Abstract
After remaining stable from 2010 to 2014, the rate of cocaine-involved overdose death increased sharply from 2015 to 2016. This study aims to determine the contribution of opioids, and fentanyl in particular, to the increase in cocaine-involved overdose death from 2015 to 2016. Using New York City death certificate data linked to medical examiner toxicology data, we identified all overdose deaths where post-mortem toxicology results were positive for cocaine from 2010 to 2016. We analyzed cocaine-involved overdose deaths by co-occurring substances. Age-adjusted rates per 100,000 residents were calculated for 6-month intervals from 2010 to 2016. Data suggest that increased deaths involving opioids, specifically fentanyl, accounted for most of the increase in cocaine-involved deaths from 2015 to 2016.
Keywords: Overdose, Fentanyl, Opioid, Cocaine, Heroin
Introduction
Fentanyl, a short-acting opioid with a potency 50 to 100 times stronger than morphine, is associated with an increased risk of fatal overdose [1]. Beginning in 2015, the rate of fatal overdose involving fentanyl began to rise in New York City [2]. Recent increases in drug overdose deaths in jurisdictions across the country have been attributed to the increased presence of non-pharmaceutical fentanyl, a drug manufactured in clandestine laboratories. Non-pharmaceutical fentanyl has been found mixed into heroin, cocaine, and illicitly produced pills, such as opioid analgesics and benzodiazepines [3, 4]. Thus recently, several cities across the USA reported outbreaks of overdose deaths involving fentanyl combined with heroin or cocaine [3, 5–7].
In New York City, the increased involvement of fentanyl in drug overdose deaths coincided with a dramatic increase in the total number of overdose deaths. Prior to 2015, fentanyl was involved in fewer than 5% of all overdose deaths annually. However, during 2015, the percentage of overdose deaths involving fentanyl increased to 16%, and by the end of 2016, fentanyl was involved in approximately half of all overdoses in New York City [2]. The increased involvement of fentanyl coincided with a 51% increase in the rate of overdose death, from 13.7 per 100,000 in 2015 to 20.7 per 100,000 in 2016, the largest single-year increase on record [2].
Data from the National Vital Statistics System (NVSS) identified an increase in the rate of overdose death in the USA involving cocaine and any opioid from 2000 to 2015 [8]. NVSS relies on death certificate data to report drug-poisoning deaths (overdose) and, during the study period, 20 to 25% of death certificates were missing drug-specific information [8]. Thus, death certificate data underreport the number of overdose deaths involving cocaine and specific drug combinations such as cocaine and opioids.
In New York City, the Department of Health and Mental Hygiene (DOHMH) links death certificates with medical examiner post-mortem toxicology results for all overdose deaths. Thus, by not relying solely on death certificate data, New York City avoids underreporting drug specificity and reports all drugs involved in overdose deaths. This study aimed to quantify two aspects of cocaine-involved overdose in New York City: (1) the extent to which fentanyl drove the increase in cocaine-involved overdose deaths from 2015 to 2016, and (2) the contribution of cocaine-fentanyl without heroin deaths, as a proxy for deaths that may have been due to a cocaine product containing fentanyl.
Materials and Methods
Data for this study were derived from death certificates obtained from the New York City Bureau of Vital Statistics and toxicology results from the New York City Office of the Chief Medical Examiner.
We define overdose deaths as deaths where the medical examiner certified the cause of death as an unintentional drug poisoning, the manner of death was accidental, and the underlying or multiple cause code was assigned an ICD-10 code of X40–X44, F11–F16, or F18–F19 (excluding F-codes with 0.2 or 0.6 third digit). The excluded F-codes indicate substance dependence and amnesic syndrome, respectively, and on their own, are not specific to drug-overdose deaths. Toxicology results were abstracted for every confirmed unintentional drug poisoning death from 2010 to 2016. We report drug-involvement based on the detection of substances in post-mortem toxicology testing.
