysis suggested that this difference in added sugar consumption may be driven by beverage consumption (Table 4). Patterns in intake also differed according to the source of AFH food. Both groups consumed similar calories from fast-food restaurants. However, SNAP participants on average consumed 151 fewer calories than nonparticipants from sit-down restaurants (p<0.001).
Table 4.
Per capita daily consumption of calories and added sugar of select food groups obtained from grocery stores, NHANESa 2011–2014b (mean ± SD)
| Caloriesc | Added sugar, gd | Added sugar, % total energy intakee | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Food groupf | SNAP participants | Non-participants | SNAP participants | Non-participants | SNAP participants | Non-participants |
| Meat | 54 ± 6 | 42 ± 6 | ||||
| Poultry | 63 ± 7 | 46 ± 6 | ||||
| Processed meats, poultry & products | 51 ± 5 | 37 ± 4 | ||||
| Eggs & egg dishes | 46 ± 5 | 26 ± 3 | ||||
| Nuts, nut butters, seeds & coconut | 25 ± 5 | 37 ± 6 | ||||
| Breads, rolls and tortillas | 118 ± 8 | 106 ± 9 | ||||
| Fruits, fresh, frozen, canned or dried | 29 ± 3 | 44 ± 3 | ||||
| Fried starchy vegetables or starchy vegetable dishes | 22 ± 8 | 10 ± 2 | ||||
| Grain-based desserts | 119 ± 10 | 108 ± 12 | ||||
| Sweeteners, syrups, jellies and toppings | 6.2 ± 0.5 | 4.0 ± 0.3 | 1.9 ± 0.4 | 1.2 ± 0.1 | ||
| Salty snacks | 89 ± 8 | 69 ± 6 | ||||
| Pasta and pasta dishes | 76 ± 19 | 53 ± 7 | ||||
| Pizza & Calzone | 19 ± 5 | 34 ± 7 | ||||
| Coffee/tea | 52 ± 10 | 29 ± 4 | 10.5 ± 2.5 | 4.7 ± 0.9 | 2.3 ± 0.4 | 1.2 ± 0.2 |
| Sugar sweetened beverages | 154 ± 11 | 103 ± 7 | 36.6 ± 2.6 | 24.0 ± 1.6 | 9.7 ± 0.7 | 7.5 ± 0.6 |
| Fluid milk | 79 ± 9 | 48 ± 5 | ||||
| Beer | 65 ± 9 | 51 ± 10 | ||||
NHANES=National Health and Nutrition Examination Survey
Results are corrected for NHANES complex survey design but are unadjusted. Sample population is restricted to adults ages 20–64 years with an income at or below 130% of the Federal Poverty Limit from NHANES 2011–2012 and 2013–2014 and who are consumers of grocery store foods, defined as having consumed at least one food item from a grocery store (n = 1,162 SNAP participants and 1,304 nonparticipants)
Results included only if mean difference between participants and nonparticipants ≥ 10 calories
Results included only if mean difference between participants and nonparticipants ≥ 1 gram
Results included only if mean difference between participants and nonparticipants ≥ 0.5% total intake
Food groups correspond to the food grouping system used by the Global Food Research Program at UNC Chapel Hill. The coffee and tea group includes presweetened teas and coffee with sweetener added by the consumer. Sugar sweetened beverages include soft drinks and fruit drinks, excluding 100% fruit juice.
FPL: Federal Poverty Level; SNAP: Supplemental Nutrition Assistance Program
Author note: we suggest this be included as an online table only
The consumption of healthy foods, including non-starchy vegetables, whole fruits and whole grains, was low for both groups. SNAP participants consumed 0.2 fewer servings of non-starchy vegetables from grocery store foods (p=0.004). Despite this, for both SNAP participants and nonparticipants, the highest proportion of servings of healthy food came from grocery stores.
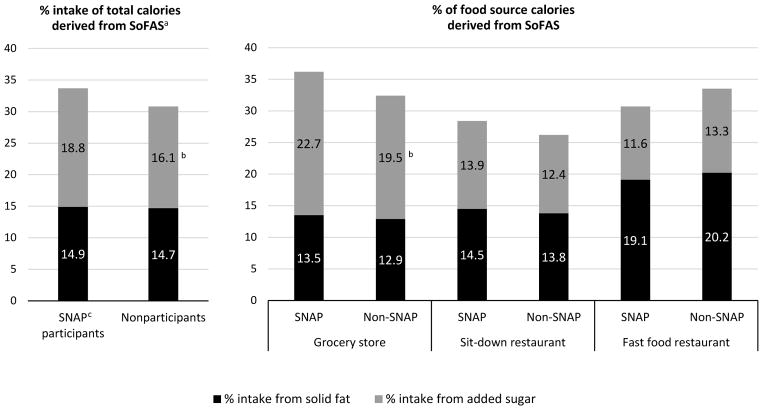
Table 3 also presents data on nutrient intakes for individuals who reported consuming food from a particular food source. SNAP participants who had food from grocery stores consumed more added sugar as a percent of their total calories from grocery store foods than nonparticipants (3.2 percentage points higher, p=0.031) (Figure 1). In other words, for SNAP participants, 22.7% of calories from grocery store foods were derived from added sugar compared to 19.5% of calories for nonparticipants.
Figure 1.
Proportion of food source calories attributable to SoFAS, by SNAP participation
Legend: Data are for adults aged 20–64 years with an income at or below 130% of the Federal Poverty Limit from the National Health and Nutrition Examination Survey (NHANES) 2011–2012 and 2013–2014. The sample size for SNAP participants, defined as receipt of benefits in past 30 days, was 1,191 and 1,332 for income-eligible non-participants. Each nutrient outcome was calculated for each category of food source and included in a separate linear regression model. All models account for complex survey design and were adjusted for year, age (age, age2), sex, marital status, employment, race-ethnicity (Mexican American, non-Hispanic White, non-Hispanic Black (ref), Other), income (poverty income ratio), education (< high school (ref), high school, some college or college graduate or above), weekend consumption and participation in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC). In order to calculate the percent of calories from a given source that are attributable to SoFAS, the calories from saturated fat or added sugar were divided by the total number of calories consumed from that source. Dietary data for solid fats and added sugars are from USDA Food Patterns Equivalents Database (FPED) 2011–2012 and 2013–2014. Added sugars are those used as ingredients in processed and prepared foods and do not include naturally occurring sugars. Discretionary solid fats include fats from animal sources or hydrogenated vegetable oils. aSoFAS=solid fats and added sugars bSignificant difference between SNAP participants and income-eligible non-participants at p<0.025 cSNAP=Supplemental Nutrition Assistance Program
Additionally, while the average per capita calories from sit-down and fast food restaurants were low, these sources are substantial sources of calories for those who consume them. For example, the per capita average consumption of fast food by SNAP participants was 354 calories, while the per consumer average was 997 calories. Among fast food consumers, no difference was found in calories, SoFAS or healthy food intake between SNAP participants and nonparticipants. However, in both participant groups the percentage of calories from fast food attributable to solid fats is notably higher than the percentage of calories from grocery stores derived from solid fats. In comparison to fast food, there is a significant association between SNAP status and calories from sit-down restaurants. In other words, even when only consumers of sit-down restaurants are considered, SNAP participants consume fewer calories than nonparticipants. However, this association is no longer significant in a sensitivity analysis increasing the income of the study sample to 200% FPL from 130% FPL due to the decrease in mean consumption by nonparticipants (Table 5).
