Abstract
Background
There have been few studies on economic evaluation of acne treatments. Chemical peel (CP), a treatment approach primarily aimed at removing acne hyperpigmentation and scarring, is gradually accepted in the Chinese market.
Objectives
This study aimed to detect willingness-to-pay (WTP) and to conduct a benefit–cost analysis for CP treatment among Chinese acne patients.
Materials and methods
The costs were obtained from the patient’s perspective and compared with benefits. The net benefits were approximated by WTP, using the contingent valuation method. A glycolic acid peel served as the demonstrated example. WTP and related information were inquired via an online questionnaire among the Chinese population. Factors for WTP were identified using generalized linear models. The benefit–cost ratio (BCR) was calculated. Discounting was not considered for both WTP and costs.
Results
The response rate of the survey was 95.4% among the 476 anonymous participants. The average cost for three-time CP treatment was USD 383.4. Statistically significant differences in WTP among the cases were identified. The mean WTP for Case 1, Case 2, and Case 3 was USD 234.6, 222.0, and 401.7, respectively. A statistically significant association between WTP and self-reported acne severity was observed for all cases after adjustments for demographic characteristics (P<0.01). The Cardiff Acne Disability Index was positively associated with WTP. The BCRs were 0.61, 0.58, and 1.4 for Case 1, Case 2, and Case 3, respectively.
Conclusion
Patients with acne in China are willing to pay for acne treatment. Although the benefits of CP treatment have not generally outweighed their aggregated costs, WTP for CP treatment was positively associated with self-reported acne severity and desirable efficacy of treatment. Individualized acne treatments are recommended to target a specific population in the Chinese market.
Keywords: acne vulgaris, benefit–cost analysis, chemical peel, willingness-to-pay
Introduction
Acne vulgaris, comprised of comedones, papules, pustules, and nodules mainly appearing on the face, is one of the most common skin disorders across age, genders, races, and skin types.1 The reported prevalence of acne ranges from 35% to above 90% worldwide.2,3 In China, the prevalence of acne among adolescents is 51.3% (52.7% in males, 49.6% in females) in the North East,4 and the prevalence of moderate-to-severe acne vulgaris among first-year college students is 10.2%.5,6 A study in Hong Kong in 1999 indicated that 81.5% of participants reported an acne history and 52.6% had post-acne scarring.7 Besides, postinflammatory hyperpigmentation (PIH) is more likely to affect people with darker skin compared to Caucasians owing to differences in genetic background, exerting a more severe diseases burden among Chinese patients with acne.8,9
With the rapid economic growth and concomitant changes of lifestyle in China, the demand for facial beauty has been surprisingly increased.10 In the general esthetic pursuit of fairer skin in East Asia,11 Chinese people increasingly pay attention to post-acne outcomes such as scars and PIH, in addition to the disease per se. Hence, the management of acne should not only include traditional anti-inflammatory and keratinization-moderated drugs but also integrate cosmetic therapy for post-acne sequelae.12
Chemical peel (CP), an adjunctive treatment for acne management, has mushroomed in treating acne blemishes and removing acne scars for the last three decades.13,14 CP not only can help speed up the resolution of acne, to the renewal of the skin surface, but can also exert anti-inflammatory effects on acne. CPs are classified into superficial, medium, and deep CP according to the concentration of acid and the depth of skin injury. Light-to-medium depth peels, such as glycolic acid (GA), are more popularized due to their significant benefits for mild-to-moderate acne scars and PIH with rare side effects.15–17 However, the application of CP should be more cautious among Asians because of the natural differences between the skin type of Asians and white people.14,18 Hence, CPs can only be legally administered in qualified clinics under the supervision of certificated dermatologists in China. This new adjunctive treatment has been gradually promoted in treating various acne indications. It was reported that improved clinical outcomes were expected after an average 3–4 times of use for superficial-to-medium CPs.17 However, the costs for facial CPs varied by countries and regions, and there were no pricing suggestions for CP in the Chinese market. Major hospitals in China set up the price individually, ranging from 100 to 200 USD per treatment.
The common approach to detecting patients’ preferences and to understanding whether patient’s preferences outweigh costs is to inquire about willingness-to-pay (WTP) for certain diseases and to perform benefit–cost analysis (BCA) for a specific treatment.19,20 WTP, a preference-based monetary tool to measure the disease burden and to explore people’s attitudes to specific attributes of an illness, can serve as a proxy of the gained benefits.20 Although WTP is not a utility, it can reflect the quality of life (QoL) in monetary value.
