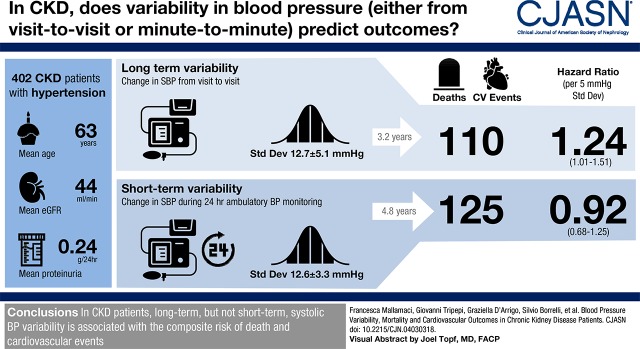
Visual Abstract
Keywords: hypertension; cardiovascular; mortality risk; chronic kidney disease; Prognosis; blood pressure; Systole; Renal Insufficiency, Chronic; Ambulatory Care
Abstract
Background and objectives
Short-term BP variability (derived from 24-hour ambulatory BP monitoring) and long-term BP variability (from clinic visit to clinic visit) are directly related to risk for cardiovascular events, but these relationships have been scarcely investigated in patients with CKD, and their prognostic value in this population is unknown.
Design, setting, participants, & measurements
In a cohort of 402 patients with CKD, we assessed associations of short- and long-term systolic BP variability with a composite end point of death or cardiovascular event. Variability was defined as the standard deviation of observed BP measurements. We further tested the prognostic value of these parameters for risk discrimination and reclassification.
Results
Mean ± SD short-term systolic BP variability was 12.6±3.3 mm Hg, and mean ± SD long-term systolic BP variability was 12.7±5.1 mm Hg. For short-term BP variability, 125 participants experienced the composite end point over a median follow-up of 4.8 years (interquartile range, 2.3–8.6 years). For long-term BP variability, 110 participants experienced the composite end point over a median follow-up of 3.2 years (interquartile range, 1.0–7.5 years). In adjusted analyses, long-term BP variability was significantly associated with the composite end point (hazard ratio, 1.24; 95% confidence interval, 1.01 to 1.51 per 5-mm Hg higher SD of office systolic BP), but short-term systolic BP variability was not (hazard ratio, 0.92; 95% confidence interval, 0.68 to 1.25 per 5-mm Hg higher SD of 24-hour ambulatory systolic BP). Neither estimate of BP variability improved risk discrimination or reclassification compared with a simple risk prediction model.
Conclusions
In patients with CKD, long-term but not short-term systolic BP variability is related to the risk of death and cardiovascular events. However, BP variability has a limited role for prediction in CKD.
Introduction
BP is a biologic variable characterized by a high variability (1). Such a variability is evident when analyzed within the 24-hour timeframe in ambulatory BP (ABP) recordings (short-term variability) or over long periods, a phenomenon captured in repeated standard measurements in the office over weeks or months (visit-to-visit BP variability) (2). Both short-term BP variability(3–5) and long-term visit-to-visit BP variability (6–9) associate with organ damage and cardiovascular events independent of average 24-hour ABP and average office BP, respectively. Although the issue still remains undefined, estimates of BP variability are considered as potentially useful for risk stratification (10).
A large survey in patients with hypertension and CKD recently documented that short-term BP variability increases in parallel with the decline of the GFR (11). Cross-sectional studies associated higher short-term (24-hour) BP variability with intracranial aneurysms in patients with adult polycystic kidney disease (12) and sleep disturbances in patients with CKD (13), but there is still no prospective cohort study investigating the relationship between the same parameter and major cardiovascular outcomes. However, higher visit-to-visit BP variability in patients with CKD has been associated with mortality and incident cardiovascular events (14,15) as well as with death and incident hemorrhagic stroke (16).
Until now, no study compared the relationship of short- and long-term BP variability with death and cardiovascular events in the CKD population. The issue is of relevance, because short-term BP variability mainly reflects the autonomic modulation of day to night BP changes (2,17), whereas long-term BP variability results from poor adherence to antihypertensive therapy (18), behavioral changes, chronic postural instability, and sympathetic overactivity and other factors (17,19). Furthermore, the prognostic power of BP variability, which is a problem different from causation, has never been properly assessed by applying recent statistical methods recommended for proper testing prognostic biomarkers on the basis of their risk discrimination and reclassification abilities (20,21).
With this background in mind, we investigated the relationship of short- and long-term BP variability with cardiovascular events and death in a cohort of patients with CKD and GFRs ranging from 5 to 90 ml/min per 1.73 m2. Patients were followed up in two nephrology units sharing a common protocol of BP assessment that calculated systematic 24-hour ABP measurements and applied clinical policies that conform to contemporary guidelines of CKD management and hypertension treatment.
