Abstract
There are few HIV risk reduction interventions to meet the unique needs of women who experience intimate partner violence (IPV). This pilot study tested the feasibility, safety, and preliminary effects of an integrated IPV-sexual risk reduction intervention for abused women. Fifty-five women were randomized to the supporting positive and healthy relationships (SUPPORT) intervention (n = 27) or to a control group (n = 28). Assessments were conducted pre- and post-intervention and at 3-month follow-up. Post-intervention, SUPPORT participants showed a significant decrease in frequency of unprotected sex and an increase in safer sex communications with steady and other sexual partners. Compared to the control group, SUPPORT participants reported a higher number of safer sex conversations with their steady partner at the 3-month follow-up, and fewer episodes of IPV at both assessments in comparison to baseline. They showed improvements in sexual relationship power at both follow-ups and in several hypothesized antecedents of HIV-risk behavior. These encouraging preliminary findings suggest the need for a larger clinical trial.
Keywords: Intimate partner violence, HIV, Sexual risk behaviors, Intervention, Women
Introduction
HIV infection continues to be a serious public health issue. Currently, more than 1.1 million people are living with HIV/AIDS in the United States (US) [1]. Of these, one in four are women. In 2010, women accounted for nearly 20 % of all the new HIV infections reported in the US with heterosexual contact identified as the primary (84 %) transmission route [1]. Over the last 15 years, research studies and several review papers have highlighted the role of intimate partner violence (IPV) in HIV acquisition among women [2–8]. Recent longitudinal, prospective studies have shown that IPV increases the risk for incident HIV infection among women by as much as 12–22 % [9, 10].
Cross-sectional studies have identified multiple pathways linking the epidemics of HIV and IPV. Abused women may use condoms less frequently [11–14], be forced or coerced to have unprotected sex [11, 14], experience fear of violent consequences when negotiating condom use [15, 16], and have diminished power to negotiate safer sex [14, 17]. They may engage in high-risk sexual behavior by having multiple or concurrent sexual partners [18], having sex with high-risk partners such as injection drug users or those with unknown HIV status [19–21], and trading sex for money or drugs [19, 22].
Abusive men are also more likely to participate in sexual risk behaviors [23, 24] and use condoms infrequently [12]. Women with abuse histories often struggle with mental health issues such as depression, PTSD, anxiety, and lower self-esteem, and they often use alcohol and/or other drugs to cope with their trauma [25–28]. They also report a higher incidence of sexually transmitted infections and other gynecological conditions [29–31]. All these problems have also been identified as risk markers for HIV infection [32].
Although research has established a strong link between IPV and subsequent HIV infection, there are few empirically-supported interventions that address the unique needs of women who experience IPV and who are at increased risk for contracting HIV [33–38]. To address this critical gap in the literature, we developed an integrated, HIV-IPV prevention intervention for racially-diverse, economically-disadvantaged, and community-based abused women.
The primary aims of this pilot study were to test the feasibility, safety, and preliminary short-term efficacy of an 8-week, theoretically-guided, psychosocial intervention to simultaneously reduce women's experiences of IPV and their risk for HIV infection. We hypothesized that the integrated IPV-HIV intervention would lead to greater reductions in HIV risk as well as experiences of IPV in comparison to the control condition.
Methods
Sample Recruitment and Selection
Recruitment was conducted between June 2012 and May 2013. Trained research assistants (RAs) recruited potential participants from several sites in upstate New York, including women's health clinics, hospitals, domestic violence agencies, Family Court, and the Department of Social Services. Women were approached by the RAs while waiting for appointments or directly after appointments. Flyers and brochures containing basic study information and contact phone numbers were also distributed at these locations. The RAs also recruited participants from support groups at community agencies. To assess eligibility, the trained RAs asked brief screening questions of the women who were interested in participating in the study (n = 204). To meet eligibility criteria, women had to report (1) being between the ages of 18 and 49; (2) having experienced physical, emotional, or sexual violence by any sexual partner in the past 3 months; and (3) having engaged in risky sexual behavior (inconsistent condom use and having multiple sexual partners or a partner who had more than one sexual partner; any sexual partner was HIV-positive; or any sexual partner injected drugs) in the past 3 months. Women were excluded if they (1) did not speak or understand English; (2) were exclusively in same-sex relationships; or (3) were pregnant or were trying to conceive at the time of the study. Regardless of eligibility for the study, women were given a list of community support resources for agencies in the area, including a battered women's shelter, reproductive health centers, continuing education, and drug or alcohol dependency treatment. All study procedures were reviewed and approved by the institutional review boards of participating institutions.
Procedures
Eligible women (n = 79) were invited to schedule their first appointment with a trained RA at a convenient location in the community. At this appointment, women provided informed consent and completed a comprehensive calendar of meaningful events from the past 3 months to facilitate their recall of time-linked information in the baseline survey [39–41]. Participants then responded to an audio computer-assisted self-interview (ACASI). Fifty-five women completed this first appointment. After providing informed consent and completing the baseline survey, the 55 women were randomized to the supporting positive and healthy relationships (SUPPORT) intervention group (n = 27) or the control group (n = 28). The random allocation sequence was created using SAS and consisted of a sequence of group assignments within blocks of 10.
Participants who completed the baseline appointment received $25, a parking or bus pass, and a light snack. For each completed intervention or control group session, participants were given $10, a parking or bus pass, and light refreshments. In addition, they received $30 for completing a post-intervention assessment after the 8-week intervention, and $40 for completing a 3-month follow up assessment. Participants who completed all three assessments were entered into a lottery to win a $100 gift card.
Interventions
SUPPORT Intervention
The theoretical framework for the SUPPORT intervention combined key elements of three models. The Information–Motivation–Behavioral-Skills (IMB) Model is an intervention-oriented framework that combines aspects of social cognitive theory [42] and other widely used health behavior models [43] to reduce health-related risk behaviors. According to the model, the initiation and maintenance of preventive behaviors occur on the basis of information about the health issue, motivation to engage in the preventive behaviors, and behavioral skills required to perform preventive acts [44]. The SUPPORT intervention also integrated the Theory of Gender and Power (TGP; [45]), acknowledging the importance of attending to social contextual factors specifically related to women and their risk for HIV. TGP highlights the relational and contextual influences that impact women in intimate relationships, reconceptualizing HIV risk as a function of such variables as sexual and economic power. The third model that informed the intervention was transitional family therapy [46], a family systems model that helps women examine their lives through the lens of intergenerational transmission of unresolved grief, trauma, and loss, and that leverages family motivation for change. Information gathered during individual and focus group interviews from women with experiences of IPV also influenced the design of the intervention.
The SUPPORT intervention consisted of eight weekly intervention sessions (three individual and five group) that were between 2 and 2.5 h long. Both the individual and the group sessions began with a 5-min exercise in mindfulness meditation where the participants listened to and followed along with an audio recording. Women were also given a CD of the audio recording and asked to practice for 5 min every day between the intervention sessions. The purpose of this mindfulness “warm up” was to help the participants be present focused and to become aware of their thoughts and feelings without judging them.
The three individual sessions (sessions 1, 3, and 4) were focused on developing a 3- to 5-generation genogram with the participants. These sessions highlighted: (1) intergenerational transmission of unresolved trauma, loss, and grief; (2) family strengths and resilience; (3) sources of personal support and triggers; (4) psycho-education on the family life cycle; and (5) a recovery message for positive change and hope for future generations. The purpose of this set of exercises was to help empower the participants to take charge of change in their lives and in the lives of subsequent generations by understanding the link between intergenerational trauma and the here-and-now.