Using toxicology data, we identified all overdose deaths where cocaine was detected. To assess the extent to which the increase in cocaine-involved overdose deaths were driven by increases in opioid-involvement, we first classified cocaine-involved overdose deaths into one of two categories: (1) cocaine with opioids; (2) cocaine without opioids. To assess the extent to which fentanyl, in particular, contributed to increased cocaine-involved overdose deaths, we then identified all drug overdose deaths involving cocaine and fentanyl. Lastly, to understand if a fentanyl-contaminated cocaine supply contributed to increased overdose deaths, we identified overdose deaths involving cocaine and fentanyl, without heroin because we assumed that when heroin and fentanyl were both present then the fentanyl was likely to have been mixed into the heroin product. All categories could include other substances unless otherwise specified. Counts, age-adjusted rates, and standard errors were calculated for each 6-month interval between 2010 and 2016. Age adjustment was performed using the 2000 US standard population and DOHMH population estimates, modified from US Census Bureau intercensal population estimates 2000 to 2016, updated September 2017. Given the small cell sizes, we used the gamma method to calculate the 95% confidence intervals [9]. Changes in rates were identified by comparing the confidence intervals; non-overlapping confidence intervals were considered statistically significant [9]. We graphed each of the five cocaine patterns (cocaine-involved, cocaine and any opioid, cocaine without any opioid, cocaine and fentanyl, and cocaine and fentanyl without heroin) for visual comparisons.
Using the 2015 and 2016 data, we compared the increase in the rate of cocaine- and fentanyl-involved overdose deaths to the increase in the rate of all cocaine-involved overdose deaths (the percentage of the absolute rate increase), representing the contribution of fentanyl to the increase in cocaine-involved overdose deaths.
This study was considered routine public health surveillance of drug overdose deaths and was not subject to institutional board review.
Results
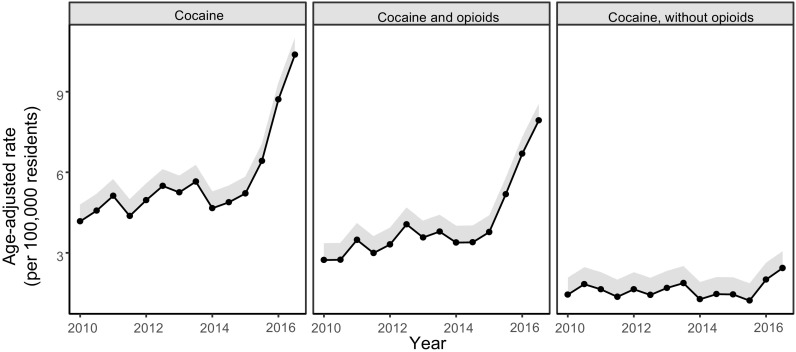
Data show two distinct periods in cocaine-involved overdoses (Figs. 1 and 2). From 2010 to 2014, rates of cocaine-involved overdoses remained stable; however, from 2015 to 2016, the rate of cocaine-involved overdoses doubled from 5.2 per 100,000 residents (95% CI = 5.2, 5.8) during the first half of 2015 to 10.4 per 100,000 residents (95% CI = 10.4, 11.0) during the last half of 2016 (Table 1).
Fig. 1.
Age-adjusted rate and 95% confidence interval of unintentional drug-poisoning death, by selected substances involved, New York City, 2010–2016.
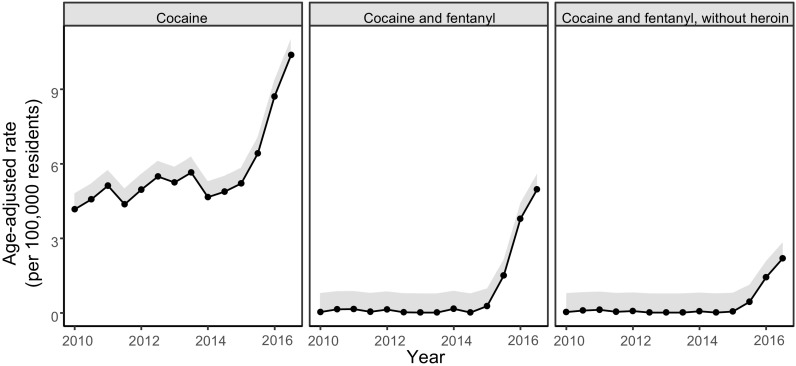
Fig. 2.
Age-adjusted rate and 95% confidence interval of unintentional drug-poisoning death, by selected substances involved, New York City, 2010–2016.
Table 1.
