Abstract
Background:
Yoga is effective for mild to moderate chronic low back pain (cLBP), but its comparative effectiveness with physical therapy (PT) is unknown. Moreover, little is known about yoga’s effectiveness in underserved patients with more severe functional disability and pain.
Objective:
To determine whether yoga is noninferior to PT for cLBP.
Design:
12-week, single-blind, 3-group randomized noninferiority trial and subsequent 40-week maintenance phase. (ClinicalTrials.gov: NCT01343927)
Setting:
Academic safety-net hospital and 7 affiliated community health centers.
Participants:
320 predominantly low-income, racially diverse adults with nonspecific cLBP.
Intervention:
Participants received 12 weekly yoga classes, 15 PT visits, or an educational book and newsletters. The maintenance phase compared yoga drop-in classes versus home practice and PT booster sessions versus home practice.
Measurements:
Primary outcomes were back-related function, measured by the Roland Morris Disability Questionnaire (RMDQ), and pain, measured by an 11-point scale, at 12 weeks. Prespecified noninferiority margins were 1.5 (RMDQ) and 1.0 (pain). Secondary outcomes included pain medication use, global improvement, satisfaction with intervention, and health-related quality of life.
Results:
One-sided 95% lower confidence limits were 0.83 (RMDQ) and 0.97 (pain), demonstrating noninferiority of yoga to PT. However, yoga was not superior to education for either outcome. Yoga and PT were similar for most secondary outcomes. Yoga and PT participants were 21 and 22 percentage points less likely, respectively, than education participants to use pain medication at 12 weeks. Improvements in yoga and PT groups were maintained at 1 year with no differences between maintenance strategies. Frequency of adverse events, mostly mild self-limited joint and back pain, did not differ between yoga and PT.
Limitations:
Participants were not blinded to treatment assignment. The PT group had disproportionate loss to follow-up.
Conclusion:
A manualized yoga program for nonspecific cLBP was noninferior to PT for function and pain.
Low back pain is the leading cause of disability globally (1). Total annual back pain–related costs in the United States are greater than $200 billion (2). Chronic low back pain (cLBP) affects approximately 10% of U.S. adults (3), but overall patient satisfaction with cLBP treatment is low (4). The impact of cLBP is greater in racial or ethnic minorities and in people of lower socioeconomic status (SES) (5). Physical therapy (PT), comprising individually tailored stretching and strengthening exercises, is the most common evidence-based, reimbursable, and nonpharmacologic physician referral for cLBP (6, 7). Clinical guidelines (8, 9), meta-analyses (10), and several large randomized controlled trials (11–13) also support yoga, a practice including physical poses, breathing exercises, and meditation, as an effective cLBP treatment.
To improve cLBP care, physicians, patients, and payers need to know how novel therapies like yoga compare with established treatments like PT. Noninferiority trials determine if a new therapy is statistically as effective as an accepted treatment (14). This is particularly useful when the new therapy may have other potential benefits, such as lower cost. The U.S. Food and Drug Administration uses noninferiority as one criterion for approving new pharmaceuticals (15). Although no criteria have been established for when a new nonpharmacologic therapy should be integrated into mainstream clinical practice, demonstrating noninferiority to effective, reimbursed, and nonpharmacologic treatments is one reasonable requirement. Thus, we conducted a randomized controlled comparative effectiveness trial testing whether yoga was noninferior to PT in adults with cLBP.
Methods
Design Overview
The study protocol (16) and treatment manuals (17–20) were published previously. We conducted a 52-week, assessor-blinded randomized trial of yoga, PT, and education (a self-care book and newsletters) for adults with nonspecific cLBP. The study was advertised as a comparison of 3 credible cLBP treatments. All participants had access to usual medical care. The study consisted of a 12-week treatment phase and 40-week maintenance phase. The primary hypothesis was that yoga is noninferior to PT in the treatment phase for improving both back-related function and pain intensity. The secondary hypothesis was that both yoga and PT are superior to education for improving function and pain.
The maintenance phase compared the effectiveness of different strategies for ongoing yoga and PT. Yoga participants who completed 1 or more yoga classes in the treatment phase were randomly assigned at 12 weeks to yoga drop-in classes or home practice. Physical therapy patients who completed 1 or more PT appointments in the treatment phase were randomly assigned to PT booster sessions or home practice. We hypothesized that at 52 weeks, yoga drop-in classes are superior to yoga home practice and PT booster sessions are superior to PT home practice.
Study recruitment occurred from June 2012 to November 2013. Follow-up was completed in November 2014. The original research protocol and a summary of protocol changes are in Supplement 1 (available at Annals.org).
Setting and Participants
The study occurred at a large academic safety-net hospital and 7 affiliated, federally qualified community health centers located in diverse neighborhoods. Staff doing data collection, entry, and analysis were masked to treatment assignment. The Boston University Institutional Review Board approved the study before data collection.
We enrolled English-speaking adults aged 18 to 64 years who reported nonspecific low back pain lasting at least 12 weeks with an average pain intensity in the previous week of 4 or greater on an 11-point (0 to 10) numerical rating scale. Persons with specific causes of cLBP (for example, spinal stenosis) were excluded. Eligibility criteria are in Table 1 of Supplement 2 (available at Annals.org). Recruitment strategies included clinician referrals, mailing letters to patients with cLBP who were identified through electronic health records, and distributing flyers in clinics and surrounding neighborhoods.
Randomization and Interventions
After initial telephone screening, staff confirmed eligibility and obtained written informed consent during in-person meetings. Staff entered participants into StudyTRAX (ScienceTrax), a data management platform. StudyTRAX generated a randomization sequence using permuted block randomization with varying block sizes and a 2:2:1 ratio of yoga, PT, and education. After participants completed baseline surveys, unmasked staff informed them of their treatment assignments. Enrollment and randomization proceeded in 4 sequential cohorts of approximately 80 participants each.
Yoga participants who attended at least 1 class in the treatment phase continued into the maintenance phase and were randomly assigned to weekly drop-in yoga classes or home practice only. Physical therapy participants with at least 1 PT visit in the treatment phase were randomly assigned to attend 5 booster sessions or home practice only during the maintenance phase. Education participants continued into the maintenance phase without additional randomization.