Table 5.
Sensitivity analysis of daily nutrient consumption according to category of where food was purchased, by SNAPa participation, NHANESb 2011–2014c
| Per capita nutrient consumption | Per consumer nutrient consumptiond | Total consumption | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Food Source | Grocery Store | Sit-down Restaurant | Fast Food | Other source | Grocery Store | Sit-down Restaurant | Fast Food | Other source | ||
| Calories | ||||||||||
| last 30 days SNAP participants in | ≤130% FPLe | 1762 ± 62f | 65 ± 19 | 354 ± 33 | 183 ± 26 | 1790 ± 61 | 828 ± 62 | 997 ± 59 | 592 ± 53 | 2363 ± 55 |
| ≤200% FPL | 1728 ± 55 | 77 ± 17 | 382 ± 29 | 179 ± 26 | 1752 ± 55 | 818 ± 55 | 983 ± 56 | 583 ± 52 | 2366 ± 53 | |
| SNAP participants in last 12 months | ≤130% FPL | 1755 ± 60 | 70 ± 17 | 362 ± 32 | 180 ± 23 | 1781 ± 60 | 823 ± 56 | 1003 ± 56 | 586 ± 48 | 2367 ± 59 |
| ≤200% FPL | 1706 ± 56 | 91 ± 18 | 387 ± 28 | 179 ± 24 | 1729 ± 55 | 803 ± 55 | 981 ± 54 | 587 ± 47 | 2363 ± 58 | |
| SNAP participants in last 30 days, excluding occasional participantsg | ≤130% FPL | 1751 ± 62 | 68 ± 19 | 350 ± 36 | 188 ± 26 | 1779 ± 62 | 840 ± 60 | 991 ± 62 | 606 ± 55 | 2356 ± 56 |
| ≤200% FPL | 1722 ± 54 | 78 ± 17 | 377 ± 31 | 185 ± 26 | 1746 ± 54 | 817 ± 57 | 978 ± 56 | 598 ± 52 | 2362 ± 52 | |
| Nonparticipants in last 30 days | ≤130% FPL | 1581h ± 48 | 216h ± 32 | 371 ± 32 | 184 ± 19 | 1599h ± 46 | 1029h ± 80 | 1003 ± 54 | 520 ± 40 | 2352 ± 40 |
| ≤200% FPL | 1522h ± 31 | 218h ± 19 | 403 ± 25 | 172 ± 18 | 1538h ± 30 | 901 ± 45 | 989 ± 40 | 492 ± 39 | 2316 ± 36 | |
| Nonparticipants in last 12 months | ≤130% FPL | 1567h ± 47 | 231h ± 36 | 364 ± 34 | 189 ± 22 | 1587h ± 44 | 1044h ± 88 | 997 ± 57 | 521 ± 42 | 2352 ± 46 |
| ≤200% FPL | 1524h ± 30 | 219h ± 19 | 402 ± 28 | 172 ± 19 | 1541h ± 28 | 913 ± 50 | 992 ± 41 | 484 ± 41 | 2317 ± 37 | |
| Nonparticipants in last 30 days, excluding occasional participants | ≤130% FPL | 1556h ± 48 | 233h ± 34 | 360 ± 36 | 194 ± 22 | 1575h ± 44 | 1059h ± 84 | 990 ± 58 | 534 ± 44 | 2342 ± 46 |
| ≤200% FPL | 1516h ± 31 | 221h ± 19 | 396 ± 30 | 179 ± 20 | 1532h ± 29 | 913 ± 51 | 986 ± 42 | 498 ± 43 | 2311 ± 47 | |
| Solid Fats (%total energy intake)i | ||||||||||
| last 30 days SNAP participants in | ≤130% FPL | 10.1 ± 0.3 | 0.5 ± 0.1 | 2.8 ± 0.3 | 1.3 ± 0.2 | 13.5 ± 0.3 | 14.5 ± 1.1 | 19.1 ± 1.3 | 14.9 ± 1.2 | 14.9 ± 0.4 |
| ≤200% FPL | 9.9 ± 0.3 | 0.5 ± 0.1 | 3.1 ± 0.2 | 1.3 ± 0.2 | 13.5 ± 0.3 | 14.1 ± 1.1 | 19.6 ± 1.1 | 15.6 ± 1.3 | 14.8 ± 0.4 | |
| SNAP participants in last 12 months | ≤130% FPL | 10.0 ± 0.3 | 0.5 ± 0.1 | 3.0 ± 0.3 | 1.2 ± 0.2 | 13.5 ± 0.3 | 14.1 ± 1.1 | 19.1 ± 1.3 | 14.2 ± 1.2 | 14.8 ± 0.4 |
| ≤200% FPL | 9.8 ± 0.3 | 0.6 ± 0.1 | 3.1 ± 0.2 | 1.2 ± 0.2 | 13.4 ± 0.3 | 13.8 ± 1.1 | 19.7 ± 1.1 | 15.1 ± 1.3 | 14.8 ± 0.4 | |
| SNAP participants in last 30 days, excluding occasional participants | ≤130% FPL | 10.1 ± 0.3 | 0.5 ± 0.1 | 2.9 ± 0.3 | 1.3 ± 0.2 | 13.6 ± 0.4 | 14.4 ± 1.1 | 19.2 ± 1.3 | 14.9 ± 1.3 | 14.9 ± 0.4 |
| ≤200% FPL | 9.9 ± 0.3 | 0.5 ± 0.1 | 3.1 ± 0.3 | 1.3 ± 0.2 | 13.5 ± 0.4 | 14.2 ± 1.1 | 19.7 ± 1.2 | 15.7 ± 1.3 | 14.8 ± 0.4 | |
| Nonparticipants in last 30 days | ≤130% FPL | 9.1h ± 0.4 | 1.3h ± 0.2 | 3.0 ± 0.2 | 1.3 ± 0.2 | 12.9 ± 0.5 | 13.8 ± 0.9 | 20.2 ± 1.0 | 14.1 ± 1.1 | 14.7 ± 0.4 |
| ≤200% FPL | 9.0h ± 0.4 | 1.3h ± 0.1 | 3.2 ± 0.2 | 1.1 ± 0.2 | 13.0 ± 0.3 | 12.8 ± 0.9 | 19.3 ± 0.8 | 13.6 ± 1.2 | 14.6 ± 0.4 | |
| Nonparticipants in last 12 months | ≤130% FPL | 9.1 ± 0.4 | 1.4h ± 0.2 | 3.0 ± 0.3 | 1.4 ± 0.2 | 13.0 ± 0.5 | 14.0 ± 0.9 | 20.5 ± 1.1 | 14.6 ± 1.0 | 14.9 ± 0.4 |
| ≤200% FPL | 9.1 ± 0.3 | 1.3h ± 0.1 | 3.2 ± 0.2 | 1.1 ± 0.2 | 13.1 ± 0.5 | 12.7 ± 1.2 | 19.2 ± 0.8 | 13.8 ± 1.2 | 14.7 ± 0.4 | |
