Abstract
Objectives:
To assess willingness of women with pelvic floor disorders to adopt non-traditional mobile communication methods with health care providers.
Methods:
Cross-sectional study of women with pelvic floor disorders. Women completed a survey regarding what technology they owned, how they utilized it and their willingness to use technology to communicate with providers.
Results:
Overall mobile technology ownership was high; however, older women were significantly less likely to own a smart phone (75%) compared to younger (100%) and middle-aged women (98%) (p < .01). On univariable analysis, factors significantly associated with willingness to use mobile technology were age (p < .01) and education status (p < .01). A relationship between travel distance to the clinic and willingness to adopt various mobile technologies was not noted. On multivariable analysis, after controlling for education and travel distance to clinic, older women remained significantly less likely to express willingness to use various technologies: video-conference technology (OR 0.97, 95% CI 0.95, 0.99), text messaging (OR 0.94, 95% CI 0.91, 0.97), internet-based patient portal (OR 0.96, 95% CI 0.94, 0.98) and e-mail (OR 0.94, 95% CI 0.91, 0.98). However, almost 50% of older women and greater than 65% of middle-aged women expressed willingness to adopt technologies for health care communication.
Conclusions:
Age-related differences exist in the ownership, utilization, and willingness to communicate with medical providers through mobile technology. However, the majority of women across all age-groups, irrespective of travel distance, are willing to adopt alternative mobile technologies to communicate with their health care providers.
Introduction
Telemedicine is the ability to provide clinical care to patients who are not physically present in the same location as their health care provider through the utilization of technology. While traditional telemedicine comprised of telephone calls, newer communication strategies include text messaging, e-mail, virtual clinical encounters via video-conferencing and virtual inpatient rounding with the use of robots. In recent years, medical professionals in several specialties are utilizing telemedicine at increasingly higher rates in the outpatient setting.
Telemedicine programs have been shown to decrease patient and family anxiety, increase patient engagement in care, and provide additional emotional and clinical support for patients with chronic medical conditions following discharge from the hospital.1–5 A robust telemedicine program has the ability to increase efficiency of care, expand access to care and increase patient satisfaction in the outpatient setting.6–10 A judicious implementation of telemedicine modalities can enhance the patient experience by improving overall communication.10–12 However, before incorporating telemedicine into a clinical practice, providers should thoroughly assess the ability and willingness of the targeted patients to participate in the proposed program.11
Women with pelvic floor disorders are a unique population composed primarily of women with pelvic organ prolapse, urinary or fecal incontinence and pelvic floor dysfunction. Many older women with pelvic floor disorders, especially those with urinary and fecal incontinence, also suffer from limited mobility, thus increasing their dependence on caregivers to travel to their providers’ office.13,14 A telemedicine program that effectively allows women with pelvic floor disorders to communicate with their health care providers has the potential of increasing patient satisfaction and reducing caregiver burden. Though prior studies suggest that adults are willing to adopt the use of mobile technology in their daily lives, precise estimates of ownership and willingness to use mobile technology for health care in women with pelvic floor disorders are lacking.15 Our primary objective was to assess ownership, use, and willingness to adopt non-traditional communication methods with health care providers among women with pelvic floor disorders, and explore age-related differences. We hypothesized that older women with pelvic floor disorders would be less likely to own, utilize and adopt mobile communication technology for health care purposes than younger women.
Materials and Methods
This is a cross sectional study of women with pelvic floor disorders (pelvic organ prolapse, urinary and fecal incontinence or pelvic floor dysfunction). Women over the age of 18 were recruited from multiple urban and suburban female pelvic medicine and reconstructive surgery (FPMRS) clinics of a tertiary academic health system between June 2017 and March 2018. Women were approached to fill out a survey at the beginning of their clinic visit. Women who could not read or write English were excluded from the study. This study was reviewed and approved by the Institutional Review Board. Participants provided written informed consent.
The survey collected demographics, information regarding what technology respondents owned, how they utilized it and their willingness to use various forms of technology to communicate with their medical providers. Technology ownership and utilization were assessed by a “yes” or “no” response. We have defined “willingness to use technology” as self-reported readiness or desire to use various mobile communication technologies.16–18 The woman’s willingness to communicate with her providers with technology was based on responses to a five-level Likert scale (strongly agree, agree, neutral, disagree and strongly disagree). This survey was modified from the Mobile Health and Cell Phone Activities surveys by the Pew Research Center.19,20 Self-reported estimate of travel distance to clinic was also collected.