A manualized yoga protocol (18) of 12 weekly 75-minute classes was adapted from previous studies in similar populations (21, 22) with input from expert yoga instructors, investigators, and former study participants (Table 2 of Supplement 2). Thirteen yoga instructors completed 8 hours of training and taught classes at 6 sites. Instructor assignments ensured a participant–instructor ratio of less than 5:1. Each class began with relaxation and meditation exercises, yoga breathing, and yoga philosophy. It continued with yoga poses and concluded with relaxation. Pose variations and aids (such as chair, strap, and blocks) accommodated various abilities. Thirty minutes of daily home practice, facilitated by a DVD, a manual, and take-home yoga supplies, was strongly encouraged. Participants recorded time spent practicing. Staff observed approximately 10% of classes to assess protocol fidelity by using a checklist. Maintenance phase classes were similarly structured except for a higher participant–instructor ratio (approximately 8:1).
The manualized PT protocol (Figure 1 and Table 3 of Supplement 2) incorporated treatment-based classification (23, 24), graded exercise (25), and screening for fear-avoidance beliefs (26). Eight physical therapists delivered the intervention in 1 hospital-based and 2 community-based PT clinics. Physical therapists completed 8 hours of in-person training and Web-based modules (27). Participants were advised to attend fifteen 60-minute appointments over 12 weeks. Appointments included one-on-one work with the therapist and supervised aerobic exercise. All participants completed the Fear-Avoidance Beliefs Questionnaire (28). For PT participants with a high fear-avoidance score (≥29 on the work subscale), therapists provided The Back Book (29) and reinforced its psychologically informed principles to lower fear avoidance. Participants received written instructions and supplies for home practice and logged the number of exercises completed daily. Staff assessed protocol fidelity by reviewing therapists’ treatment flowsheets. Participants randomly assigned to booster sessions during the maintenance phase were advised to see the therapist at 4, 6, 8, 10, and 12 months.
Education participants received The Back Pain Helpbook (30), which includes information on cLBP self-management, stretching, strengthening, and the role of emotions and fear avoidance. Previous cLBP trials (11, 12, 31) used this book as a credible control intervention. We provided a recommended reading schedule (Table 4 of Supplement 2). Every 3 weeks, participants received 1- to 2-page newsletters (32) summarizing main points from assigned chapters and 5- to 10-minute check-in calls from staff. In the maintenance phase, we made brief check-in calls every 6 weeks to encourage continuing review of the book.
Outcomes and Follow-up
Coprimary outcomes were change from baseline to 12 weeks in scores on the modified Roland Morris Disability Questionnaire (RMDQ; a 23-point measure of back-related function with higher scores indicating worse function) (33) and in pain (using an 11-point numerical rating scale for average intensity in the previous week, where 0 indicated no pain and 10 indicated worst pain possible) (34). Secondary outcomes included self-reported pain medication use in the previous week (yes or no), global improvement (7-point scale from extremely worsened to extremely improved), patient satisfaction with interventions (5-point scale from very dissatisfied to very satisfied) (35), and health-related quality of life (Short Form-36 Health Survey) (36). We collected data on work productivity, a secondary outcome, and will report them separately in a cost-effectiveness analysis. We also plan to report data on other exploratory measures collected (such as fear-avoidance beliefs, pain self-efficacy, depression, anxiety, and sleep) separately. Attendance to all yoga and PT sessions was recorded. Participants attending at least 9 yoga or 11 PT sessions (≥75% or ≥73% of sessions, respectively) were defined as adherent a priori. Education participants were asked how much of the book they had read. Those reporting having read at least 75% were defined as adherent a priori.
After baseline data collection, study staff masked to treatment assignment collected paper surveys completed at 6, 12, 26, 40, and 52 weeks. Adverse events were elicited directly from participants and in surveys. Participants received $100 gift cards after completing surveys at 12 and 52 weeks and $50 gift cards after the baseline questionnaire and surveys at 6, 26, and 40 weeks.
Statistical Analysis
The study was designed and powered to detect if yoga was noninferior to PT at 12 weeks for both primary outcomes. Noninferiority margins were prespecified for RMDQ (1.5) and pain (1.0) by halving the minimal clinically important difference (37). Although some controversy exists about the minimal clinically important difference for RMDQ (38, 39) and back pain intensity (40, 41), 3.0 and 2.0, respectively, are reasonable and commonly used. Because we required noninferiority for both primary outcomes, adjustment for multiple testing was unnecessary. Assuming 20% attrition and previously published variances (11, 12), the target sample size of 320 provided 81% and 90% power to detect noninferiority at 12 weeks of yoga to PT for function and pain, respectively.
We used analysis of variance and chi-square tests to assess between-group differences in baseline variables. For coprimary outcomes during the treatment phase, we did 1-sided 2-sample t tests to determine whether yoga was noninferior to PT for change from baseline to 12 weeks. We controlled for potential confounders, defined a priori by a baseline imbalance between groups (P < 0.10), by using multiple linear regression. To comply with the journal editors’ recommendations for handling missing data in our primary outcome analyses, we present findings based on multiple imputation using regression modeling in SAS PROC MI. Variables used in the imputation were treatment group, baseline values, and week-6 scores. Any missing week-6 values were imputed before imputation for week-12 values. Ten imputed data sets were created. Using these, the analysis for back pain score was unadjusted, whereas the analysis of RMDQ was adjusted for baseline RMDQ. Analyses using the last observation carried forward, our prespecified approach for handling missing values, are presented in Supplement 2.
For secondary outcomes, we used the last observation carried forward to manage missing data and did not adjust for multiple testing. We did 2-sided 2-sample t tests to determine whether yoga and PT were superior to education. We also performed responder analyses comparing the proportion of participants in each group with clinically meaningful change (≥30% decrease from baseline to 12 weeks) (40). Self-reported pain medication use at 12 weeks (any vs. none) and medication subtypes (nonsteroidal anti-inflammatory drugs, acetaminophen, or opioids) were examined using logistic regression adjusted for baseline use. Global improvement, patient satisfaction, and health-related quality of life were compared using multiple linear regression. Per-protocol analyses of the treatment phase included participants meeting a priori definitions of adherence. Adverse events were compared using the Fisher exact test.