| Nonparticipants in last 30 days, excluding occasional participants | ≤130% FPL | 9.0h ± 0.3 | 1.4h ± 0.2 | 3.0 ± 0.3 | 1.4 ± 0.2 | 13.0 ± 0.5 | 13.8 ± 0.9 | 20.5 ± 1.1 | 14.6 ± 1.1 | 14.8 ± 0.4 |
| ≤200% FPL | 9.0h ± 0.3 | 1.4h ± 0.1 | 3.2 ± 0.2 | 1.1 ± 0.2 | 13.1 ± 0.5 | 12.8 ± 1.2 | 19.3 ± 0.8 | 13.9 ± 1.3 | 14.7 ± 0.4 | |
| Added Sugars (% total energy intake) | ||||||||||
| last 30 days SNAP participants in | ≤130% FPL | 15.3 ± 0.7 | 0.3 ± 0.1 | 1.8 ± 0.2 | 1.4 ± 0.2 | 22.7 ± 0.7 | 13.9 ± 1.3 | 11.6 ± 0.8 | 22.6 ± 2.6 | 18.8 ± 0.7 |
| ≤200% FPL | 15.4 ± 0.6 | 0.4 ± 0.1 | 2.0 ± 0.2 | 1.4 ± 0.2 | 22.8 ± 0.7 | 13.5 ± 1.1 | 12.5 ± 1.0 | 23.2 ± 2.5 | 19.2 ± 0.7 | |
| SNAP participants in | ≤130% FPL | 15.1 ± 0.6 | 0.4 ± 0.1 | 1.9 ± 0.2 | 1.4 ± 0.2 | 22.5 ± 0.7 | 14.3 ± 1.3 | 12.3 ± 0.8 | 22.8 ± 2.5 | 18.8 ± 0.7 |
| last 12 months | ≤200% FPL | 15.2 ± 0.6 | 0.4 ± 0.1 | 2.1 ± 0.2 | 1.4 ± 0.2 | 22.7 ± 0.7 | 13.0 ± 1.1 | 13.2 ± 1.0 | 23.3 ± 2.4 | 19.1 ± 0.7 |
| SNAP participants in last 30 days, excluding occasional participants | ≤130% FPL | 15.2 ± 0.7 | 0.3 ± 0.1 | 1.9 ± 0.2 | 1.4 ± 0.2 | 22.5 ± 0.7 | 14.2 ± 1.3 | 11.9 ± 0.8 | 22.2 ± 2.6 | 18.7 ± 0.7 |
| ≤200% FPL | 15.3 ± 0.6 | 0.4 ± 0.1 | 2.0 ± 0.2 | 1.4 ± 0.2 | 22.6 ± 0.7 | 13.6 ± 1.1 | 12.7 ± 1.0 | 22.9 ± 2.5 | 19.1 ± 0.7 | |
| Nonparticipants in last 30 days | ≤130% FPL | 11.8h ± 0.6 | 1.0 ± 0.2 | 1.8 ± 0.2 | 1.4 ± 0.2 | 19.5h ± 0.6 | 12.4 ± 1.6 | 13.3 ± 1.1 | 21.7 ± 2.4 | 16.1h ± 0.7 |
| ≤200% FPL | 11.3h ± 0.4 | 1.0h ± 0.1 | 2.0 ± 0.2 | 1.4 ± 0.2 | 19.0h ± 0.7 | 11.8 ± 1.2 | 13.9 ± 1.0 | 22.8 ± 1.9 | 15.7h ± 0.5 | |
| Nonparticipants in last 12 months | ≤130% FPL | 11.5h ± 0.6 | 1.1h ± 0.2 | 1.7 ± 0.2 | 1.4 ± 0.2 | 19.3h ± 1.0 | 12.1 ± 1.6 | 12.6 ± 1.1 | 21.4 ± 2.3 | 15.7h ± 0.6 |
| ≤200% FPL | 11.1h ± 0.4 | 1.0h ± 0.1 | 2.0 ± 0.3 | 1.4 ± 0.2 | 18.7h ± 0.8 | 12.0 ± 1.6 | 13.3 ± 1.0 | 22.8 ± 1.9 | 15.5h ± 0.5 | |
| Nonparticipants in last 30 days, excluding occasional participants | ≤130% FPL | 11.4h ± 0.5 | 1.1h ± 0.2 | 1.7 ± 0.2 | 1.5 ± 0.2 | 19.1h ± 0.9 | 12.5 ± 1.7 | 13.1 ± 1.1 | 21.1 ± 2.3 | 15.7h ± 0.5 |
| ≤200% FPL | 10.9h ± 0.4 | 1.0h ± 0.1 | 2.0 ± 0.3 | 1.4 ± 0.2 | 18.6h ± 0.7 | 12.1 ± 1.2 | 13.6 ± 1.1 | 22.5 ± 1.8 | 15.4h ± 0.4 | |
SNAP=Supplemental Nutrition Assistance Program
NHANES=National Health and Nutrition Examination Survey
Data are for adults aged 20–64 years from NHANES 2011–2012 and 2013–2014. The sample size for SNAP participants, defined as receipt of benefits in past 30 days, was 1,191 and 1,332 for income-eligible non-participants. Data are nationally representative and results account for complex survey design. Each nutrient outcome was calculated for each category of food source and included in a separate linear regression model. All models were adjusted for year, age (age and age2), sex, marital status, employment, race-ethnicity (Mexican American, non-Hispanic White, non-Hispanic Black (ref), Other), income (poverty income ratio), education (< high school (ref), high school, some college or college graduate or above), weekend consumption and WIC participation.
In addition to restricting the sample to SNAP-eligible adults aged 20–64 with complete covariate and diet data, subpopulations are further restricted to those people who consumed calories from a given source. Therefore, the subpopulation for “Grocery store” only includes those people who purchased at least one food item from a grocery store (n = 1,162 for SNAP participants) and is different than the subpopulation for “Restaurant” (n=155 for SNAP participants), although there is overlap between the two. For percent intakes, the calories from saturated fat and added sugar (SOFAS) are divided by the total number of calories consumed from that source, in order to calculate the percent of calories from a given source that are attributable to SOFAS.
