Abstract
Cardiometabolic disease risk begins in early life and tracks through the life course. As described in “Sex-specific trajectories of measures of cardiovascular health during childhood and adolescence: a prospective cohort study” (O’Keeffe et al., 2018), we modelled sex-specific change in 11 key measures of cardiovascular health from birth/early childhood to age 18 years in a British birth cohort study, the Avon Longitudinal Study of Parents and Children (ALSPAC). In this article, we describe the data used in these analyses. Risk factors measured included BMI, fat and lean mass, blood pressure and blood-based biomarkers. Data are from several sources including cord blood at birth, clinic assessments, routine health records, questionnaires and nuclear magnetic resonance spectroscopy. Outcomes were measured over varying time spans from birth or mid-childhood to age 18 and with different numbers of repeated measures per outcome. Analyses were performed using fractional polynomial and linear spline multilevel models. Further information can be found in O’Keeffe et al. (2018).
Specifications table
| Subject area | Epidemiology. |
| More specific subject area | Life course epidemiology. |
| Type of data | Tables and figures of analyzed data. |
| How data was acquired | Cord blood at birth, clinic assessments, routine health records, questionnaires and nuclear magnetic resonance (NMR) spectroscopy. |
| Data format | Analyzed |
| Experimental factors | Measures of cardiovascular health from birth or mid-childhood to 18 years in a UK prospective birth cohort study. |
| Experimental features | Participants were recruited at birth and followed up repeatedly over a period of 18 years. |
| Data source location | Bristol, UK. |
| Data accessibility | Data are with this article. |
| Related research article | O׳Keeffe LM et al. Sex-specific trajectories of measures of cardiovascular health during childhood and adolescence: a prospective cohort study. Atherosclerosis. 2018; 278 (2018): 190–196. |
Value of the data
-
•
Repeated measures of 11 key measures of cardiovascular health have been analyzed and trajectories of these are available for use as exposures or outcomes to address other research questions.
-
•
These trajectories may also be useful in comparative work with other cohorts to better understand change in measures of cardiovascular health during childhood and adolescence, their determinants and associations with outcomes in later life.
-
•
Modelling strategies used for these data may also be useful for others who wish to examine change over time in risk factors, where multiple repeat measures are available.
1. Data
The data shared here are tables and figures of analyzed data from the Avon Longitudinal Study of Parents and Children (ALSPAC). The ALSPAC is a prospective birth cohort study in Southwest England and is described elsewhere in detail [1], [2], [3]. In summary, pregnant women resident in Avon, UK with expected dates of delivery 1st April 1991 to 31st December 1992 were invited to take part in the study. Of the 14,541 initial pregnancies, there was a total of 14,676 foetuses, resulting in 14,062 live births and 13,988 children who were alive at 1 year of age. Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees. Data was available for 11 measures of cardiovascular health from birth or mid-childhood to 18 years. Data on the number, timing and sources of measures are detailed elsewhere [1], [2], [3], [4], [5], [6], [7]. A comprehensive profiling of offspring circulating lipids, lipoproteins, and metabolites was done by a high-throughput nuclear magnetic resonance (NMR) metabolomics platform, providing a snapshot of offspring serum metabolome [8], [9]. Non-fasting glucose at age seven from NMR was included in these analyses. Data were analyzed by sex from birth to 18 years. Model fit statistics for analyses performed, characteristics of participants included and excluded from analyses, mean sex-specific trajectories of each measure of cardiovascular health and results from sensitivity analyses are included in this paper.