The five group sessions included psycho-education and activities focused on STDs and HIV-infection, IPV, safety and self-protection, and choosing a healthy lifestyle. The goals of the group sessions were to (1) increase HIV-related knowledge, motivation, and skills to practice safer sex; (2) deconstruct healthy and unhealthy relationships; (3) understand the impact of psychological trauma and violence on the participant and her relationships; (4) develop a safety plan; (5) understand the interconnection between IPV and STD/HIV infection; (6) analyze protective versus self-destructive decision-making; and (7) develop a grieving ritual to enable the participant and her family to move on from the past. The group facilitator emphasized the importance of confidentiality during the sessions and asked the participants about any new experiences of violence victimization every week. At the end of each session, participants were given a homework assignment to be completed prior to the next session. The facilitator called participants midweek to check on them and the progress of the homework. They brainstormed ideas for overcoming difficulties with the homework assignments, if any were presented.
Control Group
The control intervention was an IPV reduction intervention that was developed by a local domestic violence agency. The control group consisted of 8 weekly group-based intervention sessions that were 1–1.5 h in length. A different topic was addressed each week and informational handouts were shared with the participants. The group intervention covered the following topics: (1) what is abuse?; (2) the abuse cycle; (3) the impact of abuse on children; (4) grief, fear and guilt; (5) self-esteem and personal rights; (6) boundary setting and assertiveness; (7) setting realistic goals; and (8) healthy relationships and safety planning.
Facilitator Training and Intervention Quality Assurance
The SUPPORT intervention and control groups were each led by one facilitator. Both facilitators had a mental health degree and were experienced in working with abused women. A number of procedures were implemented to assure adherence to the treatment protocol. The interventions were manualized and the intervention sessions were recorded. The facilitators also maintained case notes that documented information about the activities and process of the sessions. The PI reviewed the tapes and case notes and met weekly with the facilitators for supervision.
Measures
Demographics
Demographic characteristics were self-reported, including participants’ race, income (re-coded as <$15,000 vs. ≥$15,000), education (recoded as high school or less vs. more than high school), age, and employment (re-coded as employed vs. unemployed). Participants were also asked whether they ever traded sex for money or drugs.
Feasibility
Participants were considered enrolled in the assigned condition if they attended at least one intervention session, and they were considered as having received an adequate dose of treatment if they attended five or more sessions. We also counted attendance at the follow-up sessions to determine the feasibility of conducting a randomized controlled trial and outcomes research on this topic.
Safety
To assess safety, we used four measures of recent experiences of IPV. First, the 10-item Women's Experiences with Battering (WEB) scale [47] assessed participants’ perception of their vulnerability in their relationship during the past 3 months. Each item was scored on a 6-point scale from 1 (disagree strongly) to 6 (strongly agree). Potential total scores ranged between 10 and 60, with a score of 20 or higher considered a positive screening for battering (α = 0.95). Second, the Abuse Behavior Inventory (ABI) [48] assessed women's experiences of physical, sexual, and psychological violence during the past 3 months. Respondents answered 29 items on a 4-point Likert scale from 0 (never) to 4 (very frequently). Items were summed to produce a total ABI score with a possible range of 0 to 116. A cutoff value of 10 or higher is used to denote experiences of IPV (α = 0.96). Third, relationship power dynamics were measured using the 23-item Sexual Relationship Power Scale (SRPS) [49]. The SRPS contains two subscales, relationship control and decision-making dominance. Items on the relationship control subscale were scored from 1 (strongly agree) to 4 (strongly disagree), and items on the decision-making dominance subscale were scored as 1 (your partner), 2 (both of you equally), or 3 (you). Scores for each subscale were calculated separately, then combined with equal weighting and rescaled to produce a final score from 1 to 4. Higher scores indicated higher sexual relationship power (α = 0.91). Lastly, using an event-level assessment, participants were asked to report if they had experienced sexual and/or physical violence at their last sexual experience.
Efficacy (Primary Outcomes)
Primary outcomes were sexual behavior and safer sex communications. Sexual behavior outcomes were measured by the frequency of unprotected episodes of vaginal and anal sex with their steady partner, other sex partners, and across all sex partners in the past 3 months. Safer sex communications were measured by responses to the following question: “In the past 3 months, how many times have you talked with your steady and other partners before intercourse about using a condom or having safer sex?” Such measures have been used extensively in prior research [50–53].
Efficacy (Secondary Outcomes)
Guided by the IMB model, we measured hypothesized psychological antecedents of sexual risk behavior (i.e., information, motivation, behavioral skills). Additionally, we assessed for changes in mental health (i.e., depression, self-esteem, anxiety, PTSD) given the association between poor mental health and risk for IPV and HIV.
Information was assessed using two knowledge scales. The HIV-Knowledge Questionnaire (HIV-KQ-18) [54] tested knowledge of HIV-related information using true/false questions (α = 0.87). Participants’ knowledge of other sexually transmitted diseases (STDs) was measured with the 6-item STD Knowledge Questionnaire (STD-KQ) [55], modeled after the HIV-KQ (α = 0.72). Both knowledge measures were scored by dividing the number of correct responses by the total number of items. Greater scores indicate greater HIV and STD knowledge.
Two measures validated in previous studies were used to capture HIV-related motivation. Behavioral intentions to enact safer sex [50] were assessed by presenting a high-risk scenario to participants, who then completed five items indicating how likely they would be to engage in various risk-reducing behaviors if faced with the scenario. Responses ranged from 1 (definitely no) to 4 (definitely yes). Scores were calculated as an average of the responses, with higher scores suggesting stronger intentions to practice safer sex behaviors (α = 0.70). Participants’ current attitudes towards condoms were measured using items from existing scales [56, 57]. Participants responded to six items using a 6-point Likert scale from 1 = strongly disagree to 6 = strongly agree (α = 0.59). Items were averaged with higher scores indicating more favorable condom attitudes.
We measured HIV-related behavioral skills using two previously validated instruments. Self-efficacy was assessed with a validated measure [58] adapted for the current context. Women read two scenarios, one involving a steady partner and the other involving a new partner. After each scenario participants rated how confident they would feel about enacting six safer sex behaviors (0 = not at all confident to 10 = completely confident). Responses were averaged to calculate the self-efficacy score with higher scores signifying greater confidence in engaging in risk-reduction behaviors. Internal consistency reliability was 0.93 for this sample (steady partner subscale α = 0.87; new partner subscale α = 0.92).
Condom-negotiating skills were assessed with the 7-item Condom Influence Strategy Questionnaire—Short Form (CISQ-S) [59]. Participants indicated how often they used condom influence strategies with a partner during the past 3 months, from 1 = never to 5 = almost always (α = 0.96). The total CISQ score was the average of all items. A higher score reflected more frequent use of condom influence strategies.
Depression was measured by the 9-item Center for Epidemiologic Studies Depression Scale (CES-D) [60]. Participants reported how frequently they experienced depressive symptoms during the preceding week on a 4-point scale ranging from 0 = rarely/none of the time (less than 1 day) to 1 = more/all of the time (5–7 days). Scores were summed, with higher scores denoting more depressive symptoms (α = 0.86).
Self-esteem was measured with the 10-item Rosenberg Scale [61]. Participants scored each item on a 4-point Likert scale ranging from 0 (strongly agree) to 3 (strongly disagree). Scores were summed and higher total scores indicated higher self-esteem (α = 0.89).
Anxiety was measured with the Generalized Anxiety Disorder 7-item Scale (GAD-7) [62]. Respondents were asked to rate how often they had been bothered by certain problems in the last 2-week period. Responses were assigned scores of 0 (not at all) to 3 (nearly every day; α = 0.93). The sum of all items produced the GAD-7 total score.
PTSD symptoms were assessed with the PTSD Symptom Scale—Self-Report Version (PSS-SR) [63]. Participants rated 17 items on a 4-point Likert scale to indicate how frequently they had experienced a range of symptoms in the past 2 weeks, from 0 (not at all) to 3 (almost always or five or more times per week). Items were summed and a total score higher than 13 signified a greater likelihood of PTSD (α = 0.93).