Results in grey were presented in main analysis where SNAP participation was measured by receipt of benefits in the past 30 days and the sample was restricted to adults with a family income at or below 130% of the Federal Poverty Level (FPL), the federal income eligibility criteria for SNAP. Three types of sensitivity analysis were conducted. First, since many states have expanded eligibility, the sample population was expanded to at or below 200% FPL. Second, SNAP participation was defined as receipt of benefits within the past 12 months. Third, “occasional” participants were excluded from analysis to compare current SNAP participants with individuals who had no participated for at least a year. Results of sensitivity analysis are limited to calories, solid fats and added sugars, as very few differences were observed in servings of whole fruits, non-starchy vegetables and whole grains.
Comparisons are between participant and nonparticipant groups from the same sample population, defined by family income as a % of the FPL and SNAP status.
”Occasional” participants are excluded from this analysis, or those individuals who were not currently receiving benefits but had received benefits in the past 12 months. This population of nonparticipants includes individuals who had not received benefits in at least one year and should be compared with SNAP participants who had received benefits in the past 30 days.
Significant difference between SNAP participants and income-eligible non-participants at p<.025; These results are also bolded
Dietary data for solid fats, added sugars, servings and ounce equivalents are from USDA Food Patterns Equivalents Database (FPED) 2011–2012 and 2013–2014. Added sugars are those used as ingredients in processed and prepared foods and do not include naturally occurring sugars. Discretionary solid fats include fats from animal sources or hydrogenated vegetable oils.
Author note: We suggest this table be included online only
While not the primary focus of this study, these associations between SNAP status and nutrient intakes are found to be robust when comparing cross sections from 2003–2006 and 2007–2010 (Table 6). While there is no statistically significant association between SNAP status and SoFAS from grocery stores in 2003–2006, possibly due to the small sample of SNAP participants during this time period (n=373), a substantive difference is still noted.
Table 6.
Per capita daily nutrient consumption according to category of where food was purchased, by SNAPa participation and time period, NHANESb, c
| 2003–2006 | 2007–2010 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Food Source | Grocery Store | Sit-down Restaurant | Fast Food | Other source | Total consumption | Grocery Store | Sit-down Restaurant | Fast Food | Other source | Total consumption |
| Calories | ||||||||||
| SNAP participants | 1630 ± 80 | 95 ± 31 | 357 ± 47 | 103 ± 31 | 2186 ± 91 | 1690 ± 49 | 54 ± 15 | 329 ± 26 | 110 ± 18 | 2182 ± 42 |
| Non-participants | 1753 ± 51 | 190d ± 22 | 362 ± 39 | 132 ± 16 | 2437d ± 53 | 1593 ± 43 | 174d ± 25 | 325 ± 31 | 127 ± 19 | 2219 ± 44 |
| Solid Fats (% total energy intake)e | ||||||||||
| SNAP participants | 12.7 ± 0.9f | 0.8 ± 0.2 | 3.6 ± 0.5 | 1.0 ± 0.3 | 18.1 ± 0.1 | 11.8 ± 0.3 | 0.4 ± 0.1 | 2.9 ± 0.2 | 0.7 ± 0.2 | 15.9 ± 0.4 |
| Non-participants | 10.9 ± 0.4c | 1.3d ± 0.2 | 3.5 ± 0.3 | 1.1 ± 0.1 | 18.9 ± 0.1 | 10.3d ± 0.4 | 1.1d ± 0.2 | 2.9 ± 0.2 | 0.9 ± 0.1 | 15.3 ± 0.4 |
| Added Sugars (% total energy intake) | ||||||||||
| SNAP participants | 16.6 ± 1.0 | 0.6 ± 0.2 | 1.9 ± 0.3 | 1.5 ± 0.7 | 21.0 ± 1.0 | 15.9 ± 0.6 | 0.4 ± 0.1 | 1.8 ± 0.3 | 1.0 ± 0.2 | 19.1 ± 0.6 |
| Non-participants | 15.2 ± 1.1 | 1.2 ± 0.2 | 1.2 ± 0.2 | 1.2 ± 0.2 | 18.9d ± 1.0 | 13.0d ± 0.6 | 0.8 ± 0.2 | 1.6 ± 0.2 | 1.3 ± 0.1 | 16.6d ± 0.7 |
| Non-starchy vegetables (servings) | ||||||||||
| SNAP participants | 0.6 ± 0.1 | 0.0 ± 0.0 | 0.2 ± 0.0 | 0.1 ± 0.0 | 0.9 ± 0.1 | 0.7 ± 0.0 | 0.0 ± 0.0 | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.9 ± 0.0 |
| Non-participants | 0.7 ± 0.0 | 0.1d ± 0.0 | 0.2 ± 0.0 | 0.1 ± 0.0 | 1.1d ± 0.1 | 0.7 ± 0.0 | 0.1d ± 0.0 | 0.2 ± 0.0 | 0.1 ± 0.0 | 1.1 ± 0.0 |
| Whole fruits (servings) | ||||||||||
| SNAP participants | 0.6 ± 0.2 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.1 ± 0.0 | 0.7 ± 0.2 | 0.4 ± 0.1 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.4 ± 0.1 |
| Non-participants | 0.6 ± 0.1 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.1 ± 0.0 | 0.7 ± 0.1 | 0.5 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.5 ± 0.0 |
| Whole grains (ounce equivalents) | ||||||||||
| SNAP participants | 0.4 ± 0.1 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.4 ± 0.1 | 0.4 ± 0.1 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.5 ± 0.1 |
| Non-participants | 0.5 ± 0.1 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.5 ± 0.1 | 0.5 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.6 ± 0.0 |
SNAP=Supplemental Nutrition Assistance Program
NHANES=National Health and Nutrition Examination Survey
Data are for adults aged 20–64 years with an income at or below 130% of the Federal Poverty Limit from NHANES 2003–2004, 2005–2006, 2007–2008 and 2009–2010. The sample size for SNAP participants was 373 in 2003–2006 and 1,056 in 2007–2010. The sample size for income-eligible non-participants was 1,342 in 2003–2006 and 1,498 in 2007–2010. Data are nationally representative and results account for complex survey design. Data samples were pooled, combining 2003–2004 with 2005–2006 and 2007–2008 with 2009–2010. Each nutrient outcome was calculated for each category of food source and included in a separate linear regression model. All models were adjusted for year, age (age and age2), sex, marital status, employment, race-ethnicity (Mexican American, non-Hispanic White, non-Hispanic Black (ref), Other), income (poverty income ratio), education (< high school (ref), high school, some college or college graduate or above), weekend consumption and WIC participation.
Significant difference between SNAP participants and income-eligible non-participants within the same time period, significant at p<.025; These results are also bolded
Dietary data for solid fats, added sugars, servings and ounce equivalents are from USDA MyPlate Equivalents Database (MPED) 2003–2004 and Food Patterns Equivalents Database (FPED) 2005–2006, 2007–2008 and 2009–2010. Non-starchy vegetables include dark-green and orange vegetables, tomatoes and other vegetables, and exclude starchy vegetables, potatoes and dry beans and peas. Added sugars are those used as ingredients in processed and prepared foods and do not include naturally occurring sugars. Discretionary solid fats include fats from animal sources or hydrogenated vegetable oils.
