Abstract
BACKGROUND:
Number of reported cases of human dirofilariasis in the last couple of decades has been increasing. Dogs are the main reservoir hosts, while various mosquito species represent/serve as vectors. Human infections are caused by two different parasites: Dirofilaria immitis and Dirofilaria repens. Dirofilaria repens is currently considered to be one of the most rapidly-spreading human and animal parasite species in Europe. Clinical features are characterised by subcutaneous or ocular lesions which can persist for months without any symptoms. The disease is considered to be endemic in Mediterranean countries, central Asia, Israel, and Sri Lanka with increased incidence in Central and East Europe. Apart from the local population, tourists are also susceptible to this disease. Export of domestic animals can transfer parasites between different countries. This disease is rare in Croatia.
CASE PRESENTATION:
We are presenting a case of a 58-year-old female patient with dirofilariasis of the genital region caused by Dirofilaria repens, confirmed with PCR and sequencing.
CONCLUSION:
From the clinician point of view, subcutaneous dirofilariasis should be considered as a differential diagnosis in cases of long-lasting subcutaneous swellings.
Keywords: Human dirofilariasis, Subcutaneous dirofilariasis, Dirofilaria repens, Zoonoses, Croatia
Introduction
Members within the genus Dirofilaria, namely D. repens and D. immitis are zoonotic parasites transmitted by the different mosquito species. The number of reports on human dirofilariasis in a couple of last decades has been increasing across Europe and is considered to be one of the most extensively spreading human and animal parasite in Europe. Dogs are the most important reservoirs for infection with this species. Mosquitoes of the genus Aedes, Anopheles and Culex, serve as vectors of both parasites [1], [2], [3], [4]. Vector-borne diseases are usually transmitted to human by mosquitoes [1], [5]. Human infections caused mostly by D. repens are still overlooked, and usually represent unexpected finding, most frequently manifested as skin or subconjunctival infiltrates. Dirofilaria immitis infections are clinically characterised by solitary or multiple lung lesions which must be diagnostically evaluated for differential diagnosis as tumours; primary or metastatic [1], [3]. Clinical manifestations are characterised by subcutaneous or ocular lesions that can persist for months without any symptoms [1], [3], [6]. Subcutaneous nodules can occur in any part of the body but are most frequently detected on the face, neck, eyelid, chest, back, and scrotum [1], [3], [6]. Rarely, the parasite could be located/present in the buccal mucosa, liver, spermatic cord and abdomen [6], [7]. The disease is prevalent in tropic climates, with a tendency of spreading to moderate climate regions [2]. In Europe, the disease is considered to be endemic in Mediterranean countries with increasing incidence in Italy, France, Greece, and Spain [1], [3], [4], [5], [6]. Except in the Mediterranean region, the number of reported cases has been increasing in Central Europe [6], [8], [9]. Hungarian National Centre for Epidemiology recorded 13 cases of dirofilariasis from 1879 to 2000 and 88 cases from 2001 to 2013 [6], [10], [11]. In Croatia, the disease is still considered to be rare with sporadic occurrence [1], [3].
In the following paper, we present the case of 58-year-old woman with a subcutaneous node in the genital area caused by infection with D. repens.
Case Report
A 58-year-old female patient has been admitted to the gynaecology clinic in Zagreb, Croatia due to the presence of hard (firm), painless nodule in the pubis region, without a history of any serious disease. She did not travel in the last few months from her place of residence. Patient lives in a rural area in Zagreb County with a dog and other domestic animals near a forest, without springs of natural water nearby.
After the inspection and gynaecological examination, an enlarged lymph node was suspected. The ultrasonographic finding of the nodule appeared normal. For the next two weeks, “nodule” was followed up and since there were no visible changes, excision was proposed. During the excision, a seven-centimetre filarial worm was found and removed together with surrounding subcutaneous tissue. Histopathology revealed a worm-like parasite and based on morphological characteristics, D. repens infection was suspected (Figure 1).
Figure 1.
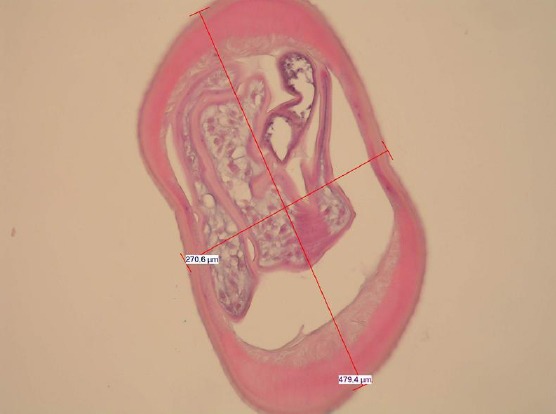
Histology of the worm suggested the diagnosis of Dirofilaria repens
The worm was surrounded by fibrous tissue infiltrated with lymphocytes and plasma cells associated with extensive eosinophil infiltration (Figure 2).
