Abstract
Objective:
The current study sought to test whether higher-quality mother-daughter communication would buffer associations between maternal depressive symptoms and girls’ internalizing and externalizing psychopathology symptoms among urban African American girls across a 12-month period.
Method:
One hundred ninety-four treatment-seeking urban African American adolescent girls, ages 12–16, and their mothers participated in the study. Every six months (for up to 3 assessments), daughters reported on their internalizing and externalizing symptoms, mothers reported on their depressive symptoms, and both mothers and daughters reported on the quality of their dyadic communication. Daughters additionally reported on the extent to which they felt accepted by their mothers at each assessment.
Results:
Results of multilevel modeling revealed that quality of communication significantly interacted with maternal depressive symptoms to predict externalizing and internalizing symptoms in daughters, such that risk associated with maternal depressive symptoms was fully buffered for daughters in high-quality communication dyads. Secondary analyses demonstrated that these patterns of results were not accounted for by higher levels of social status or maternal acceptance.
Conclusions:
Drawing on a vulnerable and understudied population of urban African American adolescent girls, this work suggests that family communication may contribute to important intergenerational psychopathology transmission processes, above and beyond more general features of the family environment.
Keywords: Ethnic minority youth, Externalizing disorders, Internalizing disorders, Parent-child relationships
Adolescence is a period of heightened vulnerability to psychopathology (Crews, He, & Hodge, 2007; Leussis & Andersen, 2007; R. E. Roberts & Attkisson, 1998), with increased rates of symptom onset reliably documented for major depression (Twenge & Nolen-Hoeksema, 2002), generalized anxiety disorder (Campbell, Brown, & Grisham, 2004), social phobia, and panic disorder (Kessler, Berglund, Demler, & Jin, 2005; Last, Perrin, Hersen, & Kazdin, 1992). Likewise, aggression that emerges during adolescence appears to predict future disruptive disorders better than aggression with childhood onset (Broidy, Nagin, & Tremblay, 2003). This developmental vulnerability affects girls in particular, such that the significant gender differences in mood and anxiety disorders that characterize adult psychopathology first emerge during adolescence (P. M. Lewinsohn, Gotlib, Lewinsohn, Seeley, & Allen, 1998; P. M. Lewinsohn, Hops, & Roberts, 1993).
Efforts to assess racial differences in adolescent vulnerability to emergent mental health problems have led to mixed findings. Some research documents lower rates of depression and anxiety disorders among African American youths than among White youths (Jackson, Torres, & Caldwell, 2004; Saluja, Iachan, & Scheidt, 2004), while other research finds no differences in prevalence rates between these populations (Cole, Martin, Peeke, & Henderson, 1998; Costello et al., 2002; McLaughlin, Hilt, & Nolen-Hoeksema, 2007). With regard to externalizing symptoms, African American adolescents consume alcohol at lower rates than their White peers, but are rated as having more aggression-related problems and higher delinquency (Cameron & Guterman, 2007; Daughters et al., 2009; Eaton, Kann, Kinchen, & Shanklin, 2012). Regardless of symptom type, however, African Americans are less likely than their White counterparts to receive care for mental health and substance problems at all developmental stages (Ialongo et al., 2017; Wells, Klap, Koike, & Sherbourne, 2001). The combination of heightened developmental vulnerability to mental health problems associated with adolescence and low rates of care increase risk for enduring negative health outcomes. Understanding the factors that contribute to symptoms of internalizing and externalizing psychopathology in African American adolescent girls will inform prevention efforts to reduce poor health trajectories.
One robust predictor of mental health symptomatology in youths is parental depression. As Elgar et al. (2004) reports, children of depressed parents have 2–5 times the rate of psychiatric disorders as children of non-depressed parents. Meta-analytic research finds that maternal depression significantly relates to higher levels of internalizing, externalizing, and general psychopathology in youths (Goodman et al., 2011). Consistent with broader gender differences, girls appear more vulnerable than boys to these effects (Bosco, Renk, Dinger, Epstein, & Phares, 2003; Burt et al., 2005; Grant et al., 2003). Similar patterns exist within urban African American communities, as maternal depressive symptoms predict elevated internalizing and externalizing symptoms in African American preschoolers (Koblinsky, Kuvalanka, & Randolph, 2006), however less is known about adolescent African American girls.
Although genetic liability contributes to the intergenerational transmission of mental health symptomatology (Lahey, van Hulle, Singh, Waldman, & Rathouz, 2011), research indicates that environmental factors are also important (Silberg, Maes, & Eaves, 2010; Singh et al., 2010). Using an adoption study paradigm, Tully, Iacono, and McGue (2008) showed that exposure to a depressed caregiver increases risk for youth depressive and disruptive disorders regardless of shared genetic profiles. Evidence suggests that transmission occurs through impaired parenting behaviors (Lim, Wood, & Miller, 2008); that is, parents with depression display more intrusive and hostile caregiving and show greater negative affect (Lovejoy, Graczyk, O’Hare, & Neuman, 2000). Among African American mothers, depression has been associated with lower levels of warmth and less child-centered parenting (Bluestone & Tamis-LeMonda, 1999). In turn, impaired parenting is reliably associated with youth mental health problems (Caron, Weiss, Harris, & Catron, 2006; Cuffe, McKeown, Addy, & Garrison, 2005; Gutman & McLoyd, 2005). In African American families, negative parenting behaviors predicts internalizing and externalizing problems (Brody & Flor, 1997; Pittman & Lansdale, 2001), worse academic and professional achievement (Pittman & Lansdale, 2001), and lower self-esteem and more delinquent behavior (Bynum & Kotchick, 2006). Furthermore, contextual features affecting African American communities, such as the prevalence of single-parent households headed by mothers (Greene, 2009) and resource instability associated with living in urban environments (Jarrett, 1994), raise the possibility that dimensions of relationships with mothers maybe especially influential in the lives of African American adolescents (Aronowitz & Morrison-Beedy, 2004).
If risk for psychopathology is conferred by problematic parenting, as described above, then it is possible that more positive dimensions of parenting may buffer vulnerability despite parental depression. Consistent with this hypothesis, Brody et al. (2005) found that parenting interventions for African American families that addressed a broad range of behaviors, like parental involvement and racial pride, were associated with better psychopathology-related outcomes among youth, including better self-control. Likewise, in an intervention targeting adolescent children of depressed parents, changes in positive parenting (such as warmth and responsiveness) accounted for improvements in youth mental health (Compas et al., 2010). What is less clear, however, is which components of more optimal parenting may account for these effects.