Materials and Methods
This cohort study enrolled consecutive patients in two outpatient nephrology clinics (University of Campania “Luigi Vanvitelli,” Naples, Italy and Consiglio Nazionale delle Ricerche-Istituto Fisiologia Clinica (CNR-IFC), Clinical Epidemiology and Physiopathology of Renal Diseases and Hypertension, Reggio Calabria, Italy) for the period from 2001 to 2009. Patients were enrolled if they had CKD defined as either an eGFR<60 ml/min per 1.73 m2 or proteinuria >0.15 g/24 h in two consecutive visits with an interval of ≥3 months, if they had a follow-up in the nephrology clinics >6 months, and if they an ABP monitoring study performed to confirm hypertension. Exclusion criteria were normotension (clinic BP <130/80 mm Hg without antihypertensive therapy), changes in antihypertensive therapy 2 weeks before ABP, atrial fibrillation, and inadequate ABP monitoring (<20 recordings during the day and fewer than seven recordings during the night) (22). Patients on dialysis and patients with transplants were excluded from the study. Complete medical history, demographic and laboratory data, and current therapy were collected at study enrollment, which coincided with the ABP monitoring study, and eGFR was calculated by the Chronic Kidney Disease Epidemiology Collaboration creatinine equation; creatinine was not standardized to isotope dilution mass spectrometry values, and we, therefore, reduced creatinine levels by 5% according to Skali et al. (23). The underlying diagnosis of kidney disease was determined by the nephrologists responsible for the care of study patients by using the categorization recommended by the European Renal Association–European Dialysis and Transplantation Association Registry (24) Institutional review boards of the participating centers approved the protocol, and written informed consent was obtained from all patients.
Clinic BP Measurement
Clinic BP was measured by aneroid sphygmomanometers that were periodically calibrated by study technicians or nurses at the two research units involved in this study. Measurements were made during a physician visit (8:00–11:00 a.m.) according to contemporary recommendations of the International Society of Hypertension (25) and the European Society of Hypertension (ESH) (26–28). Antihypertensive medications were prescribed to achieve clinic BP <130/80 mm Hg, and they were administered from 8:00 a.m. to 10:00 p.m. as per recommendations detailed in the previously mentioned guidelines (25–28).
Ambulatory BP Monitoring
The two participating centers shared the same ABP protocols: Spacelabs 90207 (29) monitors were used. The monitor recorded BP every 15 minutes during the period from 7:00 a.m. to 11:00 p.m. and every 30 minutes during the period from 11:00 p.m. to 7:00 a.m. Daytime and nighttime periods were derived from the patient’s diary. Monitoring was always done on a working day and under regular antihypertensive treatment. According to recommendations by the ESH (22), we considered only 24-hour recordings with at least 20 valid awake and seven valid asleep measurements as valid.
Long-Term Visit-To-Visit BP Measurement
To be considered for this analysis, patients had to have at least four office BP measurements during separate follow-up visits. Three hundred sixty-six patients (91% of the whole cohort) qualified for this analysis. The number of visits in these patients ranged from four to 53, and the average interval between visits was 3.3±2.2 months. In detail, the number of visits was four in 89 patients, five in 108 patients, six in 69 patients, seven in 32 patients, eight in 30 patients, and nine in 14 patients, and the number ranged from ten to 53 in the remaining 24 patients. As measures of BP variability, we adopted the SD of systolic BP across study visits (17). Only BP data preceding the occurrence of a nonfatal cardiovascular event, ESKD, or censoring were considered to assess the long-term visit-to-visit systolic BP variability.
Short-Term BP Variability Measurement
To assess short-term BP variability, we calculated the weighted SD (w-SD) of 24-hour systolic ambulatory blood pressure monitoring defined as the average of the SD of the diurnal and nocturnal systolic BP measurements weighted for the duration of the daytime and nighttime intervals according to the following formula: w-SD = [(daytime SD × hours included during daytime) + (nighttime SD × hours included during nighttime)]/24 h (17).
Outcomes
Patients were followed up from the date of 24-hour ambulatory blood pressure monitoring onward (i.e., until December 17, 2017, death, or ESKD).
Clinical and biochemical variables as well as clinical outcomes, including death and cardiovascular events, were prospectively collected and registered in the clinical files, and after event validation (see below), they subsequently transcribed into the study database (SPSS/STATA files). Cardiovascular events were defined according to consensus documents and clinical practice guidelines by major cardiology societies at the time when the study was initiated (30–32). In case of doubt, events adjudication was done by consensus among at least three clinical investigators in the two study centers. To provide an overall estimate of the risk of the two main exposures of this study (short- and long-term BP variability), the primary outcome was a combined end point composed of all-cause death and cardiovascular events (myocardial infarction, stroke, revascularization, heart failure, angina, atrial fibrillation, and cerebral aneurysm). Risk was presented as cumulative risk over follow-up.
Statistical Analyses
Continuous variables are expressed as mean ± SD or median and interquartile range (IQR) according to their distribution as assessed by the Shapiro–Wilk test. Categorical variables were expressed as percentages. Standard correlation analysis was used to evaluate the relationship between long- and short-term systolic BP variability as well as with age, sex, diabetes, smoking, background cardiovascular events, body mass index, number of antihypertensive drugs, eGFR, 24-hour urinary protein, hemoglobin, and average systolic and pulse pressures across visits. Data were expressed as Pearson correlation coefficients (r values) and P values.
The independent correlates of long-term systolic BP variability (dependent variable) were identified by simultaneously introducing into the same multiple linear regression model all univariable correlates (P<0.05) of the dependent variable and stratifying by center. In this analysis, data were expressed as standardized regression coefficients (β values) and P values. The relationships between all systolic BP determinants (namely long- and short-term systolic BP variability, average systolic office BP, and average 24-hour daytime and nighttime systolic BP) and study outcomes were tested in Cox models stratified by center and adjusted (model 1) for baseline known covariates affecting death and cardiovascular outcomes (age, sex, diabetes mellitus, cholesterol, history of cardiovascular disease, smoking, body mass index, hemoglobin, eGFR, 24-hour urinary protein, and use of antihypertensive drugs). The long-term systolic BP variability to study outcomes link was further investigated in a model (model 2) adjusting for average systolic BP across visits, whereas the short-term systolic BP variability to study outcomes link was analyzed in a model (model 2) including average 24-hour systolic BP. A similar statistical approach was used for daytime and nighttime systolic BP variability. To account for the potential distortion of the number of visits on the long-term systolic BP variability to study outcome link, this variable was forced into these models. Data were expressed as hazard ratio (HRs), 95% confidence intervals (95% CIs), and P values.
