Abstract
Objective
The purpose of this study was to determine if the standardization of using liposomal bupivacaine in transversus abdominis plane (LB TAP) blocks eliminated the benefit of intrathecal morphine (ITM) in patients after undergoing a cesarean section.
Methods
This was a retrospective review of 358 patients who underwent cesarean section over an 11-month period. Patients were divided into two groups: those who received only an LB TAP (67 patients) vs those who received an LB TAP and ITM (291 patients). All blocks were placed bilaterally under ultrasound guidance after closure of the surgical incision, and morphine was added to the spinal used for the case.
Results
The group that received ITM in addition to the LB TAP received less opioids in the first 24 hours (median 5 range 0–150 mg morphine equivalents [ME] vs 15 range 0–76 mg ME; P<0.001) and less opioids overall (35 mg range 0–450 mg ME vs 47.5 mg range 0–189 mg ME; P=0.041) when compared to the LB TAP block only group. There was no difference between the two groups in opioid use from 24 to 48 hours or 48 to 72 hours.
Conclusion
Patients who received ITM in addition to an LB TAP block received less opioids in the first 24 hours and overall when compared to those who received an LB TAP alone. This suggests that ITM still plays a role in providing analgesia to patients who have also received an LB TAP block as a part of their multimodal pain regimen for cesarean sections.
Keywords: obstetric anesthesia, acute pain, regional anesthesia, obstetric surgery
Introduction
Effective and safe pain management is an important aspect of perioperative care of women undergoing cesarean sections. Poor pain control is associated with suboptimal outcomes and recovery.1 Such outcomes include delayed function, increased risks for postpartum depression, suboptimal breastfeeding, and increased risk of developing persistent pain.1 Infiltration of local anesthetic via the transversus abdominis plane (TAP) block has been employed as a means to produce analgesia following cesarean section.1,2 While research has shown the benefit (reduced postoperative pain and opioid use) of plain bupivacaine TAP blocks after cesarean section performed without intrathecal opioids, the benefit of TAP blocks have been diminished when intrathecal opioids have been employed.2–4 For this reason, it is not considered the standard of care to perform TAP blocks when intrathecal opioids have been used.
Liposomal bupivacaine (Pacira Pharmaceuticals, Inc., Parsippany, NJ, USA) is a multivesicular formulation of 1.3% bupivacaine that allows for the gradual release of bupivacaine from liposomes and can produce clinically significant reduction in pain for up to 72 hours.5 Once released from the liposomes, the mechanism of action, pharmacokinetics, pharmacodynamics, metabolism, and elimination follows that of standard bupivacaine. Several studies have compared 0.25% bupivacaine vs liposomal bupivacaine infiltration in TAP blocks and in abdominal wound infiltration showing varying degrees of benefit when using liposome bupivacaine.6–10 However, there has been no study evaluating the benefit of TAP blocks employing liposome bupivacaine in the context of cesarean section patients receiving intrathecal opioid. The objective of this study was to determine if intrathecal morphine (ITM) provided additional benefit in patients receiving a liposomal bupivacaine in transversus abdominis plane (LB TAP) blocks following cesarean sections.
Methods
This was a University of Minnesota IRB exempt study (1507 M76081), since the design was retrospective review of a limited data set. All patient data were confidentially maintained in a secured server, and there is no clinical trial identifier for this study. We do not intend to share any de-identified data. Patients’ charts were reviewed for a period of 11 months from July 1, 2015 to May 31, 2016. During this period, LB TAP blocks were standard of care for postoperative pain relief at our institution for all patients undergoing cesarean section. All patients who had an LB TAP block and a spinal for cesarean section were included in this study. LB TAP blocks were all performed under ultrasound guidance, and all received the standard dose of 20 mL of 0.25% bupivacaine, 20 mL of 1.3% liposomal bupivacaine, and 20 mL of saline (divided into each side). Patients were divided into two groups on whether or not they received ITM (in their spinal for the surgery) based on contraindications (eg, allergy), patient refusal (eg, prior exposure to itching/nausea), or anesthesiologist’s discretion. The first group was those who had an LB TAP block without ITM (LB TAP group). The second group (LB TAP plus ITM group) was those who had an LB TAP block and ITM dose range of 100–400 µg. Intrathecal fentanyl was allowed in either group (physician choice), but any cases getting a general anesthetic or epidural for regional anesthesia were excluded. Patients with an opioid use greater than 3 weeks prior to surgery, or with a chronic pain diagnosis, were also excluded. All patients received multimodal analgesic regimen with all receiving acetaminophen, ketorolac, or ibuprofen postoperatively, unless contraindicated. The dose range of per dose of acetaminophen was 325–1,000 mg, dose range of ketorolac was 15–30 mg, and dose range of ibuprofen was 600–800 mg. The primary objective for this study was total morphine equivalents (ME) used from 0 to 72 hours. The secondary outcomes for this study were ME used in the first 24 hours, pain intensity and pain medication use, length of surgery, length of stay, and presence of nausea/vomiting.