2. Experimental design, materials and methods
2.1. Study population
The ALSPAC has been described elsewhere in detail [1], [2], [3]. The study website contains details of all the data that is available through a fully searchable data dictionary http://www.bristol.ac.uk/alspac/researchers/our-data/ [4].
2.2. Methods and statistical analysis
Two approaches, linear splines and fractional polynomials multilevel models were used in the modelling of trajectories of measures of cardiovascular health [1], [10], [11], [12], [13].
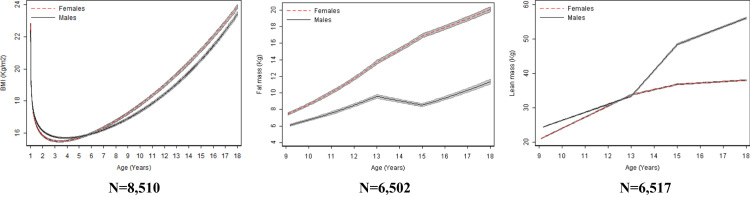
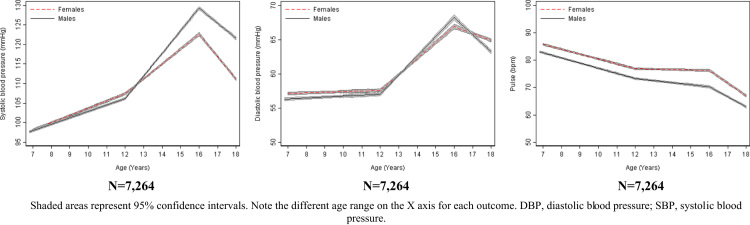
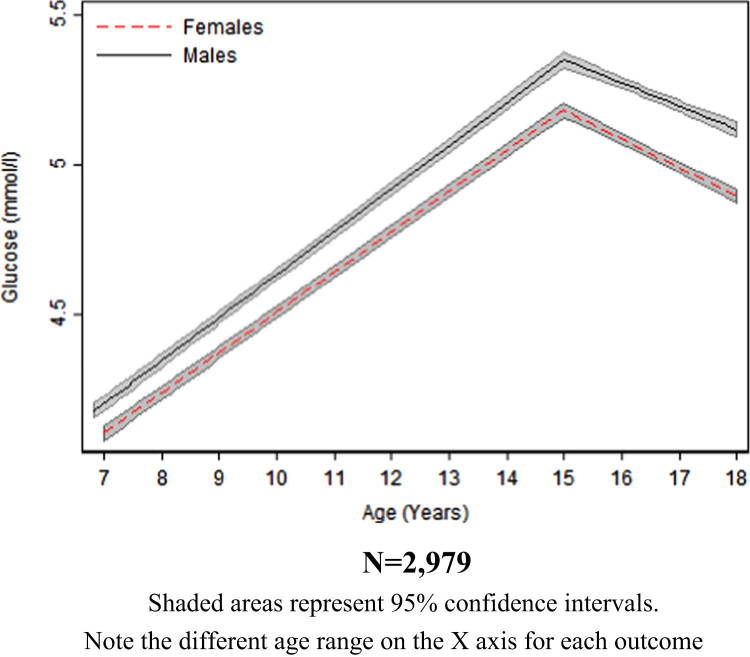
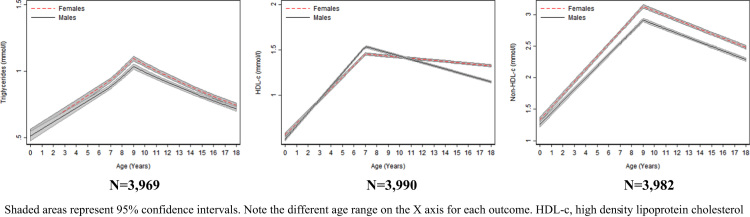
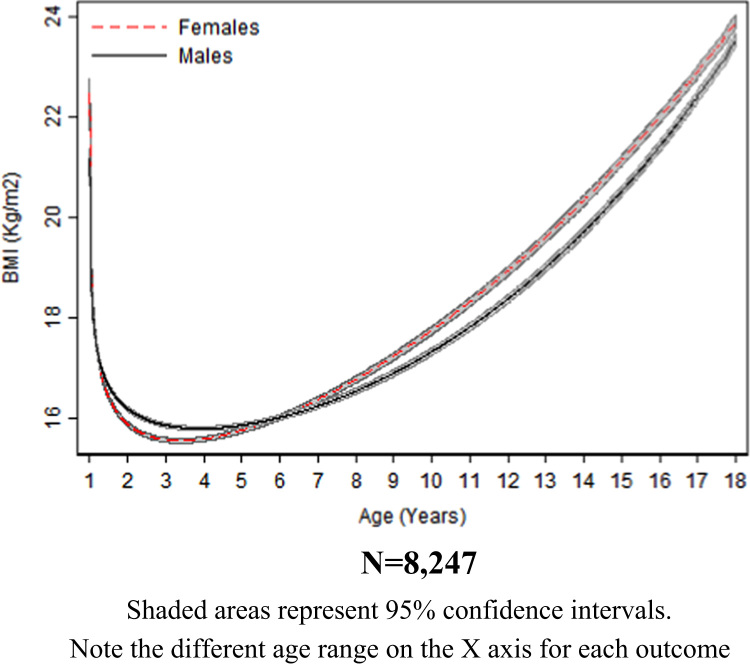
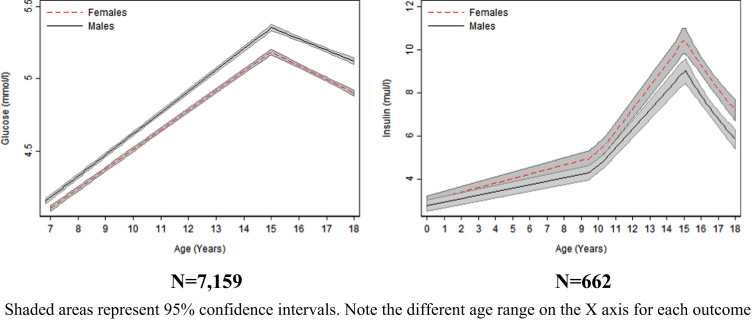
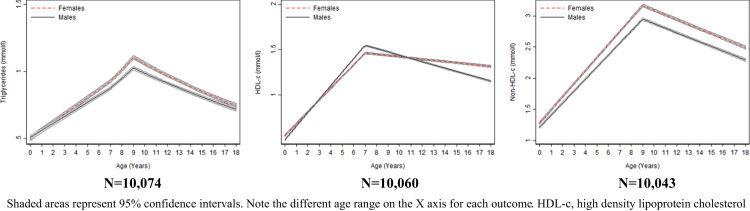
We derived appropriate powers of height adjustment for DXA-determined fat and lean mass which were age and sex-specific and included these in multilevel models (Table 1). Observed and predicted measurements for models are shown in Table 2, Table 3, Table 4, Table 5, Table 6, Table 7, Table 8, Table 9, Table 10, Table 11, Table 12. We examined the characteristics of mothers of participants included in the analysis of insulin (outcome measured on the fewest participants and with fewest repeated measures) compared with mothers of participants excluded from our analysis (Table 13). The mean sex-specific trajectories of measures of cardiovascular health are shown in Table 14, Table 15, Table 16, Table 17. We also regressed the observed risk factor at the first occasion of measurement and last occasion of measurement (18 years) on sex to examine whether sex differences estimated from the multilevel model at these ages were comparable to the observed data (Table 18). We restricted the sample for each risk factor to those with at least one measure before and one after the 11-year clinic, to examine whether results from the main analysis were driven by participants with only a single pre- or post-puberty measure (Fig. 1, Fig. 2, Fig. 3, Fig. 4). We repeated analyses of BMI restricted to participants with more than six measures to examine if results were driven by participants with a greater number of measures (Fig. 5). We also repeated analyses excluding the observations of participants at the 15- and 18-year clinics who reported eating in the four hours preceding these clinics to examine if our results were altered by the inclusion of some non-fasted bloods (Fig. 6, Fig. 7). Glucose at age 15 and 18 from the NMR platform was compared with glucose from standard clinical chemistry assays at these ages to examine the comparability of NMR and clinical chemistry measures (Table 19).
Table 1.
Age and sex-specific powers of height included in multilevel models of fat mass and lean mass
| Fat mass | Lean mass | |
|---|---|---|
| Females | ||
| Overall | ||
| Age 9 | Height^5.2 | Height^2.3 |
| Age 11 | Height^4.2 | Height^2.6 |
| Age 13 | Height^3 | Height^2 |
| Age 15 | Height^2.4 | Height^1.8 |
| Age 18 | Height^1.8 | Height^1.8 |
| Males | ||
| Overall | ||
| Age 9 | Height^6.6 | Height^2.1 |
| Age 11 | Height^5.4 | Height^2.4 |
| Age 13 | Height^2 | Height^2.8 |
| Age 15 | Height^2.4 | Height^2.4 |
| Age 18 | Height^1.9 | Height^1.8 |
Table 2.