The additional predictive value of short- and long-term systolic BP variability and the corresponding average values were tested by calculating the gain in discriminant power by these variables when the same variables were added to a simple predictive model (see Results). Furthermore, the prognostic value of short- and long-term BP variability and the corresponding average BP values were carried out by risk discrimination analysis (the Harrell c statistics [20]) and risk reclassification analysis (the integrated discrimination improvement [21], which is a categorization-free risk reclassification test).
All calculations were made using standard statistical packages (SPSS for Windows Version 24 [IBM, Armonk, NY] and STATA 13 for Windows [College Station, TX]. Two-tailed P<0.05 was considered significant.
Results
Of a global population of about 3000 patients, about 450 were excluded for being normotensive and about 600 were excluded for a follow-up shorter than 6 months. About 800 were excluded, because they had GFR>60 ml/min per 1.73 m2, proteinuria <0.15 g/24 h, or atrial fibrillation, and about 400 were excluded because of changed antihypertensive therapy 2 weeks before enrollment. About 350 refused to undergo 24-hour ABP, had recordings of insufficient quality according to the criteria established by the ESH (21), or could not undertake 24-hour ABP for logistic reasons. We also excluded two patients who were lost to follow-up. Thus, for the analysis of the short-term systolic BP variability to study outcomes relationship, the study sample was composed of 402 patients. Fifty-eight percent were men, and the mean age was 63 years old (Table 1). On average, the eGFR was 44±20 ml/min per 1.73 m2. Median proteinuria was 0.24 g/24 h, 24% were smokers, 35% had type 2 diabetes, and 29% had background cardiovascular comorbidities. Office BP at first visit was 145±19/81±12 mm Hg. Three hundred sixty-eight patients (92%) were on antihypertensive treatment. The whole study population (n=402) had suitable 24-hour ambulatory blood pressure monitoring recordings, and therefore, they could be used for the study of the predictive power of short-term systolic BP variability; however, only the subgroup with four or more office BP measurements (n=366; 91%) could be investigated for the study of long-term systolic BP variability. Two follow-up periods were considered in survival analyses. The first (the short-term systolic BP variability study) started from the day on which patients underwent to 24-hour ambulatory blood pressure monitoring (median follow-up: 4.8 years; IQR, 2.3–8.6), and the second (the long-term systolic BP variability study) started from the day after the last follow-up visit (median follow-up: 3.2 years; IQR, 1.0–7.5). During the follow-up looking at short-term systolic BP variability, 59 patients died (44 from cardiovascular causes), and 67 patients had nonfatal cardiovascular events. During the follow-up looking at long-term systolic BP variability, 52 patients died (39 for cardiovascular causes), and 58 patients had nonfatal cardiovascular events. Overall, 125 patients experienced the combined end point of death and cardiovascular events during the follow-up focusing on short-term systolic BP, and 110 had the same outcome during the follow-up focusing on long-term systolic BP. The causes of death and the list of cardiovascular events during the two follow-up periods are given in Supplemental Table 1.
Table 1.
Demographics, clinical characteristics, office and 24-hour ambulatory BP parameters, and drug treatment in the study cohort composed of 402 patients with CKD from two Italian clinics
| Variables | |
|---|---|
| Age, yr, mean ± SD | 63±14 |
| Men, N (%) | 233 (58) |
| BMI, kg/m2, mean ± SD | 27.1±4.7 |
| Smoking, N (%) | 97 (24) |
| Diabetes, N (%) | 141 (35) |
| History of cardiovascular disease, % | 29 |
| eGFR, % | |
| eGFR=120–60 ml/min per 1.73 m2 | 20 |
| eGFR=59–30 ml/min per 1.73 m2 | 50 |
| eGFR=29–15 ml/min per 1.73 m2 | 23 |
| eGFR<15 ml/min per 1.73 m2 | 6 |
| eGFR, ml/min per 1.73 m2, mean ± SD | 44±20 |
| Proteinuria, g/d, median (interquartile range) | 0.24 (0.08–0.92) |
| Hemoglobin, g/dl, mean ± SD | 12.9±1.8 |
| Total cholesterol, mg/dl, mean ± SD | 189±39 |
| Causes of kidney disease, % | |
| Hypertensive nephropathy | 44 |
| Diabetic kidney disease | 20 |
| GN | 10 |
| ADPKD | 4 |
| Other/unknown | 22 |
| BP | |
| Office systolic/diastolic BP, mm Hg, mean ± SD | 145±19/81±12 |
| Office BP <140/90 mm Hg (%) | 133 (33) |
| 24-h systolic/diastolic BP, mm Hg, mean ± SD | 126±16/72±10 |
| 24-h BP <130/80 mm Hg (%) | 209 (52) |
| Daytime systolic/diastolic BP, mm Hg, mean ± SD | 129±17/75±11 |
| Daytime BP <135/85 mm Hg (%) | 233 (58) |
| Nighttime BP systolic/diastolic BP, mm Hg, mean ± SD | 120±19/66±11 |
| Nighttime BP <120/70 mm Hg (%) | 169 (42) |
| Long-term office systolic BP variability,a mm Hg | 12.7±5.1 |
| Short-term 24-h systolic BP variability, mm Hg | 12.6±3.3 |
| Short-term daytime systolic BP variability, mm Hg | 13.1±3.9 |
| Short-term nighttime systolic BP variability, mm Hg | 11.5±3.8 |
| Treatment | |
| No. of drugs, median (interquartile range) | 3 (2–4) |
| RAS inhibitors (%) | 326 (81) |
| Calcium channel blockers (%) | 185 (46) |
| β-Blockers (%) | 145 (36) |
| Furosemide (%) | 129 (32) |
eGFR was calculated by the Chronic Kidney Disease Epidemiology Collaboration creatinine equation. BMI, body mass index; ADPKD, autosomal dominant polycystic kidney disease; RAS, renin-angiotensin system.
