Abstract
Objective:
According to the CDC, 2.6 million people in the United States have an opioid use disorder and drug overdose is the leading cause of accidental death. Opioids are involved in 63% of overdose deaths. It is imperative that we identify evidence based treatments to stem the tide of this epidemic. This pilot study serves to explore the feasibility and effectiveness of Yoga as an adjunctive intervention for individuals with opioid use disorder in active medication-assisted treatment (MAT).
Methods:
Participants (N=26) were recruited from a buprenorphine/naloxone MAT program to participate in this study. 13 participants engaged in a 12 week adjunctive yoga intervention while remaining in treatment as usual (TAU) MAT. 13 matched controls were recruited and remained in TAU MAT. Both groups were evaluated at baseline, 45 days and 90 days for changes in craving for opioids, treatment retention, relapse rates, sleep, and symptoms of anxiety and perceived stress.
Results:
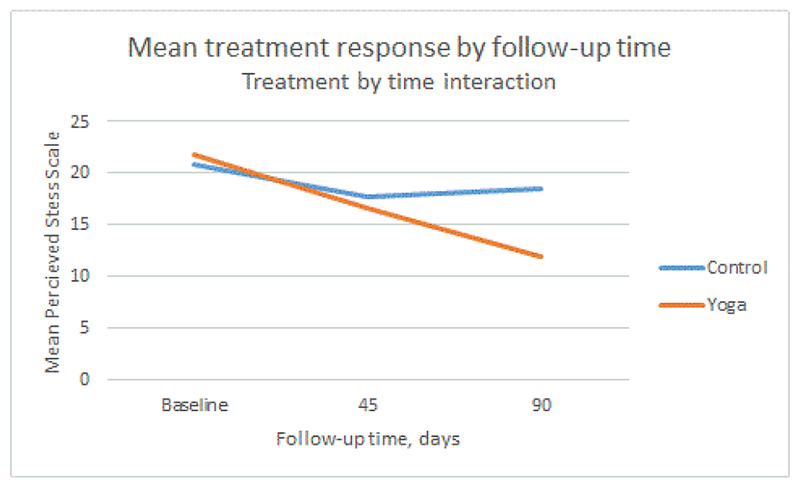
A two-way treatment by time analysis of variance was performed using a mixed effects model. The treatment by follow-up time interaction effect was significant for perceived stress (p=0.026) indicating that the yoga intervention had a larger effect than TAU (MAT). Changes in perceived stress decreased significantly over time in both the yoga intervention group and the TAU MAT matched control group.
Conclusion:
This pilot study indicated strong evidence for Yoga being an effective adjunctive treatment to MAT TAU in reducing perceived stress. Further research with a larger population is needed to determine impact on other mental health symptoms and relapse and retention rates.
Keywords: Yoga, medication-assisted treatment, Buprenorphine/naloxone, Opioid use disorder, Retention rates, Relapse rates, Perceived stress, Substance use disorder
Introduction
Opioid misuse is one of the biggest public health issues currently facing the United States. In 2016, the American Society of Addiction Medicine reported 2 million people had a substance use disorder involving prescription pain relievers and 591,000 had a substance use disorder involving heroin. Currently, medication-assisted treatment (MAT) with buprenorphine is endorsed by the Substance Abuse and Mental Health Services Administration (SAMHSA) for the treatment of opioid use disorders in combination with medication, counselling, and behavioral therapy. However one of the confounding factors in identifying effective interventions with individuals with substance use disorders is that 41.2% of individuals have a co-occurring mental health diagnosis according to the 2015 National Survey on Drug Use and Health [1]. Thus, identifying effective adjunctive treatments and integrating and adapting these evidenced-based treatments into MAT has the potential to improve outcomes by reducing mental health symptoms, increasing retention in treatment, decrease rates of relapse and ultimately reducing incidence of overdose deaths. Novel treatment modalities that provide emotional and cognitive support to individuals suffering from opioid use disorders and other psychiatric symptoms are needed to help manage the issue.
