Abstract
Context:
Ankle syndesmotic injuries present a significant challenge for athletes due to prolonged disability and recovery periods. The optimal management of these injuries and rates of return to sport in athletes remains unclear.
Objective:
The purpose of this study was to evaluate return to sport for athletes after ankle syndesmotic injuries.
Data Source:
The electronic databases MEDLINE, EMBASE, and PubMed were searched for relevant studies from database inception to January 15, 2017, and pertinent data were abstracted.
Study Selection:
Only studies reporting return-to-sport rates after ankle syndesmotic injuries were included.
Study Design:
Systematic review.
Level of Evidence:
Level 4.
Data Extraction:
Two reviewers extracted data from the included studies, which were stored in a standardized collection form (Microsoft Excel). Recorded data included demographics (eg, author, year of publication, study design), descriptive statistics (eg, patient age, percentage male, number of athletes, sample size), and outcomes (eg, time to return to sport, proportion of those who returned to sport, the self-reported questionnaire the Olerud-Molander Ankle Score).
Results:
A total of 10 studies and 312 patients with ankle syndesmotic injuries were included in this systematic review. The rate of return to preinjury or any injury level of sport after ankle syndesmotic injuries was 93.8% ± 1.2% and 97.6% ± 1.5%, respectively, for the corresponding 7 and 3 studies that reported this characteristic. The mean time to return to sport was 46.4 days (range, 15.4-70 days), with 55.2 ± 15.8 and 41.7 ± 9.8 days for operative and nonoperative management, respectively.
Conclusion:
This systematic review found a high rate of return to any as well as preinjury level of sport after ankle syndesmotic injury in both operative and nonoperative treatment groups. However, further high-level studies are required to compare operative and nonoperative treatment groups associated with return to sport after ankle syndesmotic injury.
Keywords: ankle syndesmotic injury, high ankle sprain, return to sport
The ankle syndesmosis comprises the interosseous ligament (IOL), the anterior inferior tibiofibular ligament (AITFL), posterior inferior tibiofibular ligament (PITFL), and the transverse ligament.14 The ankle syndesmosis is crucial in maintaining the structural integrity of the joint. Syndesmotic disruption typically occurs at the ankle after external rotation or dorsiflexion injuries.7,14 Athletes aged 18 to 34 years are at the greatest risk for sustaining an ankle syndesmotic injury, with the incidence falling between 10% and 20%, and increasing for those who participate in contact sports, such as football and hockey.7 Syndesmotic injuries present a significant challenge for athletes due to prolonged disability, recovery periods, and uncertainty regarding the ideal treatment approach.8,12 Furthermore, malreduction of the ankle syndesmosis is of particular concern, and it is commonly underrecognized and associated with poor outcomes.2,14
Treatment of syndesmotic sprains varies and depends on several factors, including injury severity.3,12 The West Point Ankle Grading System is used to categorize the degree of ankle sprains to aid in management.3 Grade I ankle syndesmotic injuries occur with a sprain to the AITFL and are generally treated nonoperatively due to relative stability.3 Grade II injuries, whereby rotational forces tear the AITFL and the IOL,2,14 may necessitate stabilization if the ligamentous injury is severe enough.3 Grade II injuries pose a particular challange to clinicans when determining operative or nonoperative treatment. This is mostly because of inadequate diagnostic methods to differentiate a stable and unstable syndesmosis. Grade III injuries require operative management, as they involve complete disruption of the ankle syndesmosis and present with syndesmotic instability and diastasis.3,20 They involve complete injury to the lateral ligaments, including the AITFL, IOL, and PITFL, as well as deltoid ligament avulsion medially.2 Magnetic resonance imaging (MRI) is used to image structures of the syndesmosis and is therefore useful in diagnosing syndesmotic injuries.18 In contrast to confirmation of syndesmotic injuries by ankle arthroscopy, studies have indicated that MRI has higher sensitivity and specificity values, indicating greater accuracy.18 The challenge remains in adequate recognition of the degree of disruption, particularly with standard, static radiographic imaging. This has likely contributed to the variation in treatment strategies that has been described across all grades of syndesmotic injuries.12,18 For those with an unstable ankle syndesmosis, the most common surgical treatment has been trans-syndesmotic screw fixation; however, this has been associated with complications such as malreduction or hardware failure resulting in secondary postoperative syndesmotic diastasis necessitating hardware removal. More recent surgical treatments such as suture button with adjustable loop fixation have demonstrated potentially more favorable clinical outcomes, with lower rates of malreduction and reoperation.4 Compared with lateral ankle sprains, syndesmotic injuries require longer rehabilitation periods, with a minimum of 6 to 8 weeks for recovery.2,12,15
For many athletes who suffer these injuries, determining an appropriate and safe return to sport is fundamental to ensuring a complete recovery. This review aims to systematically assess return-to-sport rates and associated performance in athletes who experience ankle syndesmotic injuries.
