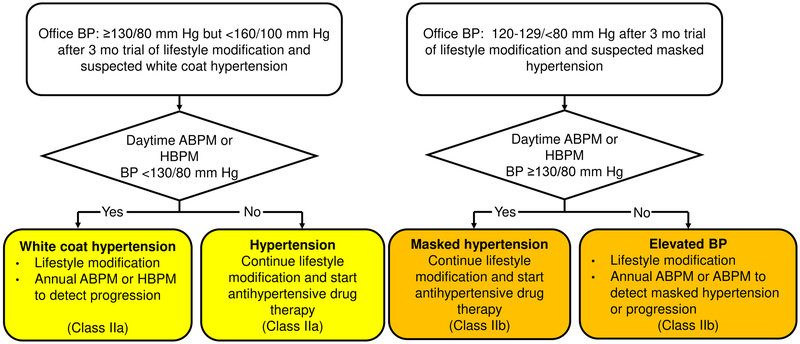
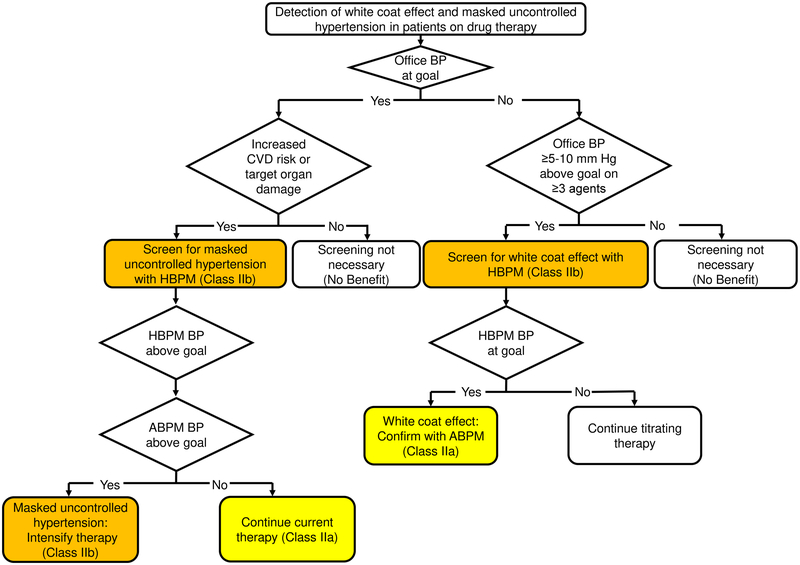
The 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure (BP) in Adults recommends classifying BP into one of four levels: normal BP, elevated BP and stage 1 and 2 hypertension based on the average of two or more measurements obtained in the office setting on two or more occasions (Table 1).1, 2 Hypertension is defined in the guideline as a mean office systolic BP (SBP) ≥ 130 mm Hg or a mean office diastolic BP (DBP) ≥ 80 mm Hg. To confirm the presence of hypertension, the ACC/AHA guideline recommends measuring BP outside of the office setting using daytime ambulatory blood pressure monitoring (ABPM) or home blood pressure monitoring (HBPM). The recommendation to use out-of-office BP measurements to confirm the presence of hypertension is consistent with several other guidelines including those from the UK National Institute for Health and Care Excellence, the Canadian Hypertension Education Program, National Heart Federation of Australia and the United States Preventive Services Task Force Recommendation Statement on High Blood Pressure Screening in Adults.3–6 The ACC/AHA guideline recommends that adults not taking antihypertensive medication with SBP ≥ 130 but <160 mm Hg or DBP ≥ 80 mm Hg but < 100 mm Hg should be screened with ABPM or HBPM for white coat hypertension (Figure 1, left panel). It also recommends screening adults not taking antihypertensive medication with SBP between 120 and 129 mm Hg or DBP between 75 and 79 mm Hg for masked hypertension (Figure 1, right panel). ABPM and HBPM are also recommended to identify a white coat effect and masked uncontrolled hypertension among adults taking antihypertensive medication (Figure 2).
Table 1.