Number and rate of unintentional drug-poisoning death, by selected substances involved, New York City, 2010–2016
| Cocaine | Cocaine, any opioid | Cocaine, without opioids | Cocaine and fentanyl | Cocaine and fentanyl, without heroin | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Rate (95% CI) | N | Rate (95% CI) | N | Rate (95% CI) | N | Rate (95% CI) | N | Rate (95% CI) | ||
| 2010 | Jan–Jun | 136 | 4.2 (4.2–4.8) | 89 | 2.7 (2.7–3.4) | 47 | 1.4 (1.4–2.1) | 1 | 0.0 (0.0–0.8) | 1 | 0.0 (0.0–0.8) |
| Jul–Dec | 152 | 4.6 (4.6–5.2) | 92 | 2.7 (2.7–3.4) | 60 | 1.8 (1.8–2.5) | 5 | 0.2 (0.2–0.9) | 3 | 0.1 (0.1–0.8) | |
| 2011 | Jan–Jun | 171 | 5.1 (5.1–5.8) | 117 | 3.5 (3.5–4.1) | 54 | 1.6 (1.6–2.3) | 6 | 0.2 (0.2–0.9) | 5 | 0.1 (0.1–0.9) |
| Jul–Dec | 148 | 4.4 (4.4–5.0) | 102 | 3.0 (3.0–3.6) | 46 | 1.4 (1.4–2.0) | 2 | 0.1 (0.1–0.8) | 2 | 0.1 (0.1–0.8) | |
| 2012 | Jan–Jun | 167 | 5.0 (5.0–5.6) | 112 | 3.3 (3.3–3.9) | 55 | 1.6 (1.6–2.3) | 5 | 0.1 (0.1–0.9) | 3 | 0.1 (0.1–0.8) |
| Jul–Dec | 181 | 5.5 (5.5–6.1) | 133 | 4.1 (4.1–4.7) | 48 | 1.4 (1.4–2.1) | 1 | 0.0 (0.0–0.8) | 0 | 0.0 (0.0–0.8) | |
| 2013 | Jan–Jun | 173 | 5.3 (5.3–5.9) | 117 | 3.6 (3.6–4.2) | 56 | 1.7 (1.7–2.3) | 1 | 0.0 (0.0–0.8) | 0 | 0.0 (0.0–0.8) |
| Jul–Dec | 191 | 5.7 (5.7–6.3) | 128 | 3.8 (3.8–4.4) | 63 | 1.9 (1.9–2.5) | 1 | 0.0 (0.0–0.8) | 1 | 0.0 (0.0–0.8) | |
| 2014 | Jan–Jun | 161 | 4.7 (4.7–5.3) | 117 | 3.4 (3.4–4.0) | 44 | 1.3 (1.3–1.9) | 6 | 0.2 (0.2–0.9) | 3 | 0.1 (0.1–0.8) |
| Jul–Dec | 165 | 4.9 (4.9–5.5) | 115 | 3.4 (3.4–4.0) | 50 | 1.5 (1.5–2.1) | 1 | 0.0 (0.0–0.8) | 0 | 0.0 (0.0–0.8) | |
| 2015 | Jan–Jun | 180 | 5.2 (5.2–5.8) | 130 | 3.8 (3.8–4.4) | 50 | 1.5 (1.5–2.1) | 11 | 0.3 (0.3–1.0) | 2 | 0.1 (0.1–0.8) |
| Jul–Dec | 223 | 6.4 (6.4–7.1) | 180 | 5.2 (5.2–5.8) | 43 | 1.2 (1.2–1.9) | 54 | 1.5 (1.5–2.2) | 15 | 0.5 (0.5–1.1) | |
| 2016 | Jan–Jun | 296 | 8.7 (8.7–9.3) | 226 | 6.7 (6.7–7.3) | 70 | 2.0 (2.0–2.6) | 124 | 3.8 (3.8–4.4) | 48 | 1.4 (1.4–2.1) |
| Jul–Dec | 359 | 10.4 (10.4–11) | 274 | 7.9 (7.9–8.6) | 85 | 2.4 (2.4–3.1) | 171 | 5.0 (5.0–5.6) | 74 | 2.2 (2.2–2.8) | |
Other substances may be present unless otherwise specified
The rate of overdose death involving cocaine and opioids increased from 3.8 per 100,000 residents (95% CI = 3.8, 4.4) during the first half of 2015 to 7.9 (95% CI = 7.9, 8.6) during the second half of 2016. The rates of overdose death involving cocaine, without opioids, also increased during this period from 1.5 per 100,000 residents (95% CI = 1.5, 2.1) to 2.4 per 100,000 (95% CI = 2.4, 3.1).
The rates of overdose death involving cocaine and fentanyl increased from 0.3 per 100,000 residents (95% CI = 0.3, 1.0) during the first half of 2015 to 5.0 per 100,000 residents (95% CI = 5.0, 5.6) during the last half of 2016.
The rates of overdose death involving cocaine and fentanyl, without heroin, also increased significantly during this period (Table 1). During the first half of 2015, there were only two fatal drug overdose deaths involving cocaine and fentanyl without heroin (0.1 per 100,000 residents, 95% CI = 0.1, 0.8); during the second half of 2016, there were 74 fatal overdoses, accounting for a rate of 2.2 per 100,000 residents (95% CI = 2.2, 2.8).