For the maintenance phase, we did longitudinal analyses with a 5-part treatment variable (yoga drop-in classes, yoga home practice, PT booster sessions, PT home practice, and education), incorporating all RMDQ and pain measurements from weeks 12 to 52 (42). The general linear model for correlated data using SAS PROC MIXED with a repeated statement was used with an unstructured covariance and a treatment-by-time interaction examining differences in patterns over time. Specific hypotheses were tested using contrasts. Missing data points were not replaced.
All analyses were performed with SAS, version 9.3 (SAS Institute).
Results
Study Population
From June 2012 to November 2013, we screened 1663 people. Of these, 479 (29%) met eligibility criteria and 320 (19%) were enrolled and randomly assigned to yoga, PT, or education (Figure 2 and Table 5 of Supplement 2). Most study participants were women, were nonwhite, were not college graduates, and were earning $30,000 or less annually (Table 1; Table 6 of Supplement 2). On average, participants reported moderate to severe functional impairment and pain. More than two thirds used analgesics for back pain. Baseline mean between-group differences were present for RMDQ, sex, and body mass index (P = 0.032, 0.088, and 0.099, respectively). However, only baseline RMDQ was identified as a confounder for the RMDQ analyses.
Table 1.
Demographic and Baseline Characteristics of All Participants, by Treatment Group*
| Characteristic† | Yoga (n = 127) |
Physical Therapy (n = 129) |
Education (n = 64) |
|---|---|---|---|
| Mean age (SD), y | 46.4 (10.4) | 46.4 (11.0) | 44.2 (10.8) |
| Female | 72 (56.7) | 90 (69.8) | 42 (65.6) |
| Race or ethnic group | |||
| Non-Hispanic white | 26 (20.5) | 20 (15.5) | 11 (17.2) |
| Non-Hispanic black | 71 (55.9) | 73 (56.6) | 39 (60.9) |
| Hispanic | 18 (14.2) | 19 (14.7) | 7 (10.9) |
| Other/missing | 12 (9.4) | 17 (13.2) | 7 (10.9) |
| Born in the United States | 91 (71.7) | 84 (65.1) | 51 (79.7) |
| Earned college degree or higher | 38 (29.9) | 30 (23.3) | 25 (39.1) |
| Currently employed | 60 (47.2) | 53 (41.1) | 30 (46.9) |
| Annual income ≤$30 000 | 76 (59.8) | 71 (55.0) | 41 (64.1) |
| Mean BMI (SD), kg/m2 | 30.8 (6.7) | 32.7 (7.4) | 32.0 (8.1) |
| Mean back pain intensity (SD) | 7.1 (1.5) | 7.2 (1.5) | 7.0 (1.4) |
| Mean RMDQ score (SD)‡ | 13.9 (5.6) | 15.6 (5.1) | 15.0 (5.0) |
| Used any pain medication in previous week | 88 (69.3) | 94 (72.9) | 47 (73.4) |
| NSAIDs | 63 (49.6) | 71 (55.0) | 37 (57.8) |
| Acetaminophen | 43 (33.9) | 41 (31.8) | 26 (40.6) |
| Opioids | 28 (22.1) | 23 (17.8) | 12 (18.7) |
| Very satisfied with overall care for back pain | 5 (4.0) | 4 (3.1) | 1 (1.6) |
| Comorbidities | |||
| Hypertension | 42 (34.4) | 46 (36.5) | 23 (36.5) |
| Neck pain | 41 (34.2) | 29 (23.8) | 23 (35.9) |
| Pulmonary disorders§ | 30 (23.8) | 31 (24.2) | 18 (28.1) |
| Diabetes | 25 (19.8) | 25 (19.5) | 8 (13.1) |
| Depression | 21 (16.9) | 33 (26.8) | 12 (19.7) |
| Mean SF-36 physical health score (SD)∥ | 36.2 (8.8) | 35.2 (7.7) | 36.6 (8.5) |
| Mean SF-36 mental health score (SD)∥ | 43.4 (12.8) | 41.4 (10.2) | 42.3 (10.5) |
BMI = body mass index; NSAID = nonsteroidal anti-inflammatory drug; RMDQ = Roland Morris Disability Questionnaire; SF-36 = Short Form-36 Health Survey.
All values are numbers (percentages) unless otherwise specified. Percentages may not sum to 100 because of rounding. Height and weight were measured at the baseline survey visit. All other characteristics were self-reported. Additional baseline characteristics are provided in Table 6 of Supplement 2 (available at Annals.org).
Baseline between-group differences were present for sex, RMDQ, and BMI (P = 0.088, 0.032, and 0.099, respectively).
Measured using an 11-point numerical rating scale for average pain intensity in the previous week, where 0 indicated no pain and 10 indicated worst pain possible.
Measure of back-related function with scores ranging from 0 to 23, where higher scores represent poorer function.
Include chronic obstructive pulmonary disease, chronic bronchitis, asthma, and emphysema.
Scores range from 0 to 100, with higher scores indicating better health-related quality of life
Adherence to Interventions and Loss to Follow-up
During the treatment phase, median yoga attendance was 7 classes (interquartile range, 3 to 10). Median PT attendance was 7 appointments (interquartile range, 2 to 12). Home practice was reported by 95 yoga participants (75%) and 83 PT participants (64%). Of these, yoga participants practiced a median of 27 minutes (interquartile range, 17 to 35 minutes) 4 days per week. Physical therapy participants did a median of 4 exercises (interquartile range, 3 to 5) 4 days per week. Fewer than half of the participants met adherence criteria: 56 yoga (44%), 46 PT (36%), and 28 education (44%) participants. Of 59 participants randomly assigned to yoga drop-in classes during the maintenance phase, 31 (53%) attended at least 1 drop-in class (median, 13; interquartile range, 4 to 22). Of 54 participants randomly assigned to PT booster sessions, 30 (56%) attended at least 1 appointment (median, 2; interquartile range, 1 to 3). Follow-up was lower in PT than in yoga or education at 12 weeks (88% vs. 98% and 95%, respectively) and 52 weeks (84% vs. 93% and 93%, respectively).