Methods
Search Strategy and Eligibility
PubMed, EMBASE, and MEDLINE were searched for literature on return to sport after ankle syndesmotic injuries from data inception to January 15, 2017. The search terms included ankle, syndesmosis, and return to play as well as additional similar phrases related to the topic (see Table A1 in the Appendix, available in the online version of this article). Inclusion criteria consisted of (1) all levels of evidence, (2) athletes with ankle syndesmotic injury (pure ligamentous injury), (3) reporting of rate or time to return to sport, (4) studies published in English in a peer-reviewed journal, and (5) studies on humans. Exclusion criteria were (1) lateral ankle sprains; (2) reviews, conference proceedings, opinion pieces, or letters to the editor; (3) case reports; and (4) studies not published in English.
Screening
In accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses), screening was done in duplicate by 2 independent reviewers for both title and abstract as well as full-text screening stages. The reviewers were blinded to study author and publication origin. Inconsistencies that arose during the title and abstract stage were resolved by automatically including them in the full-text stage. Discrepancies were resolved through discussion and agreement between both reviewers. Where agreement was not reached, a third blinded reviewer assisted in the decision-making process.
Data Extraction
Two reviewers extracted data from the included studies, which were stored in a standardized collection form (Microsoft Excel). Recorded data included demographics (eg, author, year of publication, study design), descriptive statistics (eg, patient age, percentage male, number of athletes, sample size), and outcomes (eg, time to return to sport, proportion of those who returned to sport, the self-reported questionnaire the Olerud-Molander Ankle Score [OMAS]).
Statistical Analysis
Two reviewers used the Methodological Index for Non-Randomized Studies (MINORS) appraisal tool to evaluate quality of included studies.17 A score of 0, 1, or 2 was given for each of the 8 categories of the tool, with a maximum of 16 for included noncomparative studies. A score of 0 to 6 indicated very low quality of evidence, 7 to 10 indicated low quality, 10 to 14 indicated fair quality, and >16 good quality. The kappa (κ) statistic was used to assess interreviewer agreement. Additionally, the intraclass correlation coefficient (ICC) was calculated for the quality assessment using the MINORS criteria.17 Agreement was characterized as follows: κ/ICC of 0.81 to 0.99 as excellent agreement, κ/ICC of 0.61 to 0.80 as substantial agreement, κ/ICC of 0.41 to 0.60 as moderate agreement, κ/ICC of 0.21 to 0.40 as fair agreement, and κ/ICC value of 0.20 or less as slight agreement.
Results
Eligibility
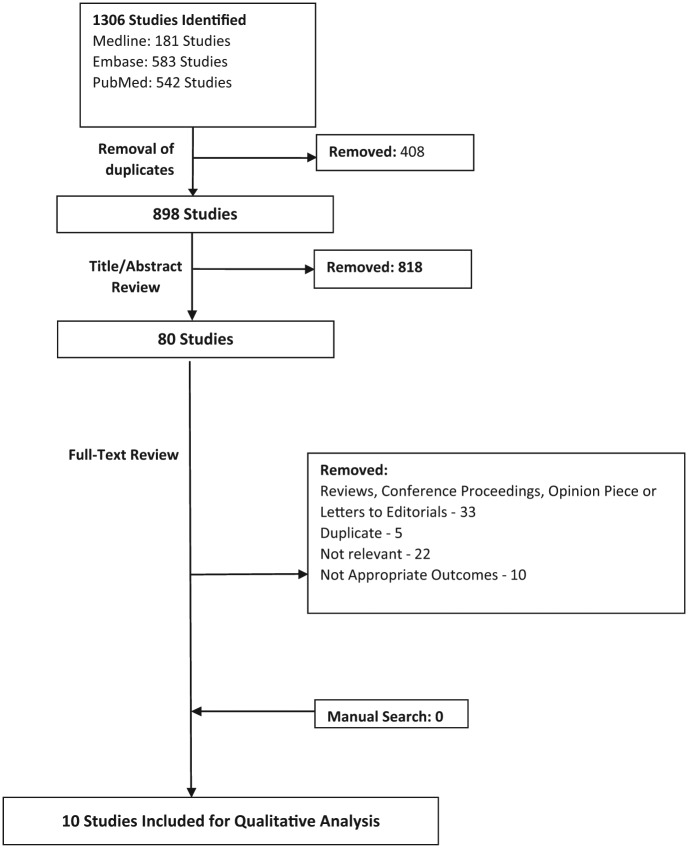
The initial search generated 1306 studies, of which 10 full-text articles met the inclusion criteria (Figure 1). There was substantial agreement between reviewers at the title screen (κ = 0.792), and excellent agreement at the abstract and full-text screens (κ = 0.892 and κ = 0.910, respectively).