Figure 2.
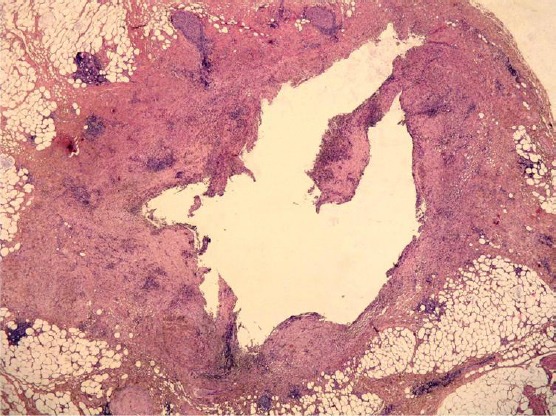
Low power magnification of the tissue that surrounded the warm
DNA was done using commercial Blood and Tissue Kit (QIAGEN) system according to manufacturer’s instructions. Molecular identification of the parasite was performed using DIDR-F1 (5’ – AGT GCG AAT TGC AGA CGC ATT GAG-3’) and DIDR-R1 (5’ – AGC GGG TAA TCA CGA CTG AGT TGA-3’) primers. Amplification was carried out according to the method developed by Rinshiw and coauthors [12]. Primers were used to amplify Internal transcribed spacer region 2 (ITS2) for D. immitis (542 bp), D. reconditum (578 bp) and D. repens (484 bp). The amplification products were analysed by capillary electrophoresis (QIAxcel System®, QIAGEN) and purified (ExoSAP-IT®, USB Corp., Cleveland, United States). The sequencing was performed by Macrogen Europe in both directions. The resulting sequences were assembled using the SeqMan program and edited with EditSeq (DNA Star). Obtained Sequence was compared to sequences in the GenBank database using BLAST. Blood with EDTA was collected from the patient and analysed with modified Knott’s method to exclude the possible presence of microfilariae. A search against the GenBank database using the BLAST algorithm revealed that the sequence with the highest similarity (99%) with the isolate from the dog (GenBank Accession No. AY693808). The patient was followed for the next two years, and no additional symptoms were noted.
Discussion
Dirofilaria is parasitic nematode of dogs that can infect humans accidentally via vectors. The first case described in the literature is by Babes in Hungary who described the parasite in 1879 [6].
D. repens is zoonotic nematode able to cause dirofilariasis in humans and is considered to be an emerging zoonosis. Some parasitic diseases are still neglected in “industrialised” world since they are considered to be tropical. Due to global changes including warming, animal trading and travelling, together with a change in vector ecology; evidence for their emerging are increasing. In the current paper, we are reporting an additional case of subcutaneous dirofilariasis in a female patient with a nodule in the pubic region, living in Central Croatia.
Subcutaneous dirofilariosis was suspected based on morphological characteristics of the worm after the parasite has been surgically removed. Worms belonging to the genus Dirofilaria are identified by their thick laminated cuticle, broad lateral ends and large muscle cells [1], [2]. D. repens was confirmed with sequencing which represents the first human sequence from Croatia. Exact identification of species may be possible only after studying the fully matured worm. Microfilaremia is absent in the case of human infection with D. repens as was the case in the current study [2]. Dirofilaria repens parasite enters the lymphatic system and forms local subcutaneous or subconjunctival lesions. Subcutaneous nodules are up to 1 cm in diameter, and the treatment is surgical removal similar to the presented case [1], [6].
In Croatia, similar to other European countries, number of reported cases has been increasing, however, the exact number of human infections with D. repens remains unknown [13], [14], [15], [16], [17], [18], [19], [20], [21], [22]. As of today, there is no obligation to report human dirofilariasis in Croatia. Global warming allows an increase in the mosquito population as well as the introduction of new species with the capacity to transmit both of Dirofilaria species [23]. The same part of increased incidence of the disease is due to better diagnostical modalities [1], [2], [6], [8].
