Abstract
Purpose:
Little published data exist on the impact of urethral stricture surgery on urinary urgency. We evaluated urinary urgency and urge incontinence before and after anterior urethroplasty.
Materials and Methods:
Male patients who underwent 1-stage anterior urethroplasty were retrospectively identified at 8 centers. Patients with preoperative and 2-month or greater postoperative subjective urinary urgency assessments were included in study. Patients who received anticholinergic medications preoperatively were excluded. Univariate and multivariate analysis was done to analyze the association of patient characteristics with preoperative and postoperative symptoms as well as improvement or worsening of symptoms after surgery.
Results:
Symptom and followup data on urgency and urge incontinence were available in in 439 and 305 patients, respectively. Preoperatively 58% of the men reported urgency and 31% reported urge incontinence. Postoperatively this decreased to 40% of men for urgency and 12% for urge incontinence (each p <0.01). Of the men 37% reported improvement in urgency and 74% experienced improvement in urge incontinence. Few of those without preoperative symptoms showed worse symptoms, including urgency in 9% and urge incontinence in 5%. New urgency was more likely to develop in men with a higher body mass index (OR 1.09, p = 0.02). Men with stricture recurrence were less likely to show improvement in urgency (OR 0.24, p = 0.03). Older men were more likely to have new urge incontinence (OR 1.06, p = 0.01) and less likely to notice improvement in urge symptoms (OR 0.92, p <0.01).
Conclusions:
The prevalence of urgency and urge incontinence in male patients with anterior urethral stricture is high. The majority of men experience symptom stability or improvement in urinary urge symptoms following anterior urethroplasty.
Keywords: urethra, urinary bladder, overactive, lower urinary tract symptoms, urethral stricture, urinary incontinence, urge
Symptoms of urinary urgency or urge incontinence may develop in men with longstanding urethral stricture disease as a result of detrusor instability caused by chronic urinary obstruction. In these circumstances chronically increased post-void residual urine in the bladder could result in fibrotic changes to the bladder, ultimately causing decreased compliance and functionally smaller storage capacity. Furthermore, high residual urine could also predispose to chronic urinary infections, which could result in urge related symptoms. However, sparse data exist on the prevalence of urgency symptoms among patients with stricture.1 One retrospective study of patients who presented with urethral stricture and a prior history of hypospadias repair showed that at presentation 82% manifested voiding symptoms, including dysuria, stream spraying, straining, sense of complete emptying, weak stream, frequency and urgency.2
Most large series of patients treated with urethroplasty have not specifically addressed storage symptoms such as urinary urgency or urge incontinence preoperative or postoperatively.3–5 Recently, a single surgeon series evaluated 42 men with overactivity symptoms before and after urethroplasty, demonstrating that two-thirds reported preoperative overactivity symptoms.6 Of the 28 men with preoperative symptoms 25 reported symptom improvement and 1 had worse symptoms with an overall 54% median reduction in overactivity symptoms in the cohort. Apart from this small, single surgeon series to our knowledge the true rates of underlying urgency related symptoms and the effect of urethroplasty on these symptoms are unknown.
It is important to understand the impact of urethroplasty on urinary urgency symptoms to counsel patients and guide patient expectations. In this study we sought to evaluate urinary urgency and urge incontinence before and after anterior urethroplasty. We hypothesized that men with urethral stricture disease who experienced urinary urgency symptoms preoperatively would have a reduction in symptoms after anterior urethroplasty.
METHODS
Men with urethral stricture disease who underwent 1-stage anterior urethroplasty between September 1, 2010 and September 1, 2015 were retrospectively identified from 8 centers in TURNS (Trauma and Urologic Reconstruction Network of Surgeons). Data were collected from a multicenter prospectively maintained database. The 449 and 309 men who had completed assessment of urgency 449 and urge incontinence, respectively, preoperatively and 2-months or more postoperatively were included in analysis. Ten men with urgency and 4 with urge incontinence who received anticholinergic medications before urethroplasty were excluded.