Classification of blood pressure according to the 2017 American College of Cardiology/American Heart Association blood pressure guideline.
| Office blood pressure levels | 2017 ACC/AHA guideline classification |
||
|---|---|---|---|
| SBP, mm Hg | DBP, mm Hg | ||
| <120 | and | <80 | Normal blood pressure |
| 120–129 | and | <80 | Elevated blood pressure |
| 130–139 | or | 80–89 | Stage 1 hypertension |
| ≥140 | or | ≥90 | Stage 2 hypertension |
Participants with systolic blood pressure and diastolic blood pressure in two categories (e.g., systolic blood pressure < 120 mm Hg and diastolic blood pressure between 80 and 89 mm Hg) should be designated into the higher category.
2017 ACC/AHA guideline - 2017 American College of Cardiology / American Heart Association Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults.
SBP – Systolic blood pressure; DBP – diastolic blood pressure.
Reprinted with permission: Hypertension.2018;71:e13-e115 © 2017 by the American College of Cardiology Foundation and the American Heart Association, Inc.
Figure 1.
Algorithm to screen for white coat hypertension and masked hypertension among adults not taking antihypertensive medication in the 2017 American College of Cardiology/American Heart Association blood pressure guideline.
ABPM – Ambulatory blood pressure monitoring; HBPM – home blood pressure monitoring; BP – blood pressure.
Reprinted with permission: Hypertension.2018;71:e13-e115 © 2017 by the American College of Cardiology Foundation and the American Heart Association, Inc.
Figure 2.
Algorithm to screen for white coat effect or masked uncontrolled hypertension among adults taking antihypertensive medication in the 2017 American College of Cardiology/American Heart Association blood pressure guideline.
ABPM – Ambulatory blood pressure monitoring; HBPM – home blood pressure monitoring; CVD – cardiovascular disease; BP – blood pressure.
Reprinted with permission: Hypertension.2018;71:e13-e115 © 2017 by the American College of Cardiology Foundation and the American Heart Association, Inc.
In 2003, the Seventh Report of the Joint National Committee (JNC7) guideline provided BP thresholds on ABPM for defining hypertension in US adults.7 In the JNC7 guideline, awake and asleep hypertension were defined by mean SBP/DBP levels ≥ 135/85 mm Hg and ≥ 120/75 mm Hg, respectively. These thresholds were determined assuming office SBP/DBP readings ≥ 140/90 mm Hg as the reference point for the definition of hypertension rather than the office SBP/DBP ≥ 130/80 mm Hg recommendation adopted in the 2017 ACC/AHA guideline. Many scientific statements and guidelines have published BP thresholds for defining hypertension based on ABPM and HBPM since the JNC7 guideline.8, 9 In the current manuscript, we describe how out-of-office BP thresholds based on ABPM and HBPM corresponding to BP levels in the office setting were selected by the 2017 ACC/AHA writing committee. To provide the context for the writing committee’s decisions, we describe three approaches that have been used in epidemiological studies to identify ABPM and HBPM BP thresholds that are deemed high or that correspond to values obtained in an office setting. We also review data gaps and future research needs.
Approaches for defining high BP on ABPM/HBPM
In the early 1990s, BP thresholds for ABPM were identified based on populations’ distributions, a method called the distribution-based approach.10, 11 For example, in one study, BP above the 95th percentile or two standard deviations above the mean was identified as being significantly elevated and a BP between one and two standard deviations above the mean was considered to be marginally elevated.10 In another study, the percentage of participants with an office SBP/DBP ≥ 140/90 mm Hg was identified and ABPM SBP and DBP values with a similar percentage of participants above these levels were identified and used as the upper limit of normotension.12 The ABPM thresholds used to define elevated or high BP with the distribution-based approach varied markedly across populations.11, 13, 14 This likely reflects the enrollment of populations with different characteristics including the proportion taking antihypertensive medication and office BP levels. Furthermore, there is no scientific basis to assume that a fixed percentage of the population has high BP on ABPM or HBPM.
