Abstract
Background: Research shows that individuals can improve mental health by increasing experiences of positive emotions. However, the role of positive emotions in perinatal mental health has not been investigated. This study explored the extent to which positive emotions during infant feeding are associated with maternal depression and anxiety during the first year postpartum.
Materials and Methods: One hundred and sixty-four women drawn from a longitudinal cohort of mother–infant dyads were followed from the third trimester through 12 months postpartum. We measured positive emotions during infant feeding at 2 months using the mean subscale score of the modified Differential Emotions Scale. Depression and anxiety symptoms were assessed with the Beck Depression Inventory-II and State Trait Anxiety Inventory-State subscale at months 2, 6, and 12. Generalized linear mixed models were used to estimate crude and multivariable associations.
Results: Among women with no clinical depression during pregnancy, higher positive emotions during infant feeding at 2 months were associated with significantly fewer depression symptoms at 2, 6, and 12 months and with lower odds of clinically significant depression symptoms at 2 and 6 months. In contrast to depression outcomes, women with clinical anxiety during pregnancy who experienced higher positive emotions had significantly fewer anxiety symptoms at 2, 6, and 12 months and lower odds of clinically significant anxiety at 2 and 6 months.
Conclusions: Positive emotions during infant feeding are associated with depression and anxiety outcomes during the first year postpartum and may be a modifiable protective factor for maternal mental health.
Keywords: postpartum depression, postpartum anxiety, positive affect, breastfeeding, longitudinal study
Introduction
Perinatal depression and anxiety are two of the most common complications of childbirth,1,2 which are associated with adverse outcomes for both mother and infant.3–5 Despite their prevalence and morbidity, perinatal depression and anxiety are underdiagnosed and undertreated, with only <50% of symptomatic women receiving a diagnosis6,7 or seeking treatment.8 Among those who seek treatment, many pregnant and breastfeeding women prefer nonpharmacologic options due to concerns about infant exposure to psychotropic medications.2,9 To reduce morbidity for mothers and infants, novel strategies are needed to prevent and treat perinatal depression and anxiety.
One promising target for intervention is positive emotionality. Positive emotions are pleasantly-valenced discrete responses to one's appraisal of circumstances as favorable,10 with biobehavioral features that are empirically distinguishable from negative emotions.11 Positive psychology interventions that increase experiences of positive emotions have been shown to experimentally reduce depression and anxiety symptoms12–14 and to improve resilience to future stressors through resources such as social support15 and coping skills.16,17 The broaden-and-build theory of positive emotions18 posits that these durable psychological and social resources result from the broadened cognitive and creative context associated with experiences of positive emotions.19,20
Preliminary evidence suggests an association between positive emotions and postpartum mental health. Among 344 Norwegian mothers followed up for 6 months postpartum, those using positive reappraisal as a coping strategy reported fewer depression symptoms.21 An observational study of 195 Greek women found an inverse association between positive emotions in the third trimester and depression symptoms at 1 week postpartum.22 However, neither of the above studies controlled for women's baseline mental health status, calling the causal direction of this association into question. In a sample of breastfeeding mothers, those with fewer postpartum depression and anxiety symptoms reported higher positive affect during observed feeding sessions at 2 and 8 weeks.23 Positive emotions experienced during regular mother–infant interactions such as infant feeding may broaden their associated benefits by increasing maternal sensitivity and attachment.24,25 Mothers who describe breastfeeding as a positive activity express feeling connected to their infant, self-confident as a parent, and supported to face new challenges.25 To our knowledge, no study has explored the association between positive emotions experienced during infant feeding and prospective maternal mental health outcomes.
To better understand the role of positive emotions in perinatal mental health, we estimated the association between positive emotions during infant feeding and maternal depression and anxiety symptoms across the first year postpartum. Grounded in the broaden-and-build theory, we hypothesized that women reporting more positive emotions during infant feeding at 2 months would have fewer postpartum depression and anxiety symptoms at 2, 6, and 12 months. We also explored the extent to which associations between positive emotions and depression and anxiety symptoms differed by women's baseline psychopathology.
Materials and Methods
Sample
Our sample was drawn from 220 pregnant women who were enrolled to the longitudinal cohort study Mood, Mother and Infant: The Psychobiology of Impaired Dyadic Development (MMI) and followed up from the third trimester until 12 months postpartum. The MMI cohort comprised women living near Chapel Hill, North Carolina, recruited through study fliers and obstetric or psychiatric visits. We oversampled women at elevated risk for postpartum depression and anxiety based on a history of depression/anxiety or an active depressive/anxiety disorder in the third trimester of pregnancy using a Structured Clinical Interview for DSM-IV (SCID). Eligible participants were 18–45 years old; 34–37 weeks' gestation of a singleton pregnancy; able to communicate in English; and intending to breastfeed for more than 2 months. Women were excluded from the study if they met any of the following criteria: history or current diagnosis of psychiatric disorders other than depression/anxiety; substance use disorder; neonatal intensive care unit admission >48 hours; major congenital anomaly, or neonatal death; use of tricyclic antidepressants; or contraindication for breastfeeding. A full description of the study can be found at http://mmi.web.unc.edu
For this analysis, we restricted to participants completing their 12-month visit by May 2017 (n = 177). We excluded women missing exposure data (n = 12) and one influential outlier based upon a priori criteria. The remaining 164 women comprise our analytic sample.