Data that were abstracted from the electronic medical chart included age, weight, body mass index (BMI), and American Society of Anesthesiologists Physical Status Classification System, intraoperative characteristics, such as length of surgery, estimated blood loss (EBL), intrathecal opioids, and intrathecal non-opioid pain medications. Postoperative characteristics that were obtained were daily opioids, daily acetaminophen, daily NSAIDs, daily pain scores, length of stay, and presence of any nausea or vomiting postoperatively. All patients were given opioids, acetaminophen, and NSAIDs for postoperative pain relief. Any complications or adverse events were also recorded. Pain scores were assessed by bedside nurses at minimum of once per shift. The highest and lowest for each 24-hour time period were analyzed. Pain scores are analyzed via the clinically aligned pain assessment tool (CAPA©) as is standard for all patients in our hospital system.11 This was then converted to an 11-point (0–10) comfort, pain, and function scale. All intravenous and oral opioid use were normalized to milligrams of intravenous morphine using standard conversions.12
All continuous outcomes (besides age, weight, and BMI) were not normally distributed (P<0.05 for Shapiro–Wilk test for normality); therefore, comparisons between the groups used the robust, non-parametric Kruskal–Wallis test. Comparing the LB TAP plus ITM and LB TAP only groups for nausea/vomiting at any point postsurgery up to 72 hours and were completed using a chi-squared test. Age, weight, and BMI were analyzed using a Student’s t-test. P-values are not adjusted for multiple comparisons and should be interpreted cautiously. All analyses completed with R version 3.3.1.
Results
Three hundred fifty-eight patients were included in the analysis of this study. There were 291 in the LB TAP plus ITM group and 67 in the LB TAP group. There were no significant differences between the two groups in terms of patient age, weight, BMI, length of surgery, and EBL (Table 1).
Table 1.
Surgical and patient characteristics
| Outcomes | LB TAP plus ITM median (min–max) or mean (SD) | LB TAP only median (min–max) or mean (SD) | P-value |
|---|---|---|---|
| Length of surgery (minutes) | 48.0 (9–137) N=291 |
48.0 (7–86) N=65 |
0.661 |
| Length of stay (hours) | 78.9 (25–1,291) N=291 |
87.0 (46–681) N=67 |
0.046 |
| EBL (mL) | 800 (500–2,000) N=289 |
900 (500–2,500) N=67 |
0.060 |
| Age (years) | 32.39 (4.99) N=291 |
31.93 (6.03) N=67 |
0.508 |
| BMI (kg/m2) | 32.11 (7.59) N=243 |
32.38 (6.43) N=58 |
0.802 |
| Weight (kg) | 84.31 (19.21) N=281 |
84.92 (20.41) N=66 |
0.818 |
Notes: P-values for length of surgery, length of stay, and EBL were generated using a non-parametric Kruskal–Wallis test. P-values for age, weight, and BMI were generated using a Student’s t-test.
Abbreviations: BMI, body mass index; EBL, estimated blood loss; ITM, intrathecal morphine; LB, liposome bupivacaine; N, number of patients; LB TAP, liposomal bupivacaine in, transversus abdominis plane.