Primary Outcomes
Improvement in RMDQ for yoga (mean within-group change, −3.8 [95% CI, −4.6 to −2.9]) was noninferior to that for PT (mean within-group change, −3.5 [CI, −4.5 to −2.6]) (Table 2 and Figure). The mean difference in RMDQ between yoga and PT was −0.26 (1-sided CI, −∞ to 0.83). Decreased pain for yoga (mean within-group change, −1.7 [CI, −2.1 to −1.4]) was noninferior to that for PT (mean within-group change, −2.3 [CI, −2.7 to −1.9]). The mean difference in pain between yoga and PT was 0.51 (1-sided CI, −∞ to 0.97). Noninferiority plots for primary outcomes are shown in Figure 3 of Supplement 2. Analyses using the last observation carried forward to account for missing data yielded similar results (Table 7 of Supplement 2).
Table 2.
Primary Outcomes at 12 Weeks*
| Mean Between-Group Difference | ||||||
|---|---|---|---|---|---|---|
| Variable | Yoga | Physical Therapy |
Education | Yoga vs. Physical Therapy |
Yoga vs. Education |
Physical Therapy vs. Education |
| Participants analyzed, n† | 127 | 129 | 64 | - | - | - |
| RMDQ score‡ | ||||||
| Mean score (SD) | 11.0 (4.9) | 11.3 (5.1) | 12.3 (5.0) | - | - | - |
| Mean change from baseline (95% CI) | −3.8 (−4.6 to −2.9) | −3.5 (−4.5 to −2.6) | −2.5 (−3.8 to −1.3) | −0.26 (−∞ to 0.83) | −1.3 (−2.8 to 0.25) | −1.0 (−2.6 to 0.79) |
| Back pain intensity score§ | ||||||
| Mean score (SD) | 5.3 (2.1) | 5.0 (2.1) | 5.6 (2.2) | - | - | - |
| Mean change from baseline (95% CI) | −1.7 (−2.1 to −1.4) | −2.3 (−2.7 to −1.9) | −1.4 (−2.0 to −0.9) | 0.51 (−∞ to 0.97) | −0.33 (−0.97 to 0.32) | −0.84 (−1.5 to −0.18) |
RMDQ = Roland Morris Disability Questionnaire.
Intention-to-treat analyses of the full study population used multiple imputation to account for missing data at 6 and/or 12 weeks.
Because multiple imputation was used for the primary analyses, the number of participants analyzed included the entire sample with baseline data.
Scores range from 0 to 23, with higher scores reflecting poorer back-related function. Mean changes in RMDQ scores are based on models adjusted for baseline RMDQ only. Sex and body mass index were assessed for potential confounding using multiple regression models and were found not to substantively change the results.
Measured using an 11-point numerical rating scale for average pain intensity in the previous week, where 0 indicated no pain and 10 indicated worst pain possible.
Sex, body mass index, and baseline RMDQ were assessed for potential confounding of back pain intensity score and found not to substantively change the results. Results presented are therefore unadjusted.
Figure. Primary outcomes from baseline to 52 weeks.
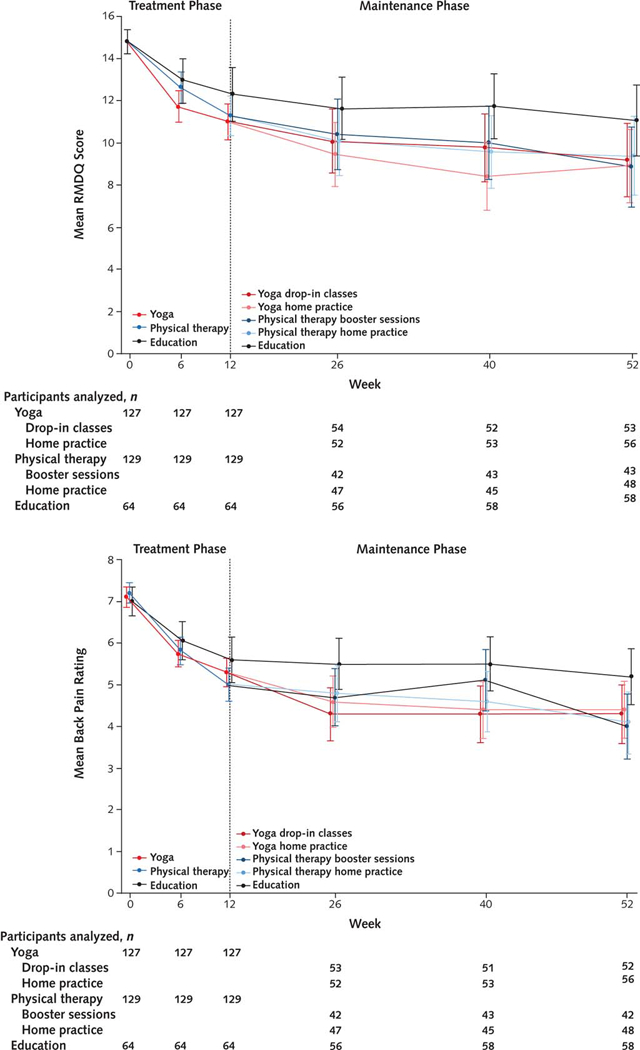
The study was divided into a treatment phase (baseline to 12 weeks) and maintenance phase (12 to 52 weeks). Intention-to-treat analyses are shown. Plotted values in the treatment phase derive from models using multiple imputation to handle missing data. Values in the maintenance phase derive from longitudinal models using all available data. 95% CIs are shown. Data points are slightly offset from each other to aid interpretation. RMDQ = Roland Morris Disability Questionnaire. Top. Mean RMDQ scores adjusted for baseline scores and anchored at the study population mean at baseline. Bottom. Mean unadjusted back pain scores.
Secondary and Exploratory Outcomes
Yoga and PT were not superior to education at 12 weeks for RMDQ (Table 2). However, both yoga and PT were more likely than education to have clinically meaningful responses in RMDQ (Table 3). Forty-eight percent of yoga participants versus 23% of education participants responded (odds ratio, 3.1 [CI, 1.6 to 6.2]). Thirty-seven percent of PT participants responded (odds ratio [vs. education], 2.0 [CI, 1.0 to 4.0]). For pain, yoga was not superior to education (mean between-group difference, −0.33 [CI, −0.97 to 0.32]) but PT was (mean between-group difference, −0.84 [CI, −1.5 to −0.18]). The only significant between-group difference in clinically meaningful response in pain was in the PT group compared with education (43% vs. 25%; odds ratio, 2.3 [CI, 1.1 to 4.5]).