In conclusion, to have accurate data on the incidence of the human dirofilariasis, all individual cases should be analysed with molecular methods for species confirmation. Better reporting system could be a helpful tool in providing answers on prevalence, distribution, and an actual increase in the number of occurrences, rather than an increase in some published cases.
From the clinician point of view, subcutaneous dirofilariasis should be considered as differential diagnosis in cases of long-lasting subcutaneous swellings.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Vicković N, Granić J, Desnica B, Makek N, Balen-Topić M. Subkutana dirofilarizoa - prikaz bolesnika. Infektološki glasnik. 2007;27:135–137. [Croatian] [Google Scholar]
- 2.Matějů J, Chanová M, Modrý D, Mitková B, Hrazdilová K, Žampachová V, Kolářová L. Dirofilaria repens:emergence of autochthonous human infections in the Czech Republic (case reports) BMC Infect Dis. 2016;16(1):171. doi: 10.1186/s12879-016-1505-3. https://doi.org/10.1186/s12879-016-1505-3 PMid:27094256 PMCid:PMC4837637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glavan N, Pećanić S, Bosak A, Gačanin L, Abram M, Jonjić N. Dirofilaria repens infection in a ten-year-old boy from the Istria Peninsula:case report. ActaClin Croat. 2013;52(4):533–6. PMid:24697007. [PubMed] [Google Scholar]
- 4.Pampiglione S, Rivasi F. Human dirofilariasis due to Dirofilaria (Nochtiella) repens:an update of world literature from 1995 to 2000. Parassitologia. 2000;42(3-4):231–54. PMid:11686084. [PubMed] [Google Scholar]
- 5.Pampiglione S, Rivasi F, Angeli G, Boldorini R, Incensati RM, Pastormerlo M, et al. Dirofilariasis due to Dirofilaria repens in Italy, an emergent zoonosis:report of 60 new cases. Histopathology. 2001;38(4):344–54. doi: 10.1046/j.1365-2559.2001.01099.x. https://doi.org/10.1046/j.1365-2559.2001.01099.x PMid:11318900. [DOI] [PubMed] [Google Scholar]
- 6.Dóczi I, Bereczki L, Gyetvai T, Fejes I, Skribek Á, Szabó Á, et al. Description of five dirofilariasis cases in South Hungary and review epidemiology of this disease for the country. Wien Klin Wochenschr. 2015;127(17-18):696–702. doi: 10.1007/s00508-015-0825-4. https://doi.org/10.1007/s00508-015-0825-4 PMid:26178869. [DOI] [PubMed] [Google Scholar]
- 7.Desai RS, Pai N, Nehete AP, Singh JS. Oral dirofilariasis. Indian J Med Microbiol. 2015;33(4):593–4. doi: 10.4103/0255-0857.167342. https://doi.org/10.4103/0255-0857.167342 PMid:26470974. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki J, Kobayashi S, Okata U, Matsuzaki H, Mori M, Chen KR, et al. Molecular analysis of Dirofilaria repens removed from a subcutaneous nodule in a Japanese woman after a tour to Europe. Parasite. 2015;22:2. doi: 10.1051/parasite/2015002. https://doi.org/10.1051/parasite/2015002 PMid:25619827 PMCid:PMC4306022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rudolf I, Šebesta O, Mendel J, Betášová L, Bocková E, Jedličková P, et al. Zoonotic Dirofilaria repens (Nematoda:Filarioidea) in Aedes vexans mosquitoes, Czech Republic. Parasitol Res. 2014;113(12):4663–7. doi: 10.1007/s00436-014-4191-3. https://doi.org/10.1007/s00436-014-4191-3 PMid:25346197. [DOI] [PubMed] [Google Scholar]
- 10.Szénási Z, Kovács AH, Pampiglione S, Fioravanti ML, Kucsera I, Tánczos B, et al. Human dirofilariosis in Hungary:an emerging zoonosis in central Europe. Wien Klin Wochenschr. 2008;120(3-4):96–102. doi: 10.1007/s00508-008-0928-2. https://doi.org/10.1007/s00508-008-0928-2 PMid:18322771. [DOI] [PubMed] [Google Scholar]