All surveys were administered to patients at the beginning of their clinical encounter and surveys were handed directly back to study personnel. The study personnel verified that all questions were answered and if any answer choices were left blank, the patients were encouraged to either answer the question or choose the option, “prefer not to answer”. Respondents were placed in the following age groups: young (age < 45), middle-aged (age ≥45 and <65) and older (age ≥ 65) based on age group definitions used in similar studies.15,21–24 Willingness to use mobile technology to communicate with a medical provider was categorized as a yes/no variable. Women were classified as willing to use mobile technology if they responded “strongly agree” or “agree”. Data between groups were analyzed using Pearson chi-square and Fisher’s exact tests as appropriate. Univariable logistic regression models were used to examine the association of patient age, education level and distance from the clinic with willingness to use mobile communication technology. Variables with a p-value less than 0.1 were then included in multivariable logistic regression. All reported p-values were two-sided and p-values < 0.05 were considered statistically significant. Statistical analysis was performed using Stata version 13.1 Software (StataCorp, College Station, TX, USA).
Precise estimates on willingness of older adults with pelvic floor disorders to use mobile communication technology are not available. Prior studies indicate that 30–40% of older adults with chronic medical conditions are willing to use mobile communication technology for their health care.25 We estimated a sample size of 46 women per group to detect a 2-fold difference in willingness to use mobile communication technology among older women with pelvic floor disorders compared to younger women (40% in older women and 80% in younger women). Given our three group comparison (young, middle-aged and older women) we chose a conservative Type I error rate of 0.125 (traditional Type I error rate of 0.05 divided by the 4 possible match pairings) and a power of 0.90.
Results
A total of 200 women completed the survey. Demographic data are presented in Table 1. The median age of respondents was 59 years old (range 22 to 90 years old). Majority of the subjects were Caucasian. The median number of miles traveled for their clinic visit was 11 miles (range 1 to 108 miles). Forty-eight percent of women traveled less than 10 miles while 11% of women traveled more than 30 miles. One third of the women presented with a chief complaint of pelvic organ prolapse and 55% of the women presented with various urinary problems (incontinence, urinary urgency and frequency and recurrent urinary tract infections). Our missing data rate was 2% for 4 subjects who did not provide information on race and employment status.
Table 1.
Demographics
| N = 200 (n, %) | |
|---|---|
| Age (median, range) | 59 (22–90) |
| Young (age <45) | 50 (25) |
| Middle-Aged (age ≥45 and <65) | 89 (45) |
| Older (aged ≥ 65) | 61 (30) |
| Parity (median, range) | 2 (0–7) |
| Race | |
| Caucasian | 153 (76) |
| Black | 33 (17) |
| Asian | 3 (2) |
| Other | 7 (3) |
| Prefer not to state | 4 (2) |
| Employment status | |
| Employed for wages | 101 (51) |
| Self employed | 19 (9) |
| Homemaker | 15 (8) |
| Student | 3 (1) |
| Retired | 47 (24) |
| Unemployed | 4 (2) |
| Disabled | 10 (5) |
| Prefer not to state | 1 (1) |
| Level of education | |
| Some high school | 11 (5) |
| High school graduate | 22 (11) |
| Some college | 22 (11) |
| Associates degree | 16 (8) |
| Bachelor’s degree | 56 (28) |
| More than college | 73 (36) |
| Distance from home to clinic (median, range) | 11 (1–108) |
| ≤ 3 miles | 45 (23) |
| >3 and ≤10 miles | 50 (25) |
| >10 and ≤30 miles | 84 (42) |
| > 30 miles | 21 (10) |
| Primary Reason for Visit | |
| Urinary problem | 77 (39) |
| Pelvic organ prolapse | 67 (33) |
| Defecatory problem | 1 (1) |
| Pelvic pain | 14 (7) |
| Recurrent UTI | 27 (13) |
| Hematuria | 6 (3) |
| Other | 8 (4) |
| History of hysterectomy | 62 (31) |
| History of prolapse surgery | 64 (32) |
| History of urinary incontinence procedure | 49 (25) |
| Urinary incontinence | 128 (64) |
| Fecal incontinence | 15 (8) |
| Charlson Comorbidity Index (median, range) | 2 (0–6) |
In our population of 200 women with pelvic floor disorders, the overall ownership of mobile technology was high, with smartphones (92%) being the most popular device followed by computers (81%) and tablet devices (63%). The majority of women were capable of sending text messages (93%), taking pictures (94%) and videos (86%) with their mobile devices, and using video-conference technology such as FaceTime and Skype (71%). Greater than 66% of women expressed a willingness to communicate with their providers via alternative communication methods beyond the telephone.