Figure 1.
Outline of systematic search strategy used.
Study Characteristics
Included studies were conducted between 1998 and 2016, of which 5 (50%) were published in the past 5 years. A total of 312 participants had syndesmotic injuries; 38.8% (121/312) were athletes playing sport at an amateur level, and 40.1% (125/312) played sport at a professional level. The level of play for the remaining 66 patients was not specified. The most commonly played sport at the amateur and professional levels was American football (n = 10; 8.3%) and rugby (n = 40; 30.1%), respectively. Grade I ankle syndesmotic injuries occurred in 8.0% (25/312) of athletes, grade II injuries occurred in 28.8% (90/312) of athletes, and grade III injuries occurred in 2.2% (7/312) of athletes. The mean total sample size per included study was 33.5 patients (range, 5-126 patients). Of the studies that reported patient sex and age characteristics, the average proportion of males was 79.3%, with a mean age of 26.7 ± 8.3 years. The mean follow-up across the 5 studies that reported on it was 34.1 months (Table 1).
Table 1.
Characteristics of included studies
| Primary Author | Year | Study Design (Level of Evidence) | Total Sample Size, n | Syndesmotic Injuries, n | % Male | Mean Age (Range), y | Mean Follow-up, mo | Consensus MINORS Score a |
|---|---|---|---|---|---|---|---|---|
| Steinmetz | 2016 | Retrospective cohort (4) | 126 | 126 | 61 | 45 ± 15.7 (16-86.5) | 70.8 ± 5.9 | 10 |
| Calder | 2016 | Prospective cohort (2) | 64 | 64 | NR | NR | 37 (range 24-66) | 13 |
| Sman | 2014 | Prospective cohort (2) | 32 | 32 | 90.6 | 21.4 ± 3.3 | NR | 9 |
| Osbahr | 2013 | Retrospective cohort (3) | 36 | 36 | NR | NR | NR | 8 |
| Porter | 2014 | Case series (4) | 27 | 27 | 70.4 | 18.1 ± 5.9 (12-37) | 28 (range 12-43) | 11 |
| Taylor | 2007 | Case series (4) | 6 | 6 | 100 | 19 | 34.3 | 12 |
| Flik | 2005 | Prospective cohort (3) | 113 | 5 | 100 | NR | NR | 8 |
| Wright | 2004 | Retrospective cohort (4) | 14 | 14 | NR | NR | NR | 8 |
| Gerber | 1998 | Prospective cohort (2) | 16 | 16 | NR | 20 (17-24) | 3.75 (range 1.5-6) | 8 |
| Ogilvie-Harris | 1997 | Case series (4) | 100 | 7 | 54 | 29 (17-51) | 33 | 10 |
MINORS, Methodological Index for Non-Randomized Studies; NR, not reported.
Score range is 0 to 16 for noncomparative studies.
Study Quality
All studies in this systematic review were nonrandomized in design. The studies were level 4 (n = 5), level 3 (n = 2), and level 2 (n = 3) evidence (Table 2), and the remaining studies included case series. There was a substantial level of agreement among quality assessment scores using the MINORS criteria (ICC, 0.932). The mean MINORS score was 9.7 ± 2.0 for noncomparative studies, which indicates low quality of evidence for nonrandomized studies. Overall, there was a high rate of prospective collection of data. However, few studies had a clear stated aim and appropriate endpoints to the aim of the study. Additionally, studies lacked reporting of whether an unbiased assessment of study outcomes was performed, appropriate follow-up period, and prospective calculation of study size.
