Abstract
Background:
Multiple sclerosis (MS) is a neurologic disease that results in balance and mobility impairments that are associated with elevated fall risk. One common patient-reported outcome measure of balance is the 16-item Activities-specific Balance Confidence (ABC) scale. The ABC scale is valid and reliable in assessing balance confidence in people with MS. However, a shorter, six-question version of the ABC scale, the ABC-6 scale, has been proposed to save time in a clinical setting. Thus, we assessed the convergent validity and internal consistency reliability of the ABC-6 scale in people with MS.
Methods:
A total of 221 participants were included in this secondary analysis to compare the ABC-6 scale with the ABC scale. Convergent validity and internal consistency reliability were applied to participants based on fall history and physiological fall risk.
Results:
Statistical analysis indicated a main effect of group of the ABC and ABC-6 scales (P < .001). Both scales showed good to very good internal consistency (Cronbach α range, 0.832–0.975) and good reliability (intraclass correlation coefficient score range, 0.888–0.941). Furthermore, both versions had moderate convergent validity. Sensitivity ranged from 30% to 97%, and specificity ranged from 64% to 100% across groups tested.
Conclusions:
The ABC and ABC-6 scales demonstrated good internal consistency reliability and moderate convergent validity in predicting balance confidence in people with MS. However, poor sensitivity of both versions in distinguishing between MS groups at risk for falls may call into question the usefulness of this self-report measure.
Keywords: Accidental falls, Activities-specific Balance Confidence scale, Balance, Multiple sclerosis (MS), Posture, Questionnaires
Multiple sclerosis (MS) is a common neurologic disease that presents with intermittent occurrences of inflammation, demyelination, and axonal injury in the central nervous system.1 This neuronal damage results in numerous impairments, including muscular weakness, spasticity, and balance deficits.2,3 The various physical impairments caused by MS are linked to various adverse consequences, including reduced quality of life and falls.4
Given the importance of balance to functioning, researchers have examined the validity of various measures of balance in persons with MS. This research has revealed numerous valid approaches to assess balance, including force platforms, clinical assessments such as the Berg Balance Scale, and patient-reported outcome measures.5–8 Force platforms are able to quantify small amounts of postural sway, but they are expensive and require space and data processing expertise.5,6,8 Clinical assessments are used to evaluate the subcomponents that underlie postural control, but they may require clinical expertise to administer.5–8 Patient-reported outcome measures are inexpensive, are used to identify whether a balance problem exists, and have been proved reliable and valid in assessing a person's balance.5,6,8 One common self-report measure used to evaluate balance confidence is the 16-question Activities-specific Balance Confidence (ABC) scale.6,9–11 Balance confidence is important to assess because lower balance confidence has been shown to predict future falls.12 The ABC scale asks individuals to self-report their balance confidence in successfully performing 16 specific movement activities of varied balance difficulty.11
The ABC scale has been found to be reliable and valid in people with MS.13–17 Furthermore, the ABC scale has moderate-to-good concurrent convergent validity compared with various clinical and biomechanical balance tests, and it has been found to discriminate between people with MS with and without a history of falling.18 The ABC scale can take 5 to 20 minutes to administer. This time commitment has been considered a constraint in the clinical setting; thus, it has been suggested that a shorter version of the ABC scale may be advantageous to assess balance confidence.19 A short, six-question version of the ABC scale, the ABC-6 scale, has been established and found to be valid and reliable in people with higher-level gait disorders and those with Parkinson disease.19 These six tasks were determined through item reduction in a previous study and indicated the highest fear of falling.19 The ABC-6 scale has individuals report their balance confidence in the six most challenging tasks of the ABC scale: standing on tiptoes and reaching for something overhead, standing on a chair to reach for something, being bumped into by people while walking through a mall, stepping off an escalator holding onto the railing, stepping off an escalator without holding onto the railing, and walking on an icy sidewalk. These tasks correspond to questions 5, 6, 13, 14, 15, and 16 of the ABC scale. Given differences in MS and other neurologic impairments, it is unclear whether the ABC-6 scale will be valid and reliable in this specific population.