- 11.Miterpáková M, Iglódyová A, Čabanová V, Stloukal E, Miklisová D. Canine dirofilariosis endemic in Central Europe-10 years of epidemiological study in Slovakia. Parasitol Res. 2016 Mar 28; doi: 10.1007/s00436-016-4989-2. [Epub ahead of print] https://doi.org/10.1007/s00436-016-4989-2 PMid:27021185. [DOI] [PubMed] [Google Scholar]
- 12.Rishniw M, Barr SC, Simpson KW, Frongillo MF, Franz M, Dominguez Alpizar JL. Discrimination between six species of canine microfilariae by a single polymerase chain reaction. Vet Parasitol. 2006;135(3-4):303–14. doi: 10.1016/j.vetpar.2005.10.013. https://doi.org/10.1016/j.vetpar.2005.10.013 PMid:16289566. [DOI] [PubMed] [Google Scholar]
- 13.Sævik BK, Jörundsson E, Stachurska-Hagen T, Tysnes K, Brun-Hansen H, Wikström HC, et al. Dirofilaria repens infection in a dog imported to Norway. Acta Vet Scand. 2014;56:6. doi: 10.1186/1751-0147-56-6. https://doi.org/10.1186/1751-0147-56-6 PMid:24447798 PMCid:PMC3933376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bertozzi M, Rinaldi VE, Prestipino M, Giovenali P, Appignani A. Dirofilariasis Mimicking an Acute Scrotum. Pediatr Emerg Care. 2015;31(10):715–6. doi: 10.1097/PEC.0000000000000346. https://doi.org/10.1097/PEC.0000000000000346 PMid:25626639. [DOI] [PubMed] [Google Scholar]
- 15.Senanayake MP, Infaq ML, Adikaram SG, Udagama PV. Ocular and subcutaneous dirofilariasis in a Sri Lankan infant:an environmental hazard caused by dogs and mosquitoes. Paediatr Int Child Health. 2013;33(2):111–2. doi: 10.1179/2046905512Y.0000000024. https://doi.org/10.1179/2046905512Y.0000000024 PMid:23925286. [DOI] [PubMed] [Google Scholar]
- 16.Révész E, Markovics G, Darabos Z, Tóth I, Fok E. Dirofilaria in the abdominal cavity. Magy Seb. 2008;61(5):281–4. doi: 10.1556/MaSeb.61.2008.5.6. https://doi.org/10.1556/MaSeb.61.2008.5.6 PMid:19028661. [DOI] [PubMed] [Google Scholar]
- 17.Sviben M, Mestrović T, Nemer K, Bartulović KP, Skara R, Galinović GM. Dirofilaria repens as a cause of subconjunctival infection in a 77-years old female patient from Croatia--a case report. Coll Antropol. 2013;37(3):995–7. PMid:24308248. [PubMed] [Google Scholar]
- 18.Janjetović Z, Arar ZV, Paradzik MT, Sapina L, Bitunjac M, Lojen G, et al. Ocular dirofilariasis:a case report. Acta Med Croatica. 2010;64(1):41–5. (in Croatian) PMid:20653124. [PubMed] [Google Scholar]
- 19.Bezić J. Human dirofiliariasis in Croatia. Acta Dermatovenerol Croat. 2009;17(1):82–3. PMid:19386219. [PubMed] [Google Scholar]
- 20.Marusić Z, Stastny T, Kirac I, Stojcević D, Kruslin B, Tomas D. Subcutaneous dirofilariasis caused by Dirofilaria repens diagnosed by histopathologic and polymerase chain reaction analysis. Acta Dermatovenerol Croat. 2008;16(4):222–5. PMid:19111148. [PubMed] [Google Scholar]
- 21.Bezić J, Vrbicić B, Guberina P, Alfier V, Projić P, Marović Z. A 52-year-old woman with a subcutaneous, slightly movable and painless nodule in the left breast. Ann Saudi Med. 2006;26(5):403–4, 414. doi: 10.5144/0256-4947.2006.403. https://doi.org/10.5144/0256-4947.2006.403 PMid:17019090 PMCid:PMC6074100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Puizina-Ivić N, Dzakula N, Bezić J, Punda-Polić V, Sardelić S, Kuzmić-Prusac I. First two cases of human dirofilariasis recorded in Croatia. Parasite. 2003;10(4):382–4. PMid:14710638. [PubMed] [Google Scholar]
- 23.Silaghi C, Beck R, Capelli G, Montarsi F, Mathis A. Development of Dirofilaria immitis and Dirofilaria repens in Aedes japonicus and Aedes geniculatus. Parasit Vectors. 2017;10(1):94. doi: 10.1186/s13071-017-2015-x. https://doi.org/10.1186/s13071-017-2015-x PMid:28219407 PMCid:PMC5319011. [DOI] [PMC free article] [PubMed] [Google Scholar]