Calculated on 366 patients (i.e., patients with four or more longitudinal visits).
Long-Term Visit-To-Visit Systolic BP Variability(SD): Correlates and Relationship with Death and Incident Cardiovascular Events
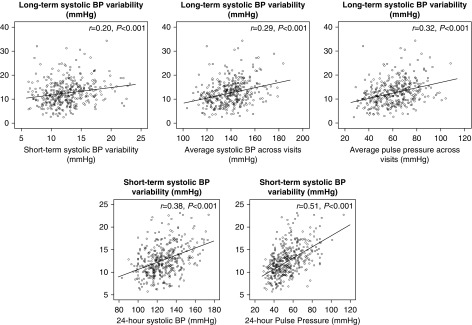
The average systolic BP over follow-up was 139±14/78±8 mm Hg, and average variability (SD) of the same measurement was 12.7±5.1 mm Hg. Long-term systolic BP variability was associated with average systolic BP (r=0.29, P<0.001) and average pulse pressure (r=0.32, P<0.001). To a weaker extent, long-term systolic BP variability was associated with short-term (24-hour) systolic BP variability (r=0.20, P<0.001) (Figure 1), the number of antihypertensive drugs (r=0.20, P<0.001), hemoglobin (r=−0.20, P<0.001), eGFR (r=−0.13, P=0.01), 24-hour urinary protein (r=0.11, P=0.04), age (r=0.13, P=0.02), and men (r=−0.15, P=0.004), but it was unrelated to diabetes (r=0.07, P=0.17), body mass index (r=0.04, P=0.43), smoking (r=0.06, P=0.25), and background cardiovascular events (r=−0.01, P=0.80). The relationships of long-term BP variability with average pulse pressure (β=0.27, P<0.001) and average office systolic BP (β=0.20, P=0.001) remained also significant in multiple regression models, including the univariable correlates of systolic BP variability (number of antihypertensive drugs, hemoglobin, eGFR, 24-hour urinary protein, age, and sex).
Figure 1.
Mutual association of long- and short-term BP and associations of the same variabilities with systolic and pulse pressure. (Upper panels) Association of visit-to-visit systolic BP variability (SD) with short-term systolic BP variability (weighted SD; left panel), average systolic BP (center panel), and pulse pressure (right panel) across visits. The lower panels show the relationship of average 24-hour systolic BP (left panel) and 24-hour pulse pressure (right panel) with short-term BP variability (weighted SD).
In unadjusted Cox regression analyses, a 5-mm Hg higher systolic office BP variability (SD) was associated with a 28% higher risk of death and incident cardiovascular events (HR, 1.28; 95% CI, 1.08 to 1.51; P=0.004) (Table 2). The risk for these events was also directly related to the average systolic BP across visits (HR [5 mm Hg], 1.16; 95% CI, 1.09 to 1.24; P<0.001). In analyses adjusting for age, sex, body mass index, diabetes, cholesterol, active smoking, hemoglobin, eGFR, cardiovascular comorbidities, number of antihypertensive drugs, and proteinuria as well as average office BP (Table 2, long-term systolic BP variability in model 2), the long-term systolic BP variability maintained an independent relationship with the combined end point. Furthermore, the strength of this association also did not change when forcing the number of visits into the Cox model (HR [5 mm Hg], 1.24; 95% CI, 1.01 to 1.51; P=0.04). Similar results were obtained by adopting the coefficient of variation as a metric of BP variability (Supplemental Table 2). Of note, in the fully adjusted model, average systolic BP across visits just failed to significantly predict the combined end point (Table 2, model 2). The cumulative risk for the combined end point for average office systolic BP and the weighted systolic BP variability across tertiles of the same variables are reported in Supplemental Table 3, and the detailed numbers of events, unadjusted incidence rates, and HRs across the same categories are reported in Supplemental Table 4.
Table 2.