Data Analysis
All measures were compared between experimental and control groups using Chi square tests and two-sample independent t-tests. Generalized estimating equation (GEE) method was applied to perform the multivariable modeling of outcomes against intervention wherein participants’ baseline characteristics (e.g., race, age, income, relationship status, and baseline measurements for each of the outcomes) were controlled. In the multivariable modeling, the link function of identity distribution was used to analyze continuous outcomes, and the link function of Poisson distribution was used to analyze count data (i.e., number of unprotected events, steady partner and other partners) with an over dispersion parameter to account for the heterogeneity between subjects. We chose Poisson regression over Negative Binomial because of better model fit with deviance around 1.0. Data were inspected for outliers [>3 × the interquartile range (IQR) from the 75th percentile] and trimmed (to 3 × IQR from the 75th percentile + 1). Analyses were performed with α set at 0.05 (to minimize the chance of Type II error given the pilot nature of this research).
Results
Participants
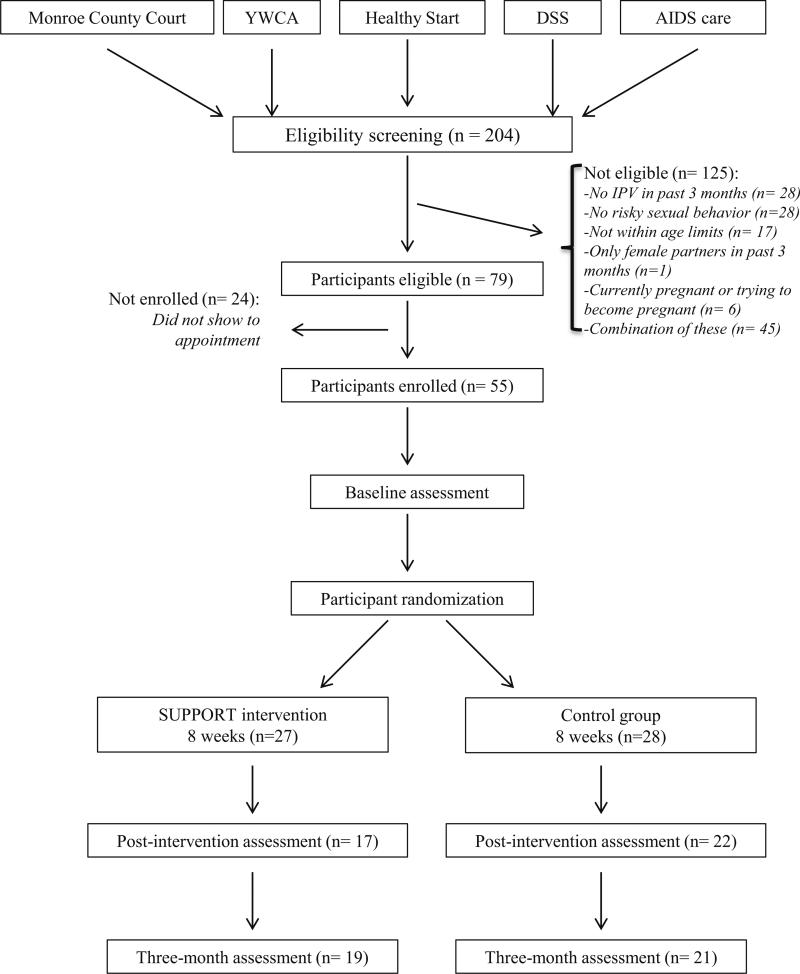
Figure 1 provides participant flow and recruitment data. A total of 357 women expressed interest in the study. A small number of them (n = 19) could not be reached using the contact information that they provided (loss of cell phone service and housing instability were common among the women). Of the 338 women contacted and given a detailed study description, 134 declined to be screened. The main reasons for declining screening included: no experience of IPV (n = 41), lack of time (n = 20), childcare and transportation issues (n = 12), not interested in counseling (n = 19), receiving other treatment (n = 15), and relocating to another city (n = 4). Twenty-three women did not provide a reason for lack of interest in participating in the study. Out of the remaining 204 participants screened for eligibility, 79 (39 %) were found to be eligible and were invited to participate in the study. Twenty-four women did not attend their first appointment; thus, 55 women (70 %) were randomized into the trial.
Fig. 1.
Participant flow and recruitment data
Demographic characteristics are presented in Table 1. The participants, on average, were 34.5 years old (SD 7.68). Nearly 51 % of the women were African American (n = 28), and 33 % were Caucasian (n = 18). Twenty-six participants had a high school education or less (47 %). Nearly 62 % of the sample was unemployed (n = 34); 64 % had an annual income of <$15,000 (n = 35). More than half the participants had never been married in their lifetime (n = 29, 53 %). Participants reported a median of 19 lifetime partners, 1.5 partners in the past 3 months (SD 1.2), and an average of 21 episodes of unprotected sex in the past 3 months (SD 27.23). Participants reported high overall levels of experiences of violence (mean 53 [possible range 0–116], SD 30.50) and perceptions of battering (mean = 46 [possible range 10–60], SD 13.32).
Table 1.
Demographic characteristics by condition at baseline
| Total N = 55 n (%) | Control n = 28 n (%) | Intervention n = 27 n (%) | |
|---|---|---|---|
| Mean age (SD, range)* | 34.51 (7.68, 18–49) | 32.18 (7.07, 18–49) | 36.93 (7.66, 18–49) |
| Race** | |||
| African-American | 28 (51 %) | 14 (50 %) | 14 (52 %) |
| White | 18 (33 %) | 12 (43 %) | 6 (22 %) |
| Other races | 9 (16 %) | 2 (7 %) | 7 (26 %) |
| Education | |||
| Less than high school | 16 (29 %) | 8 (29 %) | 8 (30 %) |
| HS diploma or GED | 10 (18 %) | 5 (18 %) | 5 (18 %) |
| Some college | 18 (33 %) | 10 (36 %) | 8 (30 %) |
| College graduate | 11 (20 %) | 5 (18 %) | 6 (22 %) |
| Employment | |||
| Full time | 12 (22 %) | 6 (21.5 %) | 6 (22 %) |
| Part time | 9 (16 %) | 6 (21.5 %) | 3 (11 %) |
| Unemployment | 34 (62 %) | 16 (57 %) | 18 (67 %) |
| Single or married* | |||
| Single | 29 (53 %) | 19 (68 %) | 10 (37 %) |
| Married or been married | 26 (47 %) | 9 (32 %) | 17 (63 %) |
| Income*,a | |||
| <$15,000 | 35 (64 %) | 19 (68 %) | 16 (59 %) |
| $15,000–$30,000 | 13 (24 %) | 9 (32 %) | 4 (15 %) |
| $30,000–$45,000 | 4 (7 %) | 0 (0 %) | 4 (15 %) |
| $45,000 | 2 (4 %) | 0 (0 %) | 2 (7 %) |
| Number of children | |||
| 0 | 6 (11 %) | 3 (11 %) | 3 (11 %) |
| 1 | 19 (35 %) | 10 (36 %) | 9 (33 %) |
| 2+ | 30 (54 %) | 15 (53 %) | 15 (56 %) |
SD standard deviation, HS high school, GED general educational development credential
Significant difference between control and intervention groups, p < 0.05
Significant difference between control and intervention groups, p = 0.09
Income reported by 54 participants (n = 26 for intervention group)
Equivalence of Groups at Baseline
Of the 79 eligible women, 55 were randomly assigned to either the SUPPORT intervention (n = 27) or the control group (n = 28). The 24 eligible participants who did not enroll in the study differed from the 55 who enrolled in the study in terms of method of contact. Participants who were recruited via the phone were more likely to complete their baseline assessment as compared to those recruited in person, (χ2 (1, N = 79) = 6.06, p = 0.01). To determine the equivalence of the two randomized groups, we conducted t tests for continuous variables and Chi square tests for categorical variables. The two groups differed significantly in terms of age (t (53) = −2.39, p = 0.02), race (χ2 (2, N = 55) = 4.76, p = 0.09), relationship status (χ2 (1, N = 55) = 5.23, p = 0.02), and income (χ2 (3, N = 54) = 8.11, p = 0.04). Participants assigned to the SUPPORT intervention were, on average, older compared to women in the control group (37 vs. 32 years). Compared to women in the control group, participants in the SUPPORT intervention were more likely to be of races Other than Black or White (26 vs. 7 %), married at some point in their lifetime (63 vs. 32 %), and to report higher income (>$30,000/year, 22 vs. 0 %; see Table 1). Therefore, age, race, relationship status, and annual income were controlled in all analyses. There were no significant differences between intervention and control groups on baseline safety measures (see Table 2), sexual risk behavior outcomes (see Table 3), or secondary outcomes (see Table 5).