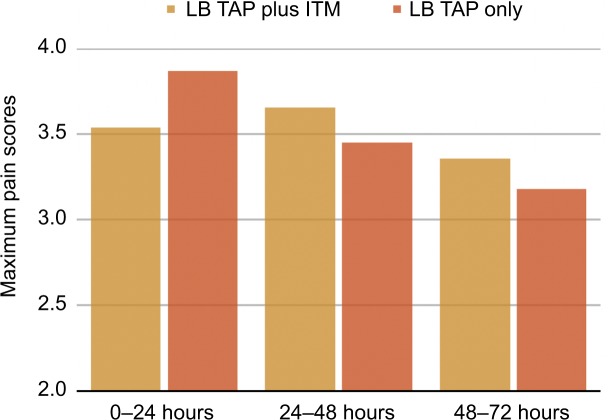
We found a significant reduction in total ME usage for the LB TAP plus ITM group over the 0–72 hours (35 range 0–450 mg ME vs 47.5 range 0–189 mg ME; P=0.041), as well as the first 24 hours (median 5 range 0–150 mg ME vs 15 range 0–76 mg ME; P<0.001). There was no difference between the two groups in ME from 24 to 48 and 48 to 72 hours (Table 2). Those in the LB TAP group used significantly more acetaminophen (1,950 mg, range 0–3,900 mg) from 0 to 24 hours compared to the LB TAP plus ITM group (1,150 mg, range 0–4,550 mg, Table 3). However, there was no difference in the amount of ketorolac, acetaminophen, or ibuprofen used at any of the other time points analyzed (0–24, 24–48, and 48–72 hours, Table 3). Additionally, no patients received any ketorolac from 48 to 72 hours. There was a significant reduction in length of stay for the LB TAP plus ITM group compared to the LB TAP group (median 78.9 range 25–1,291 vs 87 range 46–681 hours; P=0.046). Furthermore, there were no significant differences between the two groups in mean maximum pain scores at any of the time points analyzed (Figure 1). From 0 to 24 hours, the LB TAP plus ITM mean maximum pain score was 3.54±1.61 vs LB TAP 3.87±1.63 with P=0.123. From 24 to 48 hours, the LB TAP plus ITM mean maximum pain score was 3.66±1.49 vs LB TAP 3.45±1.36 with P=0.286. From 48 to 72 hours, the LB TAP plus ITM mean maximum pain score was 3.36±1.52 vs LB TAP 3.18±1.39 with P=0.420.
Table 2.
ME comparison between patients receiving LB TAP plus ITM vs those receiving an LB TAP only
| Time period (hours) | ME LB TAP plus ITM median (min–max) | ME LB TAP only median (min–max) | P-value |
|---|---|---|---|
| 0–24 | 5.0 (0–150) N=291 |
15.0 (0–76) N=67 |
<0.001 |
| 24–48 | 17.5 (0–150) N=291 |
22.5 (0–81) N=67 |
0.515 |
| 48–72 | 12.5 (0–150) N=291 |
15.0 (0–50) N=66 |
0.522 |
| 0–72 | 35.0 (0–450) N=291 |
47.5 (0–189) N=67 |
0.041 |
Notes: P-values were generated using a non-parametric Kruskal–Wallis test. N is number of patients.
Abbreviations: ITM, intrathecal morphine; LB TAP, liposomal bupivacaine in transversus abdominis plane; ME, morphine equivalents.
Table 3.
Non-opioid medication comparison between patients LB TAP plus ITM vs those receiving an LB TAP only
| Time period and drug (dose) | ME LB TAP plus ITM median (min–max) | ME LB TAP only median (min–max) | P-value |
|---|---|---|---|
| 0–24 hours Acetaminophen (mg) | 1,150 (0–4,550) N=254 |
1,950 (0–3,900) N=67 |
0.029 |
| 0–24 hours Ketorolac (mg) | 90 (0–120) N=254 |
90 (0–90) N=67 |
0.097 |
| 0–24 hours Ibuprofen (mg) | 0 (0–2,400) N=254 |
0 (0–1,600) N=67 |
0.524 |
| 24–48 hours Acetaminophen (mg) | 2,600 (0–3,900) N=254 |
2,600 (0–4,000) N=67 |
0.479 |
| 24–48 hours Ketorolac (mg) | 0 (0–90) N=254 |
0 (0–90) N=67 |
0.856 |
| 24–48 hours Ibuprofen (mg) | 2,400 (0–3,200) N=254 |
2,400 (0–3,200) N=67 |
0.151 |
| 48–72 hours Acetaminophen (mg) | 1,950 (0–3,900) N=254 |
1,950 (0–3,900) N=67 |
0.603 |
| 48–72 hours Ketorolac (mg) | 0 (0–0) | 0 (0–0) | n/a |
| 48–72 hours Ibuprofen (mg) | 2,400 (0–4,000) N=254 |
2,400 (0–3,200) N=67 |
0.842 |
| 0–72 hours Acetaminophen (mg) | 5,850 (0–10,400) N=254 |
6,175 (0–11,375) N=67 |
0.215 |
| 0–72 hours Ketorolac (mg) | 90 (0–150) N=254 |
90 (0–180) N=67 |
0.116 |
| 0–72 hours Ibuprofen (mg) | 4,800 (0–8,000) N=254 |
4,800 (0–8,000) N=67 |
0.783 |
Notes: P-values were generated using a non-parametric Kruskal–Wallis test. N is number of patients.