Greyed results reflect models which failed an F-test of overall significance with a p-value >0.05. In other words, the model fails to fit the data better than simply using the intercept, or the mean nutrient intake from a given food source, to predict individual outcomes.
Author note: we suggest this be included as an online table only
Discussion
Few studies have analyzed the relationship between SNAP status and dietary quality relative to where food is obtained.8,9 Although SNAP participants consume a greater proportion of total calories from grocery store foods (Table 2), this does not translate to an improvement in dietary quality. The present study confirms previous findings that SNAP participants have slightly unhealthier diets compared to income-eligible nonparticipants.4,8,22,28 In particular, this difference in dietary quality appears to be primarily from foods consumed from grocery stores: SNAP participants consume more SoFAS and fewer non-starchy vegetables from grocery stores than nonparticipants.
The present study also aligns with previous findings that most added sugar in the US diet is consumed from AH versus AFH foods45 and adds that SNAP participants consume a greater proportion of calories from added sugar than nonparticipants. The association between SNAP status and added sugar is robust across several analyses. First, SNAP participants consumed more added sugar from all food sources as a proportion of total calories compared to nonparticipants. Second, participants consumed a larger proportion of calories from grocery store foods from added sugar than nonparticipants. Almost one quarter of all calories consumed by participants from grocery store foods came from added sugar alone (Table 4). Recent studies using purchase data have also found that SNAP households buy more foods with added sugar compared to nonparticipants.7,8,46 The use of 24-hour recall data confirms that average consumption patterns reflect purchasing decisions among adults.
One possible explanation for the observed associations is that SNAP participation is an indicator of underlying food preference. SNAP participants may prefer foods with more added sugars than nonparticipants. In particular, several recent studies find SNAP participation is associated with SSB consumption.9,24,41,47,48 Food preference may be partly explained by biopsychological effects of stress that result in unhealthy food choices,49 and the present study confirms that SNAP participants are more likely to have lower income than nonparticipants (Table 1). Alternatively, greater consumption of added sugar and fewer non-starchy vegetables may be explained by food access and store preference. For example, SNAP participants are more likely to shop at supercenters if they are in their neighborhood.15,50 SNAP participants who shop at supercenters are more likely to purchase more of every food, including SSBs and high calorie items.15
Despite the relative healthfulness of AH food,51 these results indicate that it is not sufficient to improve nutrition in adults participating in SNAP solely by increasing the consumption of AH food. Food consumed from grocery stores and convenience stores makes up over 73% of total intake for participants, significantly more than 65% intake for nonparticipants (Table 2). There is evidence that SNAP participants would prefer restrictions on eligible foods and/or incentives that encourage healthier diets.52–54 To take advantage of these preferences, successful nutrition education programs like SNAP-Ed55 could be expanded. In addition, SNAP participants could be “nudged” to follow their preferences for a healthier diet using strategies from behavioral economics.14,56 For example, authorized SNAP retailers could be required to follow choice architecture guidelines that increase the display of healthy food in prominent locations while reducing shelf space for foods and beverages high in added sugar.14
Modifying SNAP-eligible foods using a combination of incentives and restrictions could also improve the dietary quality of AH foods.1,57,58 For example, results from the Healthy Incentives Pilot (HIP) found that providing a rebate of 30 cents for every dollar spent on fruits and vegetables significantly increased the daily consumption of fruits and vegetables. Importantly, participants receiving the rebate did not use their increase in SNAP benefits to consume more unhealthy foods.59 Recent research estimates that fruit and vegetable incentive programs, including HIP, are cost effective due to the improved quality of life of SNAP participants60 and reduced societal cost of chronic disease.61 In addition, recent research indicates that restricting the eligibility of specific unhealthy foods would decrease the consumption of SoFAS.62–64 Supplementary analysis in the present study found the difference in added sugar consumption from AH food may be driven by the consumption of sugar-sweetened beverages (Table 4), including sweetened coffee and tea, sodas and fruit drinks. Further research is needed to establish which food groups are the primary drivers of the difference SoFAS consumption between participants and nonparticipants and therefore the most appropriate targets for purchase restrictions.
While research shows that SNAP participants spend less on AFH foods compared to income-eligible nonparticipants,65 the present study indicates that participants consume a lower proportion of AFH food specifically because they eat out less at sit-down restaurants. In comparison, both groups consume a similar amount of calories from fast food (Table 3) which is associated with poor diet quality and health outcomes.17,66 These results were unexpected - SNAP participants were anticipated to consume less fast food than nonparticipants because benefits should make grocery store food relatively cheaper, reducing fast food consumption. The similar consumption of fast food suggests SNAP benefits are not sufficiently high to overcome the “cost” of preparing food at home.67 The time costs combined with the financial costs of AH food may make home food preparation relatively more expensive than fast food consumption. The findings from this study support the Institute of Medicine’s recommendations that SNAP benefits be increased to account for the time needed to prepare food at home.68 While SNAP cannot impact the quality of fast food consumption, a sufficient increase in benefits may decrease the relative cost of AH food enough to reduce the consumption of fast food compared to nonparticipants. Alternatively, SNAP-eligible foods could be expanded to include healthy, prepared foods, like rotisserie chicken, reducing preparation time.69 This is an important area for potential future research, especially since fast food consumption has been found to attenuate the association between home cooking and improved dietary quality among SNAP participants and nonparticipants.42 Interventions which increase benefits or expand SNAP-eligible purchases to include prepared foods could collect time use and food diaries to evaluate how SNAP benefits and cooking time influence purchasing decisions and dietary quality.
The present study has several limitations. Since SNAP participation is voluntary and non-random, it is not possible to make any causal claims about the association between SNAP participation and the consumption of added sugar or healthy food. Eligibility varies by state, and individuals may not participate due to an application process that may be time consuming and, at times, demeaning.70 SNAP participants may also self-select into the program based on unobservable characteristics that are associated with poorer food selection. Future research is necessary to identify whether participation in SNAP is causally related to the dietary quality of food from different sources. Study findings are also limited by two types of misclassification error. First, self-reported dietary data is often misreported, where unhealthy foods are more likely to be underreported than healthy foods.71 Therefore, consumption of SoFAS may be lower than in reality, although there is unlikely to be differential misclassification between SNAP participants and nonparticipants. Second, participants often report themselves to be nonparticipants.5,55,72,73 Mixing SNAP participants with nonparticipants would make the two groups more similar and attenuate observed differences.
Despite these limitations, this study has several strengths. In comparison with household purchase data, 24 hour dietary recall data captures foods consumed at an individual level rather than purchased at the household level. This data includes food without barcodes, such as loose produce, as well as examine sources of food other than stores. Unlike purchase data, 24 hour recall data does not have to account for food waste or differential preferences within households. NHANES is also a nationally representative survey that oversamples populations with lower incomes, providing a large sample size to evaluate trends in nutrient consumption in SNAP-eligible populations.