To assess urgency symptoms patients were asked a validated question from CLSS,7 that is how often they experienced “a sudden strong desire to urinate, which is difficult to postpone.” Responses were graded on a Likert scale of 0 to 3, including 0—no, 1—rarely, 2—sometimes and 3—often. They were asked a question from AUA SI, that is how often they “found it difficult to postpone urination.” Responses were graded on a Likert scale of 0 to 5, including 0—not at all, 1—less than 1 in 5 times, 2—less than half the time, 3—about half the time, 4—more than half the time and 5—almost always.8
Items related to urine urge and urge incontinence from 2 patient reported outcome measures were used due to a change in the survey instrument used by TURNS surgeons. To correlate the 2 items the AUA SI item was transposed to the CLSS item with a AUA SI score of 0 correlating to a CLSS score of 0, 1 correlating to 1, 2 or 3 correlating to 2 and 4 or 5 correlating to 3, respectively.
To assess urge incontinence symptoms all patients were asked a validated question from the CLSS outcome measure, that is how often each one experienced “leaking of urine because you cannot hold it.” Responses were graded on a Likert scale of 0 to 3, including 0—no, 1—rarely, 2—sometimes and 3—often. Since there is no item in the AUA SI about urge incontinence, only responses from CLSS were assessed.
Patients were administered the outcome measures before and 2 months or more after surgery. For patients with multiple postoperative evaluations the most recent postoperative symptom score (the score at the furthest date from surgery) was used.
To evaluate the presence of urinary urgency and urge incontinence as an outcome symptoms were dichotomized with responses occurring never or rarely (CLSS score 0 or 1) considered absent and symptoms occurring sometimes or often (CLSS score 2 or 3) considered present. Improvement of symptoms from preoperative to postoperative time points was defined as moving from present to absent symptoms. Worsening symptoms from preoperative to postoperative time points was defined as moving from absent to present symptoms. Outcomes were dichotomized as we believed it to be more clinically relevant. For example, a change in urgency score of 0 (never) to 1 (rarely) did not seem to be as clinically relevant as a change from never or rarely having symptoms to sometimes or often having symptoms. Similarly, we did not think that an improvement from a score of 3 (often) to 2 (sometimes) represented a clinically significant difference.
Univariate analysis was performed to evaluate the association of patient demographic characteristics with preoperative and postoperative urge related symptoms as well as improvement or worsening of urge related symptoms. Stricture recurrence was defined as the need for an adjuvant procedure to maintain urethral patency. Statistical analysis included univariate analysis using the chi-square test with the Fisher test as necessary for small cell sizes as well as the t-test, ANOVA and logistic regression to determine ORs. Multivariate logistic regression analysis was performed using variables significant on univariate analysis when more than 1 predictor was significant on univariate analysis. STATA®, version 13 was used for analysis with 2-tailed p <0.05 considered significant.
RESULTS
Urinary Urgency
The 439 men with complete urinary urgency followup data were included in the final cohort analysis. Mean followup was 15.3 months (range 2.0 to 79.5). Of the cohort 58% reported having urgency preoperatively compared to 40% who reported symptoms postoperatively (p <0.01). Compared to patients with urgency symptoms preoperatively those without preoperative urgency were more likely to have a bulbar stricture (p <0.01) and undergo buccal urethroplasty (p = 0.01) or a penile fasciocutaneous flap procedure (p = 0.02) on univariate analysis (table 1). All of these predictors remained significant on multivariate analysis (bulbar stricture p <0.01, buccal urethroplasty p = 0.01 and penile fasciocutaneous flap p = 0.02). Compared to patients with postoperative urgency symptoms those without postoperative urgency were more likely to have a bulbar stricture (p = 0.01) and less likely to have stricture recurrence (p = 0.01). These predictors remained significant on multivariate analysis (bulbar stricture p = 0.04 and stricture recurrence p = 0.02).
Table 1.