Measures
Baseline data were collected through questionnaires and interviews with study staff at the third-trimester laboratory visit, and follow-up contacts occurred through monthly phone interviews and laboratory visits at 2, 6, and 12 months postpartum.
Positive emotions during infant feeding
At 2 months postpartum, participants completed the modified Differential Emotions Scale (mDES),26 rating the “greatest amount” they experienced 20 positive and negative emotions during infant feeding over the past week using a five-point Likert scale (0 = not at all; 4 = extremely). The mDES was adapted from Izard's Differential Emotions Scale27 and has a high internal reliability ranging from 0.82 to 0.94.15,28 Our exposure uses the positive emotions subscale of the mDES, which provides a mean score across 10 discrete emotions: amusement, awe, contentment, gratitude, hope, joy, interest, love, pride, and inspiration. The experience of positive emotions during infant feeding at 2 months was analyzed as a continuous exposure and compared for consistency with alternate categorizations, such as binary (at the mean, median, and cutpoints between 2 and 3), tertiles, quartiles, and splines, based on distributions observed in the data. Using the criteria of model fit and interpretability, we chose a dichotomous exposure to compare high (≥2.5) versus low (≤2.5) positive emotions during infant feeding.
Postpartum depression and anxiety symptoms
At 2, 6, and 12 months, depression symptoms were measured using the Beck Depression Inventory-II (BDI-II),29 and anxiety symptoms were measured using the State Trait Anxiety Inventory-State (STAI-S) subscale.30 Both instruments have been validated in perinatal populations.31,32 Outcomes were assessed as both continuous symptoms and binary thresholds for meeting clinically significant cutoffs for depression or anxiety. A BDI-II cutoff of ≥14 has been shown to have a 92% sensitivity and 83% specificity for major depression based on a Mini International Neuropsychiatric Interview in a postpartum outpatient sample,33 and a STAI-S >40 administered at 1 week postpartum had a 67.5% sensitivity and 87.1% specificity in identifying anxious mothers at 8 weeks.34
Potential covariates
We used a directed acyclic graph35 to identify potential confounding and effect measure modification (Supplementary Fig. S1; Supplementary Data are available online at www.liebertpub.com/jwh). Potential confounding variables were indexed as follows: Maternal race/ethnicity, marital status, income, and education were reported at baseline prenatal visit. Baseline depression and anxiety symptoms were quantified using BDI-II and STAI-S scores. Moderate/severe childhood trauma was defined as abuse (physical ≥10; emotional ≥13; sexual ≥8) or neglect (physical ≥10; emotional ≥15)36 using Childhood Trauma Questionnaire (CTQ). Psychiatric treatment was defined as self-report of psychotropic medication or psychotherapy between baseline and month 2. The number of breastfeeding problems experienced during the first 2 weeks was reported at the first month 1phone interview.37 Return to work by 2 months was based on self-report at months 1 and 2. Infant temperament was assessed using Carey Early Infancy Temperament Questionnaire38 and social support using the Medical Outcomes Study Social Support Survey.39 Meeting one's prenatal breastfeeding intention by 2 months was defined as meeting baseline duration and exclusivity intentions at month 2. Concurrent negative emotions during infant feeding were defined using mDES at month 2 to highlight the unique contribution of positive emotions beyond the presence or absence of negative emotions.16,40 We also explored modification of the association between positive emotions and postpartum depression/anxiety by women's baseline psychopathology, defined as the presence or absence of clinical depression or anxiety during pregnancy using third-trimester SCID.
Statistical analyses
Generalized linear mixed models were used to estimate the crude and multivariable associations between experiences of positive emotions during infant feeding at 2 months and depression and anxiety scores at 2, 6, and 12 months. Mixed models are appropriate for longitudinal data with correlated error terms and both population-specific parameters (fixed effects) and subject-specific parameters (random effects). Based on Akaike Information Criteria (AIC) and Bayesian Information Criteria (BIC), the best fitting model for continuous outcomes included a random intercept to allow 2-month depression/anxiety scores to differ among participants, a random effect for time to account for interpersonal differences in linear change in scores over time, and a variance components covariance structure. For binary outcomes, the best fitting models included a random intercept only.
Confounders were included where they (1) were identified as important to adjust for based on subject matter knowledge as represented in the directed acyclic graph and (2) resulted in a change in the exposure–outcome effect estimate by >10% using backward elimination from the full model. Crude and adjusted estimates and their associated 95% confidence intervals (CIs) are presented for overall models. Effect measure modification was considered to be present where Likelihood Ratio Test (LRT) p values were <0.05 comparing models with and without an interaction term. Analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
Sensitivity analyses repeated the above analyses removing (1) exclusive formula feeders at 2 months, as these women may have a different emotional experience of infant feeding, and (2) women taking psychotropic medications, as their depression/anxiety symptoms may be low due to treatment despite their elevated baseline risk.