Associations of long- and short-term BP variability and related BP metrics with a composite outcome of death and cardiovascular events
| Variables | Unadjusted Analysis HR (95% CI), P Value | Model 1 HR (95% CI), P Value | Model 2 HR (95% CI), P Value |
|---|---|---|---|
| Average systolic office BP (HR per 5-mm Hg higher systolic BP) | 1.16 (1.09 to 1.24), P<0.001 | 1.11 (1.02 to 1.20), P=0.01 | 1.08 (0.99 to 1.17), P=0.07 |
| Average 24-h systolic BP (HR per 5-mm Hg higher systolic BP) | 1.14 (1.08 to 1.20), P<0.001 | 1.08 (1.03 to 1.14), P=0.004 | 1.09 (1.03 to 1.15), P=0.004 |
| Average daytime systolic BP (HR per 5-mm Hg higher systolic BP) | 1.13 (1.07 to 1.19), P<0.001 | 1.08 (1.02 to 1.14), P<0.01 | 1.09 (1.03 to 1.15), P=0.004 |
| Average nighttime systolic BP (HR per 5-mm Hg higher systolic BP) | 1.12 (1.07 to 1.17), P<0.001 | 1.07 (1.03 to 1.12), P=0.003 | 1.07 (1.02 to 1.12), P=0.01 |
| Long-term systolic BP variability SD of average visit-to-visit systolic BP (HR per 5-mm Hg higher systolic BP SD) | 1.28 (1.08 to 1.51), P=0.004 | 1.31 (1.08 to 1.58), P<0.01 | 1.24 (1.01 to 1.51), P=0.04 |
| Short-term (24-h) variability weighted SD of average 24-h systolic BP (HR per 5-mm Hg higher systolic BP weighted SD) | 1.85 (1.45 to 2.37), P<0.001 | 1.08 (0.81 to 1.43), P=0.59 | 0.92 (0.68 to 1.25), P=0.61 |
| Short-term (daytime) variability SD of average daytime systolic BP (HR per 5-mm Hg higher systolic BP weighted SD) | 1.59 (1.31 to 1.94), P<0.001 | 1.01 (0.81 to 1.27), P=0.93 | 0.91 (0.71 to 1.16), P=0.43 |
| Short-term (nighttime) variability SD of average nighttime systolic BP (HR per 5-mm Hg higher systolic BP weighted SD) | 1.43 (1.15 to 1.78), P=0.002 | 1.18 (0.94 to 1.49), P=0.16 | 1.06 (0.83 to 1.37), P=0.63 |
The combined end point of this study was all-cause death and nonfatal cardiovascular events (Supplemental Table S1 has details). For all BP metrics, data are adjusted for age, sex, body mass index, diabetes, cholesterol, smoking, hemoglobin, eGFR, background cardiovascular comorbidities, 24-hour urinary protein, and number of antihypertensive drugs in model 1. In model 2, each BP determinant is adjusted for the corresponding mean values or systolic BP variability values as appropriate. HR, hazard ratio; 95% CI, 95% confidence interval.
Short-Term Systolic BP Variability and Average 24-Hour Systolic ABP: Correlates and Relationship with Death and Incident Cardiovascular Events
The short-term (w-SD) variability of 24-hour systolic BP and the variability (SD) of daytime and nighttime systolic BP were 12.6±3.3, 13.1±3.9, and 11.6±3.8 mm Hg, respectively. Short-term systolic BP variability associated with 24-hour systolic BP (r=0.38, P<0.001) and 24-hour pulse pressure (r=0.51, P<0.001) (Figure 1). Furthermore, the same parameter was directly related to age (r=0.38, P<0.001), diabetes (r=0.21, P<0.001), background cardiovascular comorbidities (r=0.24, P<0.001), and the number of antihypertensive drugs (r=0.30, P<0.001).
On univariable Cox regression, short-term 24-hour systolic BP variability as well the variability of daytime and nighttime systolic BP significantly associated with the combined end point (Table 2, unadjusted analysis). By the same token, average 24-hour systolic BP as well as daytime and nighttime systolic BP also associated with the same outcome in unadjusted analyses (Table 2, unadjusted analysis). However, in multiple Cox regression models, metrics of short-term variability largely failed to maintain an independent association with death and cardiovascular events, whereas average 24-hour systolic BP (Table 2) as well as average daytime and nighttime systolic BP (Table 2) maintained a robust association with the combined end point. The cumulative risks for the combined end point for average 24-hour, daytime, and nighttime systolic BP across tertiles of the same variables are reported in Supplemental Table 3, and the detailed numbers of events, unadjusted incidence rates, and HRs across tertiles of short-term systolic BP variability are reported in Supplemental Table 4.
Prognostic Value of Long- and Short-Term Systolic BP Variability
To estimate the prognostic value of long- and short-term BP variability, we added these variables into a basic model formed by simple clinical variables, including age, sex, traditional risk factors (diabetes, serum cholesterol, body mass index, smoking habit, and number of antihypertensive drugs), and CKD-specific risk factors (GFR, proteinuria, and hemoglobin). In the whole study cohort (n=402), this model had fairly good discriminant power for the study outcome as indicated by a Harrell c index of 76.8%, a figure that is almost identical to that found (74.2%) in the subgroup of patients with the number of follow-up visits greater than or equal to four. The addition in separate models of SD of long-term BP (+0.8%), short-term systolic BP (0.0%), daytime systolic BP (0.0%), and nighttime systolic BP (−0.2%) variability added no additional predictive power to the basic model. As expected from the futile gain in prediction power with the Harrell c test, the same biomarkers did not materially improve risk reclassification (integrated discrimination improvement: long-term systolic BP variability, 0.1%; short-term 24-hour systolic BP variability, 0.3%; daytime variability, 0.3%; nighttime variability, 0.2%).
Discussion
This study in patients with CKD and various degrees of kidney dysfunction shows that long-term (visit-to-visit) but not short-term systolic BP variability was directly related to the risk of death and incident cardiovascular events independent of the corresponding average BP values. However, neither of the two estimates of BP variability proved to be useful for prognosis, because both metrics added no predictive power to a prediction model formed by simple, easily available clinical variables in patients with CKD.
Short-term BP variability predicted incident cardiovascular events in both a population-based study (33) and a large international 24-hour ABP database (34). By the same token, long-term visit-to-visit BP variability predicted cardiovascular outcomes in a community study (9) and extensive analyses performed in the databases of clinical trials and cohort studies (8). In patients with CKD, the issue has been investigated in a limited number of studies. A clear relationship of long-term visit-to-visit BP variability with cardiovascular outcomes and/or death coherently emerged in three cohort studies (14–16), but information on the relationship between short-term BP variability and these outcomes is lacking. As alluded to before, the prognostic role of BP is still poorly defined, because there are no studies in this population that have examined the problem by applying modern statistical techniques for assessing the prognostic value of prognostic biomarkers (20,21,35).