The objective of the present analysis was to evaluate the convergent validity and internal consistency reliability of the ABC-6 scale compared with the ABC scale in individuals with MS and controls. As balance confidence relates to fall risk and predicting future falls, fall risk was examined retrospectively through a person's fall history and prospectively via physiological functioning as indexed by the Physiological Profile Assessment (PPA).20–22 The PPA is a test that uses visual contrast sensitivity, lower-limb proprioception, knee extension strength, finger press reaction time, and sway on a foam surface to compute a physiological fall risk score; lower scores indicate lower fall risk, and higher scores indicate higher fall risk.21,22 Furthermore, the PPA has been shown to differentiate between fallers and nonfallers in people with MS.21–24 To determine whether the ABC-6 scale has convergent validity, its ability to distinguish between individuals with MS with and without a history of falls and controls, as well as between individuals with MS with above-average and below-average physiological fall risk and controls, was determined through bivariate correlation. Internal consistency reliability was assessed using the Cronbach α, and intraclass correlation coefficients (ICCs) were used to examine the relationship between the ABC and ABC-6 scales.
Methods
Study Design and Participants
A secondary analysis of baseline data collected in various investigations was conducted.25,26 All the studies were approved by the local institutional review board. Data from 221 participants were included. Overall, 144 individuals had a physician-confirmed diagnosis of MS, and 77 were controls who did not have MS, other neurologic disorders, or musculoskeletal conditions that may affect walking and balance. To be included in the analysis, participants had to self-report ambulation with or without an assistive device and having normal or corrected-to-normal vision and hearing. All the participants provided demographic information, including age and sex; participants also completed a survey on the number of falls sustained in the past 3 months. In addition, all the participants completed the ABC scale. The ABC scale was administered by trained members of the research laboratory as part of various research studies. Participants were given standardized instructions to record their balance confidence of doing the 16 different conditions of the ABC scale and were asked to record their responses for each condition.11 If a participant had no balance confidence for a given item/task, they were instructed to rate that item as 0%. If a participant had complete balance confidence, they were instructed to rate that item as 100%. A subsample of participants (97 with MS and 54 controlsPPA) also completed the short version of the PPA.11,21,22
Data Analysis
Evaluating fall risk is complex and requires a multidimensional approach. To evaluate the internal consistency reliability and convergent validity of the ABC-6 scale in people with MS, several distinct analyses were conducted. Data analysis was based on previous work, which established the validity of the ABC-6 scale in various clinical populations.19 The participant ratings of the six conditions of the ABC-6 scale were extracted from the participants' responses on the ABC scale.
All the analyses were completed using IBM SPSS Statistics for Windows, version 24.0 (IBM Corp, Armonk, NY). Descriptive statistics as a function of group were completed and included age, sex, number of falls in the past 3 months, and PPA scores.
Furthermore, mean ± SD ABC and ABC-6 scale scores were calculated. Each item of the ABC scale was further evaluated using the 25th percentile scores. The 25th percentile scores represent the lowest balance confidence (highest fear of falling) of the groups.19 The mean ABC and ABC-6 scale scores and participant demographic features were compared using a one-way analysis of variance. Internal consistency reliability was determined using the Cronbach α, and the ICC(2,k) was used to compare the ABC and ABC-6 scales. Convergent validity was examined through Pearson correlation values to compare the ABC and ABC-6 scales across groups. Sensitivity and specificity were calculated by comparing the results of any two groups per analysis using logistic regression and receiver operating characteristic curves. Sensitivity and specificity were interpreted as good for values from 75% to 100%, as moderate for values from 50% to 74%, and as poor for values less than 50%.27
First, convergent validity and internal consistency reliability were determined by grouping participants by fall history given that a history of falls is a common indicator of future falls.9 For this analysis, participant data were separated into three distinct groups: individuals with MS who have fallen two or more times in the previous 3 months (MS fallers), individuals with MS who have not fallen more than once in the past 3 months (MS nonfallers), and controls who do not have MS or a fall history.
A different, objective measure of future fall risk is the PPA, which uses quantifiable measures of physiological function.22 Previous research reported that individuals with MS and a PPA score of 2.3 or greater had one or more falls in a 3-month follow-up period.22 Thus, a cutoff score of 2.3 was used to differentiate between individuals with higher and lower physiological fall risk.22 Participants who completed the PPA were divided into three distinct groups: 1) high physiological fall risk—individuals with MS with PPA scores 2.3 or greater; 2) low physiological fall risk—individuals with MS with PPA scores less than 2.3; and 3) controlsPPA.