Research on the role of positive parenting in the context of youth symptomatology has generally emphasized affective parenting characteristics, such as warmth or acceptance (Hipwell et al., 2008; Waller et al., 2014). However, other aspects of parent-child relationships may impact youth mental health, such as parent-child communication. Parent-child communication that is more open, less conflictual, and more frequent (“higher quality”) may serve as an important proximal activity that both reflects and reinforces the quality of the relationship. Furthermore, although parental communication and parenting relationship quality are likely related, Wills et al. (2003) demonstrated that frequency of parental communication about sexual behavior and substance use within African American families exerted a unique protective effect, even after controlling for parental supportiveness. This suggests that high-quality communication may not simply be a proxy for a better parent-child relationship, but may contribute in unique ways to youth outcomes. For example, more open and less hostile communication may help reduce family conflict, improve collaborative problem-solving, or foster trust between parent and child. Notably, communication may also be an aspect of parenting that is amenable to change or responsive to preventative intervention, perhaps moreso than affective dimensions of parenting behaviors, like parental acceptance or warmth.
In line with the possibility that communication may facilitate or buffer intergenerational psychopathology risk, worse parent-adolescent communication has been associated with higher externalizing symptoms among urban youth seeking mental health services (Rodriguez, Nichols, Javdani, Emerson, & Donenberg, 2013). For African American mothers and adolescents, poor communication is associated with more youth depressive symptoms (Taylor & Seaton, 2008), and better communication predicts fewer youth problem behaviors (Smetana, Crean, & Daddis, 2002). Substantial research also demonstrates associations between mother-daughter communication and girls’ sexual risk, revealing that less open and less frequent communication between African American mothers and daughters is associated with daughters’ greater likelihood of having engaged in vaginal or anal intercourse (Donenberg, Emerson, & Mackesy-Amiti, 2011). Moreover, communication may be especially relevant for mothers and daughters, because they report more frequent and open communication than fathers and sons (Noller & Bagi, 1985), and because girls prefer to talk to their mothers more than their fathers about sensitive topics. While these findings support possible associations between family communication and youths’ mental health, to our knowledge no previous work has examined mother-daughter communication in the context of the intergenerational transmission of psychopathology symptoms, particularly among urban African American women and girls seeking mental health services.
To address these gaps, in this study we examined whether higher-quality mother-daughter communication would buffer associations between maternal depressive symptoms and girls’ internalizing and externalizing psychopathology among urban African American girls seeking mental health care across a twelve-month period. In contrast to most community or school-based studies, an examination of this participant sample allows for a clinically relevant test of associations, offering new insight into the unique circumstances of urban African American families who have self-identified as needing mental health services for their girls. We hypothesized that higher levels of maternal depressive symptoms would relate to more internalizing and externalizing symptoms in daughters, and that higher-quality mother-daughter communication (characterized by greater openness and fewer problems) would relate to fewer internalizing and externalizing symptoms in daughters. Importantly, we expected higher-quality communication to buffer the impact of maternal depression on girls’ internalizing and externalizing mental health problems. We also predicted that higher-quality communication would relate to better youth outcomes above and beyond broader indicators of relationship quality, such as parental acceptance, and would not be accounted for by higher social status.
Methods
Participants and Procedures
This study is part of a larger project examining HIV-risk among African American girls seeking psychiatric services. One hundred ninety-four girls, aged 12–16 years old (M=14.46; SD=1.15), and their mothers participated in the current study. Families were recruited from eight mental health clinics in a large American city. Clinic staff contacted eligible families (12–16 years-old, self-identified as Black or African American) and requested permission to forward their contact information to the research team. The project recruiter explained the study in detail and scheduled a baseline appointment.
Girls were ineligible for the study if they were identified as wards of the state or had significant cognitive impairment that would interfere with their ability to understand the assent process. Most referred daughters (82%) participated in the baseline interview (N = 281). Female caregivers provided written consent and daughters provided written assent. In the current study, only dyads with biological mothers and their daughters were examined, resulting in a sample of 194 dyads. Mothers were on average 38.95 years old (SD=6.93) and 21.5% reported being the only caregiver for their daughter. According to maternal report, 21.6% of mothers did not complete high school, 22.2% graduated high school, 43.3% attended some college or specialty training, and 12.9% earned a college degree or higher. All activities were approved by the University of Illinois at Chicago Institutional Review Board. In this study, mothers supplied demographic information, and mothers and daughters each reported on their own mental health symptoms and the quality of mother-daughter communication at baseline, 6-, and 12-months at laboratory assessments. Daughters also reported on the quality of the mother-daughter relationship. Retention was strong at 6-months (81%) and 12-months (80%). There were no significant differences on demographic features, mother or daughter psychopathology symptoms, or communication variables between dyads who participated at all points and those with missing data, with the exception that, somewhat surprisingly, families with complete data had mothers with slightly higher levels of depressive symptoms at baseline than families with missing data (56.67 vs 51.89, t=2.76, p=.006). Mothers and daughters each received $45 at baseline plus $15 for travel and parking. Remuneration increased by $5 at each follow-up.
Measures
Demographic Information.
Mothers reported on their age, their daughter’s age, whether their daughter has any other caregivers, and their highest level of education during the baseline assessment.
Youth Psychopathology Symptoms.
At each assessment, daughters reported on their symptoms of psychopathology using the Youth Self Report (YSR), the widely used adolescent self-report version of the Child Behavioral Checklist (Achenbach & Rescorla, 2001). The YSR consists of 102-items in which youths rate on a 0–2 scale whether the problem item is not true of them (0), somewhat or sometimes true of them (1), or true of them (2). Sample items include “I cry a lot,” “I get in many fights,” and “I act without stopping to think.” The YSR generates raw and T-scores for broad-band internalizing (e.g., sadness, anxiety) and externalizing (e.g., fighting, aggression) problems. Higher scores indicate greater problems. The reliability and validity of the YSR are well established, including for use in clinical and community samples and across diverse cultural settings (Compas et al., 1997; Ivanova et al., 2007). Internal reliability was high for internalizing (average α across visits = .85) and externalizing (average α across visits =.90) symptoms in this study. YSR internalizing and externalizing T-scores were used in the data analyses to preserve the contextualized scoring that accounts for developmental, racial, and gender differences in symptom presentations.1
Maternal Depressive Symptoms.