Abbreviations: ITM, intrathecal morphine; LB TAP, liposomal bupivacaine in transversus abdominis plane; ME, morphine equivalents.
Figure 1.
Maximum pain score comparison between patients receiving LB TAP plus ITM vs patients receiving LB TAP.
Notes: The number of patients analyzed for LB TAP plus ITM was 283 for 0–24 hours, 290 for 24–48 hours, and 255 for 48–72 hours. The number of patients analyzed for LB TAP only was 67 for 0–24 hours, 66 for 24–48 hours, and 57 for 48–72 hours.
Abbreviations: ITM, intrathecal morphine; LB TAP, liposomal bupivacaine in transversus abdominis plane.
We also found less nausea and vomiting in the LB TAP only group with 2 out of 67 (2.9%) reporting nausea or vomiting and 31 out of 291 (10.6%) reporting nausea in the LB TAP plus ITM group but the difference was non-significant (P=0.059).
The median ITM used was 0.2 mg (range 0.1–0.4). There were no patients in the LB TAP only group who received intrathecal fentanyl. There were, however, 37 patients in the IT morphine plus LB TAP group who received IT fentanyl. The median dose of IT fentanyl was 15.0 µg with range of 12.5–25.0 µg. No serious adverse events related to the TAP blocks or ITM use were noted in either group.
Additionally, the data were analyzed excluding the patients who received IT fentanyl. There were 254 patients in the LB TAP plus ITM (no IT fentanyl) group and 67 in the LA TAP only (no IT fentanyl) group. Results showed there was a statistical difference in opioid use between the LB TAP plus ITM (no IT fentanyl) vs LAP TAP only (no IT fentanyl) group from 0 to 24 hours (Table 4). There was no significant difference in opioid use from 24 to 48, 48 to 72 and 0 to 72 hours.
Table 4.
ME comparison between patients LB TAP plus ITM (no IT fentanyl) vs those receiving an LB TAP only
| Time period (hours) | ME LB TAP plus ITM median (min–max) | ME LB TAP only median (min–max) | P-value |
|---|---|---|---|
| 0–24 | 5.0 (0–150) N=254 |
15.0 (0–76) N=67 |
<0.001 |
| 24–48 | 17.5 (0–150) N=254 |
22.5 (0–81) N=67 |
0.578 |
| 48–72 | 12.5 (0–150) N=254 |
15.0 (0–50) N=66 |
0.614 |
| 0–72 | 35.0 (0–450) N=254 |
47.5 (0–189) N=67 |
0.056 |
Notes: P-values were generated using a non-parametric Kruskal–Wallis test. N is number of patients.
Abbreviations: LB TAP, liposomal bupivacaine in transversus abdominis plane; ITM, intrathecal morphine; ME, morphine equivalents.
Discussion
A systematic review and meta-analysis assessing the efficacy of TAP blocks in cesarean sections was done by Mishriky et al in 2012. From their nine studies that fit their inclusion criteria, they concluded when “Transversus abdominis plane block significantly improved postoperative analgesia in women undergoing CD who did not receive ITM but showed no improvement in those who received ITM.”15 This is the first study, however, comparing the use of ITM in the setting of patients receiving an LB TAP for postoperative analgesia after cesarean section. Our findings suggest that patients undergoing cesarean section with ITM and a postoperative LB TAP block had superior analgesia than an LB TAP along, based on significantly less ME over 24 hours, total ME over 72 hours and, while small, a statistically significantly shorter hospital stays. Thus, it suggests that even with a longer acting TAP block with liposomal bupivacaine, ITM is still beneficial. This 0 to 24-hour difference occurred despite the fact that the LB TAP group received more acetaminophen compared to the LB TAP plus ITM. The 0 to 24-hour and 0 to 72-hour difference was unchanged with or without the use of IT fentanyl. This suggests that the addition IT fentanyl did not contribute to the opiate reduction seen in the LB TAP plus ITM group from 0 to 24 hours and 0 to 72 hours.