The increase in the rate of overdose death involving both cocaine and fentanyl (+ 4.7 per 100,000) accounted for 90% of the overall increase in the rate of overdose death involving cocaine (+ 5.2 per 100,000) from 2015 to 2016. Increases in the rate of overdose death involving both cocaine and fentanyl, without heroin (+ 2.1 per 100,000) accounted for 40% of the overall increase in the rate of overdose death involving cocaine (+ 5.2 per 100,000) from 2015 to 2016. During the second half of 2016, deaths involving cocaine and fentanyl, excluding heroin, accounted for nearly half (43%, 74 of 171) of the deaths involving cocaine and fentanyl.
Discussion
While overdose deaths almost always involve polysubstance use, in New York City increased opioid involvement, particularly increased involvement of fentanyl, accounted for most of the increase in cocaine-involved overdose deaths from 2015 to 2016. This suggests that the increased presence of fentanyl in the illicit drug supply, including the cocaine supply, is driving these increases. Our findings also identified an increase in overdose deaths involving cocaine and fentanyl without heroin; thus, they suggest the possibility that at least some of the deaths resulted from the presence of fentanyl in cocaine products.
Although our analysis is strengthened by the use of toxicology data, we nevertheless are precluded from drawing definitive conclusions about the decedents’ intention to use a particular substance, nor can we confirm if specific substances were used in combination or sequentially. As a proxy for deaths where fentanyl might have been present in the cocaine product, we analyzed overdose deaths involving cocaine and fentanyl, but without heroin. This proxy might have misclassified deaths where the decedent used both heroin and cocaine products containing fentanyl (under-counted) or deaths where the decedent used both cocaine and fentanyl products without heroin (over-counted). Despite these limitations, the data suggest individuals who use cocaine in New York City are at an increased risk of a fatal overdose due to the presence of fentanyl in the drug supply. Our hypothesis that increased risk is due to the presence of fentanyl in both the heroin and cocaine supply is further supported by New York City law enforcement seizure data that confirmed the presence of fentanyl in cocaine products as well as in heroin products [10].
Our analysis extends and confirms national data that shows a steady increase in the rate of overdose death involving cocaine and any opioid from 2000 to 2015. Notably, rates of cocaine-involved overdose death in New York City, confirmed by toxicology data, were much higher than national rates reported using death certificate data.
One major limitation of this study is the discontinuation of routine testing for fentanyl in suspected overdose deaths by the Office of the Chief Medical Examiner during 2013. Universal testing resumed on July 1, 2016. The lack of universal testing might have resulted in our misclassifying some deaths that involved fentanyl as non-fentanyl involved. Thus, we might have underestimated the involvement of fentanyl in overdose deaths during that period.
The fentanyl contamination of the cocaine supply presents three public health challenges. First, people who use cocaine but not opioids are disproportionately susceptible to the risks associated with fentanyl. Although fentanyl increases overdose risk for all people who use drugs, individuals who do not use opioids lack tolerance, placing them at particularly high risk of fatal overdose [8].
Second, people who use cocaine but not opioids are generally not targeted by opioid-focused prevention strategies. People who do not use opioids are unlikely to have access to naloxone, the opioid overdose reversal medicine. In New York City, the majority of overdose prevention training and naloxone distribution is done by syringe exchange programs and substance use disorder treatment, particularly opioid treatment programs.
Third, people who use cocaine intermittently might not be reached by any drug-focused prevention strategies or messages. Since physical dependence is less pronounced with cocaine compared to opioids, intermittent use is likely more common among people who use cocaine only compared to people who use opioids [11], and therefore intermittent users may not intersect with services that specifically target people who use drugs. People who use drugs intermittently might benefit from more targeted outreach.
To reduce fatal overdose rates, overdose prevention interventions—including access to naloxone and information about fentanyl—should also target people who use cocaine. But, effective strategies to reach such individuals are not known. One potential strategy is to provide such information through public awareness campaigns in bar settings. In a study of powder cocaine use among gay and bisexual men in New York City, bars were the most frequently endorsed venue for cocaine use (78.9%) followed by dance clubs (72.1%) [12]. A public awareness campaign in bars is currently underway in New York City, but its effectiveness has not yet been evaluated [13, 14].
