Abstract
Background:
Sleep disorders in multiple sclerosis (MS) are associated with reduced health-related quality of life (HRQOL) and depression. However, research investigating and comparing how the two most common sleep disorders—insomnia and obstructive sleep apnea (OSA)—affect depression and HRQOL in MS is limited. The goal of this study is to examine the impact of diagnosed sleep disorders on patient-reported 1) HRQOL and 2) depressive symptoms in patients with MS.
Methods:
We performed a retrospective medical record review of 531 adult patients with MS: 287 (54%) with a comorbid sleep disorder (insomnia or OSA) and 244 (46%) without a diagnosed sleep disorder.
Results:
Neither 1) average ratings of depression or HRQOL nor 2) the proportion of moderate depression or moderately impaired HRQOL differed between individuals with MS and insomnia and those with MS and OSA. Neither sleep disorder predicted increased depression or poorer HRQOL. However, individuals with MS and a comorbid sleep disorder (insomnia or OSA) had poorer HRQOL compared with those without a diagnosed sleep disorder (MS only).
Conclusions:
Presence of a diagnosed sleep disorder may negatively affect HRQOL in MS. Providers should continue to screen for sleep disorders given their negative impact on patients with MS and the availability of effective treatments for insomnia and OSA.
Keywords: Depression, Health-related quality of life, Insomnia, Multiple sclerosis (MS), Obstructive sleep apnea
Multiple sclerosis (MS) is a chronic, autoimmune, inflammatory disease of the central nervous system that is associated with physical, mental health, and cognitive symptoms that can result in functional impairment.1 One common domain of impairment in MS is quality of life (QOL), defined as how an individual perceives their life in relation to their standards, goals, or expectations.2 Patients with MS report significantly lower QOL compared with individuals without MS.3 Reduced QOL in MS is multifactorial, likely a result of the disease process itself as well as symptoms and the effects of disease-modifying treatments.4
An important component of QOL, particularly for those with chronic diseases such as MS, is health-related QOL (HRQOL), which refers to the impact of an illness (including the disease process and its treatment) on the patient's perceived QOL.5 Health-related QOL is impaired in individuals with MS, even compared with other chronic conditions, such as epilepsy and diabetes.6 Reduced HRQOL may, in part, be due to poor sleep and fatigue, which are among the most common symptoms of MS.7 In fact, sleep quality and HRQOL are positively correlated such that poor sleep may be associated with reduced HRQOL in people with MS.8,9 Recent studies suggest that higher severity of sleep problems is associated with poorer HRQOL.7
A large proportion of patients with MS experience sleep disorders. The prevalence of diagnosed sleep disorders is higher in patients with MS compared with the general population, with estimates suggesting that 25% to 54% of people with MS meet the criteria for a sleep disorder.10 Among the sleep disorders, obstructive sleep apnea (OSA) and insomnia are the most common in patients with MS,11,12 with conservative estimates suggesting that at least 20% to 30% (and perhaps as high as 50%) of individuals with MS meet the criteria for OSA or insomnia.13 Some researchers have posited that sleep disorders can reduce HRQOL in people with MS, as people with MS who have sleep disorders show significantly lower HRQOL compared with people with MS who do not have diagnosed sleep disorders.9 Furthermore, OSA and insomnia are associated with the lowest HRQOL compared with other sleep disorders, such as restless legs syndrome.9
Sleep disorders in MS are also associated with depression. Patients with MS and chronic insomnia report higher levels of depression than those without insomnia.14 Moreover, rates of insomnia in patients with comorbid MS and depression are higher than those reported in the general MS population,15 and higher severity of insomnia predicts higher depression scores in those with MS.16 Rates of depressive disorders are also elevated in individuals with untreated OSA17 and are associated with lower HRQOL.18
Existing studies have established the relationships among sleep problems, depression, and reduced HRQOL.19 However, to our knowledge, no existing studies have tested the relationships among diagnosed sleep disorders, depression, and HRQOL simultaneously in a sample of patients with MS. This study compares how the two most common and impairing sleep disorders in MS (insomnia and OSA) affect ratings of depression and HRQOL. Specific aims are to compare 1) the prevalence of moderate depression and moderately poor HRQOL, 2) the average ratings of depression and HRQOL, and 3) whether sleep disorder diagnosis predicts increased depression or poorer HRQOL in patients with MS and insomnia (MS+insomnia) or OSA (MS+OSA). For each aim, sleep disorder diagnoses were compared (MS+OSA vs MS+insomnia), and all patients with diagnosed sleep disorders were collapsed into one group (MS+sleep) and compared with those without a diagnosed comorbid sleep disorder (MSonly).