Demographics by preoperative and postoperative urgency symptoms for anterior strictures
| Preop | Postop | ||||||
|---|---|---|---|---|---|---|---|
| Overall | No Urgency | Urgency | p Value | No Urgency | Urgency | p Value | |
| No. pts | 439 | 185 | 254 | _ | 262 | 177 | — |
| Mean ± SD followup (mos) | 15.3 ± 15.6 | 15.2 ± 16.4 | 15.3 ± 14.9 | 0.95 | 14.4 ± 15.9 | 17.3 ± 14.9 | 0.12 |
| Mean ± SD age | 45.0 ± 16.0 | 44.5 ± 16.0 | 45.4 ± 15.9 | 0.56 | 43.9 ± 15.6 | 46.7 ± 16.3 | 0.07 |
| Mean ± SD BMI (kg/m2) | 30.0 ± 6.8 | 29.6 ± 5.9 | 30.3 ± 7.3 | 0.27 | 29.7 ± 6.2 | 30.3 ± 7.5 | 0.33 |
| Mean ± SD stricture length (cm) | 3.5 ± 2.5 | 3.2 ± 1.8 | 3.7 ± 2.9 | 0.05 | 3.3 ± 2.4 | 3.7 ± 2.8 | 0.06 |
| No. stricture location (%): | |||||||
| Penile | 35 (8.0) | 15 (8.1) | 20 (7.9) | 0.06 | 20 (7.6) | 15 (8.5) | 0.19 |
| Bulbar | 357 (81.3) | 159 (86.0) | 198 (78.0) | <0.01 | 222 (84.7) | 135 (76.3) | 0.01 |
| Penobulbar | 47 (10.7) | 11 (6.0) | 36 (14.2) | 0.99 | 20 (7.6) | 27 (15.3) | 0.99 |
| No. urethroplasty type (%): | |||||||
| Buccal | 147 (34.0) | 70 (38.3) | 77 (30.8) | 0.01 | 82 (31.5) | 65 (37.6) | 0.45 |
| Augmented | 34 (7.9) | 13 (7.1) | 21 (8.4) | 0.14 | 19 (7.3) | 15 (8.7) | 0.55 |
| Excision + primary anastomosis | 213 (49.2) | 87 (47.5) | 126 (50.4) | 0.05 | 136 (52.3) | 77 (44.5) | 0.13 |
| Penile fasciocutaneous flap | 14 (3.2) | 8 (4.4) | 6 (2.4) | 0.02 | 11 (4.2) | 3 (1.7) | 0.06 |
| Perineal urethrostomy | 25 (5.8) | 5 (2.7) | 20 (8.0) | 0.99 | 12 (4.6) | 13 (7.5) | 0.99 |
| Combined approach | 6 (1.4) | 2 (1.1) | 4 (1.6) | 0.46 | 2 (0.8) | 4 (2.3) | 0.12 |
| No. recurrence (%) | 31 (7.1) | 9 (4.9) | 22 (8.7) | 0.14 | 12 (4.6) | 19 (10.7) | 0.01 |
Patients were asked how often they experienced sudden strong desire to urinate that was difficult to postpone, which was graded on Likert scale, including 0—never, 1—rarely, 2—sometimes, 3—often using CLSS, and how often they found it difficult to postpone urination, which was graded on Likert scale, including 0—not at all, 1—less than 1 in 5 times, 2—less than half time, 3—about half time, 4—more than half time and 5—almost always using AUA-SI with AUA-SI score 0 correlating to CLSS score 0, 1 correlating to 1, 2 or 3 correlating to 2 and 4 or 5 correlating to 3, respectively, and with no urgency scored as CLSS 0 or 1 and urgency scored as CLSS 1 or 2.
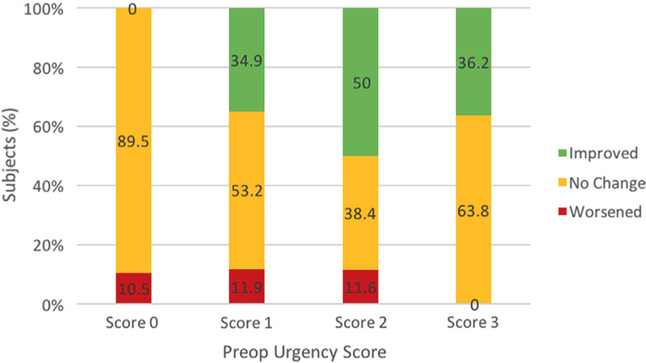
When evaluating a change in urgency symptoms after urethroplasty, 21% of men overall noticed improvement, symptoms remained stable in 75% and symptoms worsened in 4% (fig. 1). Of men with urgency preoperatively 37% noticed symptom improvement. Men who experienced recurrence were less likely to have symptom improvement on univariate analysis (OR 0.24, p = 0.03, table 2). Of men who did not have urgency preoperatively 9% noticed symptom worsening. Men with a higher BMI were more likely to have symptom worsening after urethroplasty on univariate analysis (for each additional BMI unit OR 1.09, p = 0.02).
Figure 1.