Table 2.
Return-to-sport rates and management type
| Primary Author | Year | Sample Size, n | Returned to Sport at Any Level, % | Returned to Sport at Preinjury Level, % | Management Type |
|---|---|---|---|---|---|
| Steinmetz | 2016 | 126 | NR | 83 | Operative |
| Calder | 2016 | 64 | NR | 100 | Operative (grade IIb, n = 38) and nonoperative (grade IIa, n = 26) |
| Sman | 2014 | 32 | NR | NR | Nonoperative |
| Osbahr | 2013 | 36 | 100 | NR | Nonoperative |
| Porter | 2014 | 27 | NR | 96.3 | Operative |
| Taylor | 2007 | 6 | NR | 100 | Operative |
| Flik | 2005 | 5 | NR | 100 | NR |
| Wright | 2004 | 14 | 93 | NR | Operative (n = 3), nonoperative (n = 11) |
| Gerber | 1998 | 16 | NR | 100 | Nonoperative |
| Ogilvie-Harris | 1997 | 7 | 100 | 77.8 | Operative |
NR, not reported.
Surgical Technique
Four studies described the surgical management of syndesmotic injuries, with a primary focus on grade II and III injuries.11,16,19,20 An additional 2 studies described both surgical and nonsurgical methods being used to treat varying grades of syndesmotic injuries.3,21 Surgical treatment involved variations of trans-syndesmotic procedures (n = 3) and adjunct arthroscopic surgery to treat syndesmotic instability (n = 1). Three studies reported on nonoperative techniques in the form of immobilization in a walking boot with progression to weightbearing.6,12,18
Rehabilitation Protocol
Detailed rehabilitation protocols were used for both operative and nonoperative treatment groups. Studies employed a progressive rehabilitation protocol that progressed coordination, muscular endurance, and motor control. This was supplemented with increasing focus on balancing and coordination exercises. In some studies, patients were advised to use a removable walking boot, thereby enabling progressive weightbearing as well as therapy to increase range of motion.3,4,18 Return to sport, when reported, was permitted when the athlete was able to perform a complete sport-specific functional progression program.18
Overall Return to Sport
Four studies (n = 91) reported 100% return to sport at the pre-injury level. Of these, 1 study focused solely on surgical management20 while another was nonoperative.6 Flik et al5 did not specify whether an operative or nonoperative technique was utilized but reported 100% return to sport at the preinjury level. Only 2 studies in this group described using both surgical and nonsurgical techniques to manage grade IIb and IIa syndesmotic injuries, respectively.3,21 Sman et al18 did not report on return to sport. The remaining studies reported that 83.6%, 96.3%, and 77.8% of athletes returned to sport at their preinjury level, respectively.11,16,19 Three studies reported a mean 97.6% of athletes returning to any level of sport.11,12,21 Seven studies reported on the mean time to return to sport (the recovery period), which was 55.2 ± 15.8 and 41.7 ± 9.8 days for operative and nonoperative management, respectively.3,5,11,12,18,19,20 The overall mean time to return to sport was 46.4 days (range, 15.4-70 days).
Calder et al3 included both operative and nonoperative management for grade IIb and IIa syndesmotic injuries, respectively. The nonoperative group (n = 28) was treated with a boot and rehabilitation, while the operative group (n = 36) required syndesmotic stabilization using the suture button fixation technique. All patients returned to sport at the preinjury level, with a mean return to sport of 45 days (range, 23-63 days) in the nonoperative group and 65 days (range, 27-104 days) in the operative group (P < 0.0001).
Steinmetz et al19 employed screw fixation methods and reported that 4% and 5.6% of syndesmotic screws had broken and resulted in rediastasis at the syndesmosis at 5- and 18-month follow-up, respectively. In another study, syndesmotic screws were removed in all patients once healing was complete, defined as when the athlete was able to complete a sport-specific functional progression program.8 Athletes were not permitted to return to competition until syndesmotic screws had been removed. Taylor et al20 reported hardware removal at an average of 74 days (range, 52-97 days) postoperatively, with 1 screw having broken prior to removal.