The results of this study will provide information about the impact of insomnia and OSA on mood and HRQOL in patients with MS. A better understanding of the relationship between sleep and mood in patients with MS can inform assessment and treatment approaches and is warranted.20,21
Methods
Participants
The sample was collected via retrospective medical record review for individuals with MS who sought treatment at either a sleep disorder clinic or a comprehensive treatment center for MS between January 1, 2008, and September 30, 2016. Participants were excluded from the analyses if they were younger than 18 years, had a neurologic disorder other than MS, had an unspecified sleep disorder, or did not complete the two main outcome measures of depression and HRQOL. Approval was granted from the institutional review board of Cleveland Clinic Foundation, and all the procedures comply with the ethical standards for human subjects. Data were obtained from the Knowledge Program22 through the Cleveland Clinic Neurological Institute for Outcomes Research & Evaluation.
Measures
Diagnosis and Demographic Characteristics
Diagnosis of MS, insomnia (primary, chronic, paradoxical, psychophysiological, or other), and OSA was established using International Classification of Diseases, Tenth Revision (October 1, 2015, to September 30, 2016) or Ninth Revision (January 1, 2008, to September 30, 2015) codes listed in the participant's electronic medical record.
Patient age, sex, race, and overall sample characteristics were noted.
Outcomes
The primary outcomes were depression and HRQOL. Depressive symptoms were measured using the Patient Health Questionnaire-9,23 with total scores greater than 10 suggesting symptoms of moderate depression. Health-related QOL was assessed using the EuroQoL Five-Dimension Questionnaire,24 with total scores less than 0.33 indicating moderately impaired HRQOL.
Data Analysis
Descriptive statistics were used to describe the sample characteristics. Mean scores on each of the aforementioned measures were calculated. For the first aim, χ2 tests were used to test whether there is a relationship between sleep disorder diagnosis and incidence of moderate depression and moderately impaired HRQOL in people with MS. For the second aim, independent-samples t tests tested whether there are differences in average scores on HRQOL and depression based on sleep disorder diagnosis. For the third aim, multiple regression tested whether sleep disorder diagnosis predicts depressive symptoms or poorer HRQOL. For each aim, two analyses were conducted: the first analysis compared patients with sleep disorders (MS+OSA vs MS+insomnia groups), and the second analysis compared all patients with MS and sleep disorders (combined OSA and insomnia—the MS+sleep group) to the patients without a diagnosed sleep disorder (MSonly group). For all the analyses, alpha was set to 0.05.
Results
Participants
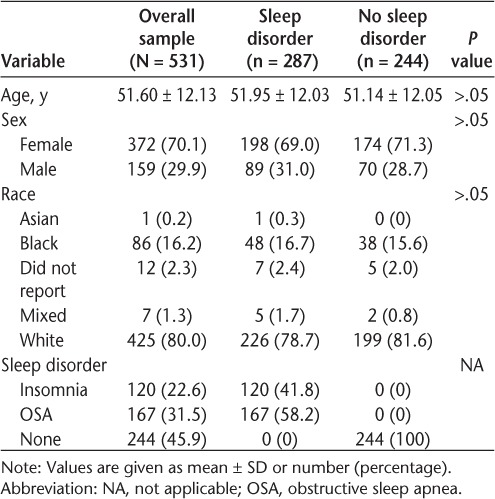
The sample comprised 531 individuals with MS, 287 (54%) of whom were diagnosed as having either OSA (MS+OSA; n = 167 [58%]) or insomnia (MS+insomnia; n = 120 [42%]). The remaining 244 participants (46%) were diagnosed as having MS but did not have a comorbid sleep disorder diagnosis (MSonly). The characteristics of the sample are given in Table 1.
Table 1.