Change in urgency symptoms after anterior urethroplasty. Patients were asked how often they experienced sudden strong desire to urinate that was difficult to postpone, which was graded on CLSS Likert scale, including 0—never, 1—rarely, 2—sometimes and 3—often. Patients were asked how often they found it difficult to postpone urination, which was graded on AUA SI Likert scale, including 0—not at all, 1—less than 1 in 5 times, 2—less than half time, 3—about half time, 4—more than half time and 5—almost always. AUA SI score 0 correlates to CLSS score 0, 1 correlates to 1, 2 or 3 correlates to 2 and 4 or 5 correlates to 3, respectively.
Table 2.
Univariate analysis of worse or improved symptoms after anterior urethroplasty
| Worse Urgency | Improved Urgency | Worse Urge Incontinence | Improved Urge Incontinence | |||||
|---|---|---|---|---|---|---|---|---|
| OR | p Value | OR | p Value | OR | p Value | OR | p Value | |
| Age | 1.00 | 0.94 | 0.98 | 0.05 | 1.06 | 0.01 | 0.92 | <0.01 |
| BMI | 1.09 | 0.02 | 1.01 | 0.55 | 0.98 | 0.08 | 0.97 | 0.26 |
| Urethroplasty: | ||||||||
| Buccal | 1.03 | 0.97 | 0.70 | 0.50 | 0.79 | 0.72 | 0.85 | 0.89 |
| Augmented | 0.58 | 0.72 | 0.93 | 0.91 | 1.00 | 0.99 | 0.33 | 0.40 |
| Excision + primary anastomosis | 0.52 | 0.57 | 1.44 | 0.47 | 1.00 | 0.99 | 1.39 | 0.79 |
| Penile fasciocutaneous flap | 1.00 | 0.99 | 3.71 | 0.18 | 1.00 | 0.99 | 1.00 | 0.99 |
| Perineal urethrostomy | 1.00 | 0.99 | 1.00 | 0.99 | 1.00 | 0.99 | 1.00 | 0.99 |
| Combined approach | 1.00 | 0.99 | 1.00 | 0.99 | 1.00 | 0.99 | 1.00 | 0.99 |
| Stricture location: | ||||||||
| Penile | 2.59 | 0.18 | 2.00 | 0.25 | 1.00 | 0.99 | 1.46 | 0.70 |
| Bulbar | 1.00 | 0.99 | 1.91 | 0.12 | 0.96 | 0.97 | 1.18 | 0.78 |
| Penobulbar | 1.00 | 0.99 | 1.00 | 0.99 | 1.00 | 0.99 | 1.00 | 0.99 |
| Stricture length | 0.99 | 0.94 | 0.96 | 0.34 | 0.94 | 0.64 | 1.03 | 0.71 |
| Recurrence | 1.00 | 0.99 | 0.24 | 0.03 | 3.20 | 0.17 | 0.51 | 0.48 |
Urinary Urge Incontinence
The 305 men with complete urge incontinence followup data were included in the final cohort analysis. Mean followup was 9.2 months (range 2.3 to 52.5). Preoperatively, 31% of the cohort reported having urge incontinence symptoms compared to 12% who reported symptoms postoperatively (p <0.01). Compared to patients without preoperative urge incontinence symptoms those with preoperative urge incontinence were more likely to be older (p <0.01), have a longer stricture (p = 0.02) and be less likely to have a bulbar stricture (p = 0.01) on univariate analysis (table 3). On multivariate analysis only age remained a significant predictor (for each additional year of age OR 1.02, p = 0.03). Compared to patients without postoperative urinary urge incontinence those with postoperative urge incontinence were significantly more likely to be older (p <0.01).
Table 3.