Results
Participant Demographics
Data from 221 participants were included in the secondary baseline analysis; of the sample, 151 participants (97 patients with MS and 54 controls) completed the PPA. Table 1 displays the participant demographic characteristics stratified by fall history and physiological function. Comparative mean testing of the fall groups revealed significant differences in age (F = 8.370, P < .0001). Post hoc Tukey analysis revealed that the control group was significantly older than the MS nonfaller group (P < .001) but not the MS faller group (P <.06). The mean age of the MS nonfaller group and that of the MS faller group were not significantly different (P = .491). Similarly, comparative mean testing of the physiological function groups revealed significant differences between the ages of the physiological function groups (F = 8.352, P < .0001). Post hoc Tukey analysis revealed that the control group was significantly older than the low physiological fall risk group (P < .001) but not the high physiological fall risk group (P < .07).
Table 1.
Participant demographic characteristics stratified by fall history and physiological function

ABC Scale Characteristics
Table 2 displays the ABC and ABC-6 scale scores as a function of group. Statistical analysis revealed a main effect of group for both versions of the scale. Post hoc analysis of the fall history groups revealed a significant difference between the groups for the ABC and ABC-6 average score, with the control group having a higher score than the MS nonfallers and MS fallers (P < .001). Furthermore, post hoc analysis of the physiological function groups revealed significant differences between the groups for the ABC average score (P = .029) but not for the ABC-6 average score (P = .165).
Table 2.
ABC and ABC-6 scale scores for fall history and physiological function

Figure 1 represents the 25th percentile data for each of the 16 items of the ABC scale based on the fall history groups. There was a significant difference (P < .05) between all fall history groups for individual items of the ABC-6 scale. Figure 2 represents the 25th percentile data for each of the 16 items of the ABC scale based on the physiological function groups. There was a significant difference (P < .05) between all the physiological function groups for individual items of the ABC-6 scale.
Figure 1.
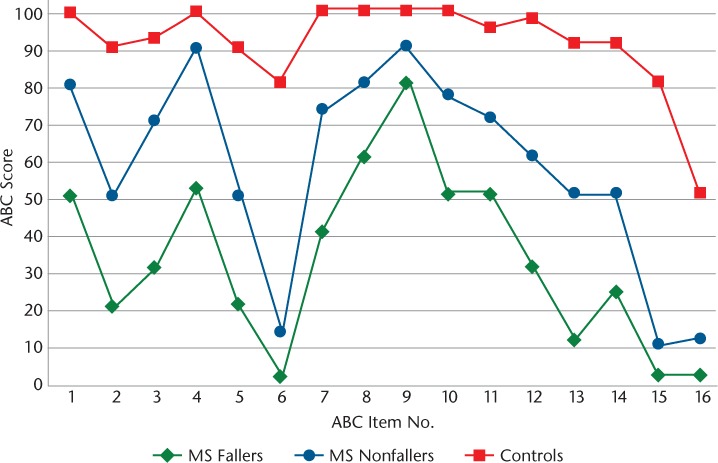
The 25th percentile values for each of the 16 items of the Activities-specific Balance Confidence (ABC) scale based on fall history
Figure 2.
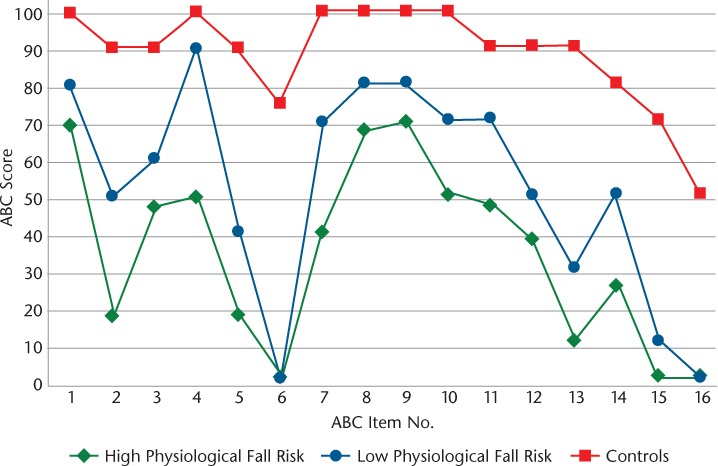
The 25th percentile values for each of the 16 items of the Activities-specific Balance Confidence (ABC) scale based on physiological fall risk
Internal Consistency Reliability
Both scales showed good to very good internal consistency, with a Cronbach α ranging from 0.904 to 0.975 for the ABC scale and from 0.832 to 0.920 for the ABC-6 scale (Table 3). Interclass correlation analysis revealed a good relationship for the short version (ABC-6) compared with the full version (ABC). The MS fallers had an ICC score of 0.888; MS nonfallers, 0.941; and controls, 0.913. For the physiological function groups, the ICC score of the high physiological fall risk group was 0.906, of the low physiological fall risk group was 0.942, and of the controlsPPA was 0.911.