Results
Study sample characteristics
Descriptive characteristics are presented for the 164 women in the study sample by high (≥2.5 to 4) versus low (0–2.5) positive emotions scores (Table 1). The mean positive emotions score was 2.8 (standard deviation [SD], 0.8), with 64.6% of the sample classified as experiencing high positive emotions. Based on the third-trimester SCID, 23.8% of the sample had a depressive disorder during pregnancy (Major Depressive Disorder, Dysthymic Disorder, Depressive Disorder Not Otherwise Specified, or Postpartum Depression) and 26.2% had an anxiety disorder (Panic Disorder, Agoraphobia without History of Panic, Social Phobia, Obsessive Compulsive Disorder, Posttraumatic Stress Disorder, or Generalized Anxiety Disorder), with no significant differences by high versus low positive emotions. Approximately 76% of the sample was non-Hispanic White, almost half reported a postgraduate level of education, and about 90% were married/partnered, with no significant differences in positive emotions by sociodemographic characteristics. Approximately 27% of the sample was taking a psychotropic medication or participating in psychotherapy between baseline and exposure. Nearly one-third of the sample had not met their prenatal breastfeeding intention for any or exclusive breastfeeding by 2 months, with a higher percentage of these women reporting low positive emotions. Almost 30% had returned to work by 2 months postpartum, and 25% reported moderate/severe childhood trauma. Women who reported high positive emotions during infant feeding at 2 months had fewer concurrent negative emotions or early breastfeeding problems and were more likely to have liked breastfeeding in the first week postpartum (Table 1).
Table 1.
Descriptive Statistics by Low Versus High Positive Emotions
| Variable | Overall Mean (SD) or N (%) | Low positive emotions Mean (SD) or N (%)a | High positive emotionsaMean (SD) or N (%) | pb |
|---|---|---|---|---|
| Total | 164 | 58 (35.4) | 106 (64.6) | |
| Positive emotions during infant feedinga | 2.8 (0.8) | 1.9 (0.6) | 3.3 (0.4) | <0.001 |
| Baseline depressionc | 0.22 | |||
| No prenatal depression | 125 (76.2) | 41 (70.7) | 84 (79.2) | |
| Clinical depression during pregnancy | 39 (23.8) | 17 (29.3) | 22 (20.8) | |
| Baseline anxietyc | 0.16 | |||
| No prenatal anxiety | 121 (73.8) | 39 (67.2) | 82 (77.4) | |
| Clinical anxiety during pregnancy | 43 (26.2) | 19 (32.8) | 24 (22.6) | |
| Race/ethnicity | 0.45 | |||
| Non-Hispanic White | 125 (76.2) | 47 (81.0) | 78 (73.6) | |
| Non-Hispanic Black | 15 (9.1) | 3 (5.2) | 12 (11.3) | |
| Hispanic, any race | 15 (9.1) | 4 (6.9) | 11 (10.4) | |
| Other | 9 (5.5) | 4 (6.9) | 5 (4.7) | |
| Educational level | 0.14 | |||
| Some high school or high school graduate | 10 (6.1) | 4 (6.9) | 6 (5.7) | |
| Some college or college graduate | 80 (48.8) | 30 (51.7) | 50 (47.2) | |
| Postgraduate level | 74 (45.1) | 24 (41.4) | 50 (47.2) | |
| Marital status | 0.69 | |||
| Married/partnered | 149 (90.9) | 52 (89.7) | 97 (91.5) | |
| Single/divorced | 15 (9.1) | 6 (10.3) | 9 (8.5) | |
| Parity | 0.88 | |||
| Nulliparous | 89 (54.3) | 31 (53.4) | 58 (54.7) | |
| Multiparous | 75 (45.7) | 27 (46.6) | 48 (45.3) | |
| Psychotropic medication or psychotherapy at 2 monthsd | 0.07 | |||
| Yes | 45 (27.4) | 21 (36.2) | 24 (22.6) | |
| No | 118 (72.0) | 37 (63.8) | 81 (76.4) | |
| Missing | 1 (0.6) | 0 (0) | 1 (0.9) | |
| Met prenatal breastfeeding intention at 2 monthse | 0.43 | |||
| Yes | 108 (66.3) | 37 (63.8) | 72 (67.9) | |
| No | 53 (32.5) | 21 (36.2) | 32 (30.2) | |
| Missing | 2 (1.2) | 0 | 2 (1.9) | |
| Returned to work by 2 months | 0.03 | |||
| Yes | 49 (29.9) | 11 (19.0) | 38 (35.8) | |
| No | 113 (68.9) | 46 (79.3) | 67 (63.2) | |
| Missing | 2 (1.2) | 1 (1.7) | 1 (0.9) | |
| Moderate to severe childhood trauma experiencef | 0.80 | |||
| Yes | 41 (25.0) | 14 (24.1) | 27 (25.5) | |
| No | 121 (73.8) | 44 (75.9) | 77 (72.6) | |
| Missing | 2 (1.2) | 0 (0) | 2 (1.9) | |
| Negative emotions during infant feedinga | 0.5 (0.5) | 0.7 (0.6) | 0.4 (0.5) | 0.003 |
| Infant temperament at 2 monthsg | 27.4 (3.3) | 27.7 (3.6) | 27.2 (3.2) | 0.34 |
| Social support at 2 monthsh | 3.4 (0.6) | 3.3 (0.7) | 3.5 (0.6) | 0.05 |
| Breastfeeding problems during first 2 weeksi | 4.1 (1.9) | 4.6 (2.0) | 3.8 (1.9) | 0.02 |
| Liked breastfeeding during the first weekj | 3.5 (1.4) | 3.1 (1.4) | 3.8 (1.3) | 0.003 |
Modified Differential Emotions Scale scores range from 0 to 4, with higher scores indicating more emotions; descriptive statistics are presented by high positive emotions (score >2.5 to 4) and low positive emotions (0–2.5).
Independent samples t-test for continuous variables; chi-square test and Fisher's exact test for categorical variables.