This study aims to explore the impact of yoga as an adjunctive intervention with individuals in early recovery from opioid use disorders. The use of the medication in the treatment of substance use disorders has been shown to increase retention in treatment and decrease relapse rates [2–4]. Yoga has been shown to help with a wide range of physical and psychological symptoms including symptoms commonly experienced in early recovery including depression, anxiety, stress, chronic pain and hypertension [5,6].
In this study, we seek to combine the two interventions: MAT with buprenorphine+naloxone and yoga, to see if the combination of yoga plus medication-assisted treatment is better than medication-assisted treatment alone with regard to reduced craving for opioids, increased treatment retention, lower relapse rates, improved sleep, and improved symptoms of anxiety and stress. This is a feasibility and effectiveness study with participants in a real world out-patient treatment setting. Participants are also tracked with regard to their compliance in attending yoga sessions. Impediments for implementing yoga in a clinical setting are evaluated.
Literature Review
Yoga and mindfulness meditation are becoming more recognized as complimentary therapies for addiction, as they target the cognitions and emotions related to relapse, and behaviors related to cravings [7]. Yoga has been shown to have a significant positive impact on individuals with PTSD, which is a co-occurring diagnosis often seen in individuals with opioid use disorders, especially those who use intravenously. A three-year National Institute of Health-funded study looked at the effects of yoga on trauma. At the end of the 10 week yoga intervention, 52% of the participants in the yoga group no longer met the diagnostic criteria for PTSD [8]. Yoga reduces the fight-or-flight response through a series of postures, breathing and relaxation, by decreasing the sympathetic nervous system’s reactive response and increasing the parasympathetic relaxation response [9]. Telles et al. reviewed multiple studies examining the impact of Yoga interventions on PTSD symptoms which showed reduction in anxiety, depression and PTSD symptoms [10]. The physical practice of yoga may also be of benefit in the treatment of opioid use disorder due to activation of similar reward pathways as those involved with drugs of abuse, specifically dopaminergic pathways in the mesolimbic system [11,12].
Yoga and mindfulness are practices that go hand-in-hand, with the practice of mindfulness being at the heart of the discipline of yoga. A randomized, controlled study done by Witkiewitz and Bowen examined Mindfulness-Based Relapse Prevention (MBRP) and its effectiveness for reduction of depression, craving and substance use [13]. MBRP is an 8-week, group-based psychoeducational intervention that uses cognitive-behavioral relapse prevention techniques along with meditation and mindful movement to teach alternative responses to emotional discomfort often associated with cravings. The study found that the MBRP group reported significantly lower rates of substance use at the 2 month follow-up. The results confirmed that MBRP influences cognitive and behavioral responses to depressive symptoms, which may explain the reduction in substance use among the treatment group.
Difficulty with sleep is also reported as a common symptom for individuals with Substance Use Disorders in early recovery. A cross-sectional study conducted at the Alcohol and Drug Recovery Center at the Cleveland Clinic found that 95% of the subjects, who met the criteria for active substance abuse, suffered from sleep impairment, while 56 percent had insomnia of a moderate-to-severe degree [14]. Yoga has been shown to improve sleep in all areas including time it takes to fall asleep, number of awakenings, total sleep time and sleep quality [15–18]. Little research has been conducted on yoga interventions and the impact on sleep with individuals in early recovery from opioid use disorder.
In addition, multiple studies have shown yoga to be effective in reducing perceived stress as well as anxiety [19–23]. One such study of 300 yoga naïve subjects showed a significant 14.7% reduction in anxiety even after a single 2 h yoga session [24]. The practice of Yoga has been found to reduce cortisol levels and increase GABA [25,26]. Less is known about how yoga can impact individuals in early recovery from substance use disorders, a time known for its intense stress as they transition from a lifestyle of active substance misuse to one involving abstinence from substances.
The goal of the current investigation is to qualitatively evaluate the effectiveness of yoga as an adjunctive intervention to medication-assisted treatment for opioid use disorder.