Table 3.
Internal consistency reliability of ABC and ABC-6 scales

Convergent Validity, Sensitivity, and Specificity
Convergent validity analysis revealed a moderate negative Pearson correlation based on the number of falls and the ABC scale score (r = −0.642, P < .001) and the ABC-6 scale score (r = −0.647, P < .001). Furthermore, convergent validity analysis also showed a moderate negative Pearson correlation of the PPA score and the ABC scale score (r = −0.565, P < .001) and the ABC-6 scale score (r = −0.560, P < .001). Table 4 displays the sensitivity and specificity values for both versions.
Table 4.
Sensitivity and specificity of ABC and ABC-6 scales

The ABC scale and the ABC-6 scale had specificity values greater than 97% and sensitivity values greater than 79% comparing participants with MS and a high fall risk (MS fallers and the high fall risk group) with controls. Furthermore, the specificity values for both versions comparing participants with MS and low fall risk (MS nonfallers and the low fall risk group) with controls were greater than 87%, yet the sensitivity values were less than 45%. In addition, sensitivity values were less than 45% and specificity values were less than 76% comparing between MS groups (MS nonfallers with MS fallers and the low fall risk group with the high fall risk group).
Discussion
The purpose of this study was to examine the convergent validity and internal consistency reliability of a short, six-question version (ABC-6 scale) of the ABC scale in a diverse sample of individuals with MS. The current investigation found that the ABC-6 had moderate convergent validity and internal consistency reliability to the full ABC scale. Both versions had good sensitivity and specificity in distinguishing between MS fallers and controls, as well as the high fall risk group and conditions. However, there is only moderate specificity and poor sensitivity in distinguishing between MS groups.
Assessing balance confidence is an important factor in fall risk assessment.12 Previous research has demonstrated that the ABC scale is a valid measure of balance confidence in individuals with MS and is able to discriminate between multiple fallers and nonfallers.18 The mean ABC scale scores for the current MS and control groups were consistent with previous research.11,18,19,28 The results of the present investigation reveal that the internal consistency of the ABC-6 scale was similar to that of the ABC scale and to reports in Parkinson disease and higher-level gait disorders.19 In addition, the results of the present study demonstrated that both versions had moderate convergent validity, which is similar to past research that has shown that the ABC scale has moderate convergent validity differentiating between individuals with MS who do and do not fall.18
The ABC and ABC-6 scales had good sensitivity and specificity in distinguishing MS participants with a high fall risk from controls. Indeed, these findings indicate that both versions are capable of differentiating balance confidence in persons with a high likelihood of falling from that in individuals without a high likelihood of falling. These findings are similar to those of past research.19 The ABC-6 has been shown to have sensitivity greater than 91% comparing patients with higher-level gait disorder with controls and patients with higher-level gait disorder with those with Parkinson disease.19 Furthermore, sensitivity and specificity were similar for both scales across all groups tested. Nevertheless, there was poor sensitivity for both versions comparing participants with MS and a low fall risk with participants with MS and a high fall risk; these findings may suggest that the ABC scale and the ABC-6 scale may not be specific enough to the unique impairments of individuals with MS. Consequently, the development of an MS-specific balance confidence scale may be warranted.
Moreover, certain conditions of the ABC scale were not able to distinguish between groups. Indeed, item 2 asking about balance confidence when walking up or down stairs seems to result in a different response in people with MS than in other clinical populations.19 In addition, question 6, which asks about balance confidence when standing on a chair, seems to be unable to differentiate between MS groups based on fall history or physiological function.
This study is not without limitations. It may be limited due to the nature of the secondary analysis and participant confidentiality; participants may have completed more than one of the studies included. The present study may also be limited by recall bias due to the use of retrospective fall data.29 Furthermore, the ABC-6 scale scores were extracted from participants' responses to the corresponding questions on the ABC scale; time to complete the questionnaire was not recorded, which may limit the findings.