Previous studies have clearly shown the analgesic benefit of LB TAPs over bupivacaine TAPs extending up to 72 hours postoperatively.7–10 Yet, despite the prolonged analgesic effect of LB TAP blocks vs regular bupivacaine TAP blocks, our results reinforce the need for the addition of ITM for maximal analgesic benefit. This was illustrated by the significant difference in opioid use for the first 24 hours (when the ITM was working with the LB TAP blocks) and then non-significant difference for the time period of 24–48 and 48–72 hours when only the LB TAP block was providing analgesia. This could be due to the visceral component of postoperative recovery from cesarean section which typically occurs within the first 24 hours after surgery. While TAP blocks can provide excellent somatic analgesia, they are inherently limited from a visceral benefit.
The quadratus lumborum block has a putative benefit to visceral pain (in addition to somatic) that may further assist in visceral pain management in cesarean patients. The benefit of a quadratus lumborum block for post cesarean section pain relief was shown by Blanco et al to be both superior to placebo13 and superior to a TAP block.14 The superiority of a quadratus lumborum block over tap block shown by Blanco et al further illustrates the need for visceral pain coverage in patients undergoing a cesarean section. A future study could involve a comparison of LB TAP plus ITM compared to quadratus lumborum then depending on results, testing the effectiveness of ITM when doing a postoperative quadratus lumborum block.
This study further points to the benefit of ITM in a multi-modal regimen for this patient population, although a prospective randomized controlled trial is needed. The limitations of this study are multifactorial. This is a retrospective study and, therefore, the two groups are unevenly distributed and recall bias can occur. We relied on data from the electronic medical record which may not always be accurate. The range of ITM dose and the use of intrathecal fentanyl only in the LB TAP plus ITM group are obvious confounders. It is entirely possible the decrease in ME over the first 24 hours could have been attributed to intrathecal fentanyl only being administrated to the LB TAP plus ITM group; however, when we eliminated those who had intrathecal fentanyl from data set we did not find any changes in the significance of opioid use between the two groups. Thus, this would suggest that the intrathecal fentanyl did not play a major role in the postoperative opioid use. Also, the range of dosing of ITM from 100 to 400 µg places the mean at what is considered a “high dose”. This could also have an effect on the lower amount of ME taken in the first 24 hours as well as the higher incidence (although non-significant) of nausea and vomiting in the LB TAP plus ITM group. The discrepancy in group size can be attributed to the study design of using patients that received blocks and the other group relied on a contraindication, patient refusal, or anesthesiologist’s choice to not use ITM and be included. Looking at more than an 11-month period of time may have resulted in a more uniform distribution between the two groups. While the TAP plane is relatively well defined ultrasonographically, there can be false planes and inadequate anesthetic spread within the plane to accurately predict the quality of block achieved. As this was retrospective, we did not have video or photographic confirmation about correct local anesthetic placement in the TAP plane. Thus, we cannot be certain that all TAP blocks were successful since it is not our practice to evaluate success of blocks using sensory testing postoperatively. Finally, while most patients received a multi-modal analgesic regimen it was not standardized between the two groups. All of these drawbacks suggest further prospective randomized studies should be done comparing ITM alone vs ITM plus liposome bupivacaine TAP.
Conclusion
Our data suggest that patients who received an LB TAP plus ITM required less total ME over 72 hours and during the first 24 hours when compared to LB TAP alone. Furthermore, the LB TAP plus ITM group had a shorter length of stay than those who had only an LB TAP and although every retrospective study has inherent limitations, we can use these data to sculpt prospective studies to further define ITM and LB TAP block’s roles in postoperative analgesia for cesarean sections.
Acknowledgments
The authors thank Alex Kaizer for his assistance with statistics and Ryan Eskuri and Jonathan Dang for their assistance with data collection.
Footnotes
Disclosure
JLH is a consultant on the speaker’s bureau and has received research funding from Pacira Pharmaceuticals. He is also a consultant and stock owner with Insitu Biologics, consultant for Acel Rx, consultant for Worrell, speaker for Sonosite and has received research funding and is a consultant for Avanos. LR has received research funding from Pacira Pharmaceuticals. AAB is on the speaker’s bureau for Pacira Pharmaceuticals and has received research funding and is a consultant for Avanos. FO, CH, and SN report no conflict of interest in this work.