Demographics by preoperative and postoperative urge incontinence symptoms for anterior urethroplasty
| Preop Urge Incontinence | Postop Urge Incontinence | ||||||
|---|---|---|---|---|---|---|---|
| Overall | No | Yes | p Value | No | Yes | p Value | |
| No. pts | 305 | 210 | 95 | _ | 269 | 36 | _ |
| Mean ± SD followup (mos) | 9.2 ± 8.5 | 8.9 ± 7.9 | 9.8 ± 9.7 | 0.40 | 9.1 ± 8.6 | 9.9 ± 8.4 | 0.61 |
| Mean ± SD age | 45.4 ± 16.0 | 43.6 ± 15.6 | 49.4 ± 16.1 | <0.01 | 43.5 ± 15.0 | 60.0 ± 15.5 | <0.01 |
| Mean ± SD stricture length (cm) | 3.8 ± 2.9 | 3.6 ± 2.7 | 4.4 ± 2.9 | 0.02 | 3.8 ± 3.0 | 3.9 ± 2.3 | 0.95 |
| No. stricture location (%) | |||||||
| Penile | 25 (8.2) | 16 (7.6) | 9 (9.5) | 0.29 | 23 (8.6) | 2 (5.6) | 0.30 |
| Bulbar | 246 (80.7) | 177 (84.3) | 69 (72.6) | 0.01 | 218 (81.0) | 28 (77.8) | 0.30 |
| Penobulbar | 34 (11.2) | 17 (8.1) | 17 (17.9) | 0.99 | 28 (10.4) | 6 (16.7) | 0.99 |
| No. urethroplasty type (%) | |||||||
| Buccal | 123 (41.1) | 77 (37.4) | 46 (49.5) | 0.70 | 106 (40.3) | 17 (47.2) | 0.82 |
| Augmented | 21 (7.0) | 11 (5.3) | 10 (10.8) | 0.87 | 16 (6.1) | 5 (13.9) | 0.44 |
| Excision + primary anastomosis | 139 (46.5) | 108 (52.4) | 31 (33.3) | 0.14 | 126 (47.9) | 13 (36.1) | 0.86 |
| Penile fasciocutaneous flap | 7 (2.3) | 5 (2.4) | 2 (2.1) | 0.40 | 7 (2.7) | 0 | 0.99 |
| Perineal urethrostomy | 9 (3.0) | 5 (2.4) | 4 (4.3) | 0.99 | 8 (3.0) | 1 (2.8) | 0.99 |
| Combined approach | 6 (2.0) | 4 (1.9) | 2 (2.1) | 0.88 | 6 (2.2) | 0 | 0.99 |
| No. recurrence (%) | 20 (6.6) | 15 (7.1) | 5 (5.3) | 0.63 | 16 (6.0) | 4 (11.1) | 0.27 |
Patients were asked how often they experienced leaking of urine because they could not hold it to assess urge incontinence symptoms, which was graded on Likert scale, including 0—never, 1—rarely, 2—sometimes and 3—often with no urge incontinence scored as 0 or 1 and urge incontinence scored as 1 or 2.
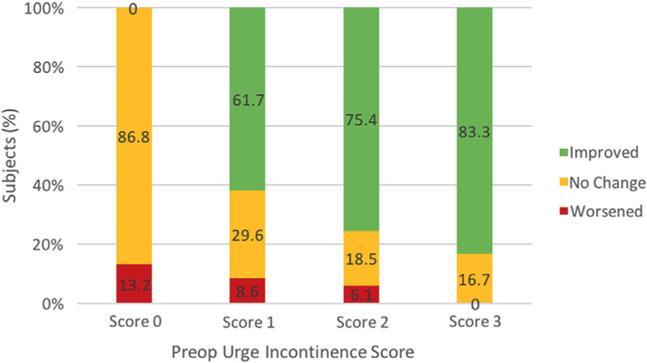
When evaluating a change in urge incontinence symptoms after anterior urethroplasty, 23% of men noticed improvement, symptoms remained stable in 73% and symptoms worsened in 4% (fig. 2). Of men who had urge incontinence preoperatively 74% noticed symptom improvement after urethroplasty. Older men were less likely to experience symptom improvement on univariate analysis (for each additional year of age OR 0.92, p <0.01, table 2). Of men who did not have urge incontinence preoperatively 5% noticed symptom worsening after urethroplasty. On univariate analysis urge incontinence symptoms were more likely to develop after urethroplasty in older men (OR 1.06 for each additional year of age, p = 0.01).
Figure 2.
Change in urge incontinence symptoms after anterior urethroplasty. To assess urge incontinence symptoms patients were asked how often they experienced urine leaking because of inability to hold urine, which was graded on Likert scale, including 0—never, 1—rarely, 2—some and 3—often.