The purpose of this investigation was to examine the convergent validity and internal consistency reliability of the ABC-6 scale compared with the ABC scale. Both versions had moderate convergent validity and good internal consistency reliability in measuring balance confidence in people with MS. Although both versions are capable of distinguishing between individuals with MS at high fall risk and controls, the questionnaires—regardless of the number of items—have poor sensitivity and only moderate specificity in distinguishing between MS groups. The sensitivity and specificity values call into question the practical usefulness of this self-report of balance confidence in people with MS. These findings indicate that the ABC-6 scale may be used in the same manner as the ABC scale in individuals with MS, and it can be assumed that with fewer questions it will take less time to complete the questionnaire. However, clinicians and researchers may need to be wary of using either version to assess balance confidence as it relates to fall risk in people with MS.
PRACTICE POINTS
MS may result in balance impairments, falls, and reduced quality of life; thus, it is important to have a measure of balance confidence.
A common self-report measure is the 16-question Activities-specific Balance Confidence (ABC) scale, which requires reporting balance confidence in successfully performing 16 specific movement activities of varied balance difficulty. However, the time to complete the ABC scale has been considered a hindrance in the clinical setting; thus, a shorter, six-question version has been suggested (ABC-6 scale).
The ABC and ABC-6 scales have been found to have internally consistent reliability and moderate convergent validity in people with MS, yet there is poor sensitivity in distinguishing between balance confidence of MS groups and fall risk. Thus, clinicians and researchers who work with people with MS should be aware of the potential limitations of the ABC and ABC-6 scales as related to fall risk.
Financial Disclosures:
The authors declare no conflicts of interest.
Funding/Support:
This project was funded in part by the National Multiple Sclerosis Society (ILLOT006 and ILLOT0018) and MC10 Inc.
References
- 1.Hemmer B., Nessler S., Zhou D., Kieseier B., Hartung HP. Immunopathogenesis and immunotherapy of multiple sclerosis. Nat Clin Pract Neurol. 2006;2:201–211. doi: 10.1038/ncpneuro0154. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Multiple Sclerosis International Federation Atlas: Multiple Sclerosis Resources in the World. Geneva: World Health Organization; 2008. [Google Scholar]
- 3.Bjartmar C., Trapp BD. Axonal and neuronal degeneration in multiple sclerosis: mechanisms and functional consequences. Curr Opin Neurol. 2001;14:271–278. doi: 10.1097/00019052-200106000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Sosnoff JJ, Socie MJ, Boes MK et al. Mobility, balance and falls in persons with multiple sclerosis. PLoS One. 2011;6 doi: 10.1371/journal.pone.0028021. e28021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin CC, Whitney SL. Quantification of static and dynamic balance while maintaining and changing body position. Top Geriatr Rehabil. 2012;28:17–26. [Google Scholar]
- 6.Mancini M., Horak FB. The relevance of clinical balance assessment tools to differentiate balance deficits. EurJ Phys Rehabil Med. 2010;46:239–248. [PMC free article] [PubMed] [Google Scholar]
- 7.Boulgarides LK, McGinty SM, Willett JA, Barnes CW. Use of clinical and impairment-based tests to predict falls by community-dwelling older adults. Phys Ther. 2003;83:328–339. [PubMed] [Google Scholar]
- 8.Horak FB. Clinical assessment of balance disorders. Gait Posture. 1997;6:76–84. [Google Scholar]
- 9.Cameron MH, Thielman E., Mazumder R., Bourdette D. Predicting falls in people with multiple sclerosis: fall history is as accurate as more complex measures. Mult Scler Int. 2013;2013 doi: 10.1155/2013/496325. 496325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perrochon A., Holtzer R., Laidet M. et al. Postural control is associated with cognition and fear of falling in patients with multiple sclerosis. J Neural Transm (Vienna) 2017;124:495–500. doi: 10.1007/s00702-016-1668-5. [DOI] [PubMed] [Google Scholar]