Table 2.
Means and standard errors of safety data by condition and over time
| Variable | Conditiona | Baseline |
Post-intervention |
3-month follow-up |
|||||
|---|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | Difference | M | SE | Difference | ||
| Women's experiences of battering (10–60) | SPT | 44.09 | 1.28 | 33.69 | 3.65 | −10.40a | 28.96 | 3.91 | −15.13a |
| CTL | 43.34 | 0.99 | 35.72 | 3.15 | −7.62a | 36.18 | 2.68 | −7.25a | |
| ABI total score (0–116) | SPT | 50.32 | 2.94 | 24.45 | 7.85 | −25.87a | 26.93 | 7.58 | −23.39a |
| CTL | 51.99 | 2.63 | 40.87 | 5.30 | −11.12 | 41.13 | 4.12 | −10.86 | |
| ABI physical violence (0–36) | SPT | 12.93 | 1.04 | 4.86 | 2.61 | −8.07a | 6.86 | 2.32 | −6.07a |
| CTL | 12.46 | 0.95 | 9.24 | 1.88 | −3.22 | 9.50 | 1.40 | −2.96 | |
| ABI psychological violence (0–68) | SPT | 33.56 | 1.65 | 18.00c | 4.66 | −15.56a | 18.56 | 4.74 | −15.00a |
| CTL | 35.73 | 1.63 | 29.29c | 3.16 | −6.44 | 29.46 | 2.91 | −6.27 | |
| ABI sexual violence (0–12) | SPT | 3.83 | 0.40 | 1.63 | 0.92 | −2.20 | 1.53 | 0.91 | −2.30a |
| CTL | 3.76 | 0.32 | 2.30 | 0.62 | −1.46 | 2.15 | 0.35 | −1.61a | |
| Sexual relationship power (1–1) | SPT | 2.30 | 0.07 | 2.88 | 0.27 | 0.58a | 2.99c | 0.21 | 0.69a |
| CTL | 2.35 | 0.08 | 2.37 | 0.15 | 0.02 | 2.29c | 0.15 | −0.06 | |
| Violence at last sex (0–1) | SPT | 0.41 | 0.06 | 0.23 | 0.14 | −0.18 | 0.01b | 0.13 | −0.40a |
| CTL | 0.29 | 0.07 | 0.13 | 0.09 | −0.16 | 0.15 | 0.08 | −0.14 | |
SPT SUPPORT intervention group, CTL control group, ABI Abuse Behavior Inventory
Within-group difference is significant compared to baseline
Mean is significantly different at 3-month compared to post-intervention
Mean of intervention group is significantly different than mean of control group
Table 3.
Means and equivalence of sexual risk behavior outcomes at baseline
| Variable | Condition | M | p value |
|---|---|---|---|
| Episodes unprotected sex, all partners | SPT | 28.00 | 0.11 |
| CTL | 15.38 | ||
| Episodes unprotected sex, steady partner | SPT | 27.73 | 0.21 |
| CTL | 17.10 | ||
| Episodes unprotected sex, other partners | SPT | 3.57 | 0.21 |
| CTL | 6.15 | ||
| Communications about safe sex, steady partner | SPT | 2.86 | 0.76 |
| CTL | 2.48 | ||
| Communications about safe sex, other partners | SPT | 5.64 | 0.95 |
| CTL | 5.92 |
SPT SUPPORT intervention group, CTL control group
Table 5.
Means and standard errors of secondary outcomes by condition and over time
| Variable (range) | Condition | Baseline |
Post-intervention |
3-month follow-up |
|||
|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | ||
| HIV knowledge (0–1) | SPT | 0.75 | 0.01 | 0.80 | 0.03 | 0.82 | 0.04 |
| CTL | 0.72 | 0.02 | 0.78 | 0.04 | 0.75 | 0.03 | |
| STD knowledge (0–1) | SPT | 0.64 | 0.02 | 0.75a | 0.04 | 0.72a | 0.04 |
| CTL | 0.61 | 0.03 | 0.66 | 0.04 | 0.71 | 0.05 | |
| Behavior intention (1–4) | SPT | 2.97 | 0.04 | 3.01 | 0.06 | 2.94 | 0.08 |
| CTL | 3.05 | 0.04 | 2.97 | 0.07 | 3.00 | 0.10 | |
| Condom attitude (1–6) | SPT | 4.48 | 0.05 | 4.46 | 0.13 | 4.37 | 0.17 |
| CTL | 4.37 | 0.05 | 4.35 | 0.18 | 4.29 | 0.18 | |
| Self-efficacy steady partner (0–10) | SPT | 6.32 | 0.19 | 6.92 | 0.40 | 7.20 | 0.58 |
| CTL | 6.32 | 0.16 | 7.20a | 0.40 | 5.98 | 0.61 | |
| Self-efficacy new partner (0–10) | SPT | 7.37 | 0.18 | 8.59a | 0.30 | 9.20a | 0.38 |
| CTL | 7.83 | 0.16 | 8.30 | 0.36 | 8.25 | 0.39 | |
| Self-efficacy all partners (0–10) | SPT | 6.87 | 0.18 | 7.75a | 0.31 | 8.21a | 0.40 |
| CTL | 7.10 | 0.14 | 7.76 | 0.32 | 6.92 | 0.52 | |
| Condom influence (1–5) | SPT | 1.94 | 0.10 | 2.80a,c | 0.26 | 2.14b | 0.24 |
| CTL | 1.88 | 0.10 | 1.71c | 0.20 | 1.79 | 0.23 | |
| Depression (0–9) | SPT | 4.24 | 0.33 | 3.93 | 0.60 | 3.62 | 0.66 |
| CTL | 3.91 | 0.31 | 2.55a | 0.53 | 2.67 | 0.55 | |
| Self esteem (0–40) | SPT | 17.02 | 0.26 | 19.37a | 1.17 | 19.54a | 1.20 |
| CTL | 16.93 | 0.37 | 17.68 | 0.83 | 16.70 | 0.94 | |
| Generalized anxiety (0–21) | SPT | 12.16 | 0.46 | 8.69a | 1.18 | 7.09a | 1.48 |
| CTL | 12.61 | 0.60 | 9.94a | 1.07 | 10.13 | 1.10 | |
| PTSD symptoms (0–51) | SPT | 25.13 | 0.50 | 19.77a | 2.63 | 21.01 | 3.23 |
| CTL | 25.08 | 0.71 | 22.02 | 2.43 | 23.38 | 2.85 | |
SPT SUPPORT intervention group, CTL control group, HIV human immunodeficiency virus, STD sexually transmitted disease, PTSD post-traumatic stress disorder
Significant within-group change between baseline and post-intervention or baseline and 3-month assessment
Significant within-group change between post-intervention and 3-month assessment
Significant difference between intervention and control groups
Feasibility: Intervention Attendance, Participation, and Retention
Of the 27 women assigned to the SUPPORT intervention, 23 (85 %) enrolled in the intervention and 12 (44 %) completed five or more sessions; of the 28 participants assigned to the control group, 21 (75 %) enrolled in the intervention and 12 (43 %) completed five or more sessions. Participants assigned to the SUPPORT intervention and control group attended an average of 3.7 (SD 2.83) and 3.6 (SD 2.88) sessions respectively.