Based on Structured Clinical Interview for DSM-IV criteria for active depression (including Major Depressive Disorder, Dysthymic Disorder, Depressive Disorder Not Otherwise Specified, or Postpartum Depression); a history of depressive disorder and current treatment with antidepressants or psychotherapy for more than once per month; active anxiety (including Panic Disorder, Agoraphobia, Social Phobia, Obsessive Compulsive Disorder, Generalized Anxiety Disorder, or Posttraumatic Stress Disorder); or a history of anxiety disorder and current treatment with antidepressants, benzodiazepines, or psychotherapy for more than once per month.
Includes self-reported psychotherapy or any of the following medications: antidepressants, benzodiazepines, antipsychotics, and hypnotics.
Defined as meeting prenatal intention for any and exclusive breastfeeding.
Defined as meeting the threshold for moderate/severe emotional abuse, physical abuse, sexual abuse, emotional neglect, or physical neglect on the 28-item Childhood Trauma Questionnaire.
Carey Early Infancy Temperament Questionnaire comprises nine categories of temperament, with higher scores indicating more difficult/negative qualities.
Medical Outcomes Study Social Support Survey scores range from 0 to 4, with higher scores indicating more support.
Early breastfeeding problem scores range from 0 to 18, with higher scores indicating more problems.
Likert scale from “1: Disliked very much” to “5: Liked very much.”
Bolded results are significant at p < 0.05.
Positive emotions during feeding and depression outcomes
In the overall sample, the mean BDI-II score was 8.0 (SD, 5.4) at 2 months, 7.2 (SD, 5.5) at 6 months, and 7.5 (SD, 7.0) at 12 months, with significant between-person trajectories of change over time. Approximately 16.5% of the sample met the criteria for clinically significant depression (BDI-II ≥14) at 2 months, 15.2% at 6 months, and 16.5% at 12 months. In crude models, high positive emotions during feeding were associated with a 2.85 (95% CI, 1.28–4.41) point decrease in BDI-II score at 2 months, a 2.90 (95% CI, 1.35–4.44) point decrease at 6 months, and a 2.98 (95% CI, 0.29–4.72) point decrease at 12 months (Table 2). These results remained significant but attenuated by month 12 after adjustment for prenatal depression scores, social support, and concurrent negative emotions during feeding: high positive emotions were associated with an adjusted 1.53 (95% CI, 0.20–2.87) point decrease in BDI-II score at 2 months, a 1.59 (95% CI, 0.32–2.86) point decrease at 6 months, and a 1.67 (95% CI, −0.26 to 3.60) point decrease at 12 months (Table 2). Our results remained robust to sensitivity analyses testing both the exclusion of exclusive formula feeders and women taking psychotropic medications (Supplementary Table S1).
Table 2.
Estimates of Association Between High Versus Low Positive Emotions During Infant Feeding at 2 Months and Postpartum Depression and Anxiety Outcomes at 2, 6, and 12 Months
| N | 2 months | 6 months | 12 months | |
|---|---|---|---|---|
| Continuous depression outcome (BDI-II)a | Beta (95% CI) | Beta (95% CI) | Beta (95% CI) | |
| Mean score (SD) | 8.0 (5.4) | 7.2 (5.5) | 7.5 (7.0) | |
| Crude model | 164 | −2.85 (−4.41 to −1.28) | −2.90 (−4.44 to −1.35) | −2.98 (−5.16 to −0.79) |
| Overall adjusted model | 164 | −1.53 (−2.87 to −0.20) | −1.59 (−2.86 to −0.32) | −1.67 (−3.60 to 0.26) |
| By baseline psychopathology, adjusted modelb | ||||
| No prenatal depression | 125 | −2.36 (−3.98 to −0.73) | −2.41 (−4.02 to −0.84) | −2.49 (−4.71 to −0.27) |
| Prenatal depression diagnosis | 39 | −0.41 (−3.09 to 2.27) | −0.46 (−3.14 to 2.21) | −0.54 (−3.62 to 2.53) |
| Clinically significant depression (BDI-II ≥14)a | Odds (95% CI) | Odds (95% CI) | Odds (95% CI) | |
|---|---|---|---|---|
| N (%) | 27 (16.5) | 25 (15.2) | 27 (16.5) | |
| Crude model | 164 | 0.20 (0.06 to 0.68) | 0.25 (0.09 to 0.69) | 0.36 (0.10 to 1.28) |
| Overall adjusted model | 164 | 0.38 (0.12 to 1.16) | 0.48 (0.20 to 1.16) | 0.70 (0.22 to 2.23) |
| By baseline psychopathology, adjusted modelb | ||||
| No prenatal depression | 125 | 0.20 (0.06 to 0.76) | 0.26 (0.09 to 0.78) | 0.37 (0.10 to 1.42) |
| Prenatal depression diagnosis | 39 | 0.80 (0.14 to 4.60) | 1.01 (0.20 to 5.09) | 1.45 (0.24 to 8.76) |
| Continuous anxiety outcome (STAI-S)c | Beta (95% CI) | Beta (95% CI) | Beta (95% CI) | |
|---|---|---|---|---|
| Mean score (SD) | 28.6 (7.4) | 28.2 (6.5) | 29.7 (8.0) | |