Mothers reported their depressive symptoms on the depression subscale of the SCL-90 (Derogatis, 2004) at each assessment point. The depression subscale consists of 13-items probing the extent to which participants have been bothered by depressive symptoms on a 0 (“not at all”) to 4 (“extremely”) scale over the past month. Higher scores correspond to more depressive symptomatology and have been shown to converge with other self- and observer-reports of depression (Aben, Verhey, Lousberg, Lodder, & Honig, 2011). The average Cronbach’s α across the three visits was .88. As with youth symptoms, T-scores based on racial, age, and gender norms were used to reflect the contextualized symptom severity.
Mother-Daughter Communication.
At each assessment, mothers and daughters separately completed the Parent-Adolescent Communication Scale (Barnes & Olson, 1982), probing perceptions of openness, responsiveness, and difficulty communicating with each other. Participants rated the extent to which they agreed or disagreed with 20-items on a 1 (“strongly disagree”) to 5 (“strongly agree”) scale. Ten items correspond to open communication, such as “I am very satisfied with how my mother/adolescent and I talk together,” and “My mother/adolescent is always a good listener.” Ten items correspond to problems with communication, including “My mother/adolescent insults me when she is angry with me,” or “When we are having a problem, I often give my mother/adolescent the silent treatment.” Scores on the problem subscale were reverse scored and then summed with the openness items, resulting in a total score corresponding to more optimal, higher-quality communication (average α for daughters across visits = .87, average α for mothers across visits=.82). Mothers’ and daughters’ scores were significantly correlated at each time point (rs=.29-.40, ps<.001); reports were averaged to create a family communication variable at each visit.
Maternal Acceptance.
At each visit, girls reported on the extent to which they felt accepted by their mother on the Child Report of Parent Behavior (Schaefer, 1965). We used the Acceptance subscale consisting of 8 statements rated on a 3-point scale (1=not like my mother, 2=somewhat like my mother, 3=a lot like my mother). Sample items include “My mother makes me feel better after talking things over with her” and “My mother believes in showing her love for me.” This measure has been extensively studied and validated in both European-American and African-American samples (Krishnakumar & Buehler, 2004). Internal reliability was acceptable (average α = .89).
Social Status.
At baseline, mothers also provided information about the occupation and education level for up to two people who contribute to household finances. Using the procedures outlined in Hollingshead (1975), these items were coded and combined to compute a Hollingshead index score, where lower scores correspond to lower social status.
Data Analytic Plan
Descriptive statistics and bivariate correlations were first computed to examine characteristics of the sample. Focal analyses then examined whether higher-quality mother-daughter communication buffered children from the effects of maternal depressive symptoms on daughters’ externalizing and internalizing psychopathology symptoms. To test this, we conducted a series of multilevel models with robust standard errors using Hierarchical Linear and Nonlinear Modeling (HLM) software (Version 6.08; Raudenbush, Bryk, & Congdon, 2004). Daughters’ externalizing psychopathology symptoms were predicted by maternal depressive symptoms, family communication, and the interaction between depressive symptoms and communication at each available time point plus visit number (to account for linear trends) and a random-effects intercept (Level 1), while covarying for daughters’ age, mothers’ age, whether she is the daughter’s only caregiver (dummy coded), and mothers’ highest education level (Level 2), to account for possible effects of demographic factors. HLM was the preferred method for analysis because it accounts for the non-independence of observations within a person as well as linear trends in symptoms over time. All variables were centered at the grand mean of the sample prior to analyses and all available data were used. A portion of the model is presented below:
thru modeled as above
Following any significant interaction terms, simple slopes analyses were conducted following techniques developed by Preacher, Curran, and Bauer (2006) examining the slope of mothers’ depressive symptoms on daughters’ externalizing psychopathology symptoms at the mean, 25th percentile (i.e., low-quality), and 75th percentiles (i.e., high-quality) of the sample distribution of communication. This was repeated to model daughter’s internalizing symptoms. Lastly, secondary analyses were conducted to test the possibility that observed associations might be accounted for by 1) broader family social status or 2) by a better overall relationship. Here, multilevel models were re-run while covarying family’s Hollingshead index value. Then, models were rerun with daughters’ report of their mother’s acceptance at Level 1.
Results
Bivariate Associations
Descriptive statistics and zero-order correlations amongst study variables are displayed in Table 1. Of note, bivariate correlations pooling data across all time points show that daughter’s internalizing and externalizing symptoms were significantly correlated with their mother’s depressive symptoms, family communication, and maternal acceptance. Twenty-nine percent of daughters self-reported clinically significant (T-score >62) internalizing problems, and 36% endorsed clinically significant externalizing symptoms. Appoximately 32% of mothers reported clinically-significant depressive symptoms.
Table 1.
Descriptive Statistics and Bivariate Correlations for Study Variables at Across All Timepoints
| Variable | Mean (SD) | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. |
|---|---|---|---|---|---|---|---|---|---|
| 1.Child age | 14.46 (1.15) | .29** | .11* | .04 | .16** | .09* | .00 | −.12** | −.08 |
| 2.Mother age | 38.95 (6.93) | .18** | −.01 | .01 | −.14 | .04 | −.08 | −.12 | |
| 3.Mother’s Education Category | 4.49 (1.05) | −.15** | −.02 | −.10* | −.04 | .07 | .02 | ||
| 4.Only Caregiver | 21.5% | .06 | .14* | .08 | −.03 | .03 | |||
| 5.Externalizing Sx T-Score (Child) | 55.29 (11.33) | .53** | .23** | −.50** | −.32** | ||||
| 6.Internalizing Sx T-Score (Child) | 52.02 (10.14) | .20** | −.35** | −.14** | |||||
| 7.Mother Depression T-Score | 54.07 (10.87) | −.20** | .03 | ||||||
| 8.Communication | 67.77 (10.96) | .66** | |||||||
| 9.Acceptance | 23.75 (5.41) | ||||||||
| Variable | Mean (SD) | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. |
| 10.Child age | 14.46 (1.15) | .29** | .11* | .04 | .16** | .09* | .00 | −.12** | −.08 |
| 11.Mother age | 38.95 (6.93) | .18** | −.01 | .01 | −.14 | .04 | −.08 | −.12 | |
| 12.Mother’s Education Category | 4.49 (1.05) | −.15** | −.02 | −.10* | −.04 | .07 | .02 | ||
| 13.Only Caregiver | 21.5% | .06 | .14* | .08 | −.03 | .03 | |||
| 14.Externalizing Sx T-Score (Child) | 55.29 (11.33) | .53** | .23** | −.50** | −.32** | ||||
| 15.Internalizing Sx T-Score (Child) | 52.02 (10.14) | .20** | −.35** | −.14** | |||||
| 16.Mother Depression T-Score | 54.07 (10.87) | −.20** | .03 | ||||||
| 17.Communication | 67.77 (10.96) | .66** | |||||||
| 18.Acceptance | 23.75 (5.41) | ||||||||
Note. The only caregiver variable is dummy coded where 0=daughter has more than one caregiver and 1=mother is only caregiver for daughter
p<.05;
p<.01.