The current study aimed to detect WTP and to conduct BCA for a typical superficial-to-medium CP treatment (ie, GA) among Chinese acne patients.
Materials and methods
Study design and participants
Chinese adults aged above 18 years with a self-reported diagnosis of acne were invited to participate in the study via “WeChat,” the most popular mobile chatting application in China. Anonymous online questionnaires were distributed and were completed by patients voluntarily. Informed consents were obtained from all participants beforehand. The institutional research ethics board of Xiangya Hospital, Central South University, Changsha, China approved the study protocol before implementation.
Benefits: WTP
WTP approximated benefits in our study via the contingent valuation method.21 This approach is widely acknowledged as a theoretically acceptable method for the valuation of goods and services by potential consumers. The participants received education about the process and adverse effects of CPs, specified in GA treatment. Therefore, the respondents had adequate knowledge about the studied treatment. Three typical cases demonstrating typical and average effects of three-time use of GA treatment in Chinese patients (Figure S1) were presented to the participants. WTP is elicited by the same standardized question: “How much would you be willing to pay today for one new treatment with minor side effects to achieve the effects as shown in contrast figure? (This new treatment requires three-time visits and cost two hours per time.)” The options of WTP consisted of seven discrete amounts of monetary value as follows: Chinese yuan (CNY) 50, 100, 250, 500, 1,000, 2,500, and 5,000.
Aggregated costs
We estimated costs from the patient perspective. Direct medical costs (physician visit fees, GA treatment fees, and post-treatment complementary costs), direct nonmedical costs (travel costs), and indirect costs (time off from work to visit physician) were considered (Table 1). Since there was no standard pricing for GA treatment in China, the price per GA treatment was estimated using the mean cost in three Chinese tertiary hospitals (Xiangya Hospital; The Third Xiangya Hospital; and Xiangya Second Hospital, Central South University). Physicians’ professional fees and indirect costs in term of time loss were estimated according to the data from the 2017 Yearbook of Health Statistics of China.31 All costs in this study are expressed in USD with an exchange rate of USD 1=CNY 6.23 (2017).
Table 1.
Aggregated costs of glycolic acid (GA) treatment per time
| Cost | Hospital 1 (USD) | Hospital 2 (USD) | Hospital 3 (USD) | Average (USD) |
|---|---|---|---|---|
|
| ||||
| Direct costs | ||||
| Physician visit | 10 | 7 | 7 | 8 |
| GA treatment | 95 | 85 | 100 | 93.3 |
| Post-treatment costs | 12 | 15 | 17 | 15 |
| Direct nonmedical cost | ||||
| In-city transportation | 1.5 | 1.5 | 1.5 | 1.5 |
| Indirect costs | ||||
| Time off from work | 10 | 10 | 10 | 10 |
| Total | 128.5 | 118.5 | 135.5 | 127.8 |
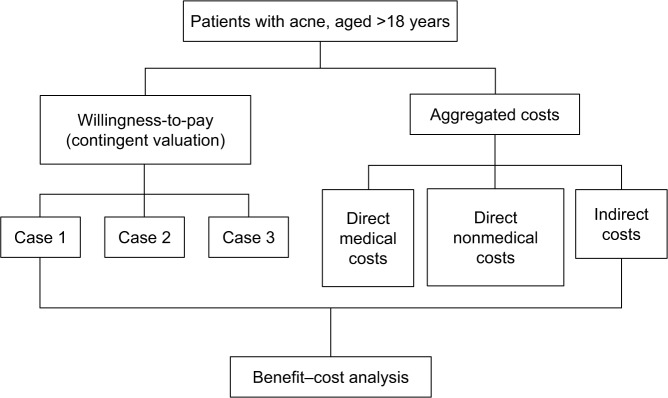
BCA
The BCA model was based on the benefit–cost ratio (BCR), calculated as the average WTP divided by the total cost for GA peels, from the patient perspective (Figure 1). If the benefits outweighed the costs (ie, BCR>1), the GA treatment was considered worth providing.
Figure 1.
Flow chart for benefit–cost analysis.
Other variables
The Cardiff Acne Disability Index (CADI),22,23 a widely used tool to assess adults’ acne disability, was used to examine the correlation between CADI and WTP. A higher CADI score implies a greater QoL impairment. Information regarding age, gender, income, marital status, acne history, and self-rated acne severity (0–5) were also collected.