| Crude model | 164 | −3.15 (−5.23 to −1.08) | −2.94 (−4.85 to −1.04) | −2.63 (−5.08 to −0.19) |
| Overall adjusted model | 164 | −1.22 (−3.08 to 0.63) | −1.02 (−2.64 to 0.61) | −0.71 (−2.89 to 1.48) |
| By baseline psychopathology, adjusted modelb | ||||
| No prenatal anxiety | 121 | −1.93 (−2.29 to 0.42) | −0.81 (−2.06 to 0.45) | −0.61 (−2.14 to 0.92) |
| Prenatal anxiety diagnosis | 43 | −2.64 (−4.77 to −0.50) | −2.51 (−4.58 to −0.43) | −2.31 (−4.56 to −0.06) |
| Clinically significant anxiety (STAI-S >40)c | Odds (95% CI) | Odds (95% CI) | Odds (95% CI) | |
|---|---|---|---|---|
| N (%) | 12 (7.3) | 8 (4.9) | 16 (9.8) | |
| Crude model | 164 | 0.29 (0.06 to 1.38) | 0.41 (0.13 to 1.35) | 0.70 (0.16 to 3.06) |
| Overall adjusted model | 164 | 0.68 (0.15 to 3.11) | 0.96 (0.30 to 3.05) | 1.61 (0.37 to 7.01) |
| By baseline psychopathology, adjusted modelb | ||||
| No prenatal anxiety | 121 | 1.18 (0.20 to 6.89) | 1.66 (0.38 to 7.20) | 2.76 (0.49 to 15.57) |
| Prenatal anxiety diagnosis | 43 | 0.17 (0.01 to 0.56) | 0.07 (0.01 to 0.63) | 0.12 (0.01 to 1.23) |
Mixed models were used to estimate the crude and multivariable associations. Linear mixed models for continuous depression/anxiety outcomes included a random intercept to allow baseline depression/anxiety scores to differ among participants, a random effect for time to account for interpersonal differences in scores over time, and a variance components covariance structure to account for intrapersonal correlations across repeat measures. For binary outcomes, generalized linear mixed models included a random intercept and unstructured covariance structure. All adjusted models controlled for prenatal depression (BDI-II) or anxiety (STAI-S) scores, social support at 2 months, and concurrent negative emotions during infant feeding at 2 months. Bolded results are significant at p < 0.05.
BDI-II scores range from 0 to 63, with higher scores indicating more depression symptoms.
Baseline psychopathology was determined using SCID in the third trimester of pregnancy. The “no diagnosis” group includes those with no history and those with a history of depression/anxiety, whereas the “prenatal diagnosis” group met criteria for an active disorder during pregnancy.
Spielberger STAI-S scores range from 20 to 80, with higher scores indicating more anxiety symptoms.
BDI-II, Beck Depression Inventory-II; CI, confidence interval; STAI-S, State Trait Anxiety Inventory-State.
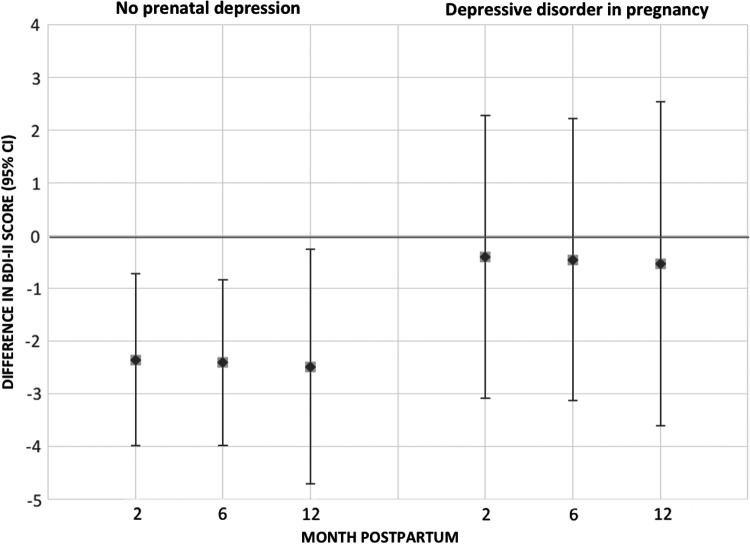
Baseline diagnosis of clinical depression significantly modified the association between positive emotions and depression scores (LRT, 14.6; p ≤ 0.001). Among women with no clinical depression during pregnancy, positive emotions during feeding were associated with significantly lower BDI-II scores at 2, 6, and 12 months. No significant association was observed among women with a depression diagnosis during pregnancy (Fig. 1).
FIG. 1.
The association between high versus low positive emotions during infant feeding and depression scores (BDI-II) at 2, 6, and 12 months, by baseline depression status. Point estimates show the association between high versus low positive emotions and BDI-II scores at 2, 6, and 12 months postpartum. The error bars indicate 95% confidence intervals; error bars that include 0 are not statistically significant. BDI-II, Beck Depression Inventory-II.
Similar patterns were observed for the clinically significant depression outcome. Stronger effects of positive emotions during feeding were observed for women without a prenatal diagnosis of depression: high positive emotions were associated with significantly lower odds of clinically significant depression symptoms (BDI ≥14) at 2 and 6 months among women with no diagnosis of prenatal depression (Table 2).
Positive emotions during feeding and anxiety outcomes
The mean STAI-S anxiety score in the sample was 28.6 (SD, 7.4) at 2 months, 28.2 (SD, 6.5) at 6 months, and 29.7 (SD, 8.0) at 12 months. Approximately 7.3% of the sample met the criteria for clinically significant anxiety (STAI-S > 40) at 2 months, 4.9% at 6 months, and 9.8% at 12 months. In crude models, high positive emotions during feeding were associated with a 3.15 (95% CI, 1.08–5.23) point decrease in STAI-S score at 2 months, a 2.94 (95% CI, 1.04–4.85) point decrease at 6 months, and a 2.63 (95% CI, 0.19–5.08) point decrease at 12 months (Table 2). These associations were attenuated and became nonsignificant after adjustment for baseline anxiety scores, social support, and concurrent negative emotions (Table 2).