Model details for log BMI trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed BMI, log BMI in kg/m2 (SD) | Mean predicted BMI, log BMI in kg/m2 (SD) | Mean difference (observed – predicted), log BMI in kg/m2 | 95% level of agreement between observed and predicted, log BMI in kg/m2 | |
| Females | ||||||
| Overall | 56,103 | 6815 | ||||
| 1–3 years | 9995 | 5288 | 2.82 (0.09) | 2.81 (0.07) | 0.01 | -0.10 to 0.11 |
| 3–7 years | 12,435 | 5631 | 2.77 (0.11) | 2.77 (0.08) | -0.002 | -0.15 to 0.15 |
| 7–9 years | 7114 | 4209 | 2.81 (0.13) | 2.82 (0.13) | -0.01 | -0.08 to 0.06 |
| 9–11 years | 8170 | 4184 | 2.88 (0.16) | 2.88 (0.15) | -0.001 | -0.08 to 0.08 |
| 11–13 years | 6681 | 3852 | 2.96 (0.17) | 2.95 (0.16) | 0.01 | -0.07 to 0.10 |
| 13–15 years | 6036 | 3742 | 3.00 (0.16) | 3.00 (0.16) | 0.01 | -0.11 to 0.12 |
| 15–18 years | 5672 | 3474 | 3.10 (0.17) | 3.11 (0.16) | -0.01 | -0.11 to 0.08 |
| Males | ||||||
| Overall | 56,665 | 7170 | ||||
| 1–3 years | 10,884 | 5629 | 2.84 (0.09) | 2.83 (0.07) | 0.01 | -0.10 to 0.11 |
| 3–7 years | 13,470 | 5987 | 2.78 (0.10) | 2.78 (0.07) | -0.004 | -0.14 to 0.14 |
| 7–9 years | 7247 | 4342 | 2.79 (0.12) | 2.80 (0.11) | -0.01 | -0.08 to 0.06 |
| 9–11 years | 7986 | 4120 | 2.86 (0.15) | 2.86 (0.14) | 0.003 | -0.07 to 0.08 |
| 11–13 years | 6398 | 3756 | 2.93 (0.17) | 2.92 (0.15) | 0.01 | -0.06 to 0.09 |
| 13–15 years | 5895 | 3686 | 2.97 (0.16) | 2.97 (0.16) | 0.001 | -0.11 to 0.11 |
| 15–18 years | 4785 | 2991 | 3.07 (0.16) | 3.08 (0.16) | -0.01 | -0.10 to 0.07 |
Table 3.
Model details for log fat mass trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed (SD), log fat mass in kg | Mean predicted (SD), log fat mass in kg | Mean difference (observed – predicted), log fat mass in kg | 95% level of agreement between observed and predicted, ln log fat mass in kg | |
| Females | ||||||
| Overall | 15,619 | 4461 | ||||
| 9 years | 3664 | 3664 | 2.14 (0.51) | 2.15 (0.48) | -0.003 | -0.15 to 0.14 |
| 9–13 years | 7204 | 4135 | 2.29 (0.52) | 2.29 (0.50) | 0.002 | -0.17 to 0.17 |
| 13–15 years | 3085 | 3056 | 2.69 (0.44) | 2.70 (0.42) | -0.01 | -0.21 to 0.19 |
| 15–18 years | 5330 | 3305 | 2.92 (0.41) | 2.92 (0.38) | 0.002 | -0.15 to 0.16 |
| Males | ||||||
| Overall | 14,524 | 4341 | ||||
| 9 years | 3577 | 3577 | 1.81 (0.60) | 1.82 (0.55) | -0.01 | -0.21 to 0.19 |
| 9–13 years | 7005 | 4055 | 1.98 (0.62) | 1.97 (0.58) | 0.01 | -0.22 to 0.24 |
| 13–15 years | 2964 | 2949 | 2.20 (0.62) | 2.23 (0.58) | -0.03 | -0.33 to 0.27 |
| 15–18 years | 4555 | 2870 | 2.31 (0.64) | 2.31 (0.60) | 0.01 | -0.22 to 0.23 |
Table 4.
Model details for lean mass trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed (SD), kg | Mean predicted (SD), kg | Mean difference (observed – predicted), kg | 95% level of agreement between observed and predicted, kg | |
| Females | ||||||
| Overall | 15,680 | 4474 | ||||
| 9 years | 3675 | 3675 | 23.66 (3.19) | 23.65 (3.03) | 0.01 | -2.12 to 2.15 |
| 9–13 years | 7228 | 4148 | 26.46 (4.82) | 26.49 (4.55) | -0.03 | -2.16 to 2.10 |
| 13–15 years | 3097 | 3068 | 35.21 (4.04) | 35.08 (3.91) | 0.13 | -2.11 to 2.36 |
| 15–18 years | 5355 | 3319 | 37.52 (4.17) | 37.56 (3.86) | -0.03 | -1.75 to 1.68 |
| Males | ||||||
| Overall | 14,540 | 4344 | ||||
| 9 years | 3586 | 3586 | 25.51 (2.98) | 25.55 (2.43) | -0.04 | -3.02 to 2.94 |
| 9–13 years | 7010 | 4057 | 27.78 (4.31) | 27.75 (4.02) | 0.03 | -2.71 to 2.77 |
| 13–15 years | 2964 | 2949 | 40.90 (7.16) | 41.04 (6.28) | -0.14 | -3.57 to 3.28 |
| 15–18 years | 4564 | 2874 | 52.25 (7.09) | 52.20 (6.88) | 0.05 | -2.18 to 2.28 |
Table 5.
Model details for SBP trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed (SD), mmHg | Mean predicted (SD), mmHg | Mean difference (observed – predicted), mmHg | 95% level of agreement between observed and predicted, mmHg | |
| Females | ||||||
| Overall | 23,731 | 4957 | ||||
| 7 years | 3967 | 3967 | 99.06 (9.27) | 98.93 (5.49) | 0.14 | -10.91 to 11.19 |
| 7–12 years | 14,696 | 4706 | 102.96 (9.73) | 103.10 (6.30) | -0.14 | -12.01 to 11.73 |
| 12–16 years | 6228 | 3671 | 114.67 (10.95) | 114.17 (7.72) | 0.50 | -11.16 to 12.17 |
| 16–18 years | 2807 | 2702 | 112.59 (8.53) | 112.95 (5.46) | -0.36 | -12.75 to 12.03 |
| Males | ||||||
| Overall | 22,590 | 4965 | ||||
| 7 years | 4090 | 4090 | 98.83 (9.06) | 98.75 (5.33) | 0.08 | -10.49 to 10.65 |
| 7–12 years | 14,497 | 4769 | 102.35 (9.34) | 102.46 (6.06) | -0.11 | -11.50 to 11.28 |
| 12–16 years | 5894 | 3532 | 116.82 (12.36) | 116.42 (9.59) | 0.40 | -11.42 to 12.21 |
| 16–18 years | 2199 | 2139 | 122.27 (9.42) | 122.59 (5.81) | -0.32 | -12.21 to 11.58 |
SBP; systolic blood pressure.
Table 6.
Model details for DBP trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed (SD), mmHg | Mean predicted (SD), mmHg | Mean difference (observed – predicted), mmHg | 95% level of agreement between observed and predicted, mmHg | |
| Females | ||||||
| Overall | 23,731 | 4957 | ||||
| 7 years | 3967 | 3967 | 56.86 (6.57) | 57.07 (3.27) | -0.21 | -9.04 to 8.63 |
| 7–12 years | 14,696 | 4706 | 58.51 (6.99) | 58.10 (3.58) | 0.41 | -9.81 to 10.64 |
| 12–16 years | 6228 | 3671 | 61.00 (9.23) | 61.84 (4.69) | -0.84 | -12.43 to 10.75 |
| 16–18 years | 2807 | 2702 | 64.87 (5.98) | 65.17 (3.43) | -0.29 | -13.17 to 12.58 |
| Males | ||||||
| Overall | 22,589 | 4965 | ||||
| 7 years | 4090 | 4090 | 56.09 (6.66) | 56.32 (3.46) | -0.24 | -8.87 to 8.40 |
| 7–12 years | 14,497 | 4769 | 57.68 (6.89) | 57.27 (3.62) | 0.41 | -9.45 to 10.27 |
| 12–16 years | 5894 | 3532 | 61.16 (9.91) | 62.05 (5.49) | -0.89 | -12.36 to 10.58 |
| 16–18 years | 2199 | 2139 | 63.47 (6.19) | 63.85 (3.66) | -0.37 | -12.78 to 12.03 |
DBP; diastolic blood pressure.