Table 3.
Secondary Outcomes at 12 Weeks*
| Odds Ratio (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Variable | Yoga | Physical Therapy |
Education | Yoga vs. Physical Therapy |
Yoga vs. Education |
Physical Therapy vs. Education |
| Clinically meaningful response | ||||||
| Participants analyzed, n | 125 | 113 | 61 | – | – | – |
| ≥30% reduction in RMDQ, n (%) | 60 (48.0) | 42 (37.2) | 14 (23.0) | 1.6 (0.93 to 2.6) | 3.1 (1.6 to 6.2) | 2.0 (1.0 to 4.0) |
| ≥30% reduction in back pain, n (%) | 44 (35.2) | 48 (42.5) | 15 (24.6) | 0.74 (0.44 to 1.2) | 1.7 (0.84 to 3.3) | 2.3 (1.1 to 4.5) |
| Use of pain medication in previous week | ||||||
| Participants analyzed, n | 124 | 110 | 61 | – | – | – |
| Any pain medication, n (%) | 68 (54.8) | 59 (53.6) | 46 (75.4) | 1.2 (0.66 to 2.1) | 0.36 (0.17 to 0.78) | 0.31 (0.14 to 0.67) |
| Acetaminophen, n (%) | 41 (33.1) | 24 (21.8) | 24 (39.3) | 1.9 (1.0 to 3.7) | 0.87 (0.42 to 1.8) | 0.45 (0.21 to 0.97) |
| NSAIDs, n (%) | 41 (33.1) | 47 (42.7) | 29 (47.5) | 0.65 (0.36 to 1.2) | 0.56 (0.28 to 1.1) | 0.85 (0.42 to 1.7) |
| Opioids, n (%) | 28 (22.6) | 15 (13.6) | 11 (18.0) | 2.4 (0.95 to 5.8) | 1.5 (0.53 to 4.3) | 0.64 (0.21 to 1.9) |
| Self-rated global improvement§ | ||||||
| Participants analyzed, n | 124 | 112 | 61 | – | – | – |
| Improved, n (%) | 42 (33.9) | 47 (42.0) | 13 (21.3) | 0.71 (0.42 to 1.2) | 1.9 (0.92 to 3.9) | 2.7 (1.3 to 5.5) |
| Satisfaction with intervention∥ | ||||||
| Participants analyzed, n | 125 | 113 | 61 | – | – | – |
| Very satisfied, n (%) | 54 (43.2) | 56 (49.6) | 13 (21.3) | 0.77 (0.46 to 1.3) | 2.8 (1.4 to 5.7) | 3.6 (1.8 to 7.4) |
|
Between-Group Mean Difference (95% CI) |
||||||
| SF-36 physical health score¶ | ||||||
| Participants analyzed, n | 125 | 112 | 61 | – | – | – |
| Mean score (SD) | 41.4 (8.6) | 40.1 (9.0) | 41.2 (9.0) | – | – | – |
| Mean change from baseline (95% CI) | 5.1 (3.7 to 6.5) | 5.0 (3.6 to 6.5) | 4.5 (3.0 to 6.0) | 0.11 (−1.9 to 2.1) | 0.62 (−1.6 to 2.9) | 0.51 (−1.8 to 2.8) |
| SF-36 mental health score¶ | ||||||
| Participants analyzed, n | 125 | 112 | 61 | – | – | – |
| Mean score (SD) | 47.1 (12.4) | 45.2 (11.7) | 44.2 (11.9) | – | – | – |
| Mean change from baseline (95% CI) | 3.3 (1.6 to 5.0) | 3.5 (1.6 to 5.5) | 1.8 (−0.90 to 4.5) | −0.19 (−2.8 to 2.4) | 1.5 (−1.7 to 4.7) | 1.7 (−1.6 to 5.0) |
NSAID = nonsteroidal anti-inflammatory drug; RMDQ = Roland Morris Disability Questionnaire; SF-36 = Short Form-36 Health Survey.
All secondary outcome analyses used the last observation carried forward (when available at 6 weeks) to account for missing data at 12 weeks. Number of participants analyzed includes those with week-6 or week-12 values. All secondary outcome analyses are unadjusted except for pain medication use, which was adjusted for baseline use. Adjustment for baseline RMDQ did not substantively change the results of clinically meaningful response rates.
Rated on a 0- to 6-point Likert scale, where 0 indicated extremely worsened, 3 indicated no change, and 6 indicated extremely improved. Participants who reported a 5 or 6 were considered improved.
Rated on a 5-point Likert scale from very dissatisfied to very satisfied.
Scores range from 0 to 100, with higher scores indicating better health-related quality of life.
At 12 weeks, yoga and PT participants were 21 and 22 percentage points, respectively, less likely than education participants to use any pain medication (Table 3). Although PT participants were less likely than education participants to use acetaminophen, there were no other significant differences in medication subgroups. Self-rated global improvement and satisfaction with the intervention did not significantly differ between yoga and PT. Global improvement for PT, but not for yoga, was superior to that for education. Satisfaction with yoga and PT were both superior to that with education. No significant between-group differences were seen in Short Form-36 Health Survey scores.
Given the low proportion of participants meeting prespecified adherence criteria (36% to 44%), per-protocol between-group comparisons are highly susceptible to bias and are not presented. However, mean within-group RMDQ changes for adherent participants at 12 weeks were −4.6, −5.7, and −2.7 for yoga, PT, and education, respectively (Table 8 of Supplement 2). Clinically meaningful improvement in RMDQ scores occurred in 57%, 56%, and 21% of participants, respectively. For pain intensity at 12 weeks, mean within-group changes for adherent participants were −2.1, −2.6, and −1.3 for yoga, PT, and education, respectively. Clinically meaningful improvement in pain intensity occurred in 50%, 52%, and 14% of participants, respectively.
In the maintenance phase, RMDQ or pain changes did not significantly differ between yoga drop-in classes and yoga home practice or between PT booster sessions and PT home practice (Figure; Tables 9 and 10 of Supplement 2).