Conclusion
After remaining relatively stable, rates of cocaine-involved overdose sharply increased in 2016. Data suggest that this increase is driven by the presence of fentanyl in the New York City drug supply. While the presence of fentanyl in heroin confers additional risk to people using opioids, the presence of fentanyl in cocaine poses a dramatically heightened risk of overdose among individuals who use only cocaine and lack opioid tolerance. Therefore, harm reduction efforts should be expanded to include targeted outreach, education, and overdose prevention messages for people who use cocaine but are opioid naïve.
Acknowledgements
The authors would like to thank Bennett Allen for his editorial assistance.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This research was conducted with the support of the New York City Department of Health and Mental Hygiene. At the time the study was conducted, all authors were employees of the New York City Department of Health and Mental Hygiene. Authorization to submit and publish the enclosed manuscript was received from the institution.
Authors’ Contributions
Michelle Nolan and Sindhu Shamasunder had full access to study data and take responsibility for the accuracy of the data analysis. Michelle Nolan, Denise Paone, and Hillary Kunins were responsible for study concept and design and critical revision of the manuscript. Denise Paone, Michelle Nolan, Hillary Kunins, and Sindhu Shamasunder were responsible for the analysis and interpretation of the data. Michelle Nolan, Cody Colon-Berezin, and Sindhu Shamasunder contributed to manuscript drafting. All authors approved the final article as submitted on 31 May 2018.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Woodhead K, Wicker P. A textbook of perioperative care. Edinburgh; Elsevier/Churchill Livingstone; 2005.
- 2.Paone D, Nolan ML, Tuazon E, Blachman-Forshay J. Unintentional Drug poisoning (overdose) deaths in New York City, 2000–2016. New York: New York City Department of Health and Mental Hygiene; 2017. [Google Scholar]
- 3.Peterson AB, Gladden RM, Delcher C, et al. Increases in fentanyl-related overdose deaths - Florida and Ohio, 2013–2015. MMWR Morb Mortal Wkly Rep. 2016;65(33):844–849. doi: 10.15585/mmwr.mm6533a3. [DOI] [PubMed] [Google Scholar]
- 4.CDC . Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities. Atlanta: CDC; 2015. [Google Scholar]
- 5.Westley CH. Fact sheet: fentanyl-laced heroin and cocaine. In: Substance Abuse and Mental Health Services Administration, ed. Fact Sheet: SAMHSA, Rockville; 2013. Advailable online https://www.samhsa.gov/sites/default/files/programs_campaigns/medication_assisted/dear_colleague_letters/2013-colleague-letter-fentanyl-analogues.pdf. Accessed 25 May 2018
- 6.Somerville NJ, O'Donnell J, Gladden RM, et al. Characteristics of fentanyl overdose - Massachusetts, 2014–2016. MMWR Morb Mortal Wkly Rep. 2017;66(14):382–386. doi: 10.15585/mmwr.mm6614a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.CDC Acetyl fentanyl overdose fatalities--Rhode Island, March–May 2013. MMWR Morb Mortal Wkly Rep. 2013;62(34):703–704. [PMC free article] [PubMed] [Google Scholar]
- 8.Jones CM, Baldwin GT, Compton WM. Recent increases in cocaine-related overdose deaths and the role of opioids. Am J Public Health. 2017;107(3):430–432. doi: 10.2105/AJPH.2016.303627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fay MP, Feuer EJ. Confidence intervals for directly standardized rates: a method based on the gamma distribution. Stat Med. 1997;16(7):791–801. doi: 10.1002/(SICI)1097-0258(19970415)16:7<791::AID-SIM500>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 10.New York City Department of Health and Mental Hygiene. Presence of fentanyl in cocaine contributing to increase in drug overdose deaths; Health Advisory # 10, New York; 2017. Advailable online https://www1.nyc.gov/assets/doh/downloads/pdf/han/advisory/fentanyl-advisory10.pdf. Accessed 25 May 2018
- 11.van Amsterdam J, Opperhuizen A, Koeter M, van den Brink W. Ranking the harm of alcohol, tobacco and illicit drugs for the individual and the population. Eur Addict Res. 2010;16(4):202–207. doi: 10.1159/000317249. [DOI] [PubMed] [Google Scholar]
- 12.Palamar JJ, Mukherjee PP, Halkitis PN. A longitudinal investigation of powder cocaine use among club-drug using gay and bisexual men. J Stud Alcohol Drugs. 2008;69(6):806–813. doi: 10.15288/jsad.2008.69.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spectrum News . Health department warns NYers about cocaine laced with fentanyl in the city. New York: NY1; 2018. [Google Scholar]
- 14.Flynn G. It’s not rum and coke-but fentanyl and coke on L.E.S. New York: The Villager; 2018. [Google Scholar]