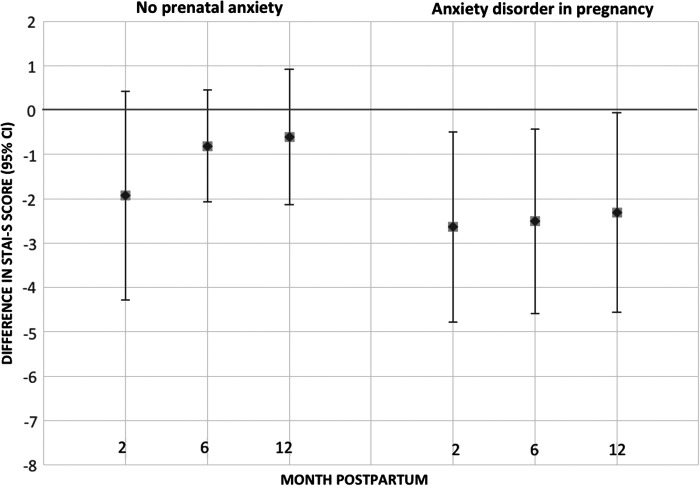
The association between positive emotions and anxiety scores was significantly different by baseline anxiety disorder diagnosis (LRT, 9.6; p = 0.002); however, in contrast to depression, positive emotions and anxiety scores were more strongly inversely associated among women with an anxiety diagnosis during pregnancy (Fig. 2). Among women with clinical anxiety at baseline, positive emotions were associated with significantly lower postpartum anxiety at 2 and 6 months.
FIG. 2.
The association between high versus low positive emotions during infant feeding and anxiety scores (STAI-S) at 2, 6, and 12 months, by baseline anxiety status. Point estimates show the association between high versus low positive emotions and STAI-S scores at 2, 6, and 12 months postpartum. The error bars indicate 95% confidence intervals; error bars that include 0 are not statistically significant. STAI-S, State Trait Anxiety Inventory-State.
Positive emotions during feeding were not associated with clinically significant anxiety symptoms (STAI > 40) in the overall sample; however, as with continuous anxiety scores, stronger and significant associations were observed among women with prenatal anxiety. Among women with clinical anxiety during pregnancy, higher positive emotions were associated with 0.17 (0.01–0.56) times the odds of clinically significant anxiety at 2 months, 0.07 (0.01–0.63) times the odds at 6 months, and 0.12 (0.01–1.23) at 12 months (Table 2). Sensitivity analyses yielded similar results (Supplementary Table S1).
Discussion
Positive emotions during infant feeding at 2 months postpartum were associated with maternal mental health across the first year postpartum. Among women without a diagnosis of depression during pregnancy, high positive emotions during feeding were associated with significantly lower depression symptoms at 2, 6, and 12 months. This association strengthened over time, even after controlling for prenatal depression symptoms, concurrent negative emotions during feeding, and social support. High positive emotions were also associated with lower odds of clinically significant depression symptoms among women without depression during pregnancy. In contrast, high positive emotions were associated with lower anxiety symptoms among women with a diagnosis of anxiety disorder during pregnancy.
The association between positive emotions and depression outcomes was stronger among women who were not actively depressed during pregnancy. High negative affect has been shown to attenuate associations with positive emotions in other contexts; for example, an observational study of women with HIV has found that the association between positive emotions and viral load suppression weakened at elevated levels of negative affect.41 Depressed individuals experienced disturbances in positive emotional functioning with attentional biases toward negative information, inability to sustain positive affect over time, and less activation of associated reward circuitry.42,43 These cognitive distortions may reduce the potential benefits of positive emotions during infant feeding.
In contrast to depression outcomes, the protective association between positive emotions and anxiety was stronger among women with a prenatal diagnosis of anxiety disorder. We speculate that positive emotions during infant feeding may buffer against developing postpartum anxiety symptoms by improving psychological resilience to stress.26,44 Women with prenatal anxiety who enjoy breastfeeding may benefit more from the anxiolytic effects of oxytocin during breastfeeding45,46 compared to women with prenatal depression.23
This is the first study to explore an association between positive emotions during infant feeding and postpartum mental health. Strengths of this investigation include the extensive longitudinal data on women's mental health, infant feeding, and descriptive characteristics, which address some limitations of previous correlational research.47 We used a prenatal SCID to control for baseline mental health status, isolating the association between positive emotions during feeding and later mental health outcomes. Unmeasured confounding was reduced due to the breadth of data collected over time on study subjects and the minor amount of missingness. Finally, we applied Fredrickson's broaden-and-build theory to a new and understudied population, mother–infant dyads in the perinatal period. Our findings support the importance of examining mother–infant relational experience in the context of maternal mental health, given that few treatments for postpartum depression/anxiety address the mother–infant relationship.48,49
Our findings should be interpreted in the context of study limitations. To be included in the study, subjects needed to intend to breastfeed for at least 2 months; as a result, study participants were more highly motivated to breastfeed than the general population. Moreover, it is likely that women with severe depression/anxiety were unable to participate in this intensive longitudinal study. Moreover, women with severe depression or anxiety symptoms may have been unwilling to enroll in this intensive year-old study. Our study sample was predominantly non-Hispanic White, partnered, and highly educated, limiting our ability to consider modification by race/ethnicity or socioeconomic status despite well-established associations between these social determinants of health and both infant feeding and mental health. Future research on positive emotions during infant feeding or while engaged in other bonding activities should be conducted among women of color and groups with lower breastfeeding intentions.