A second approach, the regression-based approach, uses regression models to estimate the ABPM or HBPM BP levels for any given office BP value.15–18 In many, but not all, prior studies, a standard ordinary least squares regression model has been used to regress out-of-office BP on office BP. An issue with this approach is the measurement error of office BP, the independent variable, results in an attenuated slope between office and out-of-office BP. To address this issue, models for continuous outcomes that address measurement error in the exposure variable (e.g., Deming regression or ordinary least products regression), should be used instead of ordinary least squares regression. Using the intercept and beta coefficient from the regression model, the level of awake SBP that is equivalent to a specific office SBP level (e.g., 120, 130, 140 and 160 mm Hg) can be estimated. Another issue with the regression-based approach is that the risk for CVD associated with ABPM and HBPM BP values may not correspond accurately to office BP due to white coat and masked effects.
The third approach, the outcomes-based approach, identifies the incidence rate for an outcome (e.g., cardiovascular disease [CVD]) associated with a range of office-based BP levels (e.g., SBP ≥ 140 mm Hg). Then, the corresponding range of BP on ABPM that is associated with a similar incidence rate is identified (e.g., SBP ≥ 135 mm Hg).19
Each of these approaches can identify ABPM or HBPM SBP and DBP thresholds that correspond to BP measured in the office setting. Also, multiple ABPM and HBPM BP thresholds can be identified (e.g., BP levels corresponding with normal BP, elevated BP, and hypertension). BP measured by ABPM and HBPM maintains a stronger association with CVD events compared to BP measured in the office setting.20 ABPM and HBPM also can be used to identify white coat hypertension and masked hypertension.9 Therefore, the ACC/AHA writing committee sought to identify ABPM and HBPM threshold levels associated with the office BP levels that were selected for BP classification. There is general consensus that ABPM and HBPM BP thresholds should be based on outcomes data and the ACC/AHA writing committee agreed that this method is currently the best approach available.
Selection of thresholds values in the 2017 ACC/AHA guideline
The 2017 ACC/AHA guideline provides HBPM SBP and DBP values and ABPM daytime, nighttime and 24-hour SBP and DBP values that correspond to office-measured SBP and DBP levels (Table 2). These BP levels were selected based on a review of large published prospective cohort studies of ABPM and HBPM.14, 21–23 When available, the outcomes-based approach was used to identify ABPM and HBPM BP levels that corresponded to BP measured in an office setting.14, 21–23 BP thresholds identified in studies that used the regression-based approach were considered when data from the outcomes-based approach were not identified.18 Given there were very few studies identified and the studies that were available provided very consistent results, the writing committee decided there was no need to meta-analyze the data. The ACC/AHA writing committee also reviewed guidelines and scientific statements that reported HBPM and ABPM BP levels corresponding to measurements obtained in an office setting.8, 24–28 Table 3 provides the ABPM thresholds identified from outcomes-based studies and from several prior guidelines and scientific statements. Table 4 provides corresponding information for HBPM. Although there were some discrepancies between the BP levels in the published research studies and prior guidelines/scientific statements, these differences were small (i.e., within 5 mm Hg).
Table 2.
Blood pressure thresholds for home and ambulatory blood pressure monitoring that correspond to office blood pressure levels in the 2017 American College of Cardiology/American Heart Association blood pressure guideline.
| Office BP | HBPM | Awake ABPM | Asleep ABPM | 24-hour ABPM |
|---|---|---|---|---|
| 120/80 | 120/80 | 120/80 | 100/65 | 115/75 |
| 130/80 | 130/80 | 130/80 | 110/65 | 125/75 |
| 140/90 | 135/85 | 135/85 | 120/70 | 130/80 |
| 160/100 | 145/90 | 145/90 | 140/85 | 145/90 |
Numbers in the table are systolic/diastolic blood pressure and are presented in mm Hg.
BP – blood pressure.
HBPM – Home blood pressure monitoring.
ABPM – Ambulatory blood pressure monitoring.
Reprinted with permission: Hypertension.2018;71:e13-e115 © 2017 by the American College of Cardiology Foundation and the American Heart Association, Inc.
Table 3.