Age-related differences in the ownership and utilization of mobile communication technology were noted (Table 2). Older women were less likely to own mobile technology compared to young and middle-aged women; however, while older women were significantly less likely to own a smart phone, ownership within each age group was greater than 75%. Utilization of the various functionalities of mobile technology followed a similar trend, with older women being on the lower end of the utilization spectrum followed by middle-aged and younger women.
Table 2.
Ownership of mobile technology among women with pelvic floor disorders
| Young1 (N = 50) Proportion (95% Confidence Interval) | Middle-Aged2 (N = 89) Proportion (95% Confidence Interval) | Older3 (N = 61) Proportion (95% Confidence Interval) | p-value4 | |
|---|---|---|---|---|
| Do you own…? | ||||
| Cellular Phone | n=50 1.0 (0.93, 1.0) | n=89 1.0 (0.96, 1.0) | n=57 0.93 (0.84, 0.98) | 0.01 |
| Smartphone | n=50 (0.93, 1.0) | n=87 0.98 (0.92, 1.0) | n=46 0.75 (0.63, 0.86) | <0.001 |
| Computer | n=38 0.76 (0.62, 0.87) | n=79 0.89 (0.80, 0.95) | n=45 0.74 (0.61, 0.84) | 0.04 |
| Tablet Device | n=34 0.68 (0.53, 0.80) | n=59 0.66 (0.55, 0.76) | n=32 0.52 (0.39, 0.65) | 0.15 |
| High Speed Internet | n=49 0.98 (0.89, 1.0) | n=86 0.97 (0.90, 0.99) | n=55 0.90 (0.80, 0.96) | 0.16 |
| Do you access or perform the following tasks on your mobile device? | ||||
| n=49 0.98 (0.89, 1.0) | n=83 0.93 (0.86, 0.97) | n=46 0.75 (0.63, 0.86) | <0.001 | |
| Text Messaging | n=50 1.0 (0.93, 1.0) | n=88 0.99 (0.94, 1.0) | n=48 0.79 (0.66, 0.88) | <0.001 |
| Take Pictures | n=50 1.0 (0.93, 1.0) | n=88 0.99 (0.94, 1.0) | n=49 0.80 (0.68, 0.89) | <0.001 |
| Record Videos | n=50 1.0 (0.93, 1.0) | n=82 0.92 (0.84, 0.97) | n=39 0.64 (0.51, 0.76) | <0.001 |
| Send Pictures | n=50 1.0 (0.93, 1.0) | n=85 0.96 (0.89, 0.99) | n=49 0.80 (0.68, 0.89) | <0.001 |
| Access Internet | n=50 1.0 (0.93, 1.0) | n=87 0.98 (0.92, 1.0) | n=49 0.80 (0.68, 0.89) | <0.001 |
| Video Chat | n=45 0.90 (0.78, 0.97) | n=68 0.76 (0.66, 0.85) | n=28 0.46 (0.33, 0.59) | <0.001 |
| Use Mobile “Apps” | n=50 1.0 (0.93, 1.0) | n=80 0.90 (0.82, 0.95) | n=42 0.69 (0.56, 0.80) | <0.001 |
| Access Health information | n=49 0.98 (0.89, 1.0) | n=81 0.91 (0.83, 0.96) | n=46 0.75 (0.63, 0.86) | 0.001 |
| Track Health information | n=39 0.78 (0.64, 0.88) | n=56 0.63 (0.52, 0.73) | n=12 0.20 (0.11, 0.32) | <0.001 |
Young (age < 45),
Middle-aged (age ≥45 and <65)
Older (aged ≥ 65).