Statistical analyses
The average WTP for each scenario was analyzed respectively. Medians, IQRs, means, and SDs were used for statistical description. Paired t-test and Wilcoxon matched-pairs signed-rank test were used to compare the mean and median WTP among the three cases. Generalized linear models with a logarithm link function and gamma distribution were used to estimate the associations of WTP with the characteristics of the participants. Regression coefficients of the log-gamma models were transformed to ORs for better interpretations. SAS 9.4 (SAS Institute, Inc., Cary, NC, USA) was used for statistical analysis. P<0.05 was considered statistically significant.
Ethics statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki. All procedures involving patients were approved by the Institutional Research Ethics Board of Xiangya Hospital, Central South University (Changsha, China). Written or electronic informed consent was obtained from all patients before the investigation.
Results
The response rate was 95.4% and a total of 476 anonymous participants (female: 69.2%, male: 30.8%) were recruited of which 454 were analyzed (Table 2).
Table 2.
Demographic characteristics of the participants
| Characteristics | N | % |
|---|---|---|
|
| ||
| Gender | ||
| Male | 140 | 30.8 |
| Female | 314 | 69.2 |
| Age, years | ||
| 18–25 | 187 | 41.2 |
| 26–29 | 168 | 37.0 |
| 30–39 | 78 | 17.2 |
| ≥40 | 21 | 4.6 |
| Marital status | ||
| Single | 162 | 35.7 |
| In a stable relationship | 123 | 27.1 |
| Married | 169 | 37.2 |
| Monthly income, USD | ||
| No stable income | 55 | 12.1 |
| <153 | 36 | 7.9 |
| 154–461 | 90 | 19.8 |
| 462–769 | 119 | 26.2 |
| 770–1,538 | 111 | 24.4 |
| >1,538 | 43 | 9.5 |
| History of acne | ||
| Never | 0 | 0 |
| Occasionally | 299 | 65.9 |
| Frequently | 155 | 34.1 |
| Self-rated acne severity | ||
| 0 | 50 | 11.0 |
| 1 | 163 | 35.9 |
| 2 | 124 | 27.3 |
| 3 | 78 | 17.2 |
| 4 | 29 | 6.4 |
| 5 | 10 | 2.2 |
| Cardiff Acne Disability Index | ||
| Mild (0–5) | 339 | 74.7 |
| Moderate (6–11) | 101 | 22.2 |
| Severe (11–15) | 14 | 3.1 |
Costs
The average cost from the patient perspective is USD 127.8 per time. The total cost per GA treatment is USD 128.5, 118.5, and 135.5 for Hospital 1, 2, and 3, respectively. The details of aggregated costs are presented in Table 1. We informed the participants that three treatments are required to achieve the demonstrated effects, which cost USD 127.8×3=USD 383.4 in total.
WTP
The mean and median WTP for the three cases are presented in Table 3. Differences in WTP were statistically significant between Case 1 and Case 3 (P<0.001), and Case 2 and Case 3 (P<0.001), but not significant between Case 1 and Case 2 (P=0.255). Factors for WTP were analyzed using log-gamma models owing to better goodness-of-fit than general linear models. As shown in Table 4, females were less willing to pay for Case 1 and Case 2 than males. Participants in the highest income group (>USD 1,538/month) were willing to pay 1.56–2.15 times the amount of money compared to those with no stable income for the cases. Patients with the highest self-reported severity were willing to pay 2.31–4.62 times the amount of money compared to those with the lowest severity score for the cases.
Table 3.
Willingness-to-pay (WTP) for different case scenarios of glycolic acid treatment per
| Case | Mean WTP per time (USD) | Mean WTP in total (USD) | Median WTP per time (USD) | IQR (USD) |
|---|---|---|---|---|
|
| ||||
| 1 | 78.2 | 234.6 | 38.5 | 15.4–76.9 |
| 2 | 74.0 | 222.0 | 38.5 | 15.4–76.9 |
| 3 | 133.9 | 401.7 | 76.9 | 38.5–153.5 |
| P-value | ||||
| 1 vs 2 | 0.251 | 0.255 | ||
| 2 vs 3 | <0.001 | <0.001 | ||
| 1 vs 3 | <0.001 | <0.001 | ||
Table 4.