DISCUSSION
We noted a high prevalence of urgency and urge incontinence among patients with urethral stricture before anterior urethroplasty. Several large studies have sought to determine the prevalence of urgency symptoms in the general population. The SIFO (Swedish Institute for Opinion Surveys) study showed that 16.6% of the general population experienced symptoms of overactive bladder with urgency in 54% and urge incontinence in 36%.9 Similarly, the NOBLE (National Overactive Bladder Evaluation) study revealed that the prevalence of overactive bladder in men was 16.0% and the prevalence of men with overactive bladder and urge incontinence was 2.6%.10 The EPIC study, which specifically evaluated symptoms of urgency and urge incontinence, demonstrated that 10.8% of men experienced urgency and only 1.2% experienced urge incontinence.11 In contrast, in our population of male patients with anterior urethral stricture we found that more than 50% experienced significant urgency and almost a third experienced significant urge incontinence at presentation. Our data echo a recent single surgeon series that showed a 67% incidence of clinically significant overactive bladder symptoms among patients with stricture.6
Age was an important predictor of urge incontinence. We noted that urge incontinence was a more common presenting symptom among men with increasing age and older men were more likely to experience postoperative symptoms as well. These findings echo data from population based studies showing an increasing prevalence of urgency and urge incontinence with age.9–11 This was further validated in our evaluation of a change in urge incontinence after urethroplasty. We found that older age was associated with a higher likelihood of worse symptoms and a lower likelihood of symptom improvement after urethroplasty.
Given the high preponderance of urgency and urge incontinence among patients with stricture, it is important to understand the effect of anterior urethroplasty on these symptoms to improve patient counseling and set appropriate patient expectations. Our data show that many men with urge related symptoms, whether urgency or urge incontinence, will experience symptom improvement after anterior urethroplasty. Overall 91% of men demonstrated stable or improved urgency symptoms and 96% had stable or improved urge incontinence symptoms. Patients were more likely to experience improvement in urgency symptoms if stricture did not recur. Because so many men with stricture reported significant urgency symptoms at presentation, it makes sense that while symptoms may improve in the short term after repair, patients might ultimately experience a relapse in urgency symptoms if the stricture recurs.
Few patients demonstrated new or worse symptoms after surgery. We found that BMI correlated with worse urgency symptoms after anterior urethroplasty. To our knowledge these findings have not been previously studied in men but they echo data from studies in women showing that urgency symptoms are more common in patients with a higher BMI.12,13 In addition, although our data were not robust enough to evaluate predictors such as a history of radiation or prostate surgery, it is likely that such factors also have a role in worsening urinary urgency or urge incontinence. These other previous treatments or possible contributing comorbidities are also important aspects to keep in mind when counseling these patients about expectations following surgery.
Urgency and urge incontinence have a significant impact on quality of life. Overactive bladder symptoms and urge incontinence have been associated with poorer health related quality of life scores, higher depression scores and poorer quality of sleep scores compared to those of matched controls.10 Furthermore, overactive bladder has been associated with a higher risk of injury in a fall and more self-reported urinary tract infections, and it represents a significant cost to the health care system.14–16 Our results suggest that anterior urethroplasty may improve patient overall quality of life merely by improving urgency and urge incontinence symptoms.
This study has several limitations, including the main limitation of incomplete data in our data set, which precluded us from analyzing several potentially important comorbidities as predictors of urge related symptoms. For example, we did not have enough power to report the presence of diabetes, benign prostatic hyperplasia, a history of transurethral prostate resection, or a history of radiation or surgery for prostate cancer. Upon review of these comorbidities in our data set we believed that the low prevalence and the lack of significance on univariate analysis reflected incomplete data entry rather than a true representation of the cohort.
In addition, we only had full urge related symptom followup data on a subset of patients in our database. Additionally, a minority of patients with urgency data used the validated urgency question from the AUA SI rather than the CLSS questionnaire, which required transposition to the CLSS Likert scale. The CLSS assessment uses a Likert ranking of 0 to 3. A wider Likert scale may have allowed for more detailed analysis of urge related symptoms.
This study also has many strengths. The data were compiled from multiple institutions where patient reported outcome measures were used before and after surgery. We also report the medium term duration of symptom assessment followup after urethroplasty. In our urgency cohort only 15 of 439 patients had less than 3-month followup at the time of patient reported outcome measure completion. In our urge incontinence cohort only 18 of 305 patients had less than 3-month followup at the time of patient reported outcome measure completion.
To our knowledge our study represents the largest experience to date that provides not only data on changes in urge and urge incontinence after urethroplasty but also robust baseline prevalence data. With longer followup after urethroplasty we may even see a higher proportion of patients with improved symptoms if we believe that detrusor remodeling occurs after the relief of obstruction.