Adverse Events
Adverse events, mostly mild self-limited joint and back pain, were reported in 9 yoga, 14 PT, and 1 education participants. Yoga and PT did not differ significantly in frequency or severity of related adverse events (Table 11 of Supplement 2).
Discussion
In a trial of yoga, PT, and education for predominantly low-income, racially diverse participants with moderate to severe nonspecific cLBP, intention-to-treat analyses found that a 12-week standardized yoga class was noninferior to individually delivered PT for change in back-related function and pain. Our secondary hypothesis, that yoga is superior to education for both function and pain, was not supported. However, participants in both yoga and PT were more likely to have clinically meaningful improvements in function than were education participants. Yoga and PT participants were also more likely than education participants to discontinue pain medication. Improvements in yoga and PT groups were maintained at 1 year regardless of whether patients were assigned to ongoing yoga classes, PT booster sessions, or home practice only. All interventions were relatively safe.
Compared with previous trials of yoga for cLBP (11–13), our trial enrolled a more racially diverse, lower SES population. For example, Sherman and colleagues’ study of yoga, stretching classes, and education recruited 228 patients with cLBP, 87% of whom were white, 62% college graduates, and 84% with incomes greater than $45 000 (12). Research has documented racial and socioeconomic disparities in disability and pain (5). Minorities with back pain receive fewer specialty referrals (43) and less-intensive rehabilitation for occupational back injuries (44) than do whites. Despite pain’s disproportionate impact on minority and low SES groups, few cLBP studies and even fewer yoga and PT trials have targeted these populations. Barriers exist for low-income minorities to access nonpharmacologic treatments, such as yoga and PT. Non-Hispanic white adults are twice as likely as non-Hispanic black adults to use yoga (45). Yoga classes are often unavailable in predominantly low-income minority neighborhoods, and fees can be prohibitive (46). People with higher education are more likely to receive PT; people covered by Medicaid are less likely (47). Some insurance plans require expensive PT copayments that may deter patient access (48).
In Sherman and colleagues’ study, yoga classes and stretching classes were superior to the same self-care book used in our study (12). Although both our study and Sherman and colleagues’ study found similar improvement for patients who used the book (for example, −2.5 vs. −2.2 for RMDQ), our yoga intervention did not perform as well (for example, −3.8 vs. −5.2 for RMDQ). One possible explanation for the modest effect of yoga and PT in our trial is lower adherence. Our yoga participants attended a median of 7 classes compared with 10 in Sherman and colleagues’ trial. This can be attributed in part to obstacles often facing lower SES populations, including inconsistent telephone service, difficulties with transportation, serious illnesses and injuries in family members, conflicting life demands (such as work, child care, and elder care), homelessness, and incarceration (49). The greater effect of yoga and PT among our adherent patients highlights the challenges and importance of compliance in exercise interventions (50). Another reason for the modest effect of our interventions may be the severity of our participants’ back conditions. Baseline mean back-related disability and pain scores were 63% and 57% more severe, respectively, in our study than in Sherman and colleagues’ study. Opioid use, obesity, depression, and other comorbid conditions were also more common.
Strengths of this study include an assessor-blinded randomized design, adequate power to assess noninferiority of yoga to PT at 12 weeks, and standardized interventions delivered by providers in community-based settings. Although blinding of participants in nonpharmacologic trials is not possible, we presented the study as comparing 3 credible treatments. Limitations include disproportionate loss to follow-up for PT. This attrition bias could increase or decrease the observed effectiveness of PT depending on the likelihood of dropouts doing worse or better than those with follow-up. Mean baseline RMDQ, a coprimary outcome, modestly differed between groups and required adjustment. The lack of difference between maintenance phase groups is difficult to interpret because only approximately half of eligible participants attended any yoga drop-in classes or PT booster sessions. Per-protocol analyses were not powered to assess noninferiority and should be interpreted with caution. Because the per-protocol population is a subgroup, differences between adherent and nonadherent participants may confound the analyses. In addition, analyses for change in use of medication subtypes, such as opioids or nonsteroidal anti-inflammatory drugs, were underpowered.
These findings suggest that a manualized yoga intervention designed specifically for cLBP is similarly effective to PT for improving physical function and reducing pain in a diverse underserved population with high levels of impairment. These results are likely generalizable to other safety-net settings and to less-impaired, higher-SES patients. However, the results may not generalize to typical nonmanualized, community-based yoga classes. Similarly, our education intervention was more time-intensive than typical office-based education and therefore was probably more effective. Future studies should focus on pragmatic trials of nonmanualized yoga classes, testing of strategies to enhance adherence, and cost-effectiveness analyses.
In conclusion, we found that yoga was noninferior to PT for improving moderate to severe nonspecific cLBP in a diverse, predominantly low-income population. Yoga and PT participants had greater improvement in function and pain than education participants; however, these differences were not uniformly significant. Yoga and PT participants were more likely than education participants to stop their pain medication. The effectiveness of yoga and PT was most evident in adherent participants. Improvements in yoga and PT were maintained at 1 year, and all interventions were relatively safe. A structured yoga program for patients with cLBP may be a reasonable alternative to PT depending on patient preferences, availability, and cost.
Presented in part at the following events: International Congress on Complementary Medicine Research, Jeju, Republic of Korea, 14 May 2015; International Congress on Integrative Medicine and Health, Henderson, Nevada, 17 May 2016; International Back and Neck Pain Forum, Buxton, United Kingdom, 1 June 2016; Academy of Integrative Pain Management, San Antonio, Texas, 24 September 2016; and North American Spine Society, Boston, Massachusetts, 28 October 2016.