To assess the feasibility of conducting a research study, we also examined attendance at the follow-up assessment. Overall, 43 (78 %) of the 55 randomized women completed at least one of the two follow-up assessments. We tested for differences between women who completed at least one follow-up assessment and those who did not complete any. Women who did not complete any follow-up assessments reported less positive perceptions of their partner's attitudes towards condoms ((2.72 vs. 3.52), t(−2.28), p = 0.02), compared to women who completed at least one follow-up assessment.
Safety: IPV and Sexual Relationship Power
Table 2 provides the summary statistics for safety data (i.e., battering, IPV, sexual relationship power, and violence at last sex) by condition at each of the three assessment occasions.
Both the SUPPORT and control group participants experienced significant reductions in self-reported experiences of battering at post-intervention (change in μs = −10.40 and −7.62, p = 0.01 and 0.02, respectively) and 3-month follow-ups (change in μs = −15.13 and −7.16, p = 0.00 and 0.02, respectively) compared to their baseline scores. SUPPORT participants also reported a significant reduction in experiences of IPV, as measured by their total ABI score, between baseline and post-intervention (change in μ = −25.87, p = 0.01). Additionally, they reported significant reductions in experiences of IPV at their last sexual experience at the 3-month follow-up compared to their post-intervention and baseline scores (change in μs = −0.22 [not in table] and −0.40, p = 0.04 and 0.02).
When considering the impact of the clinical trial on specific types of violence, SUPPORT participants reported significant reductions in episodes of physical violence at post-intervention (change in μ = −8.07, p = 0.01) and 3-month follow-ups (change in μ = −6.07, p = 0.03) compared to their baseline scores. SUPPORT participants experienced significant reductions in psychological violence at post-intervention (change in μ = −15.56, p = 0.00) and 3-month follow-ups (change in μ = −15.00, p = 0.00) compared to their baseline scores. Additionally, they reported significantly fewer experiences of psychological violence at post-intervention (difference in μs = −11.29 [not in table], p = 0.05) compared to the control group. Both the SUPPORT and control group participants showed significant reductions in sexual violence at 3-month follow-up (change in μs = −2.30 and −1.61, p = 0.05 and 0.00, respectively) compared to their baseline scores.
SUPPORT participants reported significant improvements in their experience of sexual relationship power at post-intervention (change in μ = 0.58, p = 0.04) and 3-month follow-ups (change in μ = 0.69, p = 0.00) compared to their baseline scores. They also showed significantly higher levels of sexual relationship power (μ = 0.70, p = 0.01) and greater rates of increase in this power (β = 0.75, p = 0.01) compared to the control group at the 3-month follow-up (not reported in table).
Efficacy
Table 4 provides rate ratios (RR) and 95 % confidence intervals (CI) for primary outcomes (i.e., sexual risk and communication behaviors) by treatment condition at post-intervention and 3-month follow-up assessment, with baseline as the reference group. Table 5 presents summary statistics for the secondary outcomes (i.e., sexual risk antecedents and psychological outcomes) by treatment condition at each of the three assessment occasions.
Table 4.
Rate ratios (RR) and 95 % confidence intervals (CI) for count outcomes
| Variable | Post-intervention |
3-month follow-up |
||||
|---|---|---|---|---|---|---|
| RR | 95 % CI | p | RR | 95 % CI | p | |
| Episodes unprotected sex, all partners | ||||||
| Within group changesa | ||||||
| SPT | 0.55 | 0.31, 0.95 | 0.03 | 0.75 | 0.34, 1.62 | 0.46 |
| CTL | 1.32 | 0.75, 2.30 | 0.33 | 1.66 | 0.83, 3.29 | 0.15 |
| Between group changesb | ||||||
| SPT | 0.68 | 0.34, 1.35 | 0.28 | 0.74 | 0.34, 1.62 | 0.45 |
| Change in rate of changeb | ||||||
| SPT | 0.41 | 0.20, 0.88 | 0.02 | 0.45 | 0.17, 1.18 | 0.10 |
| Episodes unprotected sex, steady partner | ||||||
| Within group changesa | ||||||
| SPT | 0.61 | 0.35, 1.06 | 0.08 | 0.76 | 0.40, 1.46 | 0.41 |
| CTL | 1.36 | 0.72, 2.55 | 0.34 | 1.11 | 0.61, 2.01 | 0.74 |
| Between group changesb | ||||||
| SPT | 0.71 | 0.38, 1.35 | 0.30 | 1.09 | 0.57, 2.11 | 0.79 |
| Change in rate of changeb | ||||||
| SPT | 0.45 | 0.20, 0.98 | 0.05 | 0.69 | 0.30, 1.60 | 0.39 |
| Episodes unprotected sex, other partners | ||||||
| Within group changesa | ||||||
| SPT | 0.22 | 0.09, 0.54 | 0.00 | 3.40 | 0.82, 14.15 | 0.09 |
| CTL | 0.99 | 0.43, 2.26 | 0.98 | 2.80 | 0.88, 8.90 | 0.08 |
| Between group changesb | ||||||
| SPT | 0.05 | 0.01, 0.28 | 0.00 | 0.30 | 0.04, 2.23 | 0.24 |
| Change in rate of changeb | ||||||
| SPT | 0.22 | 0.06, 0.74 | 0.01 | 1.21 | 0.19, 7.81 | 0.84 |
| Communications about safe sex, steady partner | ||||||
| Within group changesa | ||||||
| SPT | 1.58 | 0.89, 2.84 | 0.12 | 0.86 | 0.60, 1.23 | 0.41 |
| CTL | 1.70 | 0.51, 5.67 | 0.39 | 0.48 | 0.22, 1.05 | 0.07 |
| Between group changesb | ||||||
| SPT | 2.27 | 0.78, 6.61 | 0.13 | 4.40 | 1.78, 10.83 | 0.00 |
| Change in rate of changeb | ||||||
| SPT | 0.93 | 0.25, 3.52 | 0.92 | 1.80 | 0.76, 4.30 | 0.18 |
| Communications about safe sex, other partners | ||||||
| Within group changesa | ||||||
| SPT | 2.19 | 1.28, 3.74 | 0.00 | 2.01 | 0.59, 6.91 | 0.27 |
| CTL | 0.46 | 0.25, 0.86 | 0.02 | 2.95 | 1.35, 6.46 | 0.01 |
| Between group changesb | ||||||
| SPT | 6.31 | 1.98, 20.08 | 0.00 | 0.91 | 0.20, 4.12 | 0.90 |
| Change in rate of changeb | ||||||
| SPT | 4.73 | 2.04, 10.95 | 0.00 | 0.68 | 0.16, 2.92 | 0.61 |
SPT SUPPORT intervention group, CTL control group
Reference group: baseline
Reference group: control
Sexual Risk and Protective Behaviors
Intent-to-treat analyses documented SUPPORT intervention participants’ significant decrease in frequency of unprotected sex across all sexual partners (RR 0.55; 95 % CI 0.31, 0.95; p = 0.03) and with other partners (RR 0.22; 95 % CI 0.09, 0.54; p = 0.00) at post-intervention compared to baseline. Their frequency of unprotected sex with other partners was significantly lower than control group participants at post-intervention (RR 0.05; 95 % CI 0.01, 0.28; p = 0.00). Further, compared to the control group, SUPPORT participants experienced a stronger decrease in the frequency of unprotected sex with steady partner (RR 0.45; 95 % CI 0.20, 0.98; p = 0.05), other partners (RR 0.22; 95 % CI 0.06, 0.74; p = 0.01), and across all partners (RR 0.41; 95 % CI 0.20, 0.88; p = 0.02) from baseline to post-intervention.