Table 7.
Model details for pulse rate trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed (SD), bpm | Mean predicted (SD), bpm | Mean difference (observed – predicted), bpm | 95% level of agreement between observed and predicted, bpm | |
| Females | ||||||
| Overall | 23,731 | 4957 | ||||
| 7 years | 3967 | 3967 | 84.39 (10.69) | 84.64 (5.97) | -0.25 | -13.65 to 13.16 |
| 7–12 years | 14,696 | 4706 | 79.49 (11.37) | 79.28 (7.26) | 0.21 | -13.94 to 14.36 |
| 12–16 years | 6228 | 3671 | 75.99 (11.06) | 76.37 (6.34) | -0.37 | -14.66 to 13.91 |
| 16–18 years | 2807 | 2702 | 67.96 (10.07) | 68.24 (5.97) | -0.29 | -14.98 to 14.41 |
| Males | ||||||
| Overall | 22,590 | 4965 | ||||
| 7 years | 4090 | 4090 | 81.78 (10.59) | 81.61 (6.04) | 0.18 | -12.38 to 12.73 |
| 7–12 years | 14,497 | 4769 | 75.79 (11.49) | 75.84 (7.73) | -0.05 | -13.41 to 13.31 |
| 12–16 years | 5894 | 3532 | 72.00 (11.11) | 71.78 (6.74) | 0.22 | -13.20 to 13.64 |
| 16–18 years | 2199 | 2139 | 63.12 (9.60) | 63.37 (5.56) | -0.25 | -14.55 to 14.05 |
bpm, beats per minute.
Table 8.
Model details for glucose trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed, mmol/l (SD) | Mean predicted, mmol/l (SD) | Mean difference (observed – predicted), mmol/l | 95% level of agreement between observed and predicted, mmol/l | |
| Females | ||||||
| Overall | 6519 | 3594 | ||||
| 7 years | 2646 | 2646 | 4.14 (0.50) | 4.17 (0.24) | -0.03 | -0.56 to 0.49 |
| 7–15 years | 3070 | 2751 | 4.24 (0.54) | 4.23 (0.28) | 0.01 | -0.56 to 0.58 |
| 15–18 years | 3449 | 2347 | 5.02 (0.37) | 5.03 (0.14) | -0.01 | -0.60 to 0.58 |
| Males | ||||||
| Overall | 6533 | 3661 | ||||
| 7 years | 2834 | 2834 | 4.22 (0.50) | 4.26 (0.21) | -0.04 | -0.63 to 0.56 |
| 7–15 years | 3290 | 2941 | 4.33 (0.55) | 4.32 (0.26) | 0.01 | -0.62 to 0.64 |
| 15–18 years | 3243 | 2191 | 5.22 (0.40) | 5.23 (0.13) | -0.01 | -0.64 to 0.62 |
Table 9.
Model details for log insulin trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed (SD), log insulin in mu/l | Mean predicted (SD), log insulin in mu/l | Mean difference (observed – predicted), log insulin in mu/l | 95% level of agreement between observed and predicted, ln log insulin in mu/l | |
| Females | ||||||
| Overall | 901 | 331 | ||||
| Birth | 135 | 135 | 1.10 (0.49) | 1.10 (0.26) | -0.000000001 | -0.46 to 0.46 |
| 0–9 years | 135 | 135 | 1.10 (0.49) | 1.10 (0.26) | -0.000000001 | -0.46 to 0.46 |
| 9–15 years | 271 | 270 | 1.66 (0.61) | 1.66 (0.43) | -0.002 | -0.37 to 0.36 |
| 15–18 years | 495 | 329 | 2.17 (0.48) | 2.16 (0.27) | 0.001 | -0.50 to 0.51 |
| Males | ||||||
| Overall | 930 | 331 | ||||
| Birth | 127 | 127 | 1.03 (0.52) | 1.03 (0.16) | -0.0000000002 | -0.73 to 0.73 |
| 9 years | 127 | 127 | 1.03 (0.52) | 1.03 (0.16) | -0.0000000002 | -0.73 to 0.73 |
| 9–15 years | 284 | 283 | 1.51 (0.61) | 1.51 (0.31) | -0.001 | -0.64 to 0.63 |
| 15–18 years | 519 | 330 | 1.99 (0.55) | 1.99 (0.26) | 0.0003 | -0.75 to 0.75 |
Table 10.
Model details for log triglyceride trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed (SD), log triglyceride in mmol/l | Mean predicted (SD), log triglyceride in mmol/l | Mean difference (observed – predicted), log triglyceride in mmol/l | 95% level of agreement between observed and predicted, log triglyceride in mmol/l | |
| Females | ||||||
| Overall | 10,927 | 4992 | ||||
| Birth | 2358 | 2358 | -0.69 (0.45) | -0.69 (0.23) | -0.004 | -0.45 to 0.44 |
| 0–9 years | 4915 | 4055 | -0.34 (0.55) | -0.35 (0.39) | 0.01 | -0.50 to 0.52 |
| 9–18 years | 6012 | 3333 | -0.12 (0.40) | -0.11 (0.22) | -0.01 | -0.53 to 0.52 |
| Males | ||||||
| Overall | 10,999 | 5136 | ||||
| Birth | 2412 | 2412 | -0.68 (0.45) | -0.68 (0.20) | -0.002 | -0.49 to 0.49 |
| 0–9 years | 5157 | 4294 | -0.36 (0.53) | -0.37 (0.35) | 0.003 | -0.54 to 0.55 |
| 9–18 years | 5842 | 3276 | -0.16 (0.42) | -0.16 (0.22) | -0.003 | -0.56 to 0.55 |
Table 11.
Model details for non-HDL-c trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed (SD), mmol/l | Mean predicted (SD), mmol/l | Mean difference (observed – predicted), mmol/l | 95% level of agreement between observed and predicted, mmol/l | |
| Females | ||||||
| Overall | 10,891 | 4979 | ||||
| Birth | 2279 | 2279 | 1.25 (0.53) | 1.28 (0.21) | -0.02 | -0.65 to 0.60 |
| 0–9 years | 4856 | 4031 | 2.17 (1.05) | 2.12 (0.86) | 0.06 | -0.58 to 0.69 |
| 9–18 years | 6035 | 3337 | 2.74 (0.68) | 2.79 (0.52) | -0.04 | -0.66 to 0.57 |
| Males | ||||||
| Overall | 10,983 | 5119 | ||||
| Birth | 2341 | 2341 | 1.18 (0.52) | 1.20 (0.26) | -0.02 | -0.53 to 0.49 |
| 0–9 years | 5096 | 4264 | 2.05 (0.98) | 2.00 (0.81) | 0.05 | -0.51 to 0.60 |
| 9–18 years | 5887 | 3294 | 2.55 (0.64) | 2.59 (0.52) | -0.04 | -0.58 to 0.51 |
HDL-c, high density lipoprotein cholesterol
Table 12.