Awake, asleep and 24-hour blood pressure thresholds for ambulatory blood pressure monitoring that correspond with office blood pressure levels identified from outcomes-based studies and prior guidelines and scientific statements.
| Office blood pressure |
Awake blood pressure | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcome based studies |
Prior guidelines/scientific statements | |||||||
| ACC/AHA guideline |
Ohasama* (n= 1,542) |
IDACO† (n=5682) |
2005 AHA |
2008 ASH |
2011 Australia |
2013 ESH |
2015 Canada |
|
| 120/80 | 120/80 | 125/80 | 130/80 | 120/80 | ||||
| 130/80 | 130/80 | 133/82 | 135/85 | |||||
| 140/90 | 135/85 | 140/85 | 140/90 | 135/85 | 135/85 | 135/85 | 135/85 | |
| 160/100 | 145/90‡ | |||||||
| Office blood pressure |
Asleep blood pressure | |||||||
| Outcome based studies |
Prior guidelines/scientific statements | |||||||
| ACC/AHA guideline |
Ohasama* (n= 1,542) |
IDACO† (n=5682) |
2005 AHA |
2008 ASH |
2011 Australia |
2013 ESH |
2015 Canada |
|
| 100/65 | 115/65 | |||||||
| 130/80 | 110/65 | 120/70 | ||||||
| 140/90 | 120/70 | 121/70 | 125/75 | 120/75 | 120/70 | 120/70 | ||
| 160/100 | 140/85‡ | |||||||
| Office blood pressure |
24-hour blood pressure | |||||||
| Prior guidelines/scientific statements | ||||||||
| ACC/AHA guideline |
Ohasama* (n= 1,542) |
IDACO† (n=5682) |
2005 AHA |
2008 ASH |
2011 Australia |
2013 ESH |
2015 Canada |
|
| 120/80 | 115/75 | 119/74 | 115/75 | |||||
| 130/80 | 125/75 | 125/76 | ||||||
| 140/90 | 130/80 | 134/79 | 132/79 | 130/80 | 130/80 | |||
| 160/100 | 145/90‡ | |||||||
Numbers in the table are systolic/diastolic blood pressure and are presented in mm Hg.
Blank cells indicate office blood pressure levels for which thresholds on ambulatory blood pressure monitoring were not reported.
Ohkubo et. al. (reference 23). N.B. The Ohasama study population is also included in the IDACO (Kikuya et. al, reference 21).
Kikuya et. al. (reference 21).
As no data using the outcome-based approach were identified for these BP values, the values were determined from a study using the regression-based approach (Head et. al., reference 18).
BP – blood pressure
IDACO - The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome
ACC – American College of Cardiology
AHA – American Heart Association
ASH – American Society of Hypertension
ESH – European Society of Hypertension
Table 4.
Blood pressure thresholds for home blood pressure monitoring identified in outcomes-based studies and prior guidelines and scientific statements.
| Office blood pressure |
Home blood pressure | |||||
|---|---|---|---|---|---|---|
| Outcome-based studies |
Prior guidelines/scientific statements |
|||||
| ACC/AHA guideline |
2008 meta-analysis* |
IDHOCO† (n=6,470) |
2013 ESH |
2015 Canada |
2015 Australia |
|
| 120/80 | 120/80 | 120/80 | 120/75 | |||
| 130/80 | 130/80 | 130/80 | 125/75 | |||
| 140/90 | 135/85 | 135/85 | 130/85 | 135/85 | 135/85 | 135/85 |
| 160/100 | 145/90 | 145/90 | 145/90 | |||
Numbers in the table are systolic/diastolic blood pressure and are presented in mm Hg.
Blank cells indicate office blood pressure levels for which thresholds on home blood pressure monitoring were not reported.
Staessen et. al. (reference 14).
Niiranen TJ et. al. (reference 22)
BP – blood pressure
IDHOCO - The International Database of HOme blood pressure in relation to Cardiovascular Outcome.
ESH – European Society of Hypertension.