Methodology
This study was approved by the WVU Institutional Review Board (Protocol #1510894967). Eligible participants were recruited from their buprenorphine+naloxone MAT program after having been adherent in treatment for at least 90 days. Treatment requirements of this MAT program included weekly or every other week medication management, group therapy and attendance at community based peer recovery groups. Frequency of clinical contact varies depending on number of days abstinent. In the treatment program, patients attend weekly medication management and group therapy until they have 90 days abstinent and then attend treatment bi-weekly. Patients are also required to attend a minimum of four self-help meetings (e.g. Narcotics Anonymous, Alcoholics Anonymous, SMART recovery) weekly as part of their participation in treatment. Typically, patients are prescribed between 2–16 mg of Suboxone FILM® per day and all participants continued to receive Suboxone FILM® at the dose determined by their physician throughout this study. Patients typically remain in treatment if they relapse and report the relapse voluntarily.
Study inclusionary criteria were: diagnosis of opioid use disorder within the last 12 months as determined by DSM-5 criteria; active in the clinic based buprenorphine/naloxone medication-assisted treatment program for more than 90 days; male or a non-pregnant, female age 18 or greater; able to understand and provide written informed consent to participate; able to provide contact information; comprehend and communicate in English. Exclusionary criteria were assessed by the treating physician and included being at high risk for suicide, at high risk for study drop out due to incarceration, pregnancy, having a current psychotic disorder, or a primary substance use disorder other than for opioids.
This prospective pilot study used a quasi-experimental design using matched controls. One group of participants took part in a weekly yoga intervention for 12 weeks. The yoga sessions were taught by a certified yoga instructor who is also an Independently Licensed Counselor and Certified Addiction Counselor. The Yoga intervention incorporated Vinyasa flow movements, derived from Hatha Yoga, along with restorative yoga poses, mindful breathing and meditations. During the study, yoga participants remained in MAT which was comprised of out-patient group-based medication-assisted treatment with buprenorphine/naloxone. Non-randomized control participants were also enrolled in the study for 12 weeks. They attended MAT only and served as comparisons to the interventional yoga participants. They were matched on number of days abstinent, age, sex and frequency of clinic attendance (weekly or bi-weekly) at the time of recruitment.
Participants were given a gift card in the amount of $10.00 for each yoga session they attended, and were given a gift card in the amount of $10.00 for the completion of assessments at the three time periods.
Outcome measures
Number of days abstinent from all substances including alcohol and retention in MAT were tracked at baseline, 45 days and 90 days among both groups during the study period. Abstinence and retention were assessing based on both self-report and clinical urine drug screen records. Relapse rate was calculated as number of participants who reported at least 1 relapse on any substance (including alcohol) during the duration of the study. Basic demographic information was collected at baseline including co-morbid mental health diagnosis. Weekly yoga attendance was also tracked to determine any possible dose effect. The following measures were used to assess stress, craving, sleep and anxiety at the three time period intervals for all participants.
Perceived stress scale
The scale, created by Sheldon Cohen and colleagues, is used to measure the degree to which situations in one’s life are appraised as stressful. It is a 10 question survey evaluated on a Likert scale assessing levels of stress in the last month. Reliability was reported as Cronbach’s α between 0.84–0.86 for the PSS. Test-retest reliability for the PSS was 0.85. With regard to validity, correlation of the PSS to other measures of similar symptoms ranges between 0.52–0.76 [27,28].
Opioid craving scale
This scale is a 3 question Likert craving scale developed as part of an ancillary study of data from the Prescription Opioid Addiction Treatment Study in the National Drug Abuse Treatment Clinical Trials Network and adapted from the cocaine craving scale. It has been found to be predictive of relapse in multiple studies [29–31].