Model details for HDL-c trajectories by sex
|
No of contributing individuals |
Assessment of model fit |
|||||
|---|---|---|---|---|---|---|
| Total number of observations | Number of individuals with 1 measure | Mean observed (SD), mmol/l | Mean predicted (SD), mmol/l | Mean difference (observed – predicted), mmol/l | 95% level of agreement between observed and predicted, mmol/l | |
| Females | ||||||
| Overall | 10,939 | 4988 | ||||
| Birth | 2320 | 2320 | 0.55 (0.24) | 0.55 (0.11) | -0.00000002 | -0.27 to 0.27 |
| 0–7 years | 2321 | 2321 | 0.55 (0.25) | 0.55 (0.11) | 0.00003 | -0.27 to 0.27 |
| 7–18 years | 8618 | 3957 | 1.40 (0.31) | 1.40 (0.22) | -0.00001 | -0.28 to 0.28 |
| Males | ||||||
| Overall | 11,019 | 5127 | ||||
| Birth | 2380 | 2380 | 0.50 (0.23) | 0.50 (0.12) | -0.000001 | -0.23 to 0.23 |
| 0–7 years | 2381 | 2381 | 0.50 (0.23) | 0.50 (0.12) | 0.00005 | -0.23 to 0.23 |
| 7–18 years | 8638 | 4014 | 1.38 (0.32) | 1.38 (0.26) | -0.00001 | -0.25 to 0.25 |
HDL-c, high density lipoprotein cholesterol
Table 13.
Characteristics at birth of the mothers of children included in models of insulin (risk factor with least individuals and number of repeated measures)
|
Participants included n= 662a |
Participants excluded n=19,388b |
Pvalue for comparisonc |
|
|---|---|---|---|
| n (%) | n (%) | ||
| Sex of child | |||
| Male | 331(50.0) | 9746(51.8) | 0.355 |
| Female | 331(50.0) | 9059(48.2) | |
| Maternal marital status | |||
| Never married | 74(11.4) | 2525(19.6) | <0.001 |
| Widowed | <0.8d(<5d) | 18(0.1) | |
| Divorced | 19(2.9) | 560(4.3) | |
| Separated | 9(1.4) | 210(1.6) | |
| 1st Marriage | 512(78.6) | 8752(67.8) | |
| Marriage 2 or 3 | 37(5.7) | 848(6.6) | |
| Household social class | |||
| Professional | 115(18.6) | 1426(13.0) | <0.001 |
| Managerial & Technical | 287(46.5) | 4552(41.5) | |
| Non-Manual | 141(22.9) | 2807(25.6) | |
| Manual | 51(8.3) | 1513(13.8) | |
| Part Skilled & Unskilled | 23(3.7) | 670(6.1) | |
| Maternal education | |||
| Less than O level | 101(15.5) | 3655(30.8) | <0.001 |
| O level | 224(34.4) | 4105(34.6) | |
| A level | 199(30.6) | 2605(22.0) | |
| Degree or above | 127(19.5) | 1483(12.5) | |
| Partners highest educational qualification | |||
| Less than O level | 138(21.7) | 4016(35.3) | <0.001 |
| O level | 140(22.0) | 2416(21.2) | |
| A level | 193(30.3) | 2930(25.7) | |
| Degree or Above | 166(26.1) | 2018(17.7) | |
| Maternal smoking during pregnancy | |||
| Yes | 557(85.3) | 9440(74.3) | <0.001 |
| No | 96(14.7) | 3271(25.7) | |
| Mean (SD) | Mean (SD) | Pvalue | |
| Child gestational age at birth | 40(1.55) | 38(5.62) | <0.001 |
Denominators for included participants in this table may be less than N included in full multilevel model due to missing data for these characteristics at baseline which were not required for our model (age, sex and at least one measure of risk factor before and after age 11 years were required for inclusion). b Denominator for participants excluded may also vary due to missing data on the characteristics included in the table.
P value is for the difference in proportions for categorical variables from χ2 test or difference in means for continuous variables from t tests between included and excluded participants. d May include zero.
Table 14.
Mean sex-specific trajectories of anthropometric risk factors estimated from multilevel models
| Mean trajectory (95% CI) in females | Mean trajectory (95% CI) in males | Mean difference in trajectory (95% CI) comparing females with males | Pvalue for difference between females and males | |
|---|---|---|---|---|
| Log BMIa | ||||
| Age 1 yr (log BMI, kg/m2) | 2.90 (2.89,2.90) | 2.89 (2.89,2.90) | 0.59% (-0.06,1.23)b | 0.077 |
| Age 3 yr (log BMI, kg/m2) | 2.75 (2.75,2.75) | 2.77 (2.77,2.77) | -1.86% (-2.22, -1.49)b | <0.001 |
| Age 7 yr (log BMI, kg/m2) | 2.80 (2.80,2.80) | 2.79 (2.79,2.79) | 0.88% (0.46,1.31)b | <0.001 |
| Age 9 yr (log BMI, kg/m2) | 2.85 (2.85,2.85) | 2.83 (2.83,2.83) | 2.12% (1.61,2.65)b | <0.001 |
| Age 11 yr (log BMI, kg/m2) | 2.91 (2.91,2.91) | 2.88 (2.88,2.88) | 2.98% (2.38,3.58)b | <0.001 |
| Age 13 yr (log BMI, kg/m2) | 2.98 (2.97,2.98) | 2.95 (2.94,2.95) | 3.34% (2.69,3.98)b | <0.001 |
| Age 15 yr v kg/m2) | 3.06 (3.05,3.06) | 3.02 (3.02,3.03) | 3.14% (2.47,3.82)b | <0.001 |
| Age 18 yr (log BMI, kg/m2) | 3.14 (3.13,3.14) | 3.11 (3.11,3.12) | 2.35% (1.62,3.09b | <0.001 |
| Log height -adjusted fat mass | ||||
| Age 9 yr (log fat mass, kg) | 2.01 (1.99,2.03) | 1.77 (1.74,1.79) | 27.3% (22.94,31.82)b | <0.001 |
| Change 9–13 yr (log fat mass, kg/yr) | 0.16 (0.15,0.16) | 0.13 (0.12,0.14) | 3.02%/yr (1.93,4.12)b | <0.001 |
| Change 13–15 yr (log fat mass, kg/yr) | 0.10 (0.09,0.11) | -0.06 (-0.07, -0.05) | 17.85%/yr (16.56,19.16)b | <0.001 |
| Change 15–18 yr (log fat mass, kg/yr) | 0.06 (0.05,0.06) | 0.10 (0.09,0.10) | -3.71%/yr (-4.44, -2.98)b | <0.001 |
| Age 18 yr (log fat mass, kg) | 3.01 (3.00,3.03) | 2.44 (2.42,2.46) | 77.8% (72.98,82.77)b | <0.001 |
| Height-adjusted lean mass | ||||
| Age 9 yr (kg) | 20.78 (20.69,20.88) | 23.97 (23.86,24.09) | -3.19 kg (-3.34, -3.04) | <0.001 |
| Change 9–13 yr (kg/yr) | 3.25 (3.22,3.28) | 2.32 (2.26,2.38) | 0.93 kg/yr (0.86,1.00) | <0.001 |
| Change 13–15 yr (kg/yr) | 1.52 (1.44,1.61) | 7.62 (7.53,7.70) | -6.09 kg/yr (-6.21, -5.97) | <0.001 |
| Change 15–18 yr (kg/yr) | 0.41 (0.37,0.44) | 2.51 (2.44,2.59) | -2.11 kg/yr (-2.19, -2.02) | <0.001 |
| Age 18 yr (kg) | 37.64 (37.50,37.77) | 56.03 (55.80,56.26) | -18.39 kg (-18.66, -18.12) | <0.001 |
BMI is modelled using fractional polynomials. For ease of interpretation, the predicted log BMI for females and males is shown at each age rather than the coefficients for the fractional polynomial terms from the model.