Characteristics of sample of patients with multiple sclerosis
Aims
Moderate Depression and Moderately Poor HRQOL
There were no significant differences in the rate of moderate depression (χ21, n = 287 = 1.65, P = .20, ϕ = 0.08) or moderately impaired HRQOL (χ21, n = 287 = 0.77, P = .38, ϕ = 0.05) when comparing the MS+OSA and MS+insomnia groups. When participants with sleep disorders were collapsed into one group and compared with participants without diagnosed sleep disorders, there was a statistically significant difference in rates of moderately impaired HRQOL. Specifically, a larger proportion of the MS+sleep group endorsed poor HRQOL compared with the MSonly group (χ21, n = 531 = 4.78, P = .03, ϕ = −0.10). However, the rate of symptoms suggestive of moderate depression did not differ significantly between participants with and without sleep disorders (χ21, n = 531 = 0.24, P = .62, ϕ = 0.02).
Average Ratings of Depression and HRQOL
Similar to the first aim, there were no significant differences between the MS+OSA and MS+insomnia groups in terms of average scores on measures of depression (t285 = −0.05, P = .96) or HRQOL (t285 = 0.58, P = .56). The MS+sleep group did not report higher average ratings of depression than the MSonly group (t529 = 0.34, P = .73). Also, the MS+sleep group did not endorse significantly lower average ratings of HRQOL compared with the MSonly group (t529 = −1.74, P = .08).
Prediction of Depression or Poorer HRQOL
Type of sleep disorder did not significantly predict increased depression (F1,285 = 0.003, P = .96, R2 < 0.001) or poorer HRQOL (F1,285 = 0.34, P = .56, R2 = 0.01). Presence of a sleep disorder did not significantly predict increased depression (F1,529 = 0.12, P = .73, R2 < 0.001) and did not predict poorer HRQOL (F1,529 = 3.10, P =.08, R2 = 0.006).
Discussion
This study examined the impact of sleep disorder diagnosis on patient-reported depressive symptoms and HRQOL. The first aim was to compare whether depression or HRQOL differed between individuals with MS+insomnia versus MS+OSA. However, the proportion of participants with symptoms suggestive of moderate depression or moderately impaired HRQOL did not differ significantly when comparing the MS+insomnia and MS+OSA groups. There were also no significant differences in terms of average ratings of depression or HRQOL between the MS+insomnia and MS+OSA groups.
Although participants with insomnia did not differ significantly from those with OSA, results were significant when all patients with a sleep disorder were collapsed into one group and compared with patients with MS but without a diagnosed sleep disorder. Results suggested that presence of a sleep disorder can negatively affect HRQOL. Specifically, moderately impaired HRQOL was more common in patients with MS+insomnia or MS+OSA compared with the MSonly group. Most of the MS+sleep group (59.3%) reported moderately impaired HRQOL, and 40.7% of the MSonly group had moderately poor HRQOL. Although not significant, two trend-level findings also suggest that HRQOL is more impaired in patients with MS+sleep than with MSonly. Average ratings of HRQOL were lower, yet not statistically significantly so, in the MS+sleep group (mean = 0.74) than in the MSonly group (mean = 0.77).
However, the results did not indicate that patients with MS who also have a sleep disorder have more depression than patients without a diagnosed sleep disorder. Rates of moderate depression and overall scores on a measure of depression did not differ between these two groups. This result is somewhat surprising given the bidirectional relationship between depression and insomnia.25 Insomnia is a risk factor for depression, one of the common features of major depression, and may persist after the depressive episode has remitted, which suggests that there is a relationship between the regulation of mood and sleep.26
These findings must be considered in light of several limitations. Data on MS subtype (relapsing remitting vs progressive) were not available. It is likely that disease subtype may moderate the relationship between sleep disorder and depression or poor HRQOL; however, this hypothesis was not able to be tested in this study. Data were collected at participants' initial visit; thus, it was not possible to examine trends in depressive symptoms or HRQOL over time. Furthermore, data were collected through retrospective medical record review, which has numerous limitations, including that the medical record is not necessarily comprehensive and may include incomplete or missing data. To that end, sleep disorders are commonly undiagnosed in people with MS,13,27 thus individuals in the MSonly group may have had an undiagnosed sleep disorder. This may partially explain why differences between the MS+sleep and MSonly groups were not more pronounced. Furthermore, the correlational nature of this study does not allow for the determination that sleep disorder diagnosis is causally related to poorer HRQOL. Future studies testing these hypotheses are certainly indicated.