Sleep scale
Sleep scale from the medical outcomes study (MOS-sleep)
The MOS-Sleep is a 12-item self-report questionnaire based on a comprehensive conceptual model that covers both physical and mental health, it was originally designed for patients with chronic illness but was also validated in general population as an effective approach to the sleep assessment [32–34].
Anxiety scale
We used the Beck Anxiety Inventory (BAI), a 21 question self-report inventory used to measure the severity of an individual’s anxiety on a scale from 0–335 [35]. According to Beck, the Beck Anxiety Inventory (BAI) has shown both high internal consistency (Cronbach’s alpha=0.92) and acceptable test-retest reliability over a 1 week period, r (81)=0.7536. In the same study by Beck et al., which focused on evaluating the psychometric properties of the BAI, the inventory was able to correctly discriminate between anxious diagnostic groups and non-anxious diagnostic groups [36]. Additionally, this study also showed that the BAI was moderately correlated with the revised Hamilton Anxiety Rating Scale, r (150)=0.51, and mildly correlated with the revised Hamilton Depression Rating Scale, r (l53)=0.2536.
Statistical analysis
All categorical data were summarized with frequencies and percentages and continuous data with means and standard deviations. Analysis of treatment effects was performed using a mixed model approach in which treatment group and follow-up time were fixed effects and the pairing (e.g. pair number) was a random effect. The test for overall treatment effect was obtained from the test of treatment by time interaction and then post-hoc T tests were performed to obtain significant differences for treatment at a given time and treatment time effect within treatment group. The analyses were performed using the SAS Mixed procedure37. All statistical tests were two-tailed and performed at the 0.05 significance level.
Results
Participant characteristics
A total of 22 participants were recruited into the Yoga intervention. 13 of these individuals were retained in the intervention. 9 dropped out of the study prior to initiation the yoga intervention. The remaining 13 yoga intervention participants were then matched to controls in the TAU MAT group. With regard to the feasibility and acceptability of the yoga intervention, of those individuals who were not retained, five participants dropped out of the study due to lack of transportation, lack of childcare, and work schedule conflicts and 3 were discharged from the MAT program due to non-compliance with clinic rules. Of the 13 yoga intervention participants, 4 attended just one yoga session, 3 attended only two yoga sessions, 3 attended four to seven yoga sessions, 3 attended ten to twelve yoga sessions.
There are no statistically significant differences between the individuals in the interventional yoga group and those in the control group in their demographic profiles. Demographics of the two groups are detailed in Table 1. The majority of participants in the study are Caucasian, with one Hispanic participant in the intervention group. The average age of first use of a substance for all participants is 13.7 years old, with the average use of first use of opioids being age 17.3. In the control group, 77% of participants have a dual diagnosis, and 61% of those in the yoga intervention group have a dual diagnosis. This is much higher than the national incidence of dual diagnosis, which is 41% [1]. The majority of participants in the control group are gainfully employed (68%), whether part-time or full-time, whereas 45% of those in the yoga intervention group are gainfully employed. Despite the slightly higher majority of participants being employed in the control group Medicaid insurance rates remain high in both groups; 84% in the control group and 69% in the yoga intervention group indicating a low SES among both groups. The majority of the participants in both groups are single, with a total of 7 from both groups that are married, and 2 from both groups that are divorced.