References
- 1.Carvalho B, Butwick AJ. Postcesarean delivery analgesia. Best Pract Res Clin Anaesthesiol. 2017;31(1):69–79. doi: 10.1016/j.bpa.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Baeriswyl M, Kirkham KR, Kern C, Albrecht E. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg. 2015;121(6):1640–1654. doi: 10.1213/ANE.0000000000000967. [DOI] [PubMed] [Google Scholar]
- 3.Brogi E, Kazan R, Cyr S, Giunta F, Hemmerling TM. Transversus abdominal plane block for postoperative analgesia: a systematic review and meta-analysis of randomized-controlled trials. Can J Anesth. 2016;63(10):1184–1196. doi: 10.1007/s12630-016-0679-x. [DOI] [PubMed] [Google Scholar]
- 4.Abdallah FW, Halpern SH, Margarido CB. Transversus abdominis plane block for postoperative analgesia after caesarean delivery performed under spinal anaesthesia? A systematic review and meta-analysis. Br J Anaesth. 2012;109(5):679–687. doi: 10.1093/bja/aes279. [DOI] [PubMed] [Google Scholar]
- 5.Gorfine SR, Onel E, Patou G, Krivokapic ZV. Bupivacaine extended-release liposome injection for prolonged postsurgical analgesia in patients undergoing hemorrhoidectomy: a multicenter, randomized, double-blind, placebo-controlled trial. Dis Colon Rectum. 2011;54(12):1552–1559. doi: 10.1097/DCR.0b013e318232d4c1. [DOI] [PubMed] [Google Scholar]
- 6.Barron KI, Lamvu GM, Schmidt RC, Fisk M, Blanton E, Patanwala I. Wound infiltration with extended-release versus short-acting bupivacaine before laparoscopic hysterectomy: a randomized controlled trial. J Minim Invasive Gynecol. 2017;24(2):286–292. doi: 10.1016/j.jmig.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Hutchins JL, Kesha R, Blanco F, Dunn T, Hochhalter R. Ultrasound-guided subcostal transversus abdominis plane blocks with liposomal bupivacaine vs. non-liposomal bupivacaine for postoperative pain control after laparoscopic hand-assisted donor nephrectomy: a prospective randomised observer-blinded study. Anaesthesia. 2016;71(8):930–937. doi: 10.1111/anae.13502. [DOI] [PubMed] [Google Scholar]
- 8.Hutchins J, Vogel RI, Ghebre R, et al. Ultrasound-guided subcostal transversus abdominis plane infiltration with liposomal bupivacaine for patients undergoing robotic-assisted hysterectomy: a retrospective study. Int J Gynecol Cancer. 2015;25(5):937–941. doi: 10.1097/IGC.0000000000000429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stokes AL, Adhikary SD, Quintili A, et al. Liposomal bupivacaine use in transversus abdominis plane blocks reduces pain and postoperative intravenous opioid requirement after colorectal surgery. Dis Colon Rectum. 2017;60(2):170–177. doi: 10.1097/DCR.0000000000000747. [DOI] [PubMed] [Google Scholar]
- 10.Hutchins J, Delaney D, Vogel RI, et al. Ultrasound guided subcostal transversus abdominis plane (TAP) infiltration with liposomal bupivacaine for patients undergoing robotic assisted hysterectomy: a prospective randomized controlled study. Gynecol Oncol. 2015;138(3):609–613. doi: 10.1016/j.ygyno.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Topham D, Drew D. Quality Improvement Project: Replacing the Numeric Rating Scale with a Clinically Aligned Pain Assessment (CAPA) Tool. Pain Manag Nurs. 2017;18(6):363–371. doi: 10.1016/j.pmn.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 12.GlobalrphRPH: The Clinicians Ultimate Reference [webpage on the Internet] [Accessed November 2016 to May 2017]. Available from: https://globalrph.com/medcalcs/opioid-conversions-calc-original-single-agent/
- 13.Blanco R, Ansari T, Girgis E. Quadratus lumborum block for postoperative pain after caesarean section: a randomised controlled trial. Eur J Anaesthesiol. 2015;32(11):812–818. doi: 10.1097/EJA.0000000000000299. [DOI] [PubMed] [Google Scholar]
- 14.Blanco R, Ansari T, Riad W, Shetty N. Quadratus lumborum block versus Transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. 2016;41(6):757–762. doi: 10.1097/AAP.0000000000000495. [DOI] [PubMed] [Google Scholar]
- 15.Mishriky BM, George RB, Habib AS. Transversus abdominis plane block for analgesia after cesarean delivery: a systematic review and meta-analysis. Can J Anesth. 2012;59(8):766–778. doi: 10.1007/s12630-012-9729-1. [DOI] [PubMed] [Google Scholar]