Conclusion
The present study finds that SNAP participants consume more calories from AH foods, or grocery and convenience stores, than income-eligible nonparticipants. However, the higher consumption of AH food is not sufficient to improve the dietary quality of SNAP participants. This study finds that the lower dietary quality of SNAP participants compared to nonparticipants is attributable to the dietary quality of the AH food they consume, which is higher in added sugar and lower in non-starchy vegetables. In comparison, nonparticipants consume more food and solid fat from sit-down restaurants and both groups consume similar calories and SoFAS from fast food establishments. Since SNAP benefits can only be redeemed at grocery stores, future research should evaluate the design, impact and cost-effectiveness of point of purchase interventions that incentivize the consumption of healthy AH food.
Research Snapshot.
Research Question
Does the association between SNAP participation and dietary quality differ by food source, including grocery store, sit-down restaurant or fast food?
Key Findings
In this cross-sectional study with 2,523 adults with low income (≤130% Federal Poverty Limit) in the National Health and Nutrition Examination Survey (2011–2014), SNAP participation was associated with higher self-reported consumption of solid fat and added sugar from grocery store foods. SNAP participants consumed fewer calories from sit-down restaurants than income-eligible nonparticipants, but both groups consumed similar calories from fast food. Consumption of non-starchy vegetables, whole fruits and whole grains were low for both groups.
Practice Implications.
1. What is the current knowledge on this topic?
Supplemental Nutrition Assistance Program (SNAP) benefits can only be spent at authorized grocery stores, yet little is known about how this at-home food contributes to participants’ dietary quality compared to away-from-home food.
2. How does this research add to knowledge on this topic?
This is the first study to characterize nutrient intake according to where food is obtained by SNAP participants. Participants consume more solid fats and added sugars from grocery stores compared to low-income nonparticipants.
3. How might this knowledge impact current dietetics practice?
Consuming more at-home food was not associated with higher diet quality for SNAP participants. Therefore, interventions and dietary counseling should address healthful grocery store purchases.
Acknowledgments
We wish to thank Dr. Phil Bardsley for exceptional assistance with the data management and, Ms. Frances Dancy Burton for administrative assistance, and Ms. Denise Ammons for graphics support.
Footnotes
Authors Contributions: AML, BMP and LST participated in the design of the study; AML collected the data and conducted primary analysis; all authors reviewed and refined analysis; AML wrote the first draft; all authors reviewed and commented on subsequent drafts of the manuscript
Conflict of interest disclosures: The authors have no conflicts of interest of any type with respect to this manuscript.
Funding/financial disclosures: NIH (R01DK098072; DK056350) and the CPC (NIH P2C HD050924)
Contributor Information
Allison M Lacko, University of North Carolina at Chapel Hill, Department of Nutrition and Carolina Population Center, Address: Carolina Square, 123 W Franklin Street, Building C, Suite 310, Chapel Hill, NC 27516, Telephone: (908) 625-6323.
Barry M Popkin, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Department of Nutrition and Carolina Population Center, Address: Carolina Square, 123 W Franklin Street, Building C, Suite 210, Chapel Hill, NC 27516, Telephone: (919) 962-6139.
Lindsey Smith Taillie, University of North Carolina at Chapel Hill, Department of Nutrition and Carolina Population Center, Address: Carolina Square, 123 W Franklin Street, Building C, Suite 210, Chapel Hill, NC 27516, Telephone: (919) 445-8313.
References
- 1.Levin SM, Barnard ND, Saltalamacchia RE. A Proposal for Improvements in the Supplemental Nutrition Assistance Program. Am J Prev Med. 2017;52(2S2):S186–S192. doi: 10.1016/j.amepre.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 2.Popkin BM. The Challenge in Improving the Diets of Supplemental Nutrition Assistance Program Recipients: A Historical Commentary. Am J Prev Med. 2017;52(2S2):S106–S114. doi: 10.1016/j.amepre.2016.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelsey Farson Gray KC. Trends in Supplemental Nutrition Assistance Program Participation Rates: Fiscal Year 2010 to Fiscal Year 2015. Vol. 2017 U.S. Department of Agriculture, Food and Nutrition Service; Jun, 2017. [Google Scholar]
- 4.Condon E, Drilea S, Jowers K, et al. Diet quality of Americans by SNAP participation status: Data from the National Health and Nutrition Examination Survey, 2007–2010. Mathematica Policy Research; 2015. [Google Scholar]
- 5.Fox MK, Hamilton W, Lin B-H. Effect of Food Assistance and Nutrition Programs on Nutrition and Health: Volume 3, Literature Review. Economic Research Service, U.S. Department of Agriculture; 2004. [Google Scholar]
- 6.Andreyeva T, Tripp AS, Schwartz MB. Dietary Quality of Americans by Supplemental Nutrition Assistance Program Participation Status: A Systematic Review. Am J Prev Med. 2015;49(4):594–604. doi: 10.1016/j.amepre.2015.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garasky S, Mbwana K, Romualdo A, Tenaglio A, Roy M. Foods typically purchased by SNAP households. Vol. 2016 Alexandria, VA: Prepared by IMPAQ International, LLS for USDA, Food and Nutrition Service; Nov, 2016. [Google Scholar]
- 8.Lisa Mancino JG, Ver Ploeg Michele, Lin Biing-Hwan. Nutritional Quality of Foods Acquired by Americans: Findings From USDA’s National Household Food Acquisition and Purchase Survey. U.S. Department of Agriculture, Economic Research Service; Feb, 2018. [Google Scholar]
- 9.Nguyen BT, Powell LM. Supplemental nutrition assistance program participation and sugar-sweetened beverage consumption, overall and by source. Preventive medicine. 2015;81:82–86. doi: 10.1016/j.ypmed.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Beatty TKM, Tuttle CJ. Expenditure Response to Increases in In-Kind Transfers: Evidence from the Supplemental Nutrition Assistance Program. American Journal of Agricultural Economics. 2014;97(2):390–404. [Google Scholar]
- 11.Jilcott SB, Liu H, DuBose KD, Chen S, Kranz S. Food Stamp Participation is Associated with Fewer Meals Away From Home, Yet Higher Body Mass Index and Waist Circumference in a Nationally Representative Sample. Journal of Nutrition Education and Behavior. 2011;43(2):110–115. doi: 10.1016/j.jneb.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Pan S, Jensen HH. Does the Food Stamp Program Affect Food Security Status and the Composition of Food Expenditures? Journal of Agricultural and Applied Economics. 2008;40(1):21–35. [Google Scholar]
- 13.Mabli J, Malsberger R. Recent Trends in Spending Patterns of Supplemental Nutrition Assistance Program Participants and Other Low-Income Americans. Monthly Labor Review. 2013;136(9):1–32. [Google Scholar]