p-value < 0.05 is significant, Pearson chi- square or Fisher’s exact tests
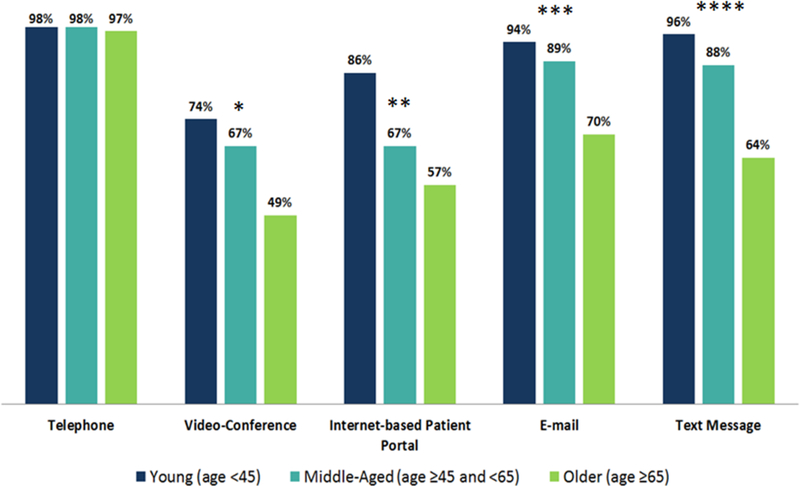
Older women were also significantly less likely than young and middle-aged women to express willingness to communicate with their healthcare providers through mobile technology (video-conference technology p-value = 0.02, Internet-based patient portal p-value = 0.01, e-mail p-value = 0.001 and text message p-value < 0.001.) (Figure 1). However, almost 50% of older women and greater than 65% of middle-aged women were willing to use alternative mobile communication technologies.
Figure 1.
Respondents who are willing to use technology to communicate with their healthcare providers is defined as answering “Strongly agree” or “Agree” with the question “Would you be willing to communicate with your medical provider via…?”.
* p=0.02, ** p=0.01, *** p=0.001, **** p < 0.001; p-values < 0.05 are significant
College graduates were more likely to express willingness to use mobile communication across all alternative technologies. The odds ratio for willingness to use video-conference technology was 2.33 (95%CI 1.28, 4.24, p-value = 0.006), for text messaging 2.58 (95%CI 1.23, 5.42, p-value = 0.012) and for e-mail 4.21 (95%CI 1.88, 9.42, p-value <0.001).
We did not observe any relationship between the distance traveled from the participant’s home to the clinic and their willingness to use various mobile communication technologies (video-conference technology p-value = 0.08, text messaging p-value = 0.21, e-mail p-value = 0.80). Even women who lived within 3 miles of the office expressed a greater than 80% willingness to communicate with their health care provider via video-conference, e-mail or text messaging, while this willingness was greater than 62% among women who lived between 3 and 10 miles, and greater than 59% in those who lived more than 10 miles away from the office.
On multivariable logistic regression, factors that remained significantly associated with willingness to use alternative technologies were age and education level. Older women were significantly less likely to express willingness to use video-conference technology (OR 0.97, 95% CI 0.95, 0.99, p = 0.01), text messaging (OR 0.94, 95% CI 0.91, 0.97, p < 0.001), Internet-based patient portal (OR 0.96, 95% CI 0.94, 0.98, p = 0.001) and e-mail (OR 0.94, 95% CI 0.91, 0.98, p = 0.001). Women with higher education level were significantly more likely to express willingness to communicate via video-conference technology (OR 2.14, 95%CI 1.15, 3.97, p = 0.02) and e-mail (OR 3.73, 95%CI 1.61, 8.67, p = 0.002).
Discussion
We found high levels of ownership of various mobile technologies such as smartphones and tablet devices among women seeking care for pelvic floor disorders across all age groups. The utilization of mobile devices for text messaging and e-mail in daily life was high across all age groups, though younger women were more likely than older women to use technology for video-chats and tracking health-related information. Willingness to use mobile technology to communicate with health care providers was significantly associated with age and education level but not with travel distance to the clinic. Though 75% of older women owned some kind of mobile technology, they were significantly less likely than younger women to express willingness to use such technology to communicate with their health care providers.