Table 1:
Demographics
| Control N=13(%) | Yoga N=13(%) | |
|---|---|---|
| Marital status | ||
| Single | 9 (69) | 8 (61) |
| Married | 3 (23) | 4 (30) |
| Divorced | 1 (8) | 1 (8) |
| Education | ||
| High school/GED | 8 (61) | 5 (38) |
| College <4 years | 4 (30) | 6 (46) |
| College grad | 0 | 2 (15) |
| Non-HS grad | 1 (8) | 0 |
| Employment | ||
| Unemployed | 3 (23) | 7 (53) |
| Part time | 4 (30) | 2 (15) |
| Full time | 5 (38) | 4 (30) |
| Disabled | 1 (8) | 0 |
| Health Insurance | ||
| Medicaid | 11 (84) | 9 (69) |
| Medicare | 1 (8) | 0 |
| Private Insurance | 1 (8) | 3 (23) |
| Self-Pay | 0 | 1 (8) |
| Race | ||
| Caucasian | 13 (100) | 12 (92) |
| Hispanic | 0 | 1(8) |
| Characteristics | ||
| Average age of first substance use | 13.5 | 13.8 |
| Average age of first opioid use | 17.6 | 17 |
| Mental Health Diagnosis | ||
| Generalized Anxiety Disorder | 4 | 3 |
| Major Depressive Disorder | 7 | 6 |
| PTSD | 0 | 4 |
| OCD | 3 | 0 |
| Bipolar Disorder | 1 | 0 |
| ADHD | 1 | 1 |
| Total with MH DX | 10 (77) | 8 (61) |
Primary outcomes
The primary outcomes of interest in the study were retention in medication-assisted treatment, relapse rates, perceived stress, craving, sleep and anxiety. With regard to retention rates, 77% of the MAT+yoga participants remained in MAT treatment for the 12 weeks of the study (10 of 13) and 77% of the control group participants were also retained in their MAT treatment (10 of 13). There were no differences in retention rates in the MAT+Yoga group versus the control group. With regard to relapse rates among participants who initiated the study, the relapse rate of for the MAT+yoga group was 61% and for the control group was 38%. Relapse rates in the MAT+Yoga group versus the control group were also not statistically significantly different using fisher exact test (p=0.43).
In the two-way analysis of variance with treatment (between subjects) and follow-up time (within subjects) as fixed effects, the treatment by time interaction was significant (p=0.026) only for the perceived stress outcome. Post-hoc analyses shown in Table 2 indicated that this result was driven by a large difference between perceived stress for the MAT+ yoga and MAT at the 90 day follow-up measurement, while the two groups were not significantly different on this measure at 45 days (Figure 1).
Table 2:
Mean and standard deviation of perceived stress by treatment group and follow-up time;
| Treatment Group | |||
|---|---|---|---|
| Time | MAT | Yoga+MAT | p value |
| Mean (SD) | Mean (SD) | ||
| Baseline | 20.9 (5.8) | 22.1 (9.1) | 0.674 |
| 45 days | 17.8 (8.1)* | 16.7 (6.4)* | 0.631 |
| 90 days | 18.7 (6.3) | 11.6 (6.5)* | 0.008 |
| p value | 0.027 | 0.001 | |
Significantly different from Baseline p<0.05.
Figure 1:
Line chart for percived stress scale (PSS).
Within subjects analysis of variance was performed to test for main effects of follow-up time, separately for each treatment group. The time effect for the MAT+yoga group was significant for perceived stress (p=0.001), with significant post-hoc differences between baseline and 45 days (p=0.030), baseline and 90 days (p=0.0003), and 45 days and 90 days (p=0.049). The overall time effect for perceived stress was also significant for the MAT group (p=0.028), with significant post-hoc differences between baseline and 45 days (p=0.010), but not baseline and 90 days (p=0.058), or 45 days and 90 days (p=0.545) (Table 2).
The time effect was not significant for the BAI for either the MAT +yoga group (p=0.156) or the MAT group (p=0.734). The time effect was also not significant for the craving for either the MAT+yoga group (p=0.132) or the MAT group (p=0.906). There were no significant time effects for any of the sleep variables for either treatment group.
Between subjects (MAT+yoga vs. MAT) analysis of variance was performed to test for treatment group differences at baseline, 45 days and 90 days. For perceived stress there were no significant differences at baseline (p=0.674) or 45 days (p=0.631) follow-up, but the 90 day group difference was significant with perceived stress much lower for the MAT+yoga group (p=0.008). All other group difference by time was not significant.