Evidence gaps
The BP thresholds selected by the ACC/AHA writing committee were based on the best evidence available at the time the guideline was prepared. However, gaps in knowledge exist. For example, none of the outcomes-based studies included African Americans, a population with a high prevalence of hypertension. A 2017 analysis from the Jackson Heart Study, a cohort comprised exclusively of African-American adults, evaluated ABPM SBP thresholds that corresponded with office SBP values among 441 adults not taking antihypertensive medication and 575 adults taking antihypertensive medication.19 DBP thresholds were not evaluated using the outcomes-based approach because DBP, when measured in an office setting, was not associated with CVD risk in this study. Using the outcomes-based approach, the ABPM SBP levels that corresponded to office-measured SBP values of 120, 130, 140 and 160 mm Hg were higher than those recommended in the ACC/AHA guideline. These data highlight the need for additional studies to evaluate thresholds for ABPM and HBPM that correspond to BP measured in an office setting in different populations, including racial/ethnic minorities. Additionally, it is unclear whether the ABPM and HBPM BP thresholds should be uniform across different age groups, for men and women, and for adults taking and not taking antihypertensive medication.29–31 In contrast to the ACC/AHA guideline, which recommends using daytime BP on ABPM, recent studies and a 2013 European Society of Hypertension position paper on ABPM suggest that 24-hour BP or daytime, nighttime and 24-hour BP should be considered when defining white coat hypertension, masked hypertension, white coat effect, and masked uncontrolled hypertension.32–34 Additional studies are needed to determine the risk for CVD and the benefits of antihypertensive medication for individuals with these phenotypes when they are defined using BP measurements from different time periods. Also, studies are needed to identify whether alternative methods to the outcomes-based approach are available to identify ABPM and HBPM BP thresholds.
The thresholds used to define normal and elevated BP and hypertension in the ACC/AHA guideline were based on office measurements.1, 2 The analogous ABPM and HBPM BP thresholds were determined using office measurements as the referent standard as described in this article. This approach may seem counterintuitive as the association of BP with CVD outcomes is stronger for measurements obtained by ABPM and HBPM compared to readings obtained in the office setting.20 Additionally, ABPM is considered the best technique to confirm the presence of hypertension.3 However, large-scale outcome trials comparing antihypertensive medication versus placebo and trials that have compared different intensities of treatment have used office BP to determine participant eligibility and BP goal achievement. There is a lack of data from randomized controlled trials using ABPM and HBPM BP levels to guide antihypertensive medication initiation and intensification. Such data will allow BP thresholds used for classification to be directly determined from ABPM and HBPM.
Perspectives
In summary, the 2017 ACC/AHA guideline provides ABPM and HBPM BP thresholds that correspond to normal BP, elevated BP, and stages 1 and 2 hypertension in an office-based setting. Additionally, thresholds corresponding to an average SBP and DBP of 160 mm Hg and 100 mm Hg, respectively, are provided. These thresholds should be used to identify adults with white coat hypertension and masked hypertension.
Supplementary Material
ACKNOWLEDGEMENT:
The authors thank Drs. Daichi Shimbo and Joseph E. Schwartz for their review and comments on a draft version of this manuscript.
SOURCES OF FUNDING: Dr. Paul Muntner received support from American Heart Association grant 15SFRN2390002. Dr. Robert M. Carey received support from grants R01-HL128189 and P01-HL074940 from the National Heart, Lung and Blood Institute. Dr. Kenneth Jamerson received support from grant 5U01-DK061028 from the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Paul K Whelton received support from grant P20GM109036 from the National Institute for General Medical Sciences.
Footnotes
DISCLOSURE: Drs. Paul Muntner, Robert M. Carey, Kenneth Jamerson, Jackson T. Wright, and Paul K. Whelton were members of the 2017 American College of Cardiology / American Heart Association Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. Dr. Kenneth Jamerson reports receiving research support from Bayer Pharma AG.