The difference between females and males for BMI and fat mass is back transformed from the log scale for ease of interpretation and is interpreted as the percentage difference in the mean level comparing females with males or percentage difference in change per year comparing females with males.
Table 15.
Mean sex-specific trajectories of blood pressure and pulse rate estimated from multilevel models
| Mean trajectory (95% CI) in females | Mean trajectory (95% CI) in males | Mean difference in trajectory (95% CI) comparing females with males | Pvalue for difference between females and males | |
|---|---|---|---|---|
| SBP | ||||
| Age 7 yr (mmHg) | 98.14 (97.84,98.43) | 98.00 (97.72,98.28) | 0.14 (-0.27,0.55) | 0.497 |
| Change 7–12 yr (mmHg/yr) | 1.85 (1.78,1.92) | 1.64 (1.57,1.70) | 0.22 (0.12,0.32) | <0.001 |
| Change 12–16 yr (mmHg/yr) | 3.82 (3.70,3.94) | 5.78 (5.66,5.90) | -1.97 (-2.13,-1.80) | <0.001 |
| Change 16–18 yr (mmHg/yr) | -5.74 (-6.00,-5.49) | -3.82 (-4.09,-3.54) | -1.93 (-2.30,-1.56) | <0.001 |
| Age 18 yr (mmHg) | 111.18 (110.86,111.51) | 121.67 (121.27,122.07) | -10.48 (-11.00,-9.97) | <0.001 |
| DBP | ||||
| Age 7 yr (mmHg) | 57.13 (56.92,57.34) | 56.34 (56.13,56.54) | 0.79 (0.50,1.09) | <0.001 |
| Change 7–12 yr (mmHg/yr) | 0.09 (0.03,0.14) | 0.14 (0.08,0.19) | -0.05 (-0.12,0.03) | 0.247 |
| Change 12–16 yr (mmHg/yr) | 2.34 (2.24,2.44) | 2.81 (2.70,2.92) | -0.47 (-0.62,-0.32) | <0.001 |
| Change 16–18 yr (mmHg/yr) | -1.01 (-1.21,-0.80) | -2.49 (-2.73,-2.25) | 1.49 (1.17,1.81) | <0.001 |
| Age 18 yr (mmHg) | 64.91 (64.67,65.16) | 63.26 (62.98,63.55) | 1.65 (1.27,2.02) | <0.001 |
| Pulse rate | ||||
| Age 7 yr (bpm) | 85.77 (85.43,86.11) | 82.71 (82.38,83.04) | 3.06 (2.58,3.54) | <0.001 |
| Change 7–12 yr (bpm/yr) | -1.77 (-1.86,-1.69) | -1.89 (-1.97,-1.81) | 0.11 (0.00,0.23) | 0.053 |
| Change 12–16 yr (bpm/yr) | -0.17 (-0.30,-0.05) | -0.76 (-0.89,-0.63) | 0.59 (0.41,0.77) | <0.001 |
| Change 16–18 yr (bpm/yr) | -4.73 (-5.00,-4.46) | -4.08 (-4.36,-3.79) | -0.65 (-1.04,-0.27) | <0.001 |
| Age 18 yr (bpm) | 66.75 (66.37,67.13) | 62.07 (61.66,62.48) | 4.68 (4.12,5.24) | <0.001 |
bpm, beats per minute; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Table 16.
Mean sex-specific trajectories of glucose and log insulin estimated from multilevel models
| Mean trajectory (95% CI) in females | Mean trajectory (95% CI) in males | Mean difference in trajectory (95% CI) comparing females with males | Pvalue for difference between females and males | |
|---|---|---|---|---|
| Glucose | ||||
| Age 7 yr (mmol/l) | 4.11 (4.09,4.13) | 4.18 (4.16,4.20) | -0.08 mmol/l (-0.10,-0.05) | <0.001 |
| Change 7–15 yr (mmol/l/yr) | 0.13 (0.13,0.14) | 0.15 (0.14,0.15) | -0.01 mmol/l/yr (-0.02,-0.01) | <0.001 |
| Change 15–18 yr (mmol/l/yr) | -0.09 (-0.10,-0.08) | -0.08 (-0.09,-0.07) | -0.02 mmol/l/yr (-0.03, 0.00) | 0.023 |
| Age 18 yr (mmol/l) | 4.90 (4.88,4.92) | 5.12 (5.10,5.14) | -0.22 mmol/l (-0.25, -0.19) | <0.001 |
| Log insulin | ||||
| Birth (log insulin, mu/l) | 1.10 (1.01,1.18) | 1.02 (0.93,1.11) | 7.81% (-4.46,21.65)a | 0.223 |
| Change 0–9 yr (log insulin, mu/l /yr) | 0.05 (0.04,0.06) | 0.04 (0.03,0.06) | 0.67%/yr (-1.19,2.56)a | 0.486 |
| Change 9–15 yr (log insulin, mu/l /yr) | 0.14 (0.12,0.15) | 0.14 (0.12,0.15) | 0.11%/yr (-2.24,2.52)a | 0.928 |
| Change 15–18 yr (log insulin, mu/l /yr) | -0.13 (-0.16, -0.09) | -0.15 (-0.18, -0.11) | 2.17%/yr (-2.52,7.08)a | 0.371 |
| Age 18 yr (log insulin, mu/l) | 1.97 (1.91,2.05) | 1.77 (1.69,1.84) | 22.85% (10.76,36.35)a | 0.000 |
The difference between females and males is back transformed from the log scale for ease of interpretation and is interpreted as the percentage difference in the mean level comparing females with males or percentage difference in change per year comparing females with males.