Discussion
The intent of this pilot study was to assess the feasibility and effectiveness of a 12 week yoga intervention as an adjunctive treatment to medication-assisted treatment for individuals with opioid use disorder. The study was conducted in a rural state with poor public transportation and the study population was predominantly of low SES. The greatest impacts on feasibility were lack of childcare, transportation impediments, work and non-retention in MAT. Overall, 69% of our participants had a co-morbid psychiatric diagnosis making this a difficult to treat population with early onset of substance use, the average age of first substance use being 14 years and the average onset of opioid use being 17 years of age. Given the fact that 3 participants were discharged from clinic prior to being able to start the yoga intervention speaks to the need to better address the clinical needs of this population, however removing obstacles to access may also involve integrating the intervention into current treatment.
Due to our small sample size, treatment effect in both control group and the yoga+MAT was not significant across most measures with the exception of the perceived stress scale. The perceived stress scale assesses how unpredictable, uncontrollable and overwhelmed participants find their lives. 22 of the 26 participants scored above the norms on the stress scale. Participants improved significantly over all time points in the yoga+MAT group and most time points in the control group, the effect size being significantly greater in the interventional group. Several animal studies and some human laboratory studies have shown that stress exposure enhances drug self-administration. Indeed stress reduction outcomes of yoga are among the best documented. The national Institute of Health has identified yoga as an effective intervention for the treatment of hypertension [38] and measurably lower cortisol levels have been found in individuals who practice yoga [26,39].
Craving did not appear to be impacted by the yoga intervention or the control intervention which may have in part been due to the fact that only 2 of 26 participants reported more than mild opioid craving at baseline. Despite this 50% of the study participants relapsed. Our stress measure may have better captured factors impacted by the MAT alone and yoga+MAT intervention than the craving scale. In addition, buprenorphine is highly effective in reducing cravings for opioids and most participants did not relapse on opioids but other substances. So the craving for opioid scale many not have captured craving for the substances participants actually relapsed on. Only 4 of the 16 individuals, who relapsed, relapsed on opioids. Other substances relapsed on included cannabis, methamphetamines, benzodiazepines, alcohol and stimulants.
With larger sample size, the trends seen in the yoga+MAT intervention impacting anxiety more greatly might be significant. A larger sample size would also provide more power to assess treatment impacts in retention and relapse rates. It is difficult to interpret the higher relapse rates among the yoga participants given the significant reduction reported in perceived stress among these same participants. Of the 8 yoga+MAT participants who relapsed, 6 of them had only attended 1–2 yoga sessions. So while the dose of yoga received may have been enough to reduce stress, it may not have been protective against relapse.
Limitations
One of the primary limitations of the study is the small sample size. Additionally, attrition resulting from participant drop out was a concern; due to not enough participants staying in the study long enough to acquire data to measure change and potential yoga dose effect. Our craving measure did not capture cravings for substances other than opioids. Being a pilot study, it was not a randomized controlled trial so there may have been some selection bias in those who elected to participate in the yoga intervention.
Conclusion
Clearly replicating the study with a larger sample size would help address issues of low power potentially contributing to the limited effect seen. To better assess the feasibility and acceptability of the yoga intervention, one possible protocol change to achieve this would be to integrate the yoga intervention into the MAT clinic in a specialized biweekly group that patients are already are required to attend. Attendance rates in the general MAT clinic are 90%. Additionally, while pain was not an outcome measured in this study yoga has been demonstrated to be an effective intervention for those with chronic pain [39], the utility of which could be studied in the chronic pain population who also struggle with substance use disorders and are a difficult population to treat.
Ultimately the goal of research into yoga as a clinical intervention is to prove the efficacy of yoga as evidence-based treatment for mental health and substance use disorders so that insurance companies pay for this intervention increasing its accessibility to a wider population of patients.