Our findings provide important insights to FPMRS providers seeking to incorporate telemedicine into their office practices. Robust telemedicine technology has the ability to not only improve communication with health care providers but also reduce provider burden by allowing patients to directly input their history, symptom questionnaires, and electronic bowel and bladder diaries into their electronic medical records. Our finding that ownership and utilization of mobile technology in women with pelvic floor disorders is high suggests that telemedicine is technologically feasible, at least at the users’ end in FPMRS. Though older women with pelvic floor disorders own mobile technology at lower rates than younger women, ownership of at least one mobile technology device was 75% in this age-group. Furthermore, women with pelvic floor disorders were highly familiar with using technology, with more than 95% of all women and greater than 75% of older women reporting experience in sending emails, text messages or pictures. Finally, women’s willingness to adopt such technology was independent of their distance from the clinic, suggesting that if telemedicine ports are established in FPMRS clinics, adoption of telemedicine among women with pelvic floor disorders is likely to be high.
Given known reduced mobility of older women with urinary and fecal incontinence, telemedicine has the potential to improve communication and reduce caregiver burden in older women with pelvic floor disorders.13,26 Our findings provide insight that could facilitate the adoption of telemedicine by older women with pelvic floors disorders. Even though more than 90% older women reported owning a smart phone, only 49% were willing to communicate using video-conferencing and only 20% reported using health care tracking devices as compared to 63% and 78% in middle-age and younger age groups. This finding is particularly important given the central role of urinary and bowel diaries in tracking symptoms and managing urinary and fecal incontinence. Even after controlling for education level, older age was significantly associated with a decreased willingness to use alternative technologies. Our study did not explore underlying reasons for why older women were less willing to use technology. Prior studies show that older adults are more likely to use technology that has been adapted to accommodate age-related changes in audio-visual perception, motor and cognitive abilities.24 Design elements such as larger font size, increased color contrast and minimal steps to achieve tasks improve usability of technology in older individuals.24 Older adults also benefit from appropriate orientation to the technology and practical hands on training, steps that will be essential not only for facilitating technology-based communication with providers but also for increasing the usability of tablet-based questionnaires and electronic bowel and bladder diaries. Future qualitative studies utilizing focus groups and cognitive interviews will allow for further investigation into successful implementation strategies for these newer technologies.
Our study is limited by the fact that survey respondents were patients seen at urban and suburban clinics of a tertiary academic medical center. It is possible that the technological demographics of a rural or non-academic clinical practice may differ. Additionally, there is a potential for sampling bias due to the fact that study participants only included women who were already seeking care for their pelvic floor disorders. Women who are unable to attend clinic for either mobility or access to care issues were not surveyed. However, the ownership and utilization patterns of technology seen in our study are similar to national trends documented by the Pew Research Center.15 A strength of our study is the wide age range of respondents to our survey. All patients regardless of their chief complaints and familiarity with technology were approached to complete the study which helped to decrease selection bias. This study is also the first report on the use of mobile technology in an FPMRS population.
In conclusion, our study shows that women with pelvic floor disorders across all age groups have high capability of using mobile technology to communicate with their health care providers. Age related differences do exist and older women with pelvic floor disorders may require training and use of technology that has been adapted to their needs. These insights will help clinics and providers develop meaningful telemedicine programs that not only expand access but also provide more patient-centered care that is aligned with the expectations of a more technologically inclined population.
Acknowledgements: None
This study was conducted at the University of Pennsylvania, Philadelphia, PA
Financial support for this project: Dr. Andy is supported by a grant from the National Institute of Aging (R03-AG-053277, PI: Andy). For the remaining authors none were declared.
Footnotes
Disclosure: The authors report no conflict of interest.