SUPPORT participants showed significant improvements in their communications about practicing safer sex with steady and other sexual partners. Compared to the control group, SUPPORT participants reported higher number of conversations about safer sex with their steady partner at the 3-month follow-up (RR 4.40; 95 % CI 1.78, 10.83; p = 0.00). They also significantly increased communications about safer sex with their other sexual partners between baseline and post-intervention (RR 2.19; 95 % CI 1.28, 3.74; p = 0.00) and their frequency of safer sex communications with these partners was significantly higher than that of control participants at post-intervention follow-up (RR 6.31; 95 % CI 1.98, 20.08; p = 0.00). Further, the rate of increase in the frequency of safer sex communications was stronger among SUPPORT participants compared to the control group at post-intervention (RR 4.73; 95 % CI 2.04, 10.95; p = 0.00).
Although the control group participants had a significant decline in the frequency of safer sex communications with their other sexual partners post-intervention (RR 0.46; 95 % CI 0.25, 0.86; p = 0.02), they showed a significant increase in these communications between baseline and the 3-month follow-up (RR 2.95; 95 % CI 1.35, 6.46; p = 0.01).
Theoretical Antecedents of Sexual Risk Behavior
Among three of the six hypothesized antecedents of HIV-risk behavior, significant results were found among SUPPORT participants (see Table 5). Women in the SUPPORT intervention showed a significant increase in STD-related knowledge (change in μ = 0.11, p = 0.02) and in self-efficacy with new partners at post-intervention (change in μ = 1.22, p = 0.00) compared to their baseline scores. Additionally, the rate of increase in self-efficacy with new partners for SUPPORT participants was significantly higher than that of control participants at the 3-month follow-up (β = 1.41; p = 0.03 [not reported in table]).
SUPPORT participants reported an increase in self-efficacy with all sexual partners at post-intervention (change in μ = 0.88, p = 0.02). SUPPORT participants also reported a significantly higher rate of increase in self-efficacy with all partners at the 3-month follow-up compared to the control group (β = 1.51, p = 0.03 [not reported in table]).
Lastly, SUPPORT participants significantly increased their condom influence skills between baseline and post-intervention (change in μ = 0.86, p = 0.00) and had statistically higher condom influence skills at post-intervention follow-up compared to the control group (change in μ = 1.09, p = 0.00 [difference not reported in table]). They also reported a statistically stronger rate of increase in condom influence skills at post-intervention compared to the control group (β = 1.03, p = 0.00 [not reported in table]). However, these gains were not sustained as the SUPPORT participants reported a significant drop in their condom influence skills at 3-month follow-up compared to post-intervention (change in μ = −0.66, p = 0.01).
The control group participants showed a significant increase in self-efficacy with their steady partner between baseline and post-intervention (change in μ = 0.88, p = 0.04). No significant effects were found for HIV-related knowledge and motivation measures.
Psychological Outcomes
The control group participants experienced a significant reduction in their depression symptoms at post-intervention (change in μ = −1.36, p = 0.04) compared to their baseline scores.
SUPPORT participants made significant gains in self-esteem. They showed an increase in self-esteem at post-intervention (change in μ = 2.35, p = 0.05) and 3-month follow-ups (change in μ = 2.52, p = 0.03) compared to their baseline scores.
Both the SUPPORT and control group participants experienced significant reductions in their self-reported levels of anxiety at post-intervention (change in μs = −3.47 and −2.67, p = 0.00 and 0.05, respectively) compared to baseline scores. SUPPORT participants’ reductions in anxiety levels were maintained at the 3-month follow-up (change in μ = −5.07, p = 0.00).
The SUPPORT participants reported significantly fewer symptoms of PTSD at post-intervention follow-up compared to their baseline measure (change in μ = −5.36, p = 0.03).
Discussion
This pilot trial indicates that engaging recently abused women at risk for HIV in an integrated HIV-IPV intervention is feasible and acceptable to low-income, community-based women. Preliminary evidence suggests the SUPPORT intervention was safe in that IPV episodes were actually reduced relative to a control condition. Also important, the intervention had a significant effect on the primary sexual risk and protective outcomes (i.e., condom use, communications about safer sex). Positive changes were also observed in secondary outcomes including condom use self-efficacy and condom influence skills as well as some mental health outcomes.
Among their gains, SUPPORT participants decreased their frequency of unprotected sex across all partners and increased their communications about safer sex with steady and other sexual partners. Compared to the control group, SUPPORT participants reported four times the number of safer sex conversations with their steady partner at the 3-month follow-up and six times the number of safer communications with other sexual partners at post-intervention follow-up. Participants of both the SUPPORT intervention and control groups reported a reduction in experiences of battering. The reduction among SUPPORT participants was more pronounced when compared to the control group. Further, SUPPORT participants experienced significant declines in their experiences of physical, emotional, and sexual IPV. While significant reductions in physical and emotional IPV were documented at post intervention assessments and were sustained at 3-month follow-up, significant reductions in sexual violence and violence at last sex were not reported until the 3-month follow-up. It is possible that the women had to first experience changes in physical and emotional violence before acting on their experience of sexual violence in their relationship.
SUPPORT participants demonstrated improvements in several hypothesized antecedents of risk behavior, including STD knowledge, self-efficacy, and condom influence skills, but no change was observed in HIV knowledge or the construct of motivation to practice safer sex. The lack of significant improvement in HIV knowledge can be attributed to the fact that both the SUPPORT intervention and control group had high levels of HIV knowledge at baseline. This is a positive sign because it is critical that women who experience IPV be exposed to HIV-related information. Earlier research [16] has demonstrated that motivation is associated with condom use among women with no history of IPV but not among women with a history of IPV. These results suggest that future research ought to examine the impact of partner motivation on condom use among abused women.
SUPPORT participants experienced significant improvements in their self-esteem, anxiety, and PTSD symptoms, with some gains extending to the 3-month assessment. However, there were no changes in their depression symptoms. The control group participants reported fewer depressive symptoms at the post-intervention follow-up but not at the 3-month follow-up. While improving depressive symptoms was not a primary focus of the SUPPORT intervention, it was surprising that the intervention had an impact on other mental health outcomes and not depression. It is possible that the supportive counseling format of the control group is more conducive for improvements in depression symptoms rather than a structured intervention focused on IPV and sexual risk reduction.
Although preliminary evidence indicates the SUPPORT intervention had short-term effects on the primary outcomes, several effects were not maintained at the 3-month follow-up. Given the complex issues with which this study was dealing and the important role that IPV plays in acquisition of HIV among women, it will be important in fully-powered replication trials to reinforce the intervention components through booster sessions. Booster sessions have been used successfully to sustain behavior changes among IV-drug users at high risk for HIV [64, 65]. In addition, given that both violence and HIV are relational issues, future research ought to examine the efficacy and effectiveness of integrated HIV-IPV couple-based interventions.
One of the challenges experienced in the implementation of the trial was that only half of the participants assigned to either the intervention (44 %) or control group (43 %) attended five or more sessions. Further, participants attended an average of four sessions irrespective of group assignment. In order to reduce barriers to sustained treatment among moderately to severely traumatized women, the intervention retention pattern needs to be examined further. One of the strengths of this study is that we were able to successfully recruit women with lifetime and very recent experiences of trauma and IPV in particular. However, we did not assess their level of psychological distress at the time of inclusion in the study. Assessing current mental health status might be important for future implementation studies, as mental health could impact both engagement and retention in treatment.
This study was limited by a small sample size, reliance on self-report, and short follow-ups. Also, the two interventions differed in two important ways: length of sessions and treatment modality. The intervention groups met for 2–2.5 h weekly for 8 weeks and consisted of a mix of three individual and five group sessions whereas the control groups met for 1–1.5 h weekly for eight group sessions. These differences may partially account for the effects of the SUPPORT intervention versus the control treatment on sexual behavior and IPV outcomes.