Functional Outcomes
Functional outcomes were reported in 2 studies. Steinmetz et al19 (n = 126), reported the following mean values: visual analog scale (VAS), 0.8 ± 1.3 (range, 0-6); American Orthopaedic Foot and Ankle Society (AOFAS) score, 93 ± 9 (range, 49-100); and OMAS, 93 ± 10 (range, 45-100). These can be interpreted as patients essentially reporting minimal or no pain (VAS) with excellent foot-specific function (AOFAS and OMAS). Taylor et al20 (n = 6) reported an Edwards and DeLee Ankle Rating of 0.8. This score is related to slight pain with excessive activity. Functional outcomes were effective in analyzing posttreatment results; however, reported outcomes mainly pertained to surgical intervention groups.
Recurrent Injuries and Complications
Complications were reported by Osbahr et al,12 where 2 of 36 athletes experienced recurrent sprains; however, this did not affect return to sport at the preinjury level. Minimal acute postoperative complications occurred in the same study12 (n = 2) and included instances of suspected infection.
Discussion
For athletes with an ankle syndesmotic injury, the literature supports a high level of return to sport at the preinjury level. Because of the lack of comparative studies, it is difficult to definitively comment on the role of surgical intervention in improving return to sport after such injuries. Return-to-sport rates were outlined by Calder et al3 when comparing operative and nonoperative groups for grade IIa and IIb injuries. In that study, all patients returned to sport at the preinjury level, with a mean return to sport of 45 days in the nonoperative group and 65 days in the operative group.
Return to sport at the preinjury level is particularly important for athletes competing at a professional level. We identified that a mean of 93.8% of all athletes returned to sport at the preinjury level. Osbahr et al12 reported that, although syndesmotic sprains are less common than lateral ankle sprains, they are associated with increased morbidity given the prolonged recovery period.4 In the study by Sman et al,18 which reported on lateral ankle sprains, the mean recovery period was stated as 15 days. Additionally, Osbahr et al12 found a mean recovery period of 6.5 ± 11.1 days for lateral ankle sprains. Comparatively, in this review, the mean time to return to sport for ankle syndesmotic injuries was 46.3 days (range, 15.4-70 days). Such substantial variability in time to return to sport may be due to the variation in how return to sport was defined.3,11,12,16,18,19,20 For instance, in the study by Ogilvie-Harris et al,11 the determination of return to sport was decided using various subjective assessments, which included evaluation on preoperative sporting activities and subsequent satisfaction surveys. In the study by Osbahr et al,12 the authors stated that it was difficult to differentiate between athletes’ return-to-play level related to preinjury performance level. Finally, in the study by Oztekin et al,13 determination of return to sport was made by a single clinician using a subjective criterion, which included completion of the rehabilitation protocol, a final clinical examination, and an on-field observational test performed by an individual surgeon.
This is in comparison with another study that implemented unbiased and safe return to sport through functional progression programs, including movement without any pain or discomfort.19 Return to sport is often defined as return to preinjury level, or return at any level across studies included in this review.3,5,6,11-13,16,18-21 It is evident from our findings that reported return-to-sport rates are variable and dependent on the study methodology and outcome definitions used. This highlights the importance of uniform diagnostic and return-to-play criteria.
More recent surgical treatments such as suture button fixation have demonstrated favorable clinical outcomes and may potentially lower complication rates. Suture button fixation obviates the need for routine implant removal to avoid potentially statically locking the syndesmosis in a malreduced position, making it an effective new technique that provides dynamic fixation.10 For this reason, some argue outcomes to be more favorable than commonly used trans-syndesmotic screw fixation, as it facilitates the stable natural motion at this complex joint without rigidly fixing it in place.9 However, this technique may be costly, and recent small case series have reported high soft tissue complication rates.19 A randomized trial by Andersen et al1 highlighted that patients treated with a suture button fixation had higher AOFAS and OMA scores and a lower VAS score for pain compared with patients treated using a single syndesmotic screw. The study underlined that there was improved syndesmotic reduction in the suture button patient group.21 Although this study highlights important findings, future larger prospective studies are required to definitively identify the optimal fixation technique with regard to return to sport.
Controversy exists with regard to the management of grade II injuries, which involve partial tearing of the syndesmotic ligaments. We found variability with respect to the management of such injuries in included studies. Grade IIb injuries include deltoid ligament injury, tenderness along the anterior interosseous membrane, a positive external rotation with a positive squeeze test, and suspicion of a widened syndesmosis on radiographs.3 The literature highlights disagreements between surgeons regarding diagnosis, appropriate treatment, and return to play. For example, in the study by Calder et al,3 26 athletes with grade IIa injury were treated nonoperatively while 38 athletes with grade IIb injury were treated operatively. Thus, it is clear that this is an area that demands future research and elaboration.