Daughters’ Externalizing Symptoms
Utilizing HLM to account for the nested structure of our data of time points nested within dyads, there was a trend-level main effect of mothers’ depressive symptoms on daughters’ externalizing symptoms (b=.09, SE=.05, p=.068), such that daughters whose mothers reported more depressive symptoms self-reported more externalizing symptoms. There was also a significant main effect of communication on daughters’ symptoms (b=−.37, SE=.05, p=.000), wherein dyads with better communication had daughters who reported fewer symptoms. Further, there was a significant interaction between maternal depression and dyadic communication (b=−.11, SE=.00, p=.009), whereby the association between maternal depressive symptoms and daughters’ externalizing symptoms was stronger when dyads had lower-quality communication. In addition, daughter’s older age was associated with more externalizing symptoms (b=1.59, SE=.64, p=.014) and there was a significant linear trend wherein externalizing symptoms declined across visits (b=−1.03, SE=.39, p=.008).
Simple slopes follow up analyses revealed that the association between mothers’ depressive symptoms and daughters’ externalizing symptoms was stronger when dyads had low-quality communication (b=.17, SE=.06, p=.004) than when dyads had average-quality communication (b=.09, SE=.05, p=.075). Notably, there was no significant association between mothers’ depressive symptoms and daughters’ externalizing symptoms when dyads had high-quality communication (b=.01, SE=.06, p=.849). These findings suggest that high-quality communication buffered daughters from the effects of their mothers’ depressive symptoms on externalizing symptoms (see Figure 1).
Figure 1.
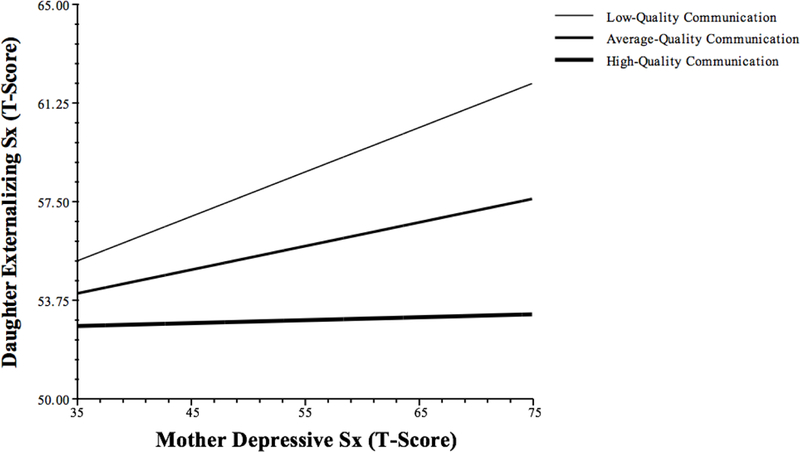
Interaction between Maternal Depressive Symptoms and Communication Predicting Daughters’ Externalizing Psychopathology Symptoms
Daughters’ Internalizing Symptoms
HLM analyses were repeated predicting daughter’s internalizing symptoms. Findings revealed a significant main effect of communication (b=−.27, SE=.05, p=.000) but not a significant main effect of parental depressive symptoms (b=.04, SE=.04, p=.270); however, findings must be interpreted in light of a significant interaction between communication and depression (b=−.01, SE=.00, p=.032). This suggests that the strength of the relationship between maternal depressive symptoms and daughters’ internalizing symptoms was stronger when dyads had lower-quality communication. In addition to these focal variables, main effects were also noted for several covariates: parents’ younger age (b=−.29, SE=.00, p=.002) and being the only caregiver (b=3.58, SE=.1.56, p=.023) were associated with more internalizing symptoms for daughters; there was also a significant trend of internalizing symptoms declining over visits (b=−2.68, SE=.30, p=.001).
Simple slopes follow up analyses revealed that there was a significant association between maternal depressive symptoms and daughter internalizing symptoms for dyads with low-quality communication (b=.10, SE=.04, p=.036), but this association was not significant for dyads with average-quality communication (b=.04, SE=.04, p=.288) nor high-quality communication (b=−.01, SE=.04, p=.817), suggesting that daughters were buffered from the effects of their mothers’ symptoms if they engaged in average or high-quality communication, as shown in Figure 2.
Figure 2.
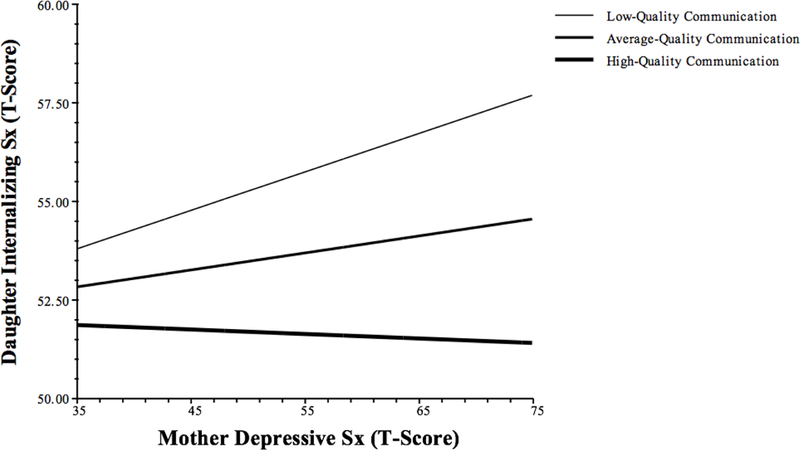
Main Effects of Maternal Depressive Symptoms and Communication Predicting Youth Internalizing Symptoms
Alternative Explanation: Other Measures of Socioeconomic Status
Although maternal education—a common index of family socioeconomic status—was included as a covariate in all analyses, it is possible that broader social status resources may contribute to the observed associations. Re-running the model predicting daughters’ externalizing symptoms while including Hollingshead index as a level 2 variable revealed identical results. Including Hollingshead index in the model of internalizing symptoms also yieled a similar pattern, however, the significance of the estimated coefficient for the slope of the internaction between maternal depression and communication on internalizing symptoms was reduced slightly to marginal significance (b=−.01, SE=.00, p=.057). Notably, there was not a main effect of Hollingshead index in either model. Together, these findings suggest that family economic resources do not account for the pattern of observed results.