Acknowledgement
This project was supported by a grant from the West Virginia University Department of Behavioral Medicine and Psychiatry. Special thanks to Samantha Sloan and Auvid Memon. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
References
- 1.Bose J, Hedden SL, Lipari RN, Park-Lee E, Porter JD, et al. (2016) Key substance use and mental health indicators in the United States: Results from the 2015 National survey on drug use and health. Substance abuse and mental health services administration, Department of Health and Human Services. [Google Scholar]
- 2.Tkacz J, Severt J, Cacciola J, Ruetsch C (2012) Compliance with buprenorphine medication-assisted treatment and relapse to opioid use. Am J Addict 21: 55–62. [DOI] [PubMed] [Google Scholar]
- 3.Schottenfeld RS, Chawarski MC, Mazlan M (2017) Maintenance treatment with buprenorphine and naltrexone for heroin dependence in Malaysia: A randomised, double-blind, placebo-controlled trial. Lancet 371: 2192–2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Timko C, Schultz NR, Cucciare MA, Vittorio L, Garrison-Diehn C (2016) Retention in medication-assisted treatment for opiate dependence: A systematic review. J Addict Dis 35: 22–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kamradt JM (2017) Integrating yoga into psychotherapy: The ethics of moving from the mind to the mat. Complement Ther Clin Pract 27: 27–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarkar S, Varshney M (2017) Yoga and substance use disorders: A narrative review. Asian J Psychiatr 25: 191–196. [DOI] [PubMed] [Google Scholar]
- 7.Khanna S, Greeson JM (2013) A narrative review of yoga and mindfulness as complementary therapies for addiction. Complement Ther Med 21: 244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Kolk B, Stone L, West J (2014) Yoga as an adjunctive treatment for posttraumatic stress disorder: A randomized controlled trial 75. [DOI] [PubMed] [Google Scholar]
- 9.Sparrowe L (2011) Transcending trauma: How yoga heals. Yoga Int 89: 48–53. [Google Scholar]
- 10.Telles S, Singh N, Balkrishna A (2012) Managing mental health disorders resulting from trauma through yoga: A review. Depress Res Treat 2012: 401513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Linke SE, Ussher M (2015) Exercise-based treatments for substance use disorders: Evidence, theory and practicality. Am J Drug Alcohol Abuse 41: 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lynch WJ, Peterson AB, Sanchez V, Abel J, Smith MA (2013) Exercise as a novel treatment for drug addiction: A neurobiological and stage-dependent hypothesis. Neurosci Biobehav Rev 37: 1622–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Witkiewitz K, Bowen S (2010) Depression, craving and substance use following a randomized trial of mindfulness-based relapse prevention. J Consult Clin Psychol 78: 362–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahfoud Y, Talih F, Streem D, Budur K (2009) Sleep disorders in substance abusers: How common are they? Psychiatry (Edgmont) 6: 38–42. [PMC free article] [PubMed] [Google Scholar]
- 15.Halpern J, Cohen M, Kennedy G, Reece J, Cahan C, et al. (2014) Yoga for improving sleep quality and quality of life for older adults. Altern Ther Health Med 20: 37–46. [PubMed] [Google Scholar]
- 16.Kennedy S (2014) Yoga as the “Next Wave” of therapeutic modalities for treatment of insomnia. Int J Yoga Ther 24: 125–129. [PubMed] [Google Scholar]
- 17.Hariprasad VR, Sivakumar PT, Koparde V, Varambally S, Thirthalli J, et al. (2013) Effects of yoga intervention on sleep and quality-of-life in elderly: A randomized controlled trial. Indian J Psychiatry 55: S364–S368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khalsa SB (2004) Treatment of chronic insomnia with yoga: A preliminary study with sleep-wake diaries. Appl Psychophysiol Biofeedback 29: 269–278. [DOI] [PubMed] [Google Scholar]