Supplementary Material
Acknowledgment:
The authors thank the study yoga instructors (Deidre Alessio, Julie Aronis, Sylvia Baedorf-Kassis, Lisa Cahill, Karen Cullen, Danielle Ciofani, Monica Delgado Chafee, Anna Dunwell, Victoria Garcia Drago, Amy Goh, Beth Kacel, Robert Montgomery), Boston Medical Center Department of Physical Therapy (Jenn Blake, Daniel Chapman, Ryan Diloreti, Alysse Ferranto, Karen Mattie, James Mergel), New England Physical Therapy Plus (Bill Sullivan, Anisha Patel, Megan Poletto, Steven Smith, Steve Buerhing, David Cunningham), study site champions (Aram Kaligian, Stephen Tringale, Yen Loh, Ani Tahmassian, Nandini Sengupta, Barbara Lottero, Dan Simpson), the Data and Safety Monitoring Board (Deborah Cotton, Bei-Hung Chang, John Denninger, Maya Breuer), and the research staff at Boston Medical Center (Sarah Baird, Katelin Blackburn, Morgan Ford, Dan Do, Emir Duhovic, Sheba Ebhote, Shayna Egan, Calvin Fong, Elvin Fontana-Martinez, Shirley Gillies, Margo Godersky, Molly Lawrence, Sarah Marchese, Alison Marshall, Taylor Mazac, Matthew Mcgrath, Marilly Palettas, Bryan Rodriguez, Michael Roxas, Kaori Sato, Darshan Shastri, Alison Smith, Huong Tran, Kristen Trimble). They also thank the study participants and staff of Boston Medical Center, Codman Square Health Center, Dimock Center, DotHouse Health, Greater Roslindale Medical & Dental Center, South Boston Community Health Center, South End Community Health Center, and Upham’s Corner Health Center.
Grant Support: By grant 5R01-AT005956 from the National Center for Complementary and Integrative Health of the National Institutes of Health.
Primary Funding Source: National Center for Complementary and Integrative Health of the National Institutes of Health.
Role of the Funding Source
This study was funded by the National Center for Complementary and Integrative Health. This agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Disclaimer: The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Complementary and Integrative Health.
Note: Drs. Saper and Weinberg had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosures:
Reproducible Research Statement: Study protocol: See Supplement 1 (available at Annals.org). Statistical code: Not available. Data set: Available to approved individuals through a written data-sharing agreement with Dr. Saper (e-mail, robert.saper@bmc.org).
Contributor Information
Robert B. Saper, Department of Family Medicine, Boston Medical Center, 1 Boston Medical Center Place, Dowling 5 South, Boston, MA 02118..
Chelsey Lemaster, Department of Family Medicine, Boston Medical Center, 1 Boston Medical Center Place, Dowling 5 South, Boston, MA 02118..
Anthony Delitto, School of Health and Rehabilitation Sciences, University of Pittsburgh, 4029 Forbes Tower, Pittsburgh, PA 15260..
Karen J. Sherman, Center for Health Studies, Group Health Cooperative, 1730 Minor Avenue, Suite 1600, Seattle, WA 98101..
Patricia M. Herman, RAND Corporation, 1776 Main Street, PO Box 2138, Santa Monica, CA 90407..
Ekaterina Sadikova, Department of Health Care Policy, Harvard Medical School, 180 Longwood Avenue, Boston, MA 02115..
Joel Stevans, School of Health and Rehabilitation Sciences, University of Pittsburgh, 4029 Forbes Tower, Pittsburgh, PA 15260..
Julia E. Keosaian, Section of General Internal Medicine, Boston Medical Center, Crosstown Center, 801 Massachusetts Avenue, 2nd Floor, Boston, MA 02118..
Christian J. Cerrada, Soto Street Building, SSB 1, 2001 North Soto Street, Los Angeles, CA 90032..
Alexandra L. Femia, Department of Family Medicine, Boston Medical Center, 1 Boston Medical Center Place, Dowling 5 South, Boston, MA 02118..
Eric J. Roseen, Department of Family Medicine, Boston Medical Center, 1 Boston Medical Center Place, Dowling 5 South, Boston, MA 02118..
Paula Gardiner, Department of Family Medicine, Boston Medical Center, 1 Boston Medical Center Place, Dowling 5 South, Boston, MA 02118..
Katherine Gergen Barnett, Department of Family Medicine, Boston Medical Center, 1 Boston Medical Center Place, Dowling 5 South, Boston, MA 02118..
Carol Faulkner, Department of Family Medicine, Boston Medical Center, 1 Boston Medical Center Place, Dowling 5 South, Boston, MA 02118..
Janice Weinberg, Department of Biostatistics, Boston University School of Public Health, Crosstown Center, 801 Massachusetts Avenue, 3nd Floor, Boston, MA 02118..
References
- 1.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. [PMID: ] doi: 10.1016/S0140-6736(16)31678-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. 2014;95:986–995.e1. [PMID: ] doi: 10.1016/j.apmr.2013.10.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila Pa 1976). 2006;31:2724–7. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 4.Patrick N, Emanski E, Knaub MA. Acute and chronic low back pain. Med Clin North Am. 2016;100:169–81. [PMID: ] doi: 10.1016/j.mcna.2015.08.015 [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Pr; 2011. [PubMed] [Google Scholar]
- 6.Hayden JA, van Tulder MW, Malmivaara AV, Koes BW. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005;142:765–75. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 7.Freburger JK, Carey TS, Holmes GM. Physician referrals to physical therapists for the treatment of spine disorders. Spine J. 2005;5:530–41. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 8.Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514–530. [PMID: ] doi: 10.7326/M16-2367 [DOI] [PubMed] [Google Scholar]
- 9.Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. Noninvasive Treatments for Low Back Pain. Comparative effectiveness review no. 169 (Prepared by the Pacific Northwest Evidence-based Practice Center under contract no. 290–2012-00014-I.) AHRQ publication no. 16-EHC004-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2016. [PubMed] [Google Scholar]
- 10.Wieland LS, Skoetz N, Pilkington K, Vempati R, D’Adamo CR, Berman BM. Yoga treatment for chronic non-specific low back pain. Cochrane Database Syst Rev. 2017;1:CD010671 [PMID: ] doi: 10.1002/14651858.CD010671.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2005;143:849–56. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 12.Sherman KJ, Cherkin DC, Wellman RD, Cook AJ, Hawkes RJ, Delaney K, et al. A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Arch Intern Med. 2011;171:2019–26. [PMID: ] doi: 10.1001/archinternmed.2011.524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tilbrook HE, Cox H, Hewitt CE, Kang’ombe AR, Chuang LH, Jayakody S, et al. Yoga for chronic low back pain: a randomized trial. Ann Intern Med. 2011;155:569–78. [PMID: ] doi: 10.7326/0003-4819-155-9-201111010-00003 [DOI] [PubMed] [Google Scholar]