In this study, we specifically confirmed in patients with CKD that short-term 24-hour systolic BP variability associates fairly well with average 24-hour systolic BP (17), but we found that this parameter was unrelated to death and incident cardiovascular events in models including average 24-hour systolic BP and other potential confounders. In a large international database of 24-hour ABP studies, the risk for fatal and nonfatal cardiovascular events by short-term BP variability was quite low and of marginal statistical significance in adjusted analyses (34). However, in classic Cox regression analyses, we also observed that long-term (visit-to-visit) BP variability associated with the risk of death and cardiovascular events in patients with CKD, which is in line with three previous cohort studies (14–16,36). High long-term BP variability may depend on poor adherence to antihypertensive therapy (18), which is a well known risk factor for cardiovascular events (37) and a concerning issue in the CKD population (38). Furthermore, long-term BP variability associates with measures of impaired BP control, like postural instability and sympathetic overactivity (19,39).
As far as prognosis is concerned, not only short-term BP variability but also, long-term visit-to-visit BP variability failed to provide meaningful prognostic information. Prognostic analyses demand an approach different from that adopted in analyses aimed at exploring causality (40). Powerful causal risk factors for cardiovascular disease, like hypercholesterolemia or high office BP, are per se weak prognostic factors. At the individual patient level, these variables add a very small clinically insignificant discriminant power to a model simply on the basis of age and smoking (41,42). Thus, although of potential value in mechanistic and clinical studies, metrics of BP variability are not useful for risk prediction at the individual level in patients with CKD.
Our study has limitations. First, the study cohort was relatively small. However, other than the Chronic Renal Insufficiency Cohort study (43), our study is one of the largest ABP studies in patients with CKD performed so far. Second, we excluded patients were normotensive, because our study was embedded in clinical practice and aimed at hypertension management. In this respect, it has to be noted that only a small minority of patients with CKD were normotensive (44,45). Third, the number of visits was quite variable. Our approach for calculating BP variability conformed to clinical practice, where the intensity of follow-up depends on the severity of CKD and associated comorbidities in a scenario where visits are not infrequently missed. Because our estimate of visit-to-visit variability is less precise than that of an approach on the basis of a fixed number of visits at preplanned intervals, the relationship between visit-to-visit variability and the study outcome could have been stronger had we been able to base the analysis on a fixed number of visits.
In conclusion, long-term (visit-to-visit) BP variability but not short-term BP variability associates with the risk of death and incident cardiovascular events independent of the corresponding average values. The link of long-term BP variability with death and cardiovascular events may be important for the interpretation of cardiovascular damage by hypertension. Nonetheless, both long- and short-term BP variability show no meaningful prognostic value for death and cardiovascular events in the CKD population, and they are, therefore, of limited value for risk stratification.
Disclosures
None.
Supplementary Material
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Blood Pressure Variability in CKD: Treatable or Hypertension’s Homocysteine?,” on pages 175–177.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.04030318/-/DCSupplemental.
Supplemental Table 1. Causes of death in the long- and short-term BP variability studies.
Supplemental Table 2. Unadjusted and adjusted Cox regression analyses of metrics of systolic BP variability expressed as coefficient of variation (CV).
Supplemental Table 3. Absolute cumulative risk during follow-up of the combined end point (CV events or death) according to tertiles of different indexes of BP burden and the long-term BP variability.
Supplemental Table 4. Absolute number, cumulative risk, incidence rate, total person-time, and crude hazard ratio of the combined end point (CV events or death) according to tertiles of different indexes of systolic BP variability.
References
- 1.Mancia G, Zanchetti A: Blood pressure variability. In: Handbook of Hypertension. Pathophysiology of Hypertension: Cardiovascular Aspects, Vol. 7, edited by Zanchetti A, Tarazi R, Amsterdam, Elsevier, 1986, pp 125–152 [Google Scholar]
- 2.Parati G, Ochoa JE, Lombardi C, Bilo G: Blood pressure variability: Assessment, predictive value, and potential as a therapeutic target. Curr Hypertens Rep 17: 537, 2015 [DOI] [PubMed] [Google Scholar]
- 3.Parati G, Pomidossi G, Albini F, Malaspina D, Mancia G: Relationship of 24-hour blood pressure mean and variability to severity of target-organ damage in hypertension. J Hypertens 5: 93–98, 1987 [DOI] [PubMed] [Google Scholar]
- 4.Frattola A, Parati G, Cuspidi C, Albini F, Mancia G: Prognostic value of 24-hour blood pressure variability. J Hypertens 11: 1133–1137, 1993 [DOI] [PubMed] [Google Scholar]
- 5.Sega R, Corrao G, Bombelli M, Beltrame L, Facchetti R, Grassi G, Ferrario M, Mancia G: Blood pressure variability and organ damage in a general population: Results from the PAMELA study (Pressioni Arteriose Monitorate E Loro Associazioni). Hypertension 39: 710–714, 2002 [DOI] [PubMed] [Google Scholar]