Factors of willingness-to-pay for different case scenarios of glycolic acid treatment: log-gamma regression models
| Variables | Case 1
|
Case 2
|
Case 3
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| β | OR | P-value | β | OR | P-value | β | OR | P-value | |
|
| |||||||||
| Gender | |||||||||
| Male | Reference | Reference | Reference | ||||||
| Female | −0.40 | 0.67 | <0.001 | −0.24 | 0.78 | 0.044 | −0.16 | 0.85 | 0.152 |
| Age, years | |||||||||
| 18–25 | Reference | Reference | Reference | ||||||
| 26–29 | 0.12 | 1.13 | 0.353 | −0.17 | 0.840 | 0.189 | 0.03 | 1.03 | 0.804 |
| 30–39 | 0.40 | 1.50 | 0.042 | 0.06 | 1.057 | 0.784 | −0.04 | 0.96 | 0.831 |
| ≥40 | 0.40 | 1.51 | 0.164 | 0.20 | 1.22 | 0.502 | 0.09 | 1.1 | 0.743 |
| Marital status | |||||||||
| Single | Reference | Reference | Reference | ||||||
| In a stable relationship | 0.21 | 1.23 | 0.123 | −0.02 | 0.98 | 0.903 | 0.01 | 1.01 | 0.923 |
| Married | −0.15 | 0.86 | 0.344 | −0.02 | 0.98 | 0.895 | −0.08 | 0.92 | 0.596 |
| Monthly income, USD | |||||||||
| No stable income | Reference | Reference | Reference | ||||||
| <153 | 0.10 | 1.10 | 0.692 | 0.09 | 1.10 | 0.703 | −0.17 | 0.85 | 0.472 |
| 154–461 | −0.34 | 0.72 | 0.088 | -0.18 | 0.84 | 0.372 | −0.30 | 0.74 | 0.111 |
| 462–769 | −0.07 | 0.93 | 0.720 | 0.24 | 1.27 | 0.217 | −0.02 | 0.99 | 0.935 |
| 770–1,538 | 0.03 | 1.03 | 0.868 | 0.38 | 1.46 | 0.066 | 0.14 | 1.15 | 0.473 |
| >1,538 | 0.46 | 1.59 | 0.049 | 0.77 | 2.15 | 0.001 | 0.45 | 1.56 | 0.053 |
| History of acne | |||||||||
| Occasionally | Reference | Reference | Reference | ||||||
| Frequently | −0.05 | 0.95 | 0.730 | -0.05 | 0.95 | 0.715 | −0.24 | 0.79 | 0.075 |
| Self-rated acne severity | |||||||||
| 0 | Reference | Reference | Reference | ||||||
| 1 | 0.11 | 1.11 | 0.553 | 0.15 | 1.17 | 0.406 | 0.16 | 1.18 | 0.358 |
| 2 | −0.21 | 0.81 | 0.288 | -0.08 | 0.93 | 0.696 | 0.16 | 1.17 | 0.403 |
| 3 | −0.11 | 0.89 | 0.620 | 0.01 | 1.01 | 0.973 | 0.32 | 1.38 | 0.141 |
| 4 | −0.26 | 0.77 | 0.406 | 0.33 | 1.39 | 0.307 | 0.16 | 1.17 | 0.600 |
| 5 | 1.19 | 3.28 | <0.001 | 1.53 | 4.62 | <0.001 | 0.84 | 2.31 | 0.034 |
| Cardiff Acne Disability Index | 0.03 | 1.03 | 0.202 | 0.05 | 1.05 | 0.047 | 0.05 | 1.05 | 0.019 |
| score (continuous) | |||||||||
CADI
The mean CADI was 4.0±2.9, and 115 (25.3%) of the participants reported moderate-to-severe impairment by acne (CADI>5). The mean CADI in females (4.5±3.1) was significantly higher than that in males (2.9±2.0). The CADI was also associated with WTP (Table 4). A 1-point increase in the CADI score was associated with 1.05 times the amount of money to pay for Case 2 and Case 3 (P<0.05). However, for Case 1 the CADI was not significantly correlated to WTP (P>0.05).
BCR
As shown in Table 5, only Case 3 had BCR>1 among the three cases, indicating that the expected benefits exceed the aggregated costs for the GA treatments. In the other two cases, the BCRs were close to 0.6. Because the denominators of the BCRs were the same across the participants, the factors for the BCRs were equivalent to those for WTP (Table 4).