Overall, these results provide preliminary evidence that presence of a diagnosed sleep disorder may be associated with poor HRQOL in patients with MS. Thus, screening for sleep disorders may have a positive effect on improving HRQOL and overall QOL. Insomnia and OSA are widely regarded as treatable through interventions such as cognitive behavioral therapy and positive airway pressure treatment.28,29 The results of this study may inform practices regarding assessment and intervention to optimize HRQOL in MS.
PRACTICE POINTS
Patients with MS and a comorbid sleep disorder reported poorer health-related quality of life (HRQOL) compared with people with MS who do not have a diagnosed sleep disorder.
Rates of depression and reduced HRQOL did not differ between patients with insomnia and those with obstructive sleep apnea.
Given that sleep disorders may have a detrimental impact on HRQOL, assessing for sleep disturbance among patients with MS is important because there are well-supported, efficacious treatment options for insomnia and obstructive sleep apnea.
Financial Disclosures:
The authors declare no conflicts of interest.
Funding/Support:
No financial funding was received for this study. Data were provided by the Cleveland Clinic Knowledge Program.22
References
- 1.Noseworthy JH, Lucchinetti C., Rodriguez M., Weinshenker BG. Multiple sclerosis. N Engl J Med. 2000;343:938–952. doi: 10.1056/NEJM200009283431307. [DOI] [PubMed] [Google Scholar]
- 2.The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41:1403–1409. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 3.Janardhan V., Bakshi R. Quality of life in patients with multiple sclerosis: the impact of fatigue and depression. J Neurol Sci. 2002;205:51–58. doi: 10.1016/s0022-510x(02)00312-x. [DOI] [PubMed] [Google Scholar]
- 4.Lobentanz IS, Asenbaum S., Vass K. et al. Factors influencing quality of life in multiple sclerosis patients: disability, depressive mood, fatigue, and sleep quality. Acta Neurol Scand. 2004;110:6–13. doi: 10.1111/j.1600-0404.2004.00257.x. [DOI] [PubMed] [Google Scholar]
- 5.Schipper H., Clinch JJ, Olweny CLM. Quality of life studies: definitions and conceptual issues. In: Spilker B., editor. Quality of Life and Pharmacoeconomics in Clinical Trials. 2nd ed. Philadelphia, PA: Lippincot-Raven Publishers; 1996. pp. 11–24. [Google Scholar]
- 6.Hermann BP, Vickrey B., Hays RD et al. A comparison of health-related quality of life in patients with epilepsy, diabetes and multiple sclerosis. Epilepsy Res. 1996;25:113–118. doi: 10.1016/0920-1211(96)00024-1. [DOI] [PubMed] [Google Scholar]
- 7.Tabrizi FM, Radfar M. Fatigue, sleep quality, and disability in relation to quality of life in multiple sclerosis. Int J MS Care. 2015;17:268–274. doi: 10.7224/1537-2073.2014-046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sarraf P., Azizi S., Moghaddasi AN, Sahraian MA, Tafakhori A., Ghajarzadeh M. Relationship between sleep quality and quality of life in patients with multiple sclerosis. Int J Prev Med. 2014;5:1582–1586. [PMC free article] [PubMed] [Google Scholar]
- 9.Veauthier C., Gaede G., Radbruch H., Wernecke KD, Paul F. Sleep disorders reduce health-related quality of life in multiple sclerosis (Nottingham Health profile data in patients with multiple sclerosis) Int J Mol Sci. 2015;16:16514–16528. doi: 10.3390/ijms160716514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stanton BR, Barnes F., Silber E. Sleep and fatigue in multiple sclerosis. Mult Scler. 2006;12:481–486. doi: 10.1191/135248506ms1320oa. [DOI] [PubMed] [Google Scholar]