Self-report measures used in analyses may have led to reporting bias, especially where affective responses are influenced by concurrent depression/anxiety. While the mDES has not been previously used in the context of infant feeding, it has been validated across numerous contexts,15,28 and we conducted a factor analysis that confirmed that the positive emotions subscale best represented one coherent construct in relation to infant feeding (Supplementary Fig. S2). Our study examined positive emotions during feeding at a single time point; future studies would benefit from exploring the emotional experience of infant feeding over time to quantify temporal dynamics of positive emotions and postpartum mental health. Finally, the relationship between positive emotions and depression/anxiety may be bidirectional. We reduced the likelihood of confounding by baseline psychopathology by using longitudinal data to support the temporality of our hypothesized associations and by controlling for prenatal depression/anxiety.
Conclusions
According to the broaden-and-build theory of positive emotions, experiences of positive emotions trigger upward spirals that improve mental health and well-being.18 Our study provides preliminary evidence for an association between positive emotions during infant feeding and postpartum mental health. These results can inform future clinical interventions to target the positive affect system in the perinatal period, leveraging the nurturing relationship between mother and infant to improve postpartum mental health.
Supplementary Material
Acknowledgments
This work was supported by the National Institute of Child Health and Human Development (R01HD073220 and 4T32HD052468-09) and the National Institute on Drug Abuse (K01 DA035153). This article uses data collected by the extraordinary MMI research team, including Brenda Pearson, Pam Beiler, Mala Elam, and Hmellisa Mlo. Barbara Fredrickson, a Kenan Distinguished Professor at the University of North Carolina at Chapel Hill, provided substantive and methodological expertise for studying positive emotions in this novel context.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. O'Hara MW, Swain AM. Rates and risk of postpartum depression—A meta-analysis. Int Rev Psychiatry 1996;8:37–54 [Google Scholar]
- 2. Sockol LE, Epperson CN, Barber JP. A meta-analysis of treatments for perinatal depression. Clin Psychol Rev 2011;31:839–849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Grote N, Bridge J, Gavin A, Melville J, Iyengar S, Katon W. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry 2010;67:1012–1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Paul IM, Downs DS, Schaefer EW, Beiler JS, Weisman CS. Postpartum anxiety and maternal-infant health outcomes. Pediatrics 2013;131:e1218–e1224 [DOI] [PubMed] [Google Scholar]
- 5. Kingston D, Tough S. Prenatal and postnatal maternal mental health and school-age child development: A systematic review. Matern Child Health J 2013;18:1728–1741 [DOI] [PubMed] [Google Scholar]
- 6. Ko JY, Farr SL, Dietz PM, Robbins CL. Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005–2009. J Womens Health (Larchmt) 2012;21:830–836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goodman JH, Tyer-Viola L. Detection, treatment, and referral of perinatal depression and anxiety by obstetrical providers. J Womens Health (Larchmt) 2010;19:477–490 [DOI] [PubMed] [Google Scholar]
- 8. Vesga-Lopez O, Blanco C. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry 2008;65:805–815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Battle CL, Salisbury A, Schofield CA, Ortiz-Hernandez S. Perinatal antidepressant use: Understanding women's preferences and concerns. J Psychiatr Pract 2013;19:443–453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fredrickson BL. Positive emotions broaden and build. In: Ashby Plant E, Devine PG, eds. Advances in experimental social psychology, Vol. 47 Burlington: Academic Press, 2013:1–53 [Google Scholar]
- 11. Garland EL, Fredrickson BL, Kring AM, Johnson DP, Meyer PS, Penn DL. Upward spirals of positive emotions counter downward spirals of negativity: Insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clin Psychol Rev 2010;30:849–864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Taylor CT, Lyubomirsky S, Stein MB. Upregulating the positive affect system in anxiety and depression: Outcomes of a positive activity intervention. Depress Anxiety 2017;34:267–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Seligman MEP, Rashid T, Parks AC. Positive psychotherapy. Am Psychol 2006;61:774. [DOI] [PubMed] [Google Scholar]
- 14. Kearney DJ, Martinez M, Kearney DJ, Mcmanus C, Malte CA. Loving-kindness meditation and the broaden-and-build theory of positive emotions among veterans with loving-kindness meditation and the broaden-and-build theory of positive emotions among veterans with posttraumatic stress disorder. Med Care 2014;52:S32–S38 [DOI] [PubMed] [Google Scholar]
- 15. Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM. Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. J Pers Soc Psychol 2008;95:1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Burns AB, Brown JS, Sachs-Ericsson N, et al. Upward spirals of positive emotion and coping: Replication, extension, and initial exploration of neurochemical substrates. Pers Individ Dif 2008;44:360–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fredrickson BL, Joiner T. Positive emotions trigger upward spirals toward emotional well-being. Psychol Sci 2002;13:172–175 [DOI] [PubMed] [Google Scholar]