Table 5.
Benefit–cost ratios
| Case | Mean willingness-to-pay for three times (USD) | Mean costs for three times (USD) | Benefit–cost ratio |
|---|---|---|---|
|
| |||
| 1 | 234.6 | 383.4 | 0.61 |
| 2 | 222 | 383.4 | 0.58 |
| 3 | 535.6 | 383.4 | 1.40 |
Discussion
WTP for cases with different efficacy ranged from USD 222.0 to 401.7. The aggregated costs for three GA treatments were USD 383.4 on average. WTP was significantly associated with gender, a higher self-reported acne severity, and a higher CADI score across the cases. Case 3 had BCR>1, while Case 1 and Case 2 had BCR<1.
Instead of detecting cost-effectiveness using the traditional methods with cost/clinical outcomes or cost/quality-adjusted life year (QALY), our study identified WTP for the efficacy of certain acne treatment and then performed BCA for GA in acne treatment, providing evidence for health-related QoL of acne and evidence of pharmacoeconomics for CP in China. In the past, the WTP method to reflect utility in monetary terms was scarcely used in the field of dermatology.24–29 For skin conditions with the rare risk of disability or death, WTP can reflect and express the disease burden in a monetary manner, which may be more accurate and direct in detecting the impaired QoL compared with the traditional tools such as QALY and time tradeoff.30 In addition, by calculating whether the expected WTP value can be sufficient to cover the expected costs, BCA can help to make decisions and subdivide patients’ demands.
In the present study, the elicited WTP values are valid because WTP was significantly related to income, in accordance with the economic common sense. Our results showed that young people in China were willing to pay for the GA treatment of acne, primarily when the efficacy of treatment was satisfactory and the self-reported acne severity was high. The visualized effects of Case 3 are more apparent compared to the other two cases since the removal of hyperpigmentation and redness in Case 3 is the most effective among the three cases. The different effects across the three cases may be due to the heterogeneity toward CP among Asians.
A significant positive association between WTP and self-reported acne severity was observed for all three cases after adjustments (P<0.01). WTP was also positively associated with the CADI with a moderate effect size, consistent with a previous study on the QoL of acne.22 Interestingly, the mean CADI score in female participants was significantly higher than that in male participants, but WTP in men was significantly higher. A possible explanation is that although female patients have a heavier perceived burden of acne, as indicated by the CADI, they have more information and channels for acne treatments as well, compared with male patients. Therefore, male patients may better appreciate the benefits of the GA treatments.
The present BCA indicates that the overall benefits outweigh the costs for the GA treatment in Case 3, but the costs offset the benefits in Case 1 and Case 2, indicating that Chinese patients hold positive attitudes toward GA treatment, especially when the acne is perceived to be severe and the expected efficacy is desirable. However, the significant differences in WTP across the cases indicate that patient segmentation for personalized acne therapies is needed.
As with any modeling-based analysis, the limitations of this study are inherent. First, the selected sample cannot represent the whole demographics of Chinese acne patients. This sample was younger and more educated compared to the general population. However, no significant difference in WTP was identified across age, employment, and educational groups. Further, WTP is different, by nature, from utility measurement. Using WTP to represent the benefits of one treatment would be partial to capture effectiveness or utility. In addition, because it is hard to standardize and quantify the expected effects due to the varying effects across different skin types and acne types, expert-selected cases for WTP detection might lead to less accuracy and more subjective conclusions. However, in order to meet both the needs for accuracy and representativeness for broader patients, illustration in visualized cases is the most feasible way to demonstrate the expected effects and to detect WTP.
Conclusion
CPs are an acceptable acne treatment from the perspective of health economics. Although the benefits of GA treatment have not generally exceeded their aggregated costs across three cases, WTP is positively associated with self-reported acne severity and desirable treatment effects. Acne treatments can be personalized and tailored according to the extent of QoL impairment in China.
Supplementary material
Contrast figures of three cases treated with glycolic acid.