It is important to note the wide spectrum of injury patterns associated with syndesmotic injuries. As such, a deltoid ligament injury may have a direct impact on treatment decision-making. Calder et al3 reported that indications for surgery include injury to the medial deltoid, given findings of an unstable syndesmosis with arthroscopic examination. Additionally, our review found patients with injuries to both the AITFL and deltoid ligament take longer to return to sport than those with an isolated AITFL injury.3 Thus, it is clear that deltoid ligament injuries may be important in predicting whether early stabilization is required as well as the timeline for athletes’ expected return to sport. Our study found that purely ligamentous syndesmotic injuries had high return to preinjury and any level of sport rates. However, the majority of included syndesmotic injuries may have been stable and focused on AITFL. Thus, the results do not accurately encapsulate more chronic situations, including involvement of the superficial deltoid and late chondral injury.
Strengths and Limitations
The main strengths of this article lie in its rigorous study methodology and strict adherence to the PRISMA guidelines. Our search covered multiple databases, and all stages of screening were done in duplicate with reviewers being blinded when able, to minimize reviewer bias.
The systematic review is limited by the relatively small sample size. Additionally, the majority of studies were noncomparative, which meant that a meta-analysis was not possible. The studies included were heterogenous with regard to both grade of injury as well as treatment type, thereby making it difficult to compare studies. Furthermore, the lack of comparative studies made it difficult to determine whether there was a superiority of certain treatment methods over others. However, in the case of ankle syndesmotic injuries, it is difficult to analyze comparative studies, as different grades of injuries may necessitate either surgical or nonsurgical management.
Additionally, many of the studies included elaborated on neither the specifics of the surgeries nor the rehabilitation protocols implemented. Furthermore, return to sport was defined differently across the literature, thereby making it difficult to ascertain a standardized recovery period measure before return to sport. Moreover, the studies that reported on the return-to-sport timeline rarely commented on the length of the sport seasons and subsequent athletes’ recovery periods. Sman et al18 reported that health care providers were responsible for clearing athletes during the competition season; however, during the off-season, athletes used their own perception of recovery to determine whether they were fit to play. Furthermore, variations existed in the type of sport played, thus affecting season lengths. An additional weakness of included studies is the lack of detail regarding return-to-sport rates. For example, Gerber et al6 reported that only 44% of the syndesmosis group had acceptable outcomes yet also stated that all patients were able to return to full activity. Thus, the 100% return-to-sport rate and residual symptoms make it difficult to draw conclusions that reflect the athlete’s healing progress. To better be able to assess return-to-sport rates and to determine ideal treatment approaches, future high-quality prospective comparative studies with large sample sizes are necessary.
Conclusion
This systematic review showed a high rate of return to preinjury and any level of sport after ankle syndesmotic injury in patients receiving both operative and nonoperative treatment. Overall, an average of 93.8% of athletes were able to return to sport at the preinjury level. However, there is an inability to comment on whether there is a significant difference between management groups due to the lack of comparative studies. The strength of these conclusions is restricted by the inconsistencies in reporting outcomes as well as the quality of the available literature.