CONCLUSIONS
Urinary urgency and urge incontinence are prevalent in men with anterior urethral stricture disease. Men with a bulbar stricture are more likely to experience urgency symptoms preoperatively and postoperatively. Fortunately, symptom improvement or stability is seen in the majority of men after anterior urethroplasty. Men with a higher BMI are more likely to experience new urgency after urethroplasty and those in whom stricture recurs are less likely to experience symptom improvement after urethroplasty. Older men are more likely to have urge incontinence symptoms preoperatively and postoperatively. Those who are older are more likely to have new symptoms and less likely to experience improvement in urge incontinence after urethroplasty.
Abbreviations and Acronyms
- AUA SI
American Urological Association Symptom Index
- BMI
body mass index
- CLSS
Core Lower Urinary Tract Symptom Score
Footnotes
Presented at annual meeting of Western Section American Urological Association, Indian Wells, California, October 25, 2015.
REFERENCES
- 1.Nuss GR, Granieri MA, Zhao LC et al. : Presenting symptoms of anterior urethral stricture disease: a disease specific, patient reported questionnaire to measure outcomes. J Urol 2012; 187: 559. [DOI] [PubMed] [Google Scholar]
- 2.Ching CB, Wood HM, Ross JH et al. : The Cleveland Clinic experience with adult hypospadias patients undergoing repair: their presentation and a new classification system. BJU Int 2011; 107: 1142. [DOI] [PubMed] [Google Scholar]
- 3.Eltahawy EA, Virasoro R, Schlossberg SM et al. : Long-term followup for excision and primary anastomosis for anterior urethral strictures. J Urol 2007; 177: 1803. [DOI] [PubMed] [Google Scholar]
- 4.Andrich DE, Dunglison N, Greenwell TJ et al. : The long-term results of urethroplasty. J Urol 2003; 170: 90. [DOI] [PubMed] [Google Scholar]
- 5.Santucci RA, Mario LA and McAninch JW: Anastomotic urethroplasty for bulbar urethral stricture: analysis of 168 patients. J Urol 2002; 167: 1715. [PubMed] [Google Scholar]
- 6.Osterberg EC, Schulster M, Blaivas JG et al. : Urethroplasty improves overactive bladder symptoms in men with anterior urethral strictures. Urology 2016; 93: 208. [DOI] [PubMed] [Google Scholar]
- 7.Homma Y, Yoshida M, Yamanishi T et al. : Core Lower Urinary Tract Symptom score (CLSS) questionnaire: a reliable tool in the overall assessment of lower urinary tract symptoms. Int J Urol 2008; 15: 816. [DOI] [PubMed] [Google Scholar]
- 8.Barry MJ, Fowler FJ, O’Leary MP et al. : The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992; 148: 1549. [DOI] [PubMed] [Google Scholar]
- 9.Milsom I, Abrams P, Cardozo L et al. : How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int 2001; 87: 760. [DOI] [PubMed] [Google Scholar]
- 10.Stewart WF, Van Rooyen JB, Cundiff GW et al. : Prevalence and burden of overactive bladder in the United States. World J Urol 2003; 20: 327. [DOI] [PubMed] [Google Scholar]
- 11.Irwin DE, Milsom I, Hunskaar S et al. : Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 2006; 50: 1306. [DOI] [PubMed] [Google Scholar]
- 12.Palma T, Raimondi M, Souto S et al. : Correlation between body mass index and overactive bladder symptoms in pre-menopausal women. Rev Assoc Med Bras 2014; 60: 111. [DOI] [PubMed] [Google Scholar]
- 13.Alling Møller L, Lose G and Jørgensen T: Risk factors for lower urinary tract symptoms in women 40 to 60 years of age. Obstet Gynecol 2000; 96: 446. [PubMed] [Google Scholar]
- 14.Wagner TH, Hu TW, Bentkover J et al. : Health-related consequences of overactive bladder. Am J Manag Care, suppl., 2002; 8: S598. [PubMed] [Google Scholar]
- 15.Tubaro A and Palleschi G: Overactive bladder: epidemiology and social impact. Curr Opin Obstet Gynecol 2005; 17: 507. [DOI] [PubMed] [Google Scholar]
- 16.Tubaro A: Defining overactive bladder: epidemiology and burden of disease. Urology 2004; 64: 2. [DOI] [PubMed] [Google Scholar]