References
- 1.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. J Am Coll Cardiol. 2017;71:e127–e248. [DOI] [PubMed] [Google Scholar]
- 2.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–1324. [DOI] [PubMed] [Google Scholar]
- 3.Siu AL. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:778–786. [DOI] [PubMed] [Google Scholar]
- 4.Leung AA, Nerenberg K, Daskalopoulou SS, et al. Hypertension Canada’s 2016 Canadian Hypertension Education Program Guidelines for Blood Pressure Measurement, Diagnosis, Assessment of Risk, Prevention, and Treatment of Hypertension. Can J Cardiol. 2016;32:569–588. [DOI] [PubMed] [Google Scholar]
- 5.National Heart Foundation of Australia. Guideline for the diagnosis and management of hypertension in adults - 2016. Available at: https://www.heartfoundation.org.au/images/uploads/publications/PRO-167_Hypertension-guideline-2016_WEB.pdf (Accessed July 1, 2018).
- 6.Krause T, Lovibond K, Caulfield M, McCormack T, Williams B, Guideline Development G. Management of hypertension: summary of NICE guidance. BMJ. 2011;343:d4891. [DOI] [PubMed] [Google Scholar]
- 7.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., Jones DW, Materson BJ, Oparil S, Wright JT Jr., Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 8.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ, Subcommittee of P, Public Education of the American Heart Association Council on High Blood Pressure R. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:142–161. [DOI] [PubMed] [Google Scholar]
- 9.Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Role of Ambulatory and Home Blood Pressure Monitoring in Clinical Practice: A Narrative Review. Ann Intern Med. 2015;163:691–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imai Y, Nagai K, Sakuma M, Sakuma H, Nakatsuka H, Satoh H, Minami N, Munakata M, Hashimoto J, Yamagishi T, et al. Ambulatory blood pressure of adults in Ohasama, Japan. Hypertension. 1993;22:900–912. [DOI] [PubMed] [Google Scholar]
- 11.O’Brien E, Murphy J, Tyndall A, Atkins N, Mee F, McCarthy G, Staessen J, Cox J, O’Malley K. Twenty-four-hour ambulatory blood pressure in men and women aged 17 to 80 years: the Allied Irish Bank Study. J Hypertens. 1991;9:355–360. [DOI] [PubMed] [Google Scholar]
- 12.de Gaudemaris R, Chau NP, Mallion JM. Home blood pressure: variability, comparison with office readings and proposal for reference values. Groupe de la Mesure, French Society of Hypertension. J Hypertens. 1994;12:831–838. [PubMed] [Google Scholar]
- 13.Staessen J, Bulpitt CJ, Fagard R, Mancia G, O’Brien ET, Thijs L, Vyncke G, Amery A. Reference values for ambulatory blood pressure: a population study. J Hypertens Suppl. 1991;9:S320–321. [PubMed] [Google Scholar]
- 14.Staessen JA, Thijs L, Ohkubo T, Kikuya M, Richart T, Boggia J, Adiyaman A, Dechering DG, Kuznetsova T, Thien T, de Leeuw P, Imai Y, O’Brien E, Parati G. Thirty years of research on diagnostic and therapeutic thresholds for the self-measured blood pressure at home. Blood Press Monit. 2008;13:352–365. [DOI] [PubMed] [Google Scholar]
- 15.Schettini C, Bianchi M, Nieto F, Sandoya E, Senra H. Ambulatory blood pressure: normality and comparison with other measurements. Hypertension Working Group. Hypertension. 1999;34:818–825. [DOI] [PubMed] [Google Scholar]
- 16.Mancia G, Sega R, Bravi C, De Vito G, Valagussa F, Cesana G, Zanchetti A. Ambulatory blood pressure normality: results from the PAMELA study. J Hypertens. 1995;13:1377–1390. [PubMed] [Google Scholar]
- 17.Thijs L, Staessen JA, Celis H, de Gaudemaris R, Imai Y, Julius S, Fagard R. Reference values for self-recorded blood pressure: a meta-analysis of summary data. Arch Intern Med. 1998;158:481–488. [DOI] [PubMed] [Google Scholar]