Conclusion
There are few evidence-based interventions that integrate risk reduction for both IPV and HIV. This study makes an important contribution to the literature on HIV prevention among women who have experienced IPV. It offers preliminary evidence that the SUPPORT intervention, a theory-based, integrated IPV-HIV intervention, can reduce episodes of unprotected sex and promote sexual communication, while reducing experiences of IPV among women with recent experiences of IPV and at risk for HIV infection. Corroboration of these findings using a fully-powered randomized controlled trial with longer follow-ups is needed.
Acknowledgments
This work was supported by the National Institutes of Mental Health (K01MH080660). We would like to thank all the women who participated in this research and the project SUPPORT team members. We would also like to thank all the non-governmental organizations that partnered with us on this project.
References
- 1.CDC. HIV surveillance report, 2011. 2013:23. [Google Scholar]
- 2.Maman S, Campbell J, Sweat MD, Gielen AC. The intersections of HIV and violence: directions for future research and interventions. Soc Sci Med. 2000;50(4):459–78. doi: 10.1016/s0277-9536(99)00270-1. [DOI] [PubMed] [Google Scholar]
- 3.Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O'Campo P. HIV/AIDS and intimate partner violence: intersecting women's health issues in the United States. Trauma Violence Abuse. 2007;8(2):178–98. doi: 10.1177/1524838007301476. [DOI] [PubMed] [Google Scholar]
- 4.Pantalone DW, Rood BA, Morris BW, Simoni JM. A systematic review of the frequency and correlates of partner abuse in HIV-infected women and men who partner with men. J Assoc Nurses AIDS Care. 2014;25(1 Suppl):S15–35. doi: 10.1016/j.jana.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phillips DY, Walsh B, Bullion JW, Reid PV, Bacon K, Okoro N. The intersection of intimate partner violence and HIV in U.S. women: a review. J Assoc Nurses AIDS Care. 2014;25(1 Suppl):S36–49. doi: 10.1016/j.jana.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Durevall D, Lindskog A. Intimate partner violence and HIV in ten sub-Saharan African countries: what do the Demographic and Health Surveys tell us? Lancet Glob Health. 2015;3(1):e34–43. doi: 10.1016/S2214-109X(14)70343-2. [DOI] [PubMed] [Google Scholar]
- 7.Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, Ehiri JE. Intimate partner violence and HIV infection among women: a systematic review and meta-analysis. J Int AIDS Soc. 2014;17:18845. doi: 10.7448/IAS.17.1.18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siemieniuk RA, Krentz HB, Gill MJ. Intimate partner violence and HIV: a review. Curr HIV/AIDS Rep. 2013;10(4):380–9. doi: 10.1007/s11904-013-0173-9. [DOI] [PubMed] [Google Scholar]
- 9.Kouyoumdjian FG, Calzavara LM, Bondy SJ, O'Campo P, Serwadda D, Nalugoda F, et al. Risk factors for intimate partner violence in women in the Rakai Community Cohort Study, Uganda, from 2000 to 2009. BMC Public Health. 2013;13:566. doi: 10.1186/1471-2458-13-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–8. doi: 10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- 11.Decker MR, Miller E, McCauley HL, Tancredi DJ, Anderson H, Levenson RR, et al. Recent partner violence and sexual and drug-related STI/HIV risk among adolescent and young adult women attending family planning clinics. Sex Transm Infect. 2014;90(2):145–9. doi: 10.1136/sextrans-2013-051288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frye V, Ompad D, Chan C, Koblin B, Galea S, Vlahov D. Intimate partner violence perpetration and condom use-related factors: associations with heterosexual men's consistent condom use. AIDS Behav. 2011;15(1):153–62. doi: 10.1007/s10461-009-9659-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hamburger ME, Moore J, Koenig LJ, Vlahov D, Schoenbaum EE, Schuman P, et al. Persistence of inconsistent condom use: relation to abuse history and HIV serostatus. AIDS Behav. 2004;8(3):333–44. doi: 10.1023/B:AIBE.0000044080.04397.97. [DOI] [PubMed] [Google Scholar]
- 14.Teitelman AM, Ratcliffe SJ, Morales-Aleman MM, Sullivan CM. Sexual relationship power, intimate partner violence, and condom use among minority urban girls. J Interpers Violence. 2008;23(12):1694–712. doi: 10.1177/0886260508314331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El-Bassel N, Gilbert L, Wu E, Go H, Hill J. HIV and intimate partner violence among methadone-maintained women in New York City. Soc Sci Med. 2005;61(1):171–83. doi: 10.1016/j.socscimed.2004.11.035. [DOI] [PubMed] [Google Scholar]
- 16.Mittal M, Senn TE, Carey MP. Fear of violent consequences and condom use among women attending an STD clinic. Women Health. 2013;53(8):795–807. doi: 10.1080/03630242.2013.847890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swan H, O'Connell DJ. The impact of intimate partner violence on women's condom negotiation efficacy. J Interpers Violence. 2012;27(4):775–92. doi: 10.1177/0886260511423240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collins RL, Ellickson PL, Orlando M, Klein DJ. Isolating the nexus of substance use, violence and sexual risk for HIV infection among young adults in the United States. AIDS Behav. 2005;9(1):73–87. doi: 10.1007/s10461-005-1683-2. [DOI] [PubMed] [Google Scholar]
- 19.Cavanaugh CE, Hansen NB, Sullivan TP. HIV sexual risk behavior among low-income women experiencing intimate partner violence: the role of posttraumatic stress disorder. AIDS Behav. 2010;14(2):318–27. doi: 10.1007/s10461-009-9623-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sormanti M, Wu E, El-Bassel N. Considering HIV risk and intimate partner violence among older women of color: a descriptive analysis. Women Health. 2004;39(1):45–63. doi: 10.1300/J013v39n01_03. [DOI] [PubMed] [Google Scholar]
- 21.Wu E, El-Bassel N, Witte SS, Gilbert L, Chang M. Intimate partner violence and HIV risk among urban minority women in primary health care settings. AIDS Behav. 2003;7(3):291–301. doi: 10.1023/a:1025447820399. [DOI] [PubMed] [Google Scholar]
- 22.Raj A, Clarke JG, Silverman JG, Rose J, Rosengard C, Hebert M, et al. Violence against women associated with arrests for sex trade but not drug charges. Int J Law Psychiatry. 2006;29(3):204–11. doi: 10.1016/j.ijlp.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 23.El-Bassel N, Gilbert L, Golder S, Wu E, Chang M, Fontdevila J, et al. Deconstructing the relationship between intimate partner violence and sexual HIV risk among drug-involved men and their female partners. AIDS Behav. 2004;8(4):429–39. doi: 10.1007/s10461-004-7327-0. [DOI] [PubMed] [Google Scholar]
- 24.Kapadia F, Latka MH, Hudson SM, Golub ET, Campbell JV, Bailey S, et al. Correlates of consistent condom use with main partners by partnership patterns among young adult male injection drug users from five US cities. Drug Alcohol Depend. 2007;91(Suppl 1):S56–63. doi: 10.1016/j.drugalcdep.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 25.Bonomi AE, Anderson ML, Reid RJ, Rivara FP, Carrell D, Thompson RS. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med. 2009;169(18):1692–7. doi: 10.1001/archinternmed.2009.292. [DOI] [PubMed] [Google Scholar]
- 26.Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23(4):260–8. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- 27.Devries KM, Mak JY, Bacchus LJ, Child JC, Falder G, Petzold M, et al. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med. 2013;10(5):e1001439. doi: 10.1371/journal.pmed.1001439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ludermir AB, Schraiber LB, D'Oliveira AF, França-Junior I, Jansen HA. Violence against women by their intimate partner and common mental disorders. Soc Sci Med. 2008;66(4):1008–18. doi: 10.1016/j.socscimed.2007.10.021. [DOI] [PubMed] [Google Scholar]