Relationship Quality
Lastly, to assess whether observed associations were due to better mother-daughter relationship quality more broadly, we tested whether daughters’ reports of perceived maternal acceptance, entered in Level 1, altered the findings for communication. Given the significant bivariate associations between communication, perceived maternal acceptance, and daughters’ internalizing and externalizing symptoms, it is possible that families with high-quality communication have better overall relationships, which in turn, accounts for associations with daughters’ symptoms. However, the pattern of results were unchanged when adding maternal acceptance to the models, suggesting that the effects of communication and maternal depressive symptoms on daughters’ psychopathology profiles are not merely the result of higher- or lower-quality mother-daughter relationships.
Discussion
This study of urban African American adolescent girls and their mothers found support for a protective role of higher-quality family communication in the intergenerational transmission of mental health symptoms. Specifically, across both externalizing and internalizing symptoms—the two most common broad-band classifications of mental health problems—more open and less problematic communication between mothers and daughters was associated with better psychological profiles for girls. Moreover, this protective effect of high-quality communication was powerful enough to completely buffer girls from internalizing and externalizing symptoms associated with their mothers’ depressive symptoms, underscoring the critical role that parent-child communication may play in the transmission of mental health problems (Hammen, Shih, & Brennan, 2004). Importantly, these patterns of findings remained significant even after accounting for daughters’ reports of maternal acceptance—an indicator of a broadly positive relationship—and when accounting for broader social status. Hence, high-quality communication may be a unique contributor to protective processes associated with the intergenerational transmission of mental health symptoms.
That communication quality may be protective for youth psychopathology risk is not entirely surprising given research documenting links between family communication and youth mental health symptoms (Rodriguez et al., 2013; Smetana et al., 2002; Taylor & Seaton, 2008). More optimal family communication may help a mother express engagement with and interest in her daughter, signaling support and affection. Significantly, high-quality mother-daughter communication appears to do more than simply convey parental approval and positive regard, however, as daughters’ perceptions of maternal acceptance did not explain the links between communication and girls’ symptoms, despite significant correlation between communication and acceptance. One possibility is that high-quality mother-daughter communication may not only be a vehicle to express maternal support, but may also serve as a pedagogical mechanism to facilitate daughter’s adaptive problem-solving or conflict resolution skills. In this way, more open and less hostile communication may help overcome the effects of maternal depressive symptoms including increased arguments, maladaptive cognitions, and impaired problem sovlving by preventing interpersonal conflict, counteracting a mother’s tendency to withdraw, or helping daughters better understand her mother’s behavior (Low & Stocker, 2005; Marchand, Hock, & Widaman, 2002).
Given the myriad impairments associated with maternal depression, it is notable that better communication between mothers and daughters reduced and even buffered youths from risk associated with maternal depressive symptoms. This raises the possibility that these processes may be important targets for treatment aimed at improving youth mental health or preventing the intergenerational transmission of psychopathology. Moreover, communication may be a particularly amenable aspect of the family environment to target, as high-quality communication strategies may be more easily operationalized and taught than other elements of family relationships, such as parental warmth or acceptance. Training in communication strategies may also be less stigmatized than traditional psychotherapy, which may help more African American families engage with an intervention. For these reasons, we interpret the findings that adolescents’ risk for internalizing and externalizing symptoms was fully buffered by high-quality communication as being especially hopeful for families struggling with maternal depression; not only may improved communication reduce parental depressive symptoms, our work suggests that even if interventions are unable to reduce maternal depressive symptoms directly, efforts to improve communication may still ameliorate psychopathology symptom risk for girls, during a developmental period when they are particular vulnerability to mental health problems. That these processes were evident even in a sample of girls seeking mental health services further attests to the clinical relevance of these family features.
Certainly, an exploration of these transmission and buffering processes among treatment-seeking urban African American young women requires careful consideration of the broader structural determinants of health. For example, mother-daughter communication processes may be especially germane for African Americans, where families are the center of activity and the matriarch is the primary head of household (Greene, 2009), due in part to the mass incarceration of African American men (Hagan & Dinovitzer, 1999; D. E. Roberts, 2004). Single mothers often provide the primary support and guidance to their youth. In turn, girls may depend on their single mothers as important and reliable resources amidst the instability of the urban environment (Jarrett, 1994). Consequently, the mother-daughter relationship may be especially important to African American girls (Aronowitz & Morrison-Beedy, 2004) and the ability to communicate effectively and openly within this relationship may be a particularly potent protective force. At the same time, future research is needed to clarify whether these associations generalize to non-African American mothers and daughters, as well as to boys and fathers. With regard to possible gender-related effects, research on early childhood development documents substantial differences in how mothers and fathers talk with their male and female children, including for conversations about psychopathology-relevant topics such as emotions and self-regulation (Adams, Kuebli, Boyle, & Fivush, 1995; Fivush, Marin, McWilliams, & Bohanek, 2009). Conversations between mothers and daughters tend to be more open and intimate than those with fathers or with sons (Noller & Bagi, 1985). Thus, it is possible that mother-son, father-son, or father-daughter dyads would show different transmission and buffering patterns.
Limitations of the current research must be considered in the context of findings. First, the direction of associations between communication and mental health symptoms in mothers and daughters is unclear. For example, it is possible that better youth functioning improves mother-daughter communication, rather than the reverse. Given that the current study drew on only three assessements, we were hesitant to use lagged modeling that would necessitate discarding a third of our data. An important direction for future work would be more intensive, massed assessments of psychopathology and communication to better determine the temporal directionality of associations between study variables. Moreover, although we view communication as a proximal behavior for parent-child functioning, it is likely that patterns of communication draw on a legacy of previous interactions. For this reason, future work examining these associations over periods longer than a year are warranted, as are studies that examine different developmental stages. For example, even within our limited age range, significant associations emerged such that older daughters demonstrated more symptomatology and also had worse communication with their mothers.
Another limitation is the reliance on self-reported mother- and daughter communication quality. Future work would benefit from observational assessments of structured communication tasks or from audio sampling devices to unobtrusively record naturally-occurring conversations in the family home. This would also allow us to consider additional dimensions of communication that may be relevant to youth psychopathology beyond openness and problematic behaviors, and to probe maladaptive forms of communication, such as expressed emotion. A strength and a limitation of the current study is its focus on girls seeking psychological services, thereby limiting generalizability but focusing on a population with clear clinical relevance. Whether children engaged with services, as well as the duration, modality, or quality of treatment, was not standardized across participants. Thus, it is difficult to untangle changes in symptoms or communication from associations with treatment. Similarly, given the considerable barriers to mental health treatment affecting the African American community, our sample of families may have additional characteristics that allowed them to overcome those obstacles and seek out professional support. Lastly, it remains unclear why certain mothers were able to maintain high-quality communication despite high levels of depressive symptoms. Previous research drawing on person-centered analyses have similarly identified groups of parents with high depressive symptoms who nonetheless engage actively with their children (Mendez et al., 2009). Future work should explore the possiblity that other factors, such as greater social support, or lower levels of chronic stress, facilitated this ability.