Supplemental Material
Supplemental material, DS_10.1177_1941738118816282 for Return to Sport After Ankle Syndesmotic Injury: A Systematic Review by Seline Y. Vancolen, Ibrahim Nadeem, Nolan S. Horner, Herman Johal, Bashar Alolabi and Moin Khan in Sports Health: A Multidisciplinary Approach
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Andersen MR, Frihagen F, Hellund JC, Madsen JE, Figved W. Randomized trial comparing suture button with single syndesmotic screw for syndesmosis injury. J Bone Joint Surg Am. 2018;100:2-12. [DOI] [PubMed] [Google Scholar]
- 2. Brown KW, Morrison WB, Schweitzer ME, Parellada JA, Nothnagel H. MRI findings associated with distal tibiofibular syndesmosis injury. AJR Am J Roentgenol. 2004;182:131-136. [DOI] [PubMed] [Google Scholar]
- 3. Calder JD, Bamford R, Petrie A, McCollum GA. Stable versus unstable grade II high ankle sprains: a prospective study predicting the need for surgical stabilization and time to return to sports. Arthroscopy. 2016;32:634-642. [DOI] [PubMed] [Google Scholar]
- 4. Duncan CR, Darin MF. Cost-effectiveness analysis of syndesmotic screw versus suture button fixation in tibiofibular syndesmotic injuries. J Orthop Trauma. 2018;32:e198-e203. [DOI] [PubMed] [Google Scholar]
- 5. Flik K, Lyman S, Marx RG. American collegiate men’s ice hockey: an analysis of injuries. Am J Sports Med. 2005;33:183-187. [DOI] [PubMed] [Google Scholar]
- 6. Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19:653-660. [DOI] [PubMed] [Google Scholar]
- 7. Jones MH, Amendola A. Syndesmosis sprains of the ankle: a systematic review. Clin Orthop Relat Res. 2007;455:173-175. [DOI] [PubMed] [Google Scholar]
- 8. Levy DM, Reid K, Gross CE. Ankle syndesmotic injuries: a systematic review. Tech Orthop. 2017;32:80-83. [Google Scholar]
- 9. Maempel J, Ward A, Chesser T, Kelly M. Use of tightrope fixation in ankle syndesmotic injuries. Chin J Traumatol. 2014;17:8-11. [PubMed] [Google Scholar]
- 10. Naqvi GA, Cunningham P, Lynch B, Galvin R, Awan N. Fixation of ankle syndesmotic injuries: comparison of tightrope fixation and syndesmotic screw fixation for accuracy of syndesmotic reduction. Am J Sports Med. 2012;40:2828-2835. [DOI] [PubMed] [Google Scholar]
- 11. Ogilvie-Harris DJ, Gilbart MK, Chorney K. Chronic pain following ankle sprains in athletes: the role of arthroscopic surgery. Arthroscopy. 1997;13:564-574. [DOI] [PubMed] [Google Scholar]
- 12. Osbahr DC, Drakos MC, O’Loughlin PF, et al. Syndesmosis and lateral ankle sprains in the National Football League. Orthopedics. 2013;36:e1378-e1384. [DOI] [PubMed] [Google Scholar]
- 13. Oztekin HH, Boya H, Ozcan O, Zeren B, Pinar P. Foot and ankle injuries and time lost from play in professional soccer players. Foot (Edinb). 2009;19:22-28. [DOI] [PubMed] [Google Scholar]
- 14. Parlamas G, Hannon CP, Murawski CD, et al. Treatment of chronic syndesmotic injury: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1931-1939. [DOI] [PubMed] [Google Scholar]
- 15. Porter DA, Jaggers RR, Barnes AF, Rund AM. Optimal management of ankle syndesmosis injuries. Open Access J Sports Med. 2014;5:173-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Porter DA, May BD, Berney T. Functional outcome after operative treatment for ankle fractures in young athletes: a retrospective case series. Foot Ankle Int. 2008;29:887-894. [DOI] [PubMed] [Google Scholar]
- 17. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [DOI] [PubMed] [Google Scholar]
- 18. Sman AD, Hiller CE, Rae K, Linklater J, Black DA, Refshauge KM. Prognosis of ankle syndesmosis injury. Med Sci Sports Exerc. 2014;46:671-677. [DOI] [PubMed] [Google Scholar]
- 19. Steinmetz S, Puliero B, Brinkert D, et al. Tibiofemoral syndesmosis injury treated by temporary screw fixation and ligament repair. Orthop Traumatol Surg Res. 2016;102:1069-1073. [DOI] [PubMed] [Google Scholar]
- 20. Taylor DC, Tenuta JJ, Uhorchak JM, Arciero RA. Aggressive surgical treatment and early return to sports in athletes with grade III syndesmosis sprains. Am J Sports Med. 2007;35:1833-1838. [DOI] [PubMed] [Google Scholar]
- 21. Wright RW, Barile RJ, Surprenant DA, Matava MJ. Ankle syndesmosis sprains in National Hockey League players. Am J Sports Med. 2004;32:1941-1945. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DS_10.1177_1941738118816282 for Return to Sport After Ankle Syndesmotic Injury: A Systematic Review by Seline Y. Vancolen, Ibrahim Nadeem, Nolan S. Horner, Herman Johal, Bashar Alolabi and Moin Khan in Sports Health: A Multidisciplinary Approach