- 18. Fredrickson BL. The broaden-and-build theory of positive emotions. Philos Trans R Soc Lond B Biol Sci 2004;359:1367–1378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Isen AM, Johnson MM, Mertz E, Robinson GF. The influence of positive affect on the unusualness of word associations. J Pers Soc Psychol 1985;48:1413–1426 [DOI] [PubMed] [Google Scholar]
- 20. Subramaniam K, Vinogradov S. Improving the neural mechanisms of cognition through the pursuit of happiness. Front Hum Neurosci 2013;7:452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Haga SM, Ulleberg P, Slinning K, Kraft P, Steen TB, Staff A. A longitudinal study of postpartum depressive symptoms: Multilevel growth curve analyses of emotion regulation strategies, breastfeeding self-efficacy, and social support. Arch Womens Ment Health 2012;15:175–184 [DOI] [PubMed] [Google Scholar]
- 22. Moraitou M, Galanakis M, Stalikas A, Garivaldis FJ. The relation of positive emotions to post partum depression. Eur J Psychol 2011;7:112–142 [Google Scholar]
- 23. Stuebe AM, Grewen KM, Meltzer-Brody S. Association between maternal mood and oxytocin response to breastfeeding. J Womens Health (Larchmt) 2013;22:352–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kok BE, Coffey KA, Cohn MA, et al. How positive emotions build physical health perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychol Sci 2013;24:1123–1132 [DOI] [PubMed] [Google Scholar]
- 25. Burns E, Schmied V, Sheehan A, Fenwick J. A meta-ethnographic synthesis of women's experience of breastfeeding. Matern Child Nutr 2010;6:201–219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J Pers Soc Psychol 2003;84:365–376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Izard C. Human emotions. New York: Plenum Press, 1977 [Google Scholar]
- 28. Cohn MA, Fredrickson BL, Brown SL, Mikels JA, Conway AM. Happiness unpacked: Positive emotions increase life satisfaction by building resilience. Emotion 2009;9:361–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation, 1996 [Google Scholar]
- 30. Spielberger CD. Manual for the State-Trait Anxiety Inventory STAI (Form Y) (“Self-Evaluation Questionnaire”), revised ed. Palo Alto, CA: Consulting Psychologists Press, 1983 [Google Scholar]
- 31. Vieira Da Silva Magalhães P, Tavares Pinheiro R, Lessa Horta B, Amaral Tavares Pinheiro K, Azevedo Da Silva R. Validity of the Beck Depression Inventory in the postpartum period. Int J Psychiatry Clin Pract 2008;12:81–84 [DOI] [PubMed] [Google Scholar]
- 32. Meades R, Ayers S. Anxiety measures validated in perinatal populations: A systematic review. J Affect Disord 2011;133:1–15 [DOI] [PubMed] [Google Scholar]
- 33. Wang Y, Gorenstein C. Assessment of depression in medical patients: A systematic review of the utility of the Beck Depression Inventory-II. Clinics 2013;68:1274–1287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dennis C, Coghlan M, Vigod S. Can we identify mothers at-risk for postpartum anxiety in the immediate postpartum period using the State-Trait Anxiety Inventory? J Affect Disord 2013;150:1217–1220 [DOI] [PubMed] [Google Scholar]
- 35. Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology 1999;10:37–48 [PubMed] [Google Scholar]
- 36. Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl 2003;27:169–190 [DOI] [PubMed] [Google Scholar]
- 37. Centers for Disease Control and Prevention. Infant feeding practices study II and its year six follow-up, 2014. Available at: www.cdc.gov/breastfeeding/data/ifps/results.htm#ch3 Accessed February22, 2016
- 38. Medoff-Cooper B, Carey WB, McDevitt SC. The Early Infancy Temperament Questionnaire. J Dev Behav Pediatr 1993;14:230–235 [PubMed] [Google Scholar]
- 39. Sherbourne CD, Stewart AL. The MOS Social Support Survey. Soc Sci Med 1991;32:705–714 [DOI] [PubMed] [Google Scholar]
- 40. Waugh CE, Fredrickson BL. Nice to know you: Positive emotions, self–other overlap, and complex understanding in the formation of a new relationship. J Posit Psychol 2006;1:93–106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wilson TE, Weedon J, Cohen MH, et al. Positive affect and its association with viral control with HIV infection. Health Psychol 2016;36:91–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Heller A, Johnstone T, Shackman A, et al. Reduced capacity to sustain positive emotion in major depression reflects diminished maintenance of fronto-striatal brain activation. Proc Natl Acad Sci U S A 2009;106:22445–22450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Carl JR, Soskin DP, Kerns C, Barlow DH. Positive emotion regulation in emotional disorders: A theoretical review. Clin Psychol Rev 2013;33:343–360 [DOI] [PubMed] [Google Scholar]
- 44. Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol 2004;86:320–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Niwayama R, Nishitani S, Takamura T, et al. Oxytocin mediates a calming effect on postpartum mood in primiparous mothers. Breastfeed Med 2017;12:103–109 [DOI] [PubMed] [Google Scholar]
- 46. Newton M, Newton NR. The let-down reflex in human lactation. J Pediatr 1948:33:698–704 [DOI] [PubMed] [Google Scholar]
- 47. Lyubomirsky S, King L, Diener E. The benefits of frequent positive affect: Does happiness lead to success? Psychol Bull 2005;131:803–855 [DOI] [PubMed] [Google Scholar]
- 48. Forman DR, O'Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Dev Psychopathol 2007;19:585–602 [DOI] [PubMed] [Google Scholar]
- 49. Letourneau NL, Cosic N, Linder J, Dennis C. The effect of perinatal depression treatment for mothers on parenting and child development: A systematic review. Depress Anxiety 2017;34:928–966 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.