- 18.Head GA, Mihailidou AS, Duggan KA, et al. Definition of ambulatory blood pressure targets for diagnosis and treatment of hypertension in relation to clinic blood pressure: prospective cohort study. BMJ. 2010;340:c1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ravenell J, Shimbo D, Booth JN 3rd, Sarpong DF, Agyemang C, Beatty Moody DL, Abdalla M, Spruill TM, Shallcross AJ, Bress AP, Muntner P, Ogedegbe G. Thresholds for Ambulatory Blood Pressure Among African Americans in the Jackson Heart Study. Circulation. 2017;135:2470–2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;162:192–204. [DOI] [PubMed] [Google Scholar]
- 21.Kikuya M, Hansen TW, Thijs L, Bjorklund-Bodegard K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA, International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes I. Diagnostic thresholds for ambulatory blood pressure monitoring based on 10-year cardiovascular risk. Circulation. 2007;115:2145–2152. [DOI] [PubMed] [Google Scholar]
- 22.Niiranen TJ, Asayama K, Thijs L, Johansson JK, Ohkubo T, Kikuya M, Boggia J, Hozawa A, Sandoya E, Stergiou GS, Tsuji I, Jula AM, Imai Y, Staessen JA, International Database of Home blood pressure in relation to Cardiovascular Outcome I. Outcome-driven thresholds for home blood pressure measurement: international database of home blood pressure in relation to cardiovascular outcome. Hypertension. 2013;61:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ohkubo T, Imai Y, Tsuji I, Nagai K, Ito S, Satoh H, Hisamichi S. Reference values for 24-hour ambulatory blood pressure monitoring based on a prognostic criterion: the Ohasama Study. Hypertension. 1998;32:255–259. [DOI] [PubMed] [Google Scholar]
- 24.Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D, American Heart A, American Society of H, Preventive Cardiovascular Nurses A. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008;52:1–9. [DOI] [PubMed] [Google Scholar]
- 25.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–1357. [DOI] [PubMed] [Google Scholar]
- 26.Cloutier L, Daskalopoulou SS, Padwal RS, Lamarre-Cliche M, Bolli P, McLean D, Milot A, Tobe SW, Tremblay G, McKay DW, Townsend R, Campbell N, Gelfer M. A New Algorithm for the Diagnosis of Hypertension in Canada. Can J Cardiol. 2015;31:620–630. [DOI] [PubMed] [Google Scholar]
- 27.Head GA, McGrath BP, Mihailidou AS, Nelson MR, Schlaich MP, Stowasser M, Mangoni AA, Cowley D, Brown MA, Ruta LA, Wilson A. Ambulatory blood pressure monitoring in Australia: 2011 consensus position statement. J Hypertens. 2012;30:253–266. [DOI] [PubMed] [Google Scholar]
- 28.Sharman JE, Howes FS, Head GA, McGrath BP, Stowasser M, Schlaich M, Glasziou P, Nelson MR. Home blood pressure monitoring: Australian Expert Consensus Statement. J Hypertens. 2015;33:1721–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ishikawa J, Ishikawa Y, Edmondson D, Pickering TG, Schwartz JE. Age and the difference between awake ambulatory blood pressure and office blood pressure: a meta-analysis. Blood Press Monit. 2011;16:159–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ntineri A, Stergiou GS, Thijs L, et al. Relationship between office and home blood pressure with increasing age: The International Database of HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO). Hypertens Res. 2016;39:612–617. [DOI] [PubMed] [Google Scholar]
- 31.Stergiou GS, Ntineri A, Kollias A, Destounis A, Nasothimiou E, Roussias L. Changing relationship among clinic, home, and ambulatory blood pressure with increasing age. J Am Soc Hypertens. 2015;9:544–552. [DOI] [PubMed] [Google Scholar]
- 32.O’Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–1768. [DOI] [PubMed] [Google Scholar]
- 33.Anstey DE, Colantonio LD, Yano Y, Booth Iii JN, Muntner P. The importance of using 24-hour and nighttime blood pressure for the identification of white coat hypertension: Data from the Jackson Heart Study. J Clin Hypertens (Greenwich). 2018; July 6. doi: 10.1111/jch.13330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de la Sierra A, Vinyoles E, Banegas JR, Segura J, Gorostidi M, de la Cruz JJ, Ruilope LM. Prevalence and clinical characteristics of white-coat hypertension based on different definition criteria in untreated and treated patients. J Hypertens. 2017;35:2388–2394. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.