- 6.Nagai M, Hoshide S, Ishikawa J, Shimada K, Kario K: Visit-to-visit blood pressure variations: New independent determinants for carotid artery measures in the elderly at high risk of cardiovascular disease. J Am Soc Hypertens 5: 184–192, 2011 [DOI] [PubMed] [Google Scholar]
- 7.Masugata H, Senda S, Murao K, Inukai M, Hosomi N, Iwado Y, Noma T, Kohno M, Himoto T, Goda F: Visit-to-visit variability in blood pressure over a 1-year period is a marker of left ventricular diastolic dysfunction in treated hypertensive patients. Hypertens Res 34: 846–850, 2011 [DOI] [PubMed] [Google Scholar]
- 8.Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B, Sever PS, Poulter NR: Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 375: 895–905, 2010 [DOI] [PubMed] [Google Scholar]
- 9.Muntner P, Shimbo D, Tonelli M, Reynolds K, Arnett DK, Oparil S: The relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population: Findings from NHANES III, 1988 to 1994. Hypertension 57: 160–166, 2011 [DOI] [PubMed] [Google Scholar]
- 10.Parati G, Ochoa JE, Salvi P, Lombardi C, Bilo G: Prognostic value of blood pressure variability and average blood pressure levels in patients with hypertension and diabetes. Diabetes Care 36[Suppl 2]: S312–S324, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarafidis PA, Ruilope LM, Loutradis C, Gorostidi M, de la Sierra A, de la Cruz JJ, Vinyoles E, Divisón-Garrote JA, Segura J, Banegas JR: Blood pressure variability increases with advancing chronic kidney disease stage: A cross-sectional analysis of 16 546 hypertensive patients. J Hypertens 36: 1076–1085, 2018 [DOI] [PubMed] [Google Scholar]
- 12.Niemczyk M, Pilecki T, Gradzik M, Bujko M, Niemczyk S, Pączek L: Blood pressure and intracranial aneurysms in autosomal dominant polycystic kidney disease. Kidney Blood Press Res 39: 630–635, 2014 [DOI] [PubMed] [Google Scholar]
- 13.Pengo MF, Ioratti D, Bisogni V, Ravarotto V, Rossi B, Bonfante L, Simioni F, Nalesso F, Maiolino G, Calò LA: In patients with chronic kidney disease short term blood pressure variability is associated with the presence and severity of sleep disorders. Kidney Blood Press Res 42: 804–815, 2017 [DOI] [PubMed] [Google Scholar]
- 14.Mallamaci F, Minutolo R, Leonardis D, D’Arrigo G, Tripepi G, Rapisarda F, Cicchetti T, Maimone I, Enia G, Postorino M, Santoro D, Fuiano G, De Nicola L, Conte G, Zoccali C: Long-term visit-to-visit office blood pressure variability increases the risk of adverse cardiovascular outcomes in patients with chronic kidney disease. Kidney Int 84: 381–389, 2013 [DOI] [PubMed] [Google Scholar]
- 15.Di Iorio B, Pota A, Sirico ML, Torraca S, Di Micco L, Rubino R, Guastaferro P, Bellasi A: Blood pressure variability and outcomes in chronic kidney disease. Nephrol Dial Transplant 27: 4404–4410, 2012 [DOI] [PubMed] [Google Scholar]
- 16.Chang TI, Tabada GH, Yang J, Tan TC, Go AS: Visit-to-visit variability of blood pressure and death, end-stage renal disease, and cardiovascular events in patients with chronic kidney disease. J Hypertens 34: 244–252, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parati G, Ochoa JE, Lombardi C, Bilo G: Assessment and management of blood-pressure variability. Nat Rev Cardiol 10: 143–155, 2013 [DOI] [PubMed] [Google Scholar]
- 18.Kronish IM, Lynch AI, Oparil S, Whittle J, Davis BR, Simpson LM, Krousel-Wood M, Cushman WC, Chang TI, Muntner P: The association between antihypertensive medication nonadherence and visit-to-visit variability of blood pressure: Findings from the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Hypertension 68: 39–45, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rothwell PM: Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet 375: 938–948, 2010 [DOI] [PubMed] [Google Scholar]
- 20.Pencina MJ, D’Agostino RB: Overall C as a measure of discrimination in survival analysis: Model specific population value and confidence interval estimation. Stat Med 23: 2109–2123, 2004 [DOI] [PubMed] [Google Scholar]
- 21.Pencina MJ, D’Agostino RB Sr., D’Agostino RB Jr., Vasan RS: Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond. Stat Med 27: 157–172, discussion 207–212, 2008 [DOI] [PubMed] [Google Scholar]
- 22.O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y; European Society of Hypertension Working Group on Blood Pressure Monitoring : European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens 31: 1731–1768, 2013 [DOI] [PubMed] [Google Scholar]
- 23.Skali H, Uno H, Levey AS, Inker LA, Pfeffer MA, Solomon SD: Prognostic assessment of estimated glomerular filtration rate by the new chronic kidney disease epidemiology collaboration equation in comparison with the modification of diet in renal disease study equation. Am Heart J 162: 548–554, 2011 [DOI] [PubMed] [Google Scholar]
- 24.Venkat-Raman G, Tomson CR, Gao Y, Cornet R, Stengel B, Gronhagen-Riska C, Reid C, Jacquelinet C, Schaeffner E, Boeschoten E, Casino F, Collart F, De Meester J, Zurriaga O, Kramar R, Jager KJ, Simpson K; ERA-EDTA Registry : New primary renal diagnosis codes for the ERA-EDTA. Nephrol Dial Transplant 27: 4414–4419, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chalmers J, MacMahon S, Mancia G, Whitworth J, Beilin L, Hansson L, Neal B, Rodgers A, Ni Mhurchu C, Clark T: 1999 World Health Organization-International Society of Hypertension Guidelines for the management of hypertension. Guidelines sub-committee of the World Health Organization. Clin Exp Hypertens 21: 1009–1060, 1999 [DOI] [PubMed] [Google Scholar]