- 14.Ammerman AS, Hartman T, DeMarco MM. Behavioral Economics and the Supplemental Nutrition Assistance Program. American journal of preventive medicine. 2017;52(2):S145–S150. doi: 10.1016/j.amepre.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 15.Gustafson AA, Allen I, James E, Schoenberg NE, Swanson M. The Relationship between Neighborhood Food Environment and Food Store Choice on Purchasing Habits among SNAP and Lower Income Households. USDA FoodAPS Data. 2016 [Google Scholar]
- 16.Guthrie J, Lin B, Frazao E. Role of Food Prepared Away from Home in the American Diet, 1977–78 versus 1994–96: Changes and Consequences. J Nutr Educ Behav. 2002:34. doi: 10.1016/s1499-4046(06)60083-3. [DOI] [PubMed] [Google Scholar]
- 17.Mancino L, Todd J, Lin B-H. Separating what we eat from where: Measuring the effect of food away from home on diet quality. Food Policy. 2009;34(6):557–562. [Google Scholar]
- 18.Poti JM, Popkin BM. Trends in Energy Intake among US Children by Eating Location and Food Source, 1977–2006. Journal of the American Dietetic Association. 2011;111(8):1156–1164. doi: 10.1016/j.jada.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National health and nutrition examination survey: sample design, 2011–2014. Vital Health Stat 2. 2014;(162):1–33. [PubMed] [Google Scholar]
- 20.Supplemental Nutrition Assistance Program: Eligibility. U.S. Department of Agriculture, Food and Nutrition Services; [Accessed July, 2017]. https://www.fns.usda.gov/snap/eligibility. [Google Scholar]
- 21.Wilde PE. The New Normal: The Supplemental Nutrition Assistance Program (SNAP) American Journal of Agricultural Economics. 2012;95(2):325–331. [Google Scholar]
- 22.Gregory C, Ploeg MV, Andrews A, Coleman-Jensen A. Supplemental Nutrition Assistance Program (SNAP) Participation Leads to Modest Changes in Diet Quality. U.S. Department of Agriculture, Economic Research Service; Apr, 2013. [Google Scholar]
- 23.Gundersen C, Kreider B. Food stamps and food insecurity - What can be learned in the presence of nonclassical measurement error? J Hum Resour. 2008;43(2):352–382. [Google Scholar]
- 24.Todd JE, Ploeg MV. Caloric Beverage Intake Among Adult Supplemental Nutrition Assistance Program Participants. American Journal of Public Health. 2014;104(9):e80–e85. doi: 10.2105/AJPH.2014.301970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey 2011–2012 (Food Security Questionnaire) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; [Accessed January 2017]. https://wwwn.cdc.gov/Nchs/Nhanes/2011-2012/FSQ_G.htm. [Google Scholar]
- 26.Cole N, Fox M. Diet Quality of Americans by Fod Stamp Participation Status: Data from the National Health and Nutrition Examination Survey. VA: U.S. Department of Agriculture, Food and Nutrition Service, Office of Research, Nutrition and Analysis; 2008. [Google Scholar]
- 27.Nguyen BT, Shuval K, Njike VY, Katz DL. The Supplemental Nutrition Assistance Program and dietary quality among US adults: findings from a nationally representative survey. Paper presented at: Mayo Clinic Proceedings; 2014. [DOI] [PubMed] [Google Scholar]
- 28.Leung CW, Ding EL, Catalano PJ, Villamor E, Rimm EB, Willett WC. Dietary intake and dietary quality of low-income adults in the Supplemental Nutrition Assistance Program. The American Journal of Clinical Nutrition. 2012;96(5):977–988. doi: 10.3945/ajcn.112.040014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey MEC In-Person Dietary Interviewers Procedure Manual. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 30.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey 2013–2014 (Dietary Intervew - Individual Foods, First Day) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; [Accessed January 2017]. https://wwwn.cdc.gov/nchs/nhanes/2013-2014/DR1IFF_H.htm. [Google Scholar]
- 31.Dodd KW, Guenther PM, Freedman LS, et al. Statistical Methods for Estimating Usual Intake of Nutrients and Foods: A Review of the Theory. Journal of the American Dietetic Association. 2006;106(10):1640–1650. doi: 10.1016/j.jada.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 32.Overview of the Food and Nutrient Database for Dietary Studies. U.S. Department of Agriculture, Agriculture Research Service; [Accessed July 7, 2017]. https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fndds/ [Google Scholar]
- 33.Overview of Food Patterns Equivalents Database. U.S. Department of Agriculture, Agriculture Research Service; [Accessed July 7, 2017]. https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fped-overview/ [Google Scholar]
- 34.2015–2020 Dietary Guidelines for Americans. US Department of Health and Human Services and US Department of Agriculture; Dec, 2015. [Google Scholar]
- 35.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey 2011–2012 (Demographics) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; [Accessed January 2017]. https://wwwn.cdc.gov/Nchs/Nhanes/2011-2012/DEMO_G.htm. [Google Scholar]
- 36.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey 2013–2014 (Demographics) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; [Accessed January 2017]. https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/DEMO_H.htm. [Google Scholar]
- 37.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey 2013–2014 (Food Security Questionnaire) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; [Accessed January 2017]. https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/FSQ_H.htm. [Google Scholar]
- 38.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey 2011–2012 (Occupation Questionnaire) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; [Accessed January 2017]. https://wwwn.cdc.gov/Nchs/Nhanes/2011-2012/OCQ_G.htm. [Google Scholar]
- 39.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey 2013–2014 (Occupation Questionnaire) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; [Accessed January 2017]. https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/OCQ_H.htm. [Google Scholar]
- 40.Johnson CL, Paulose-Ram R, Ogden CL, et al. National health and nutrition examination survey. Analytic guidelines, 1999–2010. 2013 [PubMed] [Google Scholar]
- 41.Bleich SN, Vine S, Wolfson JA. American adults eligible for the Supplemental Nutritional Assistance Program consume more sugary beverages than ineligible adults. Preventive medicine. 2013;57(6) doi: 10.1016/j.ypmed.2013.1010.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taillie LS, Poti JM. Associations of Cooking With Dietary Intake and Obesity Among Supplemental Nutrition Assistance Program Participants. American journal of preventive medicine. 2017;52(2):S151–S160. doi: 10.1016/j.amepre.2016.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 44.Cutin LR, Mohadjer LK, Dohrmann SM, et al. The National Health and Nutrition Examination Survey: Sample Design 1999–2006. National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 45.Drewnowski A, Rehm CD. Consumption of added sugars among US children and adults by food purchase location and food source. The American journal of clinical nutrition. 2014;100(3):901–907. doi: 10.3945/ajcn.114.089458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grummon AH, Taillie LS. Nutritional profile of Supplemental Nutrition Assistance Program household food and beverage purchases. The American Journal of Clinical Nutrition. 2017;105(6):1433–1442. doi: 10.3945/ajcn.116.147173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Andreyeva T, Luedicke J, Henderson KE, Tripp AS. Grocery store beverage choices by participants in federal food assistance and nutrition programs. Am J Prev Med. 2012;43(4):411–418. doi: 10.1016/j.amepre.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 48.Park J, Lin H-C, Peng C-Y. The Supplemental Nutrition Assistance Program and frequency of sugar-sweetened soft drink consumption among low-income adults in the US. Nutrition and Health. 2017 doi: 10.1177/0260106017726248. 0260106017726248. [DOI] [PubMed] [Google Scholar]