Despite these limitations, the current study is among the first to demonstrate that high-quality mother-daughter communication may buffer adolescent girls’ from the negative effects of maternal depressive symptoms. Drawing on a vulnerable and understudied population of urban African American adolescent girls, this work suggests that family communication may contribute to important intergenerational psychopathology transmission processes, above and beyond more general features of the family environment.
Acknowledgments
This research was supported by a grant from the National Institute of Mental Health (R01MH065155). We thank the mothers and daughters who participated in the study, and gratefully acknowledge the administrators and clinical staff at the outpatient mental health clinics who worked with us to identify eligible families.
Footnotes
Analyses using daughters’ raw internalizing and externalizing symptom counts as outcome variables, rather than t-scores, produced similar patterns of results.
Contributor Information
Erika M. Manczak, Department of Psychiatry and Behavioral Sciences,Stanford University,401 Quarry Road, Stanford, CA 94304
Geri R. Donenberg, School of Public Health, University of Illinois-Chicago, Chicago, IL
Erin Emerson, School of Public Health, University of Illinois-Chicago, Chicago, IL.
References
- Aben I, Verhey F, Lousberg R, Lodder J, & Honig A (2011). Validity of the Beck Depression Inventory, Hospital Anxiety and Depression Scale, SCL-90, and Hamilton Depression Rating Scale as screening instruments for depression in stroke patients. Psychosomatics, 43(5), 386–393. 10.1176/appi.psy.43.5.386 [DOI] [PubMed] [Google Scholar]
- Achenbach TM, & Rescorla L (2001). Manual for the ASEBA school-age forms & profiles: Child behavior checklist for ages 6–18, teacher’s report form, youth self-report. Assessment. [Google Scholar]
- Adams S, Kuebli J, Boyle P, & Fivush R (1995). Gender differences in parent-child conversations about past emotions: A longitudinal investigation. Sex Roles, 33(5), 309–323. [Google Scholar]
- Aronowitz T, & Morrison-Beedy D (2004). Resilience to risk-taking behaviors in impoverished African American girls: The role of mother-daughter connectedness. Research in Nursing and Health, 27(1), 29–39. 10.1002/nur.20004 [DOI] [PubMed] [Google Scholar]
- Barnes HL, & Olson DH (1982). Parent adolescent communication scale In Olson DH (Ed.), Family inventories: Inventories used in a national survey of families across the family life cycle (pp. 33–48). St. Paul: Family Social Science, University of Minnesota. [Google Scholar]
- Bluestone C, & Tamis-LeMonda CS (1999). Correlates of parenting styles in predominantly working-and middle-class African American mothers. Journal of Marriage and the Family, 61, 881–893. [Google Scholar]
- Bosco GL, Renk K, Dinger TM, Epstein MK, & Phares V (2003). The connections between adolescents’ perceptions of parents, parental psychological symptoms, and adolescent functioning. Journal of Applied Developmental Psychology, 24(2), 179–200. 10.1016/S0193-3973(03)00044-3 [DOI] [Google Scholar]
- Brody GH, & Flor DL (1997). Maternal psychological functioning, family processes, and child adjustment in rural, single-parent, African American families. Developmental Psychology, 33(6), 1000–1011. 10.1037/0012-1649.33.6.1000 [DOI] [PubMed] [Google Scholar]
- Brody GH, Murry VM, McNair L, Chen Y-F, Gibbons F, Gerrard M, & Wills TA (2005). Linking changes in parenting to parent–child relationship quality and youth self‐control: The Strong African American Families Program. Journal of Research …, 15(1), 47–69. [Google Scholar]
- Broidy LM, Tremblay RE, Brame B, Fergusson D, Horwood J, Laird RD, et al. (2003). Developmental trajectories of childhood disruptive behaviors and adolescent delinquency: A six-site, cross-national study. Developmental Psychology, 39(2), 222–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt KB, Van Dulmen MHM, Carlivati J, Egeland B, Alan Sroufe L, Forman DR, et al. (2005). Mediating links between maternal depression and offspring psychopathology: the importance of independent data. Journal of Child Psychology and Psychiatry, 46(5), 490–499. 10.1111/j.1469-7610.2004.00367.x [DOI] [PubMed] [Google Scholar]
- Bynum MS, & Kotchick BA (2006). Mother-adolescent relationship quality and autonomy as predictors of psychosocial adjustment among African American adolescents. Journal of Child and Family Studies, 15(5), 528–541. 10.1007/s10826-006-9035-z [DOI] [Google Scholar]
- Cameron M, & Guterman NB (2007). Diagnosing conduct problems of children and adolescents in residential treatment. Child and Youth Care Forum, 36(1), 1–10. 10.1007/s10566-006-9027-6 [DOI] [Google Scholar]
- Campbell LA, Brown TA, & Grisham JR (2004). The relevance of age of onset to the psychopathology of generalized anxiety disorder. Behavior Therapy, 34, 31–48. [Google Scholar]
- Caron A, Weiss B, Harris V, & Catron T (2006). Parenting behavior dimensions and child psychopathology: Specificity, task dependency, and interactive relations. Journal of Clinical Child and Adolescent Psychology, 35(1), 34–45. 10.1207/s15374424jccp3501_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter JS, & Garber J (2011). Predictors of the first onset of a major depressive episode and changes in depressive symptoms across adolescence: Stress and negative cognitions. Journal of Abnormal Psychology, 120(4), 779–796. 10.1037/a0025441 [DOI] [PubMed] [Google Scholar]
- Cole DA, Martin JM, Peeke L, Henderson A, & Harwell A (1998). Validation of depression and anxiety measures in White and Black youths: Multitrait–multimethod analyses. Psychological Assessment, 10(3), 261–276. [Google Scholar]
- Compas BE, Champion JE, Forehand R, Cole DA, Reeslund KL, Fear J, et al. (2010). Coping and parenting: Mediators of 12-month outcomes of a family group cognitive–behavioral preventive intervention with families of depressed parents. Journal of Consulting and Clinical Psychology, 78(5), 623–634. 10.1037/a0020459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Oppedisano G, Connor JK, Gerhardt CA, Hinden B, Achenbach TM, & Hammen C (1997). Gender differences in depressive symptoms in adolescence: Comparison of national samples of clinically referred and nonreferred youths. Journal of Consulting and Clinical Psychology, 65(4), 617–626. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Pine DS, Hammen CS,MJ,Plotsky PM, Weissman MM, et al. (2002). Development and natural history of mood disorders. Biological Psychiatry, 52, 529–542. [DOI] [PubMed] [Google Scholar]