Acknowledgments
This work was supported by the Ministry of Science and Technology of the People’s Republic of China (2015FY111100, 2016YFC0900802), and the Department of Science and Technology of Hunan Province (2018SK2086).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134(6):1527–1534. doi: 10.1038/jid.2013.446. [DOI] [PubMed] [Google Scholar]
- 2.Collier CN, Harper JC, Cafardi JA, et al. The prevalence of acne in adults 20 years and older. J Am Acad Dermatol. 2008;58(1):56–59. doi: 10.1016/j.jaad.2007.06.045. [DOI] [PubMed] [Google Scholar]
- 3.Wolkenstein P, Machovcová A, Szepietowski JC, Tennstedt D, Veraldi S, Delarue A. Acne prevalence and associations with lifestyle: a cross-sectional online survey of adolescents/young adults in 7 European countries. J Eur Acad Dermatol Venereol. 2018;32(2):298–306. doi: 10.1111/jdv.14475. [DOI] [PubMed] [Google Scholar]
- 4.Wei B, Pang Y, Zhu H, et al. The epidemiology of adolescent acne in North East China. J Eur Acad Dermatol Venereol. 2010;24(8):953–957. doi: 10.1111/j.1468-3083.2010.03590.x. [DOI] [PubMed] [Google Scholar]
- 5.Huang X, Zhang J, Li J, et al. Daily intake of soft drinks and moderate-to-severe acne vulgaris in Chinese adolescents. J Pediatr. 2019;204:256–262. doi: 10.1016/j.jpeds.2018.08.034. [DOI] [PubMed] [Google Scholar]
- 6.Xiao Y, Huang X, Jing D, et al. The prevalence of atopic dermatitis and chronic spontaneous urticaria are associated with parental socioeconomic status in adolescents in China. Acta Derm Venerol. 2018 2018 Dec 6; doi: 10.2340/00015555-3104. Epub. [DOI] [PubMed] [Google Scholar]
- 7.Yeung CK, Teo LH, Xiang LH, Chan HH. A community-based epidemiological study of acne vulgaris in Hong Kong adolescents. Acta Derm Venereol. 2002;82(2):104–107. doi: 10.1080/00015550252948121. [DOI] [PubMed] [Google Scholar]
- 8.Yin NC, McMichael AJ. Acne in patients with skin of color: practical management. Am J Clin Dermatol. 2014;15(1):7–16. doi: 10.1007/s40257-013-0049-1. [DOI] [PubMed] [Google Scholar]
- 9.Tian L, Xie H, Yang T, Hu Y, Li J, Wang W. TNFR 2 M196R polymorphism and acne vulgaris in Han Chinese: a case-control study. J Huazhong Univ Sci Technolog Med Sci. 2010;30(3):408–411. doi: 10.1007/s11596-010-0366-z. [DOI] [PubMed] [Google Scholar]
- 10.Xie H, Xiao X, Li J. Topical steroids in Chinese cosmetics. JAMA Dermatol. 2017;153(9):855–856. doi: 10.1001/jamadermatol.2017.1615. [DOI] [PubMed] [Google Scholar]
- 11.Lei S, Wu Q, Shi Q, Lei S. Survey on changes in the proportion for facial aesthetics. J Cent South Univ Med Sci. 2016;41(12):1358–1361. doi: 10.11817/j.issn.1672-7347.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 12.Zhou MS, Xie H, Cheng L, Li J. Clinical characteristics and epidermal barrier function of papulopustular rosacea: a comparison study with acne vulgaris. Pak J Med Sci. 2016;32(6):1344–1348. doi: 10.12669/pjms.326.11236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levy LL, Zeichner JA. Management of acne scarring, part II: a comparative review of non-laser-based, minimally invasive approaches. Am J Clin Dermatol. 2012;13(5):331–340. doi: 10.2165/11631410-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 14.Handog EB, Datuin MS, Singzon IA. Chemical peels for acne and acne scars in Asians: evidence based review. J Cutan Aesthet Surg. 2012;5(4):239–246. doi: 10.4103/0974-2077.104911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moy LS, Kotler R, Lesser T. The histologic evaluation of pulsed carbon dioxide laser resurfacing versus phenol chemical peels in vivo. Dermatol Surg. 1999;25(8):597–600. doi: 10.1046/j.1524-4725.1999.98246.x. [DOI] [PubMed] [Google Scholar]