Disclaimer: none
REFERENCES
- 1.Bowman GSH,J; Allen S; Webster RA; Thompson DR A telephone survey of medical patients 1 week after discharge from hospital. J Clin Nurs. 1994;3(6):369–373. [DOI] [PubMed] [Google Scholar]
- 2.Cox KW,E Follow-up for people with cancer: nurse-led services and telephone interventions. Journal of Advanced Nursing. 2003;43(1):51–61. [DOI] [PubMed] [Google Scholar]
- 3.Gallagher RM,S; Dracup K Effects of a telephone counseling intervention on psychosocial adjustment in women following a cardiac event. Heart Lung. 2003;32(2):79–87. [DOI] [PubMed] [Google Scholar]
- 4.Harkness KS,KM; Taraba L; Mackenzie CL; Gunn E; Arthur HM Effect of a postoperative telephone intervention on attendance at intake for cardiac rehabilitation after coronary artery bypass graft surgery. Heart Lung. 2005;34(3):179–186. [DOI] [PubMed] [Google Scholar]
- 5.Morgan GJ, Craig B, Grant B, Sands A, Doherty N, Casey F. Home videoconferencing for patients with severe congential heart disease following discharge. Congenital heart disease. 2008;3(5):317–324. [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg DH,K; Wren SM Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair instead of face-to-face clinic visit. JSLS. 2015;19(1):e2014 00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Emerson CG,L; Harper S; Woodruff C Effect of telephone followups on post vasectomy office visits. Urol Nurs. 2000;20(2):125–127, 131. [PubMed] [Google Scholar]
- 8.Fischer KH,V; Jager A; von Allmen D Efficacy and utility of phone call follow-up after pediatric general surgery versus traditional clinic follow-up. Perm. 2015;19(1):11–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hafiji JS,P; Hussain W Patient satisfaction with post-operative telephone calls after Mohs micrographic surgery: a New Zealand and U.K. experience. Br J Dermatol. 2012;167(3):570–574. [DOI] [PubMed] [Google Scholar]
- 10.Hwa KW,SM Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg. 2013;148(9):823–827. [DOI] [PubMed] [Google Scholar]
- 11.Flodgren GR,A; Farmer AJ; Inzitari M; Shepperd S Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015(9):CD002098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greiner AL. Telemedicine Applications in Obstetrics and Gynecology. Clinical obstetrics and gynecology. 2017;60(4):853–866. [DOI] [PubMed] [Google Scholar]
- 13.Fritel X, Lachal L, Cassou B, Fauconnier A, Dargent-Molina P. Mobility impairment is associated with urge but not stress urinary incontinence in community-dwelling older women: results from the Ossebo study. BJOG : an international journal of obstetrics and gynaecology. 2013;120(12):1566–1572. [DOI] [PubMed] [Google Scholar]
- 14.Greer JA, Xu R, Propert KJ, Arya LA. Urinary incontinence and disability in community-dwelling women: a cross-sectional study. Neurourology and urodynamics. 2015;34(6):539–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson M, Perrin A. Tech Adoption Climbs Among Older Adults. Washington, DC: Pew Research Center;2017. [Google Scholar]
- 16.Abelson JS, Symer M, Peters A, Charlson M, Yeo H. Mobile health apps and recovery after surgery: What are patients willing to do? Am J Surg. 2017;214(4):616–622. [DOI] [PubMed] [Google Scholar]
- 17.Serrano KJ, Yu M, Riley WT, et al. Willingness to Exchange Health Information via Mobile Devices: Findings From a Population-Based Survey. Annals of family medicine. 2016;14(1):34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiseman JT, Fernandes-Taylor S, Barnes ML, Tomsejova A, Saunders RS, Kent KC. Conceptualizing smartphone use in outpatient wound assessment: patients’ and caregivers’ willingness to use technology. The Journal of surgical research. 2015;198(1):245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duggan M, Rainie L. Cell Phone Activities 2012. Washington, D.C.: Pew Research Center;2012. [Google Scholar]
- 20.Fox S, Duggan M Mobile Health. Washington, D.C.: Pew Research Center;2012. [Google Scholar]
- 21.Heart T, Kalderon E. Older adults: are they ready to adopt health-related ICT? International journal of medical informatics. 2013;82(11):e209–231. [DOI] [PubMed] [Google Scholar]
- 22.Mazloomdoost D, Kanter G, Chan RC, et al. Social networking and Internet use among pelvic floor patients: a multicenter survey. American journal of obstetrics and gynecology. 2016;215(5):654.e651–654.e610. [DOI] [PubMed] [Google Scholar]
- 23.Olson KE, O’Brien MA, Rogers WA, Charness N. Diffusion of Technology: Frequency of Use for Younger and Older Adults. Ageing international. 2011;36(1):123–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stronge AJ, Rogers WA, Fisk AD. Human factors considerations in implementing telemedicine systems to accommodate older adults. Journal of telemedicine and telecare. 2007;13(1):1–3. [DOI] [PubMed] [Google Scholar]
- 25.Scott G, Lambdin P, Cruse C, Korenda L Deloitte Center for Health Solutions 2016 Survey of US Health Care Consumers. New York, NY: Deloitte Center for Health Solutions;2016. [Google Scholar]
- 26.Johanson JF, Irizarry F, Doughty A. Risk factors for fecal incontinence in a nursing home population. Journal of clinical gastroenterology. 1997;24(3):156–160. [DOI] [PubMed] [Google Scholar]