- Crews F, He J, & Hodge C (2007). Adolescent cortical development: A critical period of vulnerability for addiction. Pharmacology, Biochemistry, and Behavior, 86(2), 189–199. 10.1016/j.pbb.2006.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuffe SP, McKeown RE, Addy CL, & Garrison CZ (2005). Family and psychosocial risk factors in a longitudinal epidemiological study of adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 44(2), 121–129. 10.1097/00004583-200502000-00004 [DOI] [PubMed] [Google Scholar]
- Daughters SB, Reynolds EK, MacPherson L, Kahler CW, Danielson CK, Zvolensky M, & Lejuez CW (2009). Distress tolerance and early adolescent externalizing and internalizing symptoms: The moderating role of gender and ethnicity. Behaviour Research and Therapy, 47(3), 198–205. 10.1016/j.brat.2008.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR (2004). Symptom Checklist-90-R : Administration, Scoring, and Procedures Manual. [Google Scholar]
- Donenberg GR, Emerson E, & Mackesy-Amiti ME (2011). Sexual risk among African American girls: Psychopathology and mother–daughter relationships. Journal of Consulting and Clinical Psychology, 79(2), 153–158. 10.1037/a0022837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Flint K, Harris W, et al. (2012). Youth risk behavior surveillance-United States, 2011. Morbidity and Mortality Weekly Report, 61(4), 1–162. [PubMed] [Google Scholar]
- Elgar FJ, McGrath PJ, Waschbusch DA, Stewart SH, & Curtis LJ (2004). Mutual influences on maternal depression and child adjustment problems. Clinical Psychology Review, 24(4), 441–459. 10.1016/j.cpr.2004.02.002 [DOI] [PubMed] [Google Scholar]
- Fivush R, Marin K, McWilliams K, & Bohanek JG (2009). Family reminiscing style: Parent gender and emotional focus in relation to child well-being. Journal of Cognition and Development, 10(3), 210–235. 10.1080/15248370903155866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, & Heyward D (2011). Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review, 14(1), 1–27. 10.1007/s10567-010-0080 [DOI] [PubMed] [Google Scholar]
- Grant KE, Compas BE, Stuhlmacher AF, Thurm AE, McMahon SD, & Halpert JA (2003). Stressors and child and adolescent psychopathology: Moving from markers to mechanisms of risk. Psychological Bulletin, 129(3), 447–466. 10.1037/0033-2909.129.3.447 [DOI] [PubMed] [Google Scholar]
- Greene BA (2009). Sturdy Bbridges: The role of African-American mothers in the socialization of African-American children. Women & Therapy, 10(1–2), 205–225. 10.1300/J015v10n01_18 [DOI] [Google Scholar]
- Gutman LM, & McLoyd VC (2005). Financial strain, neighborhood stress, parenting behaviors, and adolescent adjustment in urban African American families. Journal of Research on Adolescence, 15(4), 425–449. [Google Scholar]
- Hagan J, & Dinovitzer R (1999). Collateral consequences of imprisonment for children, communities, and prisoners. Crime and Justice, 26, 121–162. 10.2307/1147685?ref=search-gateway:745175532d78341df70c97612c243c53 [DOI] [Google Scholar]
- Hammen C, Shih JH, & Brennan PA (2004). Intergenerational transmission of depression: Test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology, 72(3), 511–522. 10.1037/0022-006X.72.3.511 [DOI] [PubMed] [Google Scholar]
- Hipwell A, Keenan K, Kasza K, Loeber R, Stouthamer-Loeber M, & Bean T (2008). Reciprocal influences between girls’ conduct problems and depression, and parental punishment and warmth: A six year prospective analysis. Journal of Abnormal Child Psychology, 36(5), 663–677. 10.1007/s10802-007-9206-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. (1975) Four factor index of social status. New Haven, CT: Yale University. [Google Scholar]
- Ialongo N, McCreary B, Pearson J, Koenig A, Schmidt N, Poduska J, & Kellam S (2017). Major depressive disorder in a population of urban, African-American young adults: Prevalence, correlates, comorbidity and unmet mental health service need. Journal of Affective Disorders, 79, 127–136. [DOI] [PubMed] [Google Scholar]
- Ivanova MY, Achenbach TM, Rescorla LA, Dumenci L, Almqvist F, Bilenberg N, et al. (2007). The generalizability of the Youth Self-Report syndrome structure in 23 societies. Journal of Consulting and Clinical Psychology, 75(5), 729–738. 10.1037/0022-006X.75.5.729 [DOI] [PubMed] [Google Scholar]
- Jackson JS, Torres M, Caldwell CH, Neighbors H, Nesse R, Taylor R, et al. (2004). The National Survey of American Life: a study of racial, ethnic and cultural influences on mental disorders and mental health. International Journal of Methods in Psychiatric Research, 13(4), 196–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrett RL (1994). Living poor: Family life among single parent, African-American women. Social Problems, 41(1), 30–49. 10.2307/3096840 [DOI] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merkangas K, & Walter E (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Archives of General Psychiatry, 62, 593–602. 10.1016/j.jad.2007.05.007 [DOI] [PubMed] [Google Scholar]
- Koblinsky SA, Kuvalanka KA, & Randolph SM (2006). Social skills and behavior problems of urban, African American preschoolers: Role of parenting practices, family conflict, and maternal depression. American Journal of Orthopsychiatry, 76(4), 554–563. 10.1037/0002-9432.76.4.554 [DOI] [PubMed] [Google Scholar]
- Krishnakumar A, Buehler C, & Barber BK (2004). Cross‐ethnic equivalence of socialization measures in European American and African American Youth. Journal of Marriage and Family, 66, 809–820. [Google Scholar]
- Lahey B, van Hulle C, Singh A, Waldman I, & Rathouz P (2011). Higher-Order genetic and environment structure of prevalent forms of child and adolescent psychopathy. Archives of General Psychiatry, 68(2), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Last C, Perrin S, Hersen M, & Kazdin AE (1992). DSM-III-R anxiety disorders in children: Sociodemographic and clinical characteristics. Journal of the American Academy of Child & Adolescent Psychiatry, 31(6), 1070–1076. 10.1097/00004583-199211000-00012 [DOI] [PubMed] [Google Scholar]