- 26.European Society of Hypertension-European Society of Cardiology Guidelines Committee : 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 21: 1011–1053, 2003 [DOI] [PubMed] [Google Scholar]
- 27.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HAJS, Zanchetti A; ESH-ESC Task Force on the Management of Arterial Hypertension : 2007 ESH-ESC practice guidelines for the management of arterial hypertension: ESH-ESC task force on the management of arterial hypertension. J Hypertens 25: 1751–1762, 2007 [DOI] [PubMed] [Google Scholar]
- 28.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Rydén L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA: 2013 ESH/ESC guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34: 2159–2219, 2013 [DOI] [PubMed] [Google Scholar]
- 29.O’Brien E, Mee F, Atkins N, O’Malley K: Accuracy of the SpaceLabs 90207 determined by the British hypertension society protocol. J Hypertens 9: 573–574, 1991 [DOI] [PubMed] [Google Scholar]
- 30.Alpert JS, Thygesen K, Antman E, Bassand JP: Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 36: 959–969, 2000 [DOI] [PubMed] [Google Scholar]
- 31.Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS, Ganiats TG, Goldstein S, Gregoratos G, Jessup ML, Noble RJ, Packer M, Silver MA, Stevenson LW, Gibbons RJ, Antman EM, Alpert JS, Faxon DP, Fuster V, Gregoratos G, Jacobs AK, Hiratzka LF, Russell RO, Smith SC Jr.; American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1995 Guidelines for the Evaluation and Management of Heart Failure); International Society for Heart and Lung Transplantation; Heart Failure Society of America : ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: Executive summary a report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to revise the 1995 guidelines for the evaluation and management of heart failure): Developed in collaboration with the International Society for Heart and Lung Transplantation; endorsed by the Heart Failure Society of America. Circulation 104: 2996–3007, 2001 [DOI] [PubMed] [Google Scholar]
- 32.Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T: Cerebrovascular disease in the community: Results of a WHO collaborative study. Bull World Health Organ 58: 113–130, 1980 [PMC free article] [PubMed] [Google Scholar]
- 33.Mancia G, Bombelli M, Facchetti R, Madotto F, Corrao G, Trevano FQ, Grassi G, Sega R: Long-term prognostic value of blood pressure variability in the general population: Results of the pressioni arteriose monitorate e loro associazioni study. Hypertension 49: 1265–1270, 2007 [DOI] [PubMed] [Google Scholar]
- 34.Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA; International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators : Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension 55: 1049–1057, 2010 [DOI] [PubMed] [Google Scholar]
- 35.Cook NR: Statistical evaluation of prognostic versus diagnostic models: Beyond the ROC curve. Clin Chem 54: 17–23, 2008 [DOI] [PubMed] [Google Scholar]
- 36.Mezue K, Goyal A, Pressman GS, Horrow JC, Rangaswami J: Blood pressure variability predicts adverse events and cardiovascular outcomes in chronic kidney disease: A post-hoc analysis of the SPRINT trial. Am J Hypertens 31: 48–52, 2017 [DOI] [PubMed] [Google Scholar]
- 37.Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, Borghi C, Brignoli O, Caputi AP, Cricelli C, Mantovani LG: Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation 120: 1598–1605, 2009 [DOI] [PubMed] [Google Scholar]
- 38.Muntner P, Judd SE, Krousel-Wood M, McClellan WM, Safford MM: Low medication adherence and hypertension control among adults with CKD: Data from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) Study. Am J Kidney Dis 56: 447–457, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grassi G, Quarti-Trevano F, Seravalle G, Arenare F, Volpe M, Furiani S, Dell’Oro R, Mancia G: Early sympathetic activation in the initial clinical stages of chronic renal failure. Hypertension 57: 846–851, 2011 [DOI] [PubMed] [Google Scholar]
- 40.Tripepi G, Jager KJ, Dekker FW, Zoccali C: Testing for causality and prognosis: Etiological and prognostic models. Kidney Int 74: 1512–1515, 2008 [DOI] [PubMed] [Google Scholar]
- 41.Ware JH: The limitations of risk factors as prognostic tools. N Engl J Med 355: 2615–2617, 2006 [DOI] [PubMed] [Google Scholar]
- 42.Cook NR: Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation 115: 928–935, 2007 [DOI] [PubMed] [Google Scholar]
- 43.Drawz PE, Alper AB, Anderson AH, Brecklin CS, Charleston J, Chen J, Deo R, Fischer MJ, He J, Hsu CY, Huan Y, Keane MG, Kusek JW, Makos GK, Miller ER 3rd, Soliman EZ, Steigerwalt SP, Taliercio JJ, Townsend RR, Weir MR, Wright JT Jr., Xie D, Rahman M; Chronic Renal Insufficiency Cohort Study Investigators : Masked hypertension and elevated nighttime blood pressure in CKD: Prevalence and association with target organ damage. Clin J Am Soc Nephrol 11: 642–652, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sarafidis PA, Li S, Chen S-C, Collins AJ, Brown WW, Klag MJ, Bakris GL: Hypertension awareness, treatment, and control in chronic kidney disease. Am J Med 121: 332–340, 2008 [DOI] [PubMed] [Google Scholar]
- 45.De Nicola L, Minutolo R, Chiodini P, Zoccali C, Castellino P, Donadio C, Strippoli M, Casino F, Giannattasio M, Petrarulo F, Virgilio M, Laraia E, Di Iorio BR, Savica V, Conte G; TArget Blood Pressure LEvels in Chronic Kidney Disease (TABLE in CKD) Study Group : Global approach to cardiovascular risk in chronic kidney disease: Reality and opportunities for intervention. Kidney Int 69: 538–545, 2006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.