- 16.Erbagci Z, Akcali C. Biweekly serial glycolic acid peels vs. long-term daily use of topical low-strength glycolic acid in the treatment of atrophic acne scars. Int J Dermatol. 2000;39(10):789–794. doi: 10.1046/j.1365-4362.2000.00076.x. [DOI] [PubMed] [Google Scholar]
- 17.Chen CL, Kuppermann M, Caughey AB, Zane LT. A community-based study of acne-related health preferences in adolescents. Arch Dermatol. 2008;144(8):988–994. doi: 10.1001/archderm.144.8.988. [DOI] [PubMed] [Google Scholar]
- 18.Wang CM, Huang CL, Hu CTS, Chan HL. The effect of glycolic acid on the treatment of acne in Asian skin. Dermatol Surg. 1997;23(1):23–29. doi: 10.1111/j.1524-4725.1997.tb00003.x. [DOI] [PubMed] [Google Scholar]
- 19.Olsen JA, Smith RD. Theory versus practice: a review of “willingness-to-pay” in health and health care. Health Econ. 2001;10(1):39–52. doi: 10.1002/1099-1050(200101)10:1<39::aid-hec563>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 20.Layard PRG. Cost-benefit Analysis. Cambridge: Cambridge University Press; 1994. [Google Scholar]
- 21.Mitchell RC, Carson RT. Using Surveys to Value Public Goods: The Contingent Valuation Method. Washington, DC: Resources for the Future; 2013. [Google Scholar]
- 22.Motley RJ, Finlay AY. Practical use of a disability index in the routine management of acne. Clin Exp Dermatol. 1992;17(1):1–3. doi: 10.1111/j.1365-2230.1992.tb02521.x. [DOI] [PubMed] [Google Scholar]
- 23.Law MP, Chuh AA, Lee A, Molinari N. Acne prevalence and beyond: Acne disability and its predictive factors among Chinese late adolescents in Hong Kong. Clin Exp Dermatol. 2010;35(1):16–21. doi: 10.1111/j.1365-2230.2009.03340.x. [DOI] [PubMed] [Google Scholar]
- 24.Lundberg L, Johannesson M, Silverdahl M, Hermansson C, Lindberg M. Quality of life, health-state utilities and willingness to pay in patients with psoriasis and atopic eczema. Br J Dermatol. 1999;141(6):1067–1075. doi: 10.1046/j.1365-2133.1999.03207.x. [DOI] [PubMed] [Google Scholar]
- 25.Radtke MA, Schäfer I, Gajur A, Langenbruch A, Augustin M. Willingness-to-pay and quality of life in patients with vitiligo. Br J Dermatol. 2009;161(1):134–139. doi: 10.1111/j.1365-2133.2009.09091.x. [DOI] [PubMed] [Google Scholar]
- 26.Delfino M, Jr, Holt EW, Taylor CR, Wittenberg E, Qureshi AA. Willingness-to-pay stated preferences for 8 health-related quality-of-life domains in psoriasis: a pilot study. J Am Acad Dermatol. 2008;59(3):439–447. doi: 10.1016/j.jaad.2008.05.032. [DOI] [PubMed] [Google Scholar]
- 27.Beikert FC, Langenbruch AK, Radtke MA, Kornek T, Purwins S, Augustin M. Willingness to pay and quality of life in patients with atopic dermatitis. Arch Dermatol Res. 2014;306(3):279–286. doi: 10.1007/s00403-013-1402-1. [DOI] [PubMed] [Google Scholar]
- 28.Schiffner R, Brunnberg S, Hohenleutner U, Stolz W, Landthaler M. Willingness to pay and time trade-off: useful utility indicators for the assessment of quality of life and patient satisfaction in patients with port wine stains. Br J Dermatol. 2002;146(3):440–447. doi: 10.1046/j.1365-2133.2002.04613.x. [DOI] [PubMed] [Google Scholar]
- 29.Beikert FC, Langenbruch AK, Radtke MA, Augustin M. Willingness to pay and quality of life in patients with rosacea. J Eur Acad Dermatol Venereol. 2013;27(6):734–738. doi: 10.1111/j.1468-3083.2012.04549.x. [DOI] [PubMed] [Google Scholar]
- 30.Seidler AM, Bayoumi AM, Goldstein MK, Cruz PD, Jr, Chen SC. Willingness to pay in dermatology: assessment of the burden of skin diseases. Journal of Investigative Dermatology. 2012;132(7):1785–1790. doi: 10.1038/jid.2012.50. [DOI] [PubMed] [Google Scholar]
- 31.National Health and Family Planning Commission of the People’s Republic of China 2017 Yearbook of Health and Family Planning Statistics of China. Beijing: Beijing Union Medical University Press; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Contrast figures of three cases treated with glycolic acid.