- 49.Laraia BA, Leak TM, Tester JM, Leung CW. Biobehavioral Factors That Shape Nutrition in Low-Income Populations: A Narrative Review. Am J Prev Med. 2017;52(2S2):S118–S126. doi: 10.1016/j.amepre.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hillier A, Chrisinger B, Smith TE, Whiteman E, Kallan M. Influence of SNAP Participation and Food Environment on Nutritional Quality of Food at Home Purchases. University of Kentucky Center for Poverty Research Discussion Paper Series; 2016. [Google Scholar]
- 51.Lin B-H, Guthrie J. Nutritional quality of food prepared at home and away from home. Economic Research Service, US Department of Agriculture; Washington, DC: 2012. [Google Scholar]
- 52.Leung CW, Musicus AA, Willett WC, Rimm EB. Improving the Nutritional Impact of the Supplemental Nutrition Assistance Program:: Perspectives From the Participants. Am J Prev Med. 2017;52(2S2):S193–S198. doi: 10.1016/j.amepre.2016.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mancino L, Guthrie J. SNAP households must balance multiple priorities to achieve a healthful diet. Amber Waves. 2014:1D. [Google Scholar]
- 54.Rydell SA, Turner RM, Lasswell TA, et al. Participant Satisfaction with a Food Benefit Program with Restrictions and Incentives. Journal of the Academy of Nutrition and Dietetics. 2018;118(2):294–300. doi: 10.1016/j.jand.2017.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dannefer R, Abrami A, Rapoport R, Sriphanlop P, Sacks R, Johns M. A Mixed-Methods Evaluation of a SNAP-Ed Farmers’ Market–Based Nutrition Education Program. Journal of Nutrition Education and Behavior. 2015;47(6):516–525.e511. doi: 10.1016/j.jneb.2015.08.021. [DOI] [PubMed] [Google Scholar]
- 56.Just DR, Gabrielyan G. Influencing the food choices of SNAP consumers: Lessons from economics, psychology and marketing. Food Policy. 2018 [Google Scholar]
- 57.Bleich S, Rimm E, Brownell K. U.S. Nutrition Assistance, 2018 - Modifying SNAP to Promote Population Health. N Engl J Med. 2017;376(13):1205–1207. doi: 10.1056/NEJMp1613222. [DOI] [PubMed] [Google Scholar]
- 58.Klerman JA, Collins AM, Olsho LE. Improving nutrition by limiting choice in the Supplemental Nutrition Assistance Program. American journal of preventive medicine. 2017;52(2):S171–S178. doi: 10.1016/j.amepre.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 59.Olsho LE, Klerman JA, Wilde PE, Bartlett S. Financial incentives increase fruit and vegetable intake among Supplemental Nutrition Assistance Program participants: a randomized controlled trial of the USDA Healthy Incentives Pilot–3. The American journal of clinical nutrition. 2016;104(2):423–435. doi: 10.3945/ajcn.115.129320. [DOI] [PubMed] [Google Scholar]
- 60.An R. Nationwide expansion of a financial incentive program on fruit and vegetable purchases among Supplemental Nutrition Assistance Program participants: a cost-effectiveness analysis. Social Science & Medicine. 2015;147:80–88. doi: 10.1016/j.socscimed.2015.09.032. [DOI] [PubMed] [Google Scholar]
- 61.Choi SE, Seligman H, Basu S. Cost effectiveness of subsidizing fruit and vegetable purchases through the supplemental nutrition assistance program. American journal of preventive medicine. 2017;52(5):e147–e155. doi: 10.1016/j.amepre.2016.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cuffey J, Beatty TK, Harnack L. The potential impact of Supplemental Nutrition Assistance Program (SNAP) restrictions on expenditures: a systematic review. Public Health Nutrition. 2016;19(17):3216–3231. doi: 10.1017/S1368980015003511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.French SA, Rydell SA, Mitchell NR, Michael Oakes J, Elbel B, Harnack L. Financial incentives and purchase restrictions in a food benefit program affect the types of foods and beverages purchased: results from a randomized trial. International Journal of Behavioral Nutrition and Physical Activity. 2017;14(1):127. doi: 10.1186/s12966-017-0585-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Harnack L, Oakes J, Elbel B, Beatty T, Rydell S, French S. Effects of subsidies and prohibitions on nutrition in a food benefit program: A randomized clinical trial. JAMA Internal Medicine. 2016;176(11):1610–1619. doi: 10.1001/jamainternmed.2016.5633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tiehen L, Newman C, Kirlin JA. The Food-spending Patterns of Households Participating in the Supplemental Nutrition Assistance Program: Findings from USDA’s FoodAPS. United States Department of Agriculture, Economic Research Service; 2017. [Google Scholar]
- 66.Poti JM, Duffey KJ, Popkin BM. The association of fast food consumption with poor dietary outcomes and obesity among children: is it the fast food or the remainder of the diet? Am J Clin Nutr. 2014;99(1):162–171. doi: 10.3945/ajcn.113.071928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Davis GC. Food at home production and consumption: implications for nutrition quality and policy. Review of Economics of the Household. 2014;12(3):565–588. [Google Scholar]
- 68.Council). IIoMaNNR. Supplemental Nutrition Assistance Program: Examining the evidence to define benefit adequacy. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- 69.Yaktine AL, Caswell JA. SNAP Benefits: Can an Adequate Benefit Be Defined? Advances in Nutrition. 2014;5(1):21–26. doi: 10.3945/an.113.004630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Burstein NR, Patrabansh S, Hamilton WL, Siegel SY. Understanding the Determinants of Supplemental Nutrition Assistance Program Participation. Alexandria, VA: U.S. Department of Agriculture, Food and Nutrition Service, Office of Research and Analysis; 2009. [Google Scholar]
- 71.Rasmussen LB, Matthiessen J, Biltoft-Jensen A, Tetens I. Characteristics of misreporters of dietary intake and physical activity. Public Health Nutrition. 2007;10(3):230–237. doi: 10.1017/S136898000724666X. [DOI] [PubMed] [Google Scholar]
- 72.Almada L, McCarthy I, Tchernis R. What Can We Learn about the Effects of Food Stamps on Obesity in the Presence of Misreporting? American Journal of Agricultural Economics. 2016;98(4):997–1017. [Google Scholar]
- 73.Meyer BD, George R. Errors in Survey Reporting and Imputation and Their Effects on Estimates of Food Stamp Program Participation. U.S. Census Bureau, Center for Economic Studies; 2011. Paper No. CES-WP-11–14. [Google Scholar]