- 19.Riley KE, Park CL (2015) How does yoga reduce stress? A systematic review of mechanisms of change and guide to future inquiry. Health Psychol Rev 9: 379–396. [DOI] [PubMed] [Google Scholar]
- 20.Huang FJ, Chien DK, Chung UL (2013) Effects of Hatha yoga on stress in middle-aged women. J Nurs Res 21: 59–66. [DOI] [PubMed] [Google Scholar]
- 21.Katzman MA, Vermani M, Gerbarg PL (2012) A multicomponent yoga-based, breath intervention program as an adjunctive treatment in patients suffering from generalized anxiety disorder with or without comorbidities. Int J Yoga 5: 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Javnbakht M1, Hejazi Kenari R, Ghasemi M (2009) Effects of yoga on depression and anxiety of women. Complement Ther Clin Pract 15: 102–104. [DOI] [PubMed] [Google Scholar]
- 23.Hofmann SG, Curtiss J, Khalsa SBS (2015) Yoga for generalized anxiety disorder: Design of a randomized controlled clinical trial. Contemp Clin Trials 44: 70–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Telles S, Gaur V, Balkrishna A (2009) Effect of a yoga practice session and a yoga theory session on state anxiety. Percept Mot Skills 109: 924–930. [DOI] [PubMed] [Google Scholar]
- 25.Streeter CC, Jensen JE, Perlmutter RM, Cabral HJ, Tian H, et al. (2007) Yoga Asana sessions increase brain GABA levels: A pilot study. J Altern Complement Med 13: 419–426. [DOI] [PubMed] [Google Scholar]
- 26.Watanabe E, Fukuda S, Hara H, Shirakawa T (2002) Altered responses of saliva cortisol and mood status by long-period special yoga exercise mixed with meditation and guided imagery. J Int Soc Life Inf Sci 20: 585–587. [Google Scholar]
- 27.Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24: 385–396. [PubMed] [Google Scholar]
- 28.Cohen S, Williamson G (1988) Perceived stress in a probability sample of the United States. The social psychology of health: Claremont symposium on applied social psychology. [Google Scholar]
- 29.McHugh RK, Fitzmaurice GM, Carroll KM (2014) Assessing craving and its relationship to subsequent prescription opioid use among treatment-seeking prescription opioid dependent patients. Drug Alcohol Depend: 121–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weiss RD, Griffin ML, Mazurick C (2003) The relationship between cocaine craving, psychosocial treatment, and subsequent cocaine use 160: 1320–1325. [DOI] [PubMed] [Google Scholar]
- 31.Weiss RD, Griffin ML, Hufford C, Muenz LR, Najavits LM, et al. (1997) Early prediction of initiation of abstinence from cocaine. Use of a craving questionnaire. Am J Addict 6: 224–231. [PubMed] [Google Scholar]
- 32.Hays RD, Stewart AL (1992) Sleep measures In: Stewart AL, Ware JE, eds. Measuring functioning and well-being: The medical outcomes study approach. Duke university Press. [Google Scholar]
- 33.Spritzer KL, Hays RD (2003) MOS sleep scale: A manual for use and scoring, version 1.0. Los Angeles, CA, pp: 1–8. [Google Scholar]
- 34.Hays RD, Martin SA, Sesti AM, Spritzer KL (2005) Psychometric properties of the medical outcomes study sleep measure. Sleep Med 6: 41–44. [DOI] [PubMed] [Google Scholar]
- 35.Steer RA, Beck AT (1993) Beck anxiety inventory manual.
- 36.Beck AT, Epstein N, Brown G, Steer RA (1988) An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol 56: 893–897. [DOI] [PubMed] [Google Scholar]
- 37.Littell RC, Stroup WW, Freund RJ (2002) SAS for linear models. 4th ed. SAS Institute. [Google Scholar]
- 38.Arias AJ, Steinberg K, Banga A, Trestman RL (2006) Systematic review of the efficacy of meditation techniques as treatments for medical illness. J Altern Complement Med 12: 817–832. [DOI] [PubMed] [Google Scholar]
- 39.Curtis K, Osadchuk A, Katz J (2011) An eight-week yoga intervention is associated with improvements in pain, psychological functioning and mindfulness, and changes in cortisol levels in women with fibromyalgia. J Pain Res 4: 189–201. [DOI] [PMC free article] [PubMed] [Google Scholar]