Table 17.
Mean sex-specific trajectories of log triglyceride and cholesterol estimated from multilevel models
| Mean trajectory (95% CI) in females | Mean trajectory (95% CI) in males | Mean difference in trajectory (95% CI) comparing females with males | Pvalue for difference between females and males | |
|---|---|---|---|---|
| Log triglyceride | ||||
| Birth (log triglyceride, mmol/l) | -0.69 (-0.70,-0.67) | -0.68 (-0.70,-0.66) | -0.70% (-3.17,1.84)a | 0.586 |
| Change 0–9 yr (log triglyceride, mmol/l/yr) | 0.09 (0.08,0.09) | 0.08 (0.08,0.08) | 0.90%/yr (0.53,1.28)a | <0.001 |
| Change 9–18 yr (log triglyceride, mmol/l/yr) | -0.04 (-0.05,-0.04) | -0.04 (-0.04,-0.04) | -0.41%/yr (-0.72,-0.09)a | 0.012 |
| Age 18 yr (log triglyceride, mmol/l) | -0.29 (-0.31,-0.28) | -0.33 (-0.35,-0.31) | 3.80% (1.59,6.06)a | 0.001 |
| HDL-c | ||||
| Birth (mmol/l) | 0.55 (0.54,0.56) | 0.50 (0.49,0.51) | 0.05 mmol/l (0.03,0.06) | <0.001 |
| Change 0–7 yr (mmol/l/yr) | 0.13 (0.13,0.13) | 0.15 (0.15,0.15) | -0.02 mmol/l/yr (-0.02,-0.02) | <0.001 |
| Change 7–18 yr (mmol/l/yr) | -0.01 (-0.01,-0.01) | -0.04 (-0.04,-0.03) | 0.02 mmol/l/yr (0.02,0.02) | <0.001 |
| Age 18 yr (mmol/l) | 1.32 (1.31,1.33) | 1.15 (1.14,1.16) | 0.17 mmol/l (0.15,0.18) | <0.001 |
| Non-HDL-c | ||||
| Birth (mmol/l) | 1.28 (1.26,1.30) | 1.22 (1.19,1.24) | 0.07 mmol/l (0.04,0.10) | <0.001 |
| Change 0–9 yr (mmol/l/yr) | 0.21 (0.21,0.21) | 0.19 (0.19,0.20) | 0.02 mmol/l/yr (0.01,0.02) | <0.001 |
| Change 9–18 yr (mmol/l/yr) | -0.07 (-0.08,-0.07) | -0.07 (-0.08,-0.07) | 0.00 mmol/l/yr (-0.01,0.00) | 0.265 |
| Age 18 yr (mmol/l) | 2.49 (2.46,2.52) | 2.30 (2.27,2.32) | 0.19 mmol/l (0.16,0.23) | <0.001 |
HDL-c, high density lipoprotein cholesterol
The difference between females and males is back transformed from the log scale for ease of interpretation and is interpreted as the percentage difference in the mean level comparing females with males or percentage difference in change per year comparing females with males.
Tablee 18.
Sex differences in risk factors at first and last available measure from linear regressions compared to differences predicted from multilevel models
| N participants in regression of risk factor on sex at each age | Difference in females compared with males from regression (95% CI) | Difference in females compared with males from multilevel model (95% CI) | |
|---|---|---|---|
| Log BMI (kg/m2)a | |||
| Age 1 | 1060 | -1.64(-2.60,-0.68) | 0.59 (-0.05,1.24) |
| Age 18 | 995 | 2.31(0.03,4.59) | 2.35 (1.62,3.09) |
| Log fat mass (kg)a | |||
| Age 9 | 7241 | 39.53(35.98,43.08) | 27.30 (22.94,31.82) |
| Age 18 | 4804 | 75.42(70.21,80.63) | 77.80 (72.98,82.77) |
| Lean mass (kg) | |||
| Age 9 | 7261 | -1.85(-1.99,-1.71) | -3.19 (-3.34,-3.04) |
| Age 18 | 4819 | -17.14(-17.44,-16.84) | -18.39 (-18.66,-18.12) |
| SBP (mmHg) | |||
| Age 7 | 8057 | 0.23(-0.17,0.63) | 0.14 (-0.27,0.55) |
| Age 18 | 4629 | -10.17(-10.66,-9.68) | -10.48 (-11.00,-9.97) |
| DBP (mmHg) | |||
| Age 7 | 8057 | 0.77(0.48,1.06) | 0.79 (0.50,1.09) |
| Age 18 | 4629 | 1.55(1.22,1.88) | 1.65 (1.27,2.02) |
| Pulse rate (bpm) | |||
| Age 7 | 8057 | 2.61(2.14,3.07) | 3.06 (2.58,3.54) |
| Age 18 | 4629 | 4.53(3.99,5.07) | 4.68 (4.12,5.24) |
| Glucose (mmol/l) | |||
| Age 7 | 5480 | -0.08(-0.11,-0.05) | -0.08 (-0.10,-0.05) |
| Age 18 | 3266 | -0.23(-0.26,-0.21) | -0.22 (-0.25,-0.19) |
| Log insulin (mu/l)a | |||
| Birth | 262 | 7.80(-5.37,20.97) | 7.81 (-4.46,21.65) |
| Age 18 | 498 | 21.06(9.94,32.18) | 22.85 (10.76,36.25) |
| Log triglyceride (mmol/l)a | |||
| Birth | 4770 | -1.00(-3.53,1.53) | -0.70 (-3.17,1.84) |
| Age 18 | 3254 | 2.11(-0.41,4.63) | 3.80 (1.59,6.06) |
| HDL-c (mmol/l) | |||
| Birth | 4700 | 0.05(0.03,0.06) | 0.05 (0.03,0.06) |
| Age 18 | 3277 | 0.16(0.14,0.18) | 0.17 (0.15,0.18) |
| Non-HDL-c (mmol/l) | |||
| Birth | 4620 | 0.07(0.04,0.10) | 0.07 (0.04,0.10) |
| Age 18 | 3275 | 0.20(0.16,0.25) | 0.19 (0.16,0.23) |
bpm, beats per minute; DBP, diastolic blood pressure; HDL-c, high density lipoprotein; SBP, systolic blood pressure.
Risk factor is log transformed. The difference between females and males for the risk factor is back transformed from the log scale for ease of interpretation and is interpreted as the percentage difference in the mean level comparing females with males at the age shown.
Fig. 1.
Mean predicted sex-specific trajectories of BMI (1 to 18 years), height-adjusted fat mass and height-adjusted lean mass (9 to 18 years) among participants with at least one measure before and after 11 years.
Fig. 2.