- 11.Braley TJ, Segal BM, Chervin RD. Obstructive sleep apnea and fatigue in patients with multiple sclerosis. J Clin Sleep Med. 2014;10:155–162. doi: 10.5664/jcsm.3442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Merlino G., Fratticci L., Lenchig C. et al. Prevalence of ‘poor sleep’ among patients with multiple sclerosis: an independent predictor of mental and physical status. Sleep Med. 2009;10:26–34. doi: 10.1016/j.sleep.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Brass SD, Li C-S, Auerbach S. The underdiagnosis of sleep disorders in patients with multiple sclerosis. J Clin Sleep Med. 2014;10:1025–1031. doi: 10.5664/jcsm.4044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Viana P., Rodrigues E., Fernandes C. et al. InMS: chronic insomnia disorder in multiple sclerosis: a Portuguese multicentre study on prevalence, subtypes, associated factors and impact on quality of life. Mult Scler Relat Disord. 2015;4:477–483. doi: 10.1016/j.msard.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 15.Baron KG, Corden M., Jin L., Mohr DC. Impact of psychotherapy on insomnia symptoms in patients with depression and multiple sclerosis. J Behav Med. 2011;34:92–101. doi: 10.1007/s10865-010-9288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Song ML, Oldham MA, Park KM, Lee ES, Lee HB, Cho YW. Comparison of impact of insomnia on depression and quality of life in restless legs syndrome/Willis-Ekbom disease and primary insomnia patients. Sleep Med. 2015;16:1403–1408. doi: 10.1016/j.sleep.2015.06.019. [DOI] [PubMed] [Google Scholar]
- 17.Bjornsdottir E., Benediktsdottir B., Pack AI et al. The prevalence of depression among untreated obstructive sleep apnea patients using a standardized psychiatric interview. J Clin Sleep Med. 2016;12:105–112. doi: 10.5664/jcsm.5406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akashiba T., Kawahara S., Akahoshi T. et al. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest. 2002;122:861–865. doi: 10.1378/chest.122.3.861. [DOI] [PubMed] [Google Scholar]
- 19.Leonavicius R., Adomaitiene V. Features of sleep disturbances in multiple sclerosis patients. Psychiatr Danub. 2014;26:249–255. [PubMed] [Google Scholar]
- 20.Feinstein A. Mood disorders in multiple sclerosis and the effects on cognition. J Neurol Sci. 2006;245:63–66. doi: 10.1016/j.jns.2005.08.020. [DOI] [PubMed] [Google Scholar]
- 21.Labuz-Roszak B., Kubicka-Baczyk K., Pierzchala K. et al. Quality of life in multiple sclerosis: association with clinical features, fatigue and depressive syndrome [in Polish] Psychiatr Pol. 2013;47:433–442. [PubMed] [Google Scholar]
- 22.Katzan I., Speck M., Dopler C. et al. The Knowledge Program: an innovative, comprehensive electronic data capture system and warehouse. AMIA Annu Symp Proc. 2011;2011:683–692. [PMC free article] [PubMed] [Google Scholar]
- 23.Kroenke K., Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.EuroQol Group EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 25.Sivertsen B., Salo P., Mykletun A. et al. The bidirectional association between depression and insomnia: the HUNT study. Psychosomc Med. 2012;74:758–765. doi: 10.1097/PSY.0b013e3182648619. [DOI] [PubMed] [Google Scholar]
- 26.Lustberg L., Reynolds CF. Depression and insomnia: questions of cause and effect. Sleep Med Rev. 2000;4:253–262. doi: 10.1053/smrv.1999.0075. [DOI] [PubMed] [Google Scholar]
- 27.Braley TJ, Boudreau EA. Sleep disorders in multiple sclerosis. Curr Neurol Neurosci Rep. 2016;16:50. doi: 10.1007/s11910-016-0649-2. [DOI] [PubMed] [Google Scholar]
- 28.Loube DI, Gay PC, Strohl KP, Pack AI, White DP, Collop NA. Indications for positive airway pressure treatment of adult obstructive sleep apnea patients: a consensus statement. Chest. 1999;115:863–866. doi: 10.1378/chest.115.3.863. [DOI] [PubMed] [Google Scholar]
- 29.Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379:1129–1141. doi: 10.1016/S0140-6736(11)60750-2. [DOI] [PubMed] [Google Scholar]