- Leussis MP, & Andersen SL (2007). Is adolescence a sensitive period for depression? Behavioral and neuroanatomical findings from a social stress model. Synapse, 62(1), 22–30. 10.1002/syn.20462 [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Gotlib IH, Lewinsohn M, Seeley JR, & Allen NB (1998). Gender differences in anxiety disorders and anxiety symptoms in adolescents. Journal of Abnormal Psychology, 107(1), 109–117. 10.1037/0021-843X.107.1.109 [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, & Andrews J (1993). Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III—R disorders in high school students. Journal of Abnormal Psychology, 102(1), 133–144. [DOI] [PubMed] [Google Scholar]
- Lim J, Wood BL, & Miller BD (2008). Maternal depression and parenting in relation to child internalizing symptoms and asthma disease activity. Journal of Family Psychology, 22(2), 264–273. 10.1037/0893-3200.22.2.264 [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, & Neuman G (2000). Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review, 20(5), 561–592. [DOI] [PubMed] [Google Scholar]
- Low SM, & Stocker C (2005). Family functioning and children’s adjustment: Associations among parents’ depressed mood, marital hostility, parent-child hostility, and children’s adjustment. Journal of Family Psychology, 19(3), 394–403. 10.1037/0893-3200.19.3.394 [DOI] [PubMed] [Google Scholar]
- Marchand JF, Hock E, & Widaman K (2002). Mutual relations between mothers’ depressive symptoms and hostile-controlling behavior and young children”s externalizing and internalizing behavior problems. Parenting: Science and Practice, 2(4), 335–353. [Google Scholar]
- McLaughlin KA, Hilt LM, & Nolen-Hoeksema S (2007). Racial/ethnic differences in internalizing and externalizing symptoms in adolescents. Journal of Abnormal Child Psychology, 35(5), 801–816. 10.1007/s10802-007-9128-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendez JL, Carpenter JL, LaForett DR, & Cohen JS (2009). Parental engagement and barriers to participation in a community-based preventive intervention. American Journal of Community Psychology, 44(1–2), 1–14. 10.1023/A:1023286210205 [DOI] [PubMed] [Google Scholar]
- Noller P, & Bagi S (1985). Parent—adolescent communication. Journal of Adolescence, 8, 125–144. [DOI] [PubMed] [Google Scholar]
- Pittman LD, & Lansdale PC (2001). African American adolescent girls in impoverished communities: Parenting style and adolescent outcomes. Journal of Research on Adolescence, 11(2), 199–224. [Google Scholar]
- Roberts DE (2004). The social and moral cost of mass incarceration in African American communities. Stanford Law Review, 56(5), 1271–1305. 10.2307/40040178?ref=search-gateway:1d4a6ea73379cb14bf22938c01318d98 [DOI] [Google Scholar]
- Roberts RE, Attkisson CC, & Rosenblatt A (1998). Prevalence of psychopathology among children and adolescents. American Journal of Psychiatry, 155(6), 715–725. [DOI] [PubMed] [Google Scholar]
- Rodriguez EM, Nichols SR, Javdani S, Emerson E, & Donenberg GR (2013). Economic hardship, parent positive communication and mental health in urban adolescents seeking outpatient psychiatric care. Journal of Child and Family Studies, 24(3), 617–627. 10.1007/s10826-013-9872-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saluja G, Iachan R, Scheidt PC, Overpeck M, Sun W, & Giedd JN (2004). Prevalence of and risk factors for depressive symptoms among young adolescents. Archives of Pediatric and Adolescent Medicine, 158, 760–765. [DOI] [PubMed] [Google Scholar]
- Schaefer ES (1965). Children’s reports of parental behavior: An inventory. Child Development, 414–424. [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucus C, Dulcan M, & Schwab-Stone M (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV). Journal of the American Academy of Child & Adolescent Psychiatry, 39(1), 28–38. 10.1097/00004583-200001000-00014 [DOI] [PubMed] [Google Scholar]
- Silberg JL, Maes H, & Eaves LJ (2010). Genetic and environmental influences on the transmission of parental depression to children’s depression and conduct disturbance: An extended Children of Twins study. Journal of Child Psychology and Psychiatry, 51(6), 734–744. 10.1111/j.1469-7610.2010.02205.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh AL, D’Onofrio BM, Slutske WS, Turkheimer E, Emery RE, Harden KP, et al. (2010). Parental depression and offspring psychopathology: A Children of Twins study. Psychological Medicine, 41(07), 1385–1395. 10.1017/S0033291710002059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smetana JG, Crean HF, & Daddis C (2002). Family processes and problem behaviors in middle-class African American adolescents. Journal of Research on Adolescence, 12(2), 275–304. 10.1111/1532-7795.00034 [DOI] [Google Scholar]
- Taylor RD, Seaton E, & Dominguez A (2008). Kinship support, family relations, and psychological adjustment among low‐income African American mothers and adolescents. Journal of Research on Adolescence, 18(1), 1–22. [Google Scholar]
- Tully EC, Iacono WG, & McGue M (2008). An adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. American Journal of Psychiatry, 165(9), 1148–1154. 10.1176/appi.ajp.2008.07091438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge JM, & Nolen-Hoeksema S (2002). Age, gender, race, socioeconomic status, and birth cohort difference on the children’s depression inventory: A meta-analysis. Journal of Abnormal Psychology, 111(4), 578–588. 10.1037//0021-843X.111.4.578 [DOI] [PubMed] [Google Scholar]
- Waller R, Gardner F, Shaw DS, Dishion TJ, Wilson MN, & Hyde LW (2014). Callous-unemotional behavior and early-childhood onset of behavior problems: The role of parental harshness and warmth. Journal of Clinical Child and Adolescent Psychology, 44(4), 655–667. 10.1037/0022-006X.65.2.292.b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A, & Sherbourne C (2001). Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. American Journal of Psychiatry, 158, 2027–2032. [DOI] [PubMed] [Google Scholar]
- Wills TA, Gibbons FX, Gerrard M, Murry VM, & Brody GH (2003). Family communication and religiosity related to substance use and sexual behavior in early adolescence: A test for pathways through self-control and prototype perceptions. Psychology of Addictive Behaviors, 17(4), 312–323. 10.1037/0893-164X.17.4.312 [DOI] [PubMed] [Google Scholar]