Mean predicted sex-specific trajectories of SBP, DBP and pulse from 7 to 18 years among participants with at least one measure before and after 11 years.
Fig. 3.
Mean predicted sex-specific trajectories of glucose from 7 to 18 years among participants with at least one measure before and after 11 years.
Fig. 4.
Mean predicted sex-specific trajectories of triglyceride, HDL-c and non-HDL-c from birth to 18 years among participants with at least one measure before and after 11 years.
Fig. 5.
Mean predicted sex-specific trajectory of BMI from 1 to 18 years among participants with 6 or more measures.
Fig. 6.
Mean predicted sex-specific trajectories of glucose (7 - 18 years) and insulin (birth - 18 years) excluding participants who reported eating before either the 15- or 18-year clinic.
Fig. 7.
Mean predicted sex-specific trajectories of triglyceride, HDL-c and non-HDL-c from birth to 18 years excluding participants who reported eating before either the 15- or 18-year clinic.
Table 19.
Sex differences in glucose from main ALSPAC clinic compared with sex difference in glucose from NMR spectroscopy at 15- and 18-year clinic with females as reference group.
| N participants in regression of risk factor on sex at each age | Difference in females compared with males from main clinic (95% CI) | Difference in females compared with males from NMR spectroscopy (95% CI) | ||
|---|---|---|---|---|
| Age 15 | 3464 | -0.16 (-0.19, -0.14) | -0.14 (-0.16, -0.11) | |
| Age 18 | 3266 | -0.23 (-0.26, -0.21) | -0.17 (-0.20, -0.15) |
NMR, Nuclear Magnetic Resonance.
Acknowledgements
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses.
Financial support
The UK Medical Research Council and Wellcome (Grant ref: 102215/2/13/2) and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors listed and they will serve as guarantors for the contents of this paper. LMOK is supported by a UK Medical Research Council Population Health Scientist fellowship (MR/M014509/1). LDH and AF are supported by Career Development Awards from the UK Medical Research Council (grants MR/M020894/1 and MR/M009351/1, respectively). LMOK, AS, LDH, AF, KT, ELA, and DAL work in a unit that receives funds from the UK Medical Research Council (grant MC_UU_12013/5, MC_UU_12013/2, MC_UU_12013/9, MC_UU_00011/3, MC_UU_00011/6). AH received support from the British Heart Foundation (PG/15/75/31748, CS/15/6/31468, CS/13/1/30327), the Wellcome Trust (086676/7/08/Z), the National Institute for Health Research University College London Hospitals Biomedical Research Centre and works in a unit that receives funds from the UK Medical Research Council (Programme Code MC_UU_12019/1). All the funding sources had no role in the study design, collection, analysis, or interpretation of the data; writing the manuscript; or the decision to submit the paper for publication.
Author contributions
Author contributions for this project are detailed in Ref. [1].
Footnotes
Transparency data associated with this article can be found in the online version at doi:10.1016/j.dib.2019.01.035.
Transparency document. Supplementary material
Supplementary material
.
References
- 1.O’Keeffe L., Simpkin A., Tilling K., Anderson E., Hughes A., Lawlor D. Sex-specific trajectories of measures of cardiometabolic health during childhood and adolescence: a prospective cohort study. Atherosclerosis. 2018;278(2018):190–196. doi: 10.1016/j.atherosclerosis.2018.09.030. [DOI] [PubMed] [Google Scholar]
- 2.Boyd A., Golding J., Macleod J., Lawlor D.A., Fraser A., Henderson J. Cohort profile: the ‘Children of the 90s׳—the index offspring of the Avon Longitudinal Study of Parents and Children. Int. J. Epidemiol. 2013;42(1):111–127. doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fraser A., Macdonald-Wallis C., Tilling K., Boyd A., Golding J., Smith G.D. Cohort profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int. J. Epidemiol. 2013;42(1):97–110. doi: 10.1093/ije/dys066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.University of Bristol, Avon Longitudinal Study of Parents and Children [Available from: 〈http://www.bristol.ac.uk/alspac/researchers/access/〉, 2017.
- 5.Howe L.D., Tilling K., Matijasevich A., Petherick E.S., Santos A.C., Fairley L. Linear spline multilevel models for summarising childhood growth trajectories: a guide to their application using examples from five birth cohorts. Stat. Methods Med. Res. 2013 doi: 10.1177/0962280213503925. (0962280213503925) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howe L.D., Matijasevich A., Tilling K., Brion M.-J., Leary S.D., Smith G.D. Maternal smoking during pregnancy and offspring trajectories of height and adiposity: comparing maternal and paternal associations. Int. J. Epidemiol. 2012;41(3):722–732. doi: 10.1093/ije/dys025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Keeffe L.M., Kearney P.M., Greene R.A., Zuccolo L., Tilling K., Lawlor D.A. Maternal alcohol use during pregnancy and offspring trajectories of height and weight: a prospective cohort study. Drug Alcohol Depend. 2015;153:323–329. doi: 10.1016/j.drugalcdep.2015.02.035. [DOI] [PubMed] [Google Scholar]
- 8.Soininen P., Kangas A.J., Würtz P., Suna T., Ala-Korpela M. Quantitative serum nuclear magnetic resonance metabolomics in cardiovascular epidemiology and genetics. Circ.: Cardiovasc. Genet. 2015;8(1):192–206. doi: 10.1161/CIRCGENETICS.114.000216. [DOI] [PubMed] [Google Scholar]
- 9.Soininen P., Kangas A.J., Würtz P., Tukiainen T., Tynkkynen T., Laatikainen R. High-throughput serum NMR metabonomics for cost-effective holistic studies on systemic metabolism. Analyst. 2009;134(9):1781–1785. doi: 10.1039/b910205a. [DOI] [PubMed] [Google Scholar]
- 10.O׳Keeffe L.M., Howe L.D., Fraser A., Hughes A.D., Wade K.H., Anderson E.L. Associations of Y chromosomal haplogroups with cardiometabolic risk factors and subclinical vascular measures in males during childhood and adolescence. Atherosclerosis. 2018;274:94–103. doi: 10.1016/j.atherosclerosis.2018.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howe L.D., Parmar P.G., Paternoster L., Warrington N.M., Kemp J.P., Briollais L. Genetic influences on trajectories of systolic blood pressure across childhood and adolescence. Circ.: Cardiovasc. Genet. 2013;6(6):608–614. doi: 10.1161/CIRCGENETICS.113.000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Staley J.R., Bradley J., Silverwood R.J., Howe L.D., Tilling K., Lawlor D.A. Associations of blood pressure in pregnancy with offspring blood pressure trajectories during childhood and adolescence: findings from a prospective study. J. Am. Heart Assoc. 2015;4(5):e001422. doi: 10.1161/JAHA.114.001422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris T., Northstone K., Howe L. Examining the association between early life social adversity and BMI changes in childhood: a life course trajectory analysis. Pediatr. Obes. 2015 doi: 10.1111/ijpo.12063. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material