- 29.Campbell J, Jones AS, Dienemann J, Kub J, Schollenberger J, O'Campo P, et al. Intimate partner violence and physical health consequences. Arch Intern Med. 2002;162(10):1157–63. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- 30.Coker AL. Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse. 2007;8(2):149–77. doi: 10.1177/1524838007301162. [DOI] [PubMed] [Google Scholar]
- 31.Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C. Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: an observational study. Lancet. 2008;371(9619):1165–72. doi: 10.1016/S0140-6736(08)60522-X. [DOI] [PubMed] [Google Scholar]
- 32.WHO. HIV/AIDS and mental health. World Health Organization; 2008. pp. 1–5. [Google Scholar]
- 33.Abramsky T, Devries K, Kiss L, Nakuti J, Kyegombe N, Star-mann E, et al. Findings from the SASA! Study: a cluster randomized controlled trial to assess the impact of a community mobilization intervention to prevent violence against women and reduce HIV risk in Kampala, Uganda. BMC Med. 2014;12:122. doi: 10.1186/s12916-014-0122-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Puren A, et al. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ. 2008;337:a506. doi: 10.1136/bmj.a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnson JE, Peabody ME, Wechsberg WM, Rosen RK, Fernandes K, Zlotnick C. Feasibility of an HIV/STI risk-reduction program for incarcerated women who have experienced interpersonal violence. J Interpers Violence. 2015;30:3244–66. doi: 10.1177/0886260514555013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pronyk PM, Hargreaves JR, Kim JC, Morison LA, Phetla G, Watts C, et al. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006;368(9551):1973–83. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- 37.Wagman JA, Gray RH, Campbell JC, Thoma M, Ndyanabo A, Ssekasanvu J, et al. Effectiveness of an integrated intimate partner violence and HIV prevention intervention in Rakai, Uganda: analysis of an intervention in an existing cluster randomised cohort. Lancet Glob Health. 2015;3(1):e23–33. doi: 10.1016/S2214-109X(14)70344-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weir BW, O'Brien K, Bard RS, Casciato CJ, Maher JE, Dent CW, et al. Reducing HIV and partner violence risk among women with criminal justice system involvement: a randomized controlled trial of two motivational interviewing-based interventions. AIDS Behav. 2009;13(3):509–22. doi: 10.1007/s10461-008-9422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carey MP, Carey KB, Maisto SA, Gordon CM, Weinhardt LS. Assessing sexual risk behaviour with the timeline followback (TLFB) approach: continued development and psychometric evaluation with psychiatric outpatients. Int J STD AIDS. 2001;12:365–75. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schroder KEE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Ann Behav Med. 2003;26:104–23. doi: 10.1207/s15324796abm2602_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weinhardt LS, Forsyth AD, Carey MP, Jaworski BC, Durant LE. Reliability and validity of self-report measures of HIV-related sexual behavior: progress since 1990 and recommendations for research and practice. Arch Sex Behav. 1998;27:155–80. doi: 10.1023/a:1018682530519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bandura A. Social foundations of thought and action: a social-cognitive view. Prentice-Hall; Englewood Cliffs: 1986. [Google Scholar]
- 43.Fishbein M. The role of theory in HIV prevention. AIDS Care. 2000;12(3):273–8. doi: 10.1080/09540120050042918. [DOI] [PubMed] [Google Scholar]
- 44.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–74. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 45.Connell RW. Gender and power: society, the person, and sexual politics. Stanford University Press; Stanford: 1987. [Google Scholar]
- 46.Landau-Stanton J. Competence, impermanence, and transitional mapping: a model for systems consultation. In: Wynne LC, McDaniel S, Weber T, editors. Systems consultations: a new perspective for family therapy. Guilford Press; New York: 1986. pp. 253–69. [Google Scholar]
- 47.Smith PH, Smith JB, Earp JL. Beyond the measurement trap: a reconstructed conceptualization and measurement of woman battering. Psychol Women Q. 1999;23:177–93. [Google Scholar]
- 48.Zink T, Klesges LM, Levin L, Putnam F. Abuse behavior inventory: cutpoint, validity, and characterization of discrepancies. J Interpers Violence. 2007;22(7):921–31. doi: 10.1177/0886260507301228. [DOI] [PubMed] [Google Scholar]
- 49.Pulerwitz J, Gortmaker SL, DeJong W. Measuring sexual relationship power in HIV/STD research. Sex Roles. 2000;42(7–8):637–60. [Google Scholar]
- 50.Carey MP, Kalichman SC, Forsyth AD, Wright EM, Johnson BT. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. J Consult Clin Psychol. 1997;65(4):531–41. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carey MP, Braaten LS, Maisto SA, Gleason JR, Forsyth AD, Durant LE, et al. Using information, motivational enhancement, and skills training to reduce the risk of HIV infection for low-income urban women: a second randomized clinical trial. Health Psychol. 2000;19:3–11. doi: 10.1037//0278-6133.19.1.3. [DOI] [PubMed] [Google Scholar]
- 52.Carey MP, Senn TE, Vanable PA, Coury-Doniger P, Urban MA. Brief and intensive interventions to promote sexual risk reduction among STD clinic patients: results from a randomized controlled trial. AIDS Behav. 2010;14:504–17. doi: 10.1007/s10461-009-9587-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Carey MP, Senn TE, Walsh JL, Coury-Doniger P, Urban MA, Fortune T, et al. Evaluating a brief, video-based sexual risk reduction intervention and assessment reactivity with STI clinic patients: results from a randomized controlled trial. AIDS Behav. 2015;19:1228–46. doi: 10.1007/s10461-014-0960-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV Knowledge Questionnaire. AIDS Educ Prev. 2002;14(2):172–82. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jaworski BC, Carey MP. Effects of a brief, theory-based STD prevention program for female college students. J Adolesc Health. 2001;29(6):417–25. doi: 10.1016/s1054-139x(01)00271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brown IS. Development of a scale to measure attitude toward the condom as a method on birth control. J Sex Res. 1984;20(3):255–63. [Google Scholar]
- 57.Sacco WP, Levine B, Reed DL, Thompson K. Attitudes about condom use as an AIDS-relevant behavior: their factor structure and relation to condom use. Psychol Assess. 1991;3(2):265–72. [Google Scholar]
- 58.Murphy DA, Stein JA, Schlenger W, Mailbach E. Conceptualizing the multidimensional nature of self-efficacy: assessment of situational context and level of behavioral challenges to maintain safer sex. Health Psychol. 2001;20(4):281–90. [PubMed] [Google Scholar]
- 59.Noar SM, Morokoff PJ, Harlow LL. Condom influence strategies in a community sample of ethnically diverse men and women. J Appl Soc Psychol. 2004;34(8):1730–51. [Google Scholar]
- 60.Santor DA, Coyne JC. Shortening the CES-D to improve its ability to detect cases of depression. Psychol Assess. 1997;9(3):233–43. [Google Scholar]
- 61.Rosenberg M. Society and the adolescent self-image. Princeton University Press; Princeton: 1965. [Google Scholar]
- 62.Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 63.Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress. 1993;6(4):459–73. [Google Scholar]
- 64.Go VF, Frangakis C, Le Minh N, Latkin CA, Ha TV, Mo TT, et al. Effects of an HIV peer prevention intervention on sexual and injecting risk behaviors among injecting drug users and their risk partners in Thai Nguyen, Vietnam: a randomized controlled trial. Soc Sci Med. 2013;96:154–64. doi: 10.1016/j.socscimed.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jain B, Krishnan S, Ramesh S, Sabarwal S, Garg V, Dhingra N. Effect of peer-led outreach activities on injecting risk behavior among male drug users in Haryana, India. Harm Reduct J. 2014;11(3):1–6. doi: 10.1186/1477-7517-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]