- 11.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A:M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 12.Landers MR, Oscar S., Sasaoka J., Vaughn K. Balance confidence and fear of falling avoidance behavior are most predictive of falling in older adults: prospective analysis. Phys Ther. 2016;96:433–442. doi: 10.2522/ptj.20150184. [DOI] [PubMed] [Google Scholar]
- 13.Mercan F., Kara B., Tiftikcioglu BI, Mercan E., Sertpoyraz FM. Effects of motor-motor and motor-cognitive tasks on balance in patients with multiple sclerosis. Mult Scler Relat Disord. 2016;7:85–91. doi: 10.1016/j.msard.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 14.Garg H., Bush S., Gappmaier E. Associations between fatigue and disability, functional mobility, depression, and quality of life in people with multiple sclerosis. Int J MS Care. 2016;18:71–77. doi: 10.7224/1537-2073.2015-013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sebastiao E., Sandroff BM, Learmonth YC, Motl RW. Validity of the Timed Up and Go test as a measure of functional mobility in persons with multiple sclerosis. Arch Phys Med Rehabil. 2016;97:1072–1077. doi: 10.1016/j.apmr.2015.12.031. [DOI] [PubMed] [Google Scholar]
- 16.Cattaneo D., Regola A., Meotti M. Validity of six balance disorders scales in persons with multiple sclerosis. Disabil Rehabil. 2006;28:789–795. doi: 10.1080/09638280500404289. [DOI] [PubMed] [Google Scholar]
- 17.Cattaneo D., Jonsdottir J., Repetti S. Reliability of four scales on balance disorders in persons with multiple sclerosis. Disabil Rehabil. 2007;29:1920–1925. doi: 10.1080/09638280701191859. [DOI] [PubMed] [Google Scholar]
- 18.Nilsagard Y., Carling A., Forsberg A. Activities-specific balance confidence in people with multiple sclerosis. Mult Scler Int. 2012;2012 doi: 10.1155/2012/613925. 613925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peretz C., Herman T., Hausdorff JM, Giladi N. Assessing fear of falling: can a short version of the Activities-specific Balance Confidence scale be useful? Mov Disord. 2006;21:2101–2105. doi: 10.1002/mds.21113. [DOI] [PubMed] [Google Scholar]
- 20.Cameron MH, Thielman E., Mazumder R., Bourdette D. Predicting falls in people with multiple sclerosis: fall history is as accurate as more complex measures. Mult Scler Int. 2013;2013 doi: 10.1155/2013/496325. 496325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lord SR, Delbaere K., Gandevia SC. Use of a physiological profile to document motor impairment in ageing and in clinical groups. J Physiol. 2016;594:4513–4523. doi: 10.1113/JP271108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoang PD, Baysan M., Gunn H. et al. Fall risk in people with MS: a Physiological Profile Assessment study. Mult Scler J Exp Transl Clin. 2016;2 doi: 10.1177/2055217316641130. 2055217316641130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoang PD, Cameron MH, Gandevia SC, Lord SR. Neuropsychological, balance, and mobility risk factors for falls in people with multiple sclerosis: a prospective cohort study. Arch Phys Med Rehabil. 2014;95:480–486. doi: 10.1016/j.apmr.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 24.Hoang P., Schoene D., Gandevia S., Smith S., Lord SR. Effects of a home-based step training programme on balance, stepping, cognition and functional performance in people with multiple sclerosis: a randomized controlled trial. Mult Scler. 2016;22:94–103. doi: 10.1177/1352458515579442. [DOI] [PubMed] [Google Scholar]
- 25.Sosnoff JJ, Moon Y., Wajda DA et al. Fall risk and incidence reduction in high risk individuals with multiple sclerosis: a pilot randomized control trial. Clin Rehabil. 2015;29:952–960. doi: 10.1177/0269215514564899. [DOI] [PubMed] [Google Scholar]
- 26.Moon Y., McGinnis RS, Seagers K. et al. Monitoring gait in multiple sclerosis with novel wearable motion sensors. PLoS One. 2017;12 doi: 10.1371/journal.pone.0171346. e0171346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Starkey C., Brown SD, Ryan J. Examination of Orthopedic and Athletic Injuries. 3rd ed. Philadelphia, PA: FA Davis; 2009. Evidence-based practice in the diagnostic process. [Google Scholar]
- 28.Gandolfi M., Munari D., Geroin C. et al. Sensory integration balance training in patients with multiple sclerosis: a randomized, controlled trial. Mult Scler. 2015;21:1453–1462. doi: 10.1177/1352458514562438. [DOI] [PubMed] [Google Scholar]
- 29.Nilsagard Y., Lundholm C., Denison E., Gunnarsson LG. Predicting accidental falls in people with multiple sclerosis: a longitudinal study. Clin Rehabil. 2009;23:259–269. doi: 10.1177/0269215508095087. [DOI] [PubMed] [Google Scholar]