- 14.Piaggio G, Elbourne DR, Pocock SJ, Evans SJ, Altman DG; CONSORT Group. Reporting of noninferiority and equivalence randomized trials: extension of the CONSORT 2010 statement. JAMA. 2012;308:2594–604. [PMID: ] doi: 10.1001/jama.2012.87802 [DOI] [PubMed] [Google Scholar]
- 15.Schumi J, Wittes JT. Through the looking glass: understanding non-inferiority. Trials. 2011;12:106 [PMID: ] doi: 10.1186/1745-6215-12-106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saper RB, Sherman KJ, Delitto A, Herman PM, Stevans J, Paris R, et al. Yoga vs. physical therapy vs. education for chronic low back pain in predominantly minority populations: study protocol for a randomized controlled trial. Trials. 2014;15:67 [PMID: ] doi: 10.1186/1745-6215-15-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saper RB, Sherman KJ, Delitto A, Herman PM, Stevans J, Paris R, et al. Study Policies and Procedures Manual. Supplement to: Yoga vs. physical therapy vs. education for chronic low back pain in predominantly minority populations: study protocol for a randomized controlled trial. Trials. 2014;15:67 [PMID: ] doi: 10.1186/1745-6215-15-67 Acessed at https://static-content.springer.com/esm/art%3A10.1186%2F1745-6215-15-67/MediaObjects/13063_2013_1959_MOESM5_ESM.pdf on 16 February 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saper RB, Sherman KJ, Delitto A, Herman PM, Stevans J, Paris R, et al. Yoga Teacher Training Manual. Supplement to: Yoga vs. physical therapy vs. education for chronic low back pain in predominantly minority populations: study protocol for a randomized controlled trial. Trials. 2014;15:67 [PMID: ] doi: 10.1186/1745-6215-15-67 Accessed at https://static-content.springer.com/esm/art%3A10.1186%2F1745-6215-15-67/MediaObjects/13063_2013_1959_MOESM2_ESM.pdf on 16 February 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saper RB, Sherman KJ, Delitto A, Herman PM, Stevans J, Paris R, et al. Yoga Participant Manual. Supplement to: Yoga vs. physical therapy vs. education for chronic low back pain in predominantly minority populations: study protocol for a randomized controlled trial. Trials. 2014;15:67 [PMID: ] doi: 10.1186/1745-6215-15-67 Accessed athttps://static-content.springer.com/esm/art%3A10.1186%2F1745-6215-15-67/MediaObjects/13063_2013_1959_MOESM1_ESM.pdf on 16 February 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saper RB, Sherman KJ, Delitto A, Herman PM, Stevans J, Paris R, et al. Physical Therapist Training Manual. Supplement to: Yoga vs. physical therapy vs. education for chronic low back pain in predominantly minority populations: study protocol for a randomized controlled trial. Trials. 2014;15:67 [PMID: ] doi: 10.1186/1745-6215-15-67 Accessed at https://static-content.springer.com/esm/art%3A10.1186%2F1745-6215-15-67/MediaObjects/13063_2013_1959_MOESM3_ESM.pdf on 16 February 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saper RB, Sherman KJ, Cullum-Dugan D, Davis RB, Phillips RS, Culpepper L. Yoga for chronic low back pain in a predominantly minority population: a pilot randomized controlled trial. Altern Ther Health Med. 2009;15:18–27. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
- 22.Saper RB, Boah AR, Keosaian J, Cerrada C, Weinberg J, Sherman KJ. Comparing once- versus twice-weekly yoga classes for chronic low back pain in predominantly low income minorities: a randomized dosing trial. Evid Based Complement Alternat Med. 2013;2013:658030 [PMID: ] doi: 10.1155/2013/658030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fritz JM, Brennan GP, Clifford SN, Hunter SJ, Thackeray A. An examination of the reliability of a classification algorithm for subgrouping patients with low back pain. Spine (Phila Pa 1976). 2006;31:77–82. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 24.Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37:290–302. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 25.Meng XG, Yue SW. Efficacy of aerobic exercise for treatment of chronic low back pain: a meta-analysis. Am J Phys Med Rehabil. 2015;94:358–65. [PMID: ] doi: 10.1097/PHM.0000000000000188 [DOI] [PubMed] [Google Scholar]
- 26.Werneke MW, Hart DL, George SZ, Stratford PW, Matheson JW, Reyes A. Clinical outcomes for patients classified by fear-avoidance beliefs and centralization phenomenon. Arch Phys Med Rehabil. 2009;90:768–77. [PMID: ] doi: 10.1016/j.apmr.2008.11.008 [DOI] [PubMed] [Google Scholar]
- 27.Curran NJ, Timko M. Physical Therapy Online Training Modules. 2015. Accessed at https://cme.hs.pitt.edu on 16 February 2017.
- 28.Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002;82:973–83. [PMID: ] [PubMed] [Google Scholar]
- 29.Roland M, Waddell G, Klaber Moffett K, Burton K, Main C, Cantrell T. The Back Book. Norwich, UK: The Stationary Office; 1996. [Google Scholar]
- 30.Moore J, Lorig K, Von Korff M, Gonzalez V, Laurent DD. The Back Pain Helpbook. Reading, MA: Perseus; 1999. [Google Scholar]
- 31.Cherkin DC, Eisenberg D, Sherman KJ, Barlow W, Kaptchuk TJ, Street J, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Arch Intern Med. 2001;161:1081–8. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 32.Saper RB, Sherman KJ, Delitto A, Herman PM, Stevans J, Paris R, et al. Education Newsletters. Supplement to: Yoga vs. physical therapy vs. education for chronic low back pain in predominantly minority populations: study protocol for a randomized controlled trial. Trials. 2014;15:67 [PMID: ] doi: 10.1186/1745-6215-15-67 Accessed at https://static-content.springer.com/esm/art%3A10.1186%2F1745-6215-15-67/MediaObjects/13063_2013_1959_MOESM4_ESM.pdf on 16 February 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine (Phila Pa 1976). 1995;20:1899–908; discussion 1909. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 34.Von Korff M, Jensen MP, Karoly P. Assessing global pain severity by self-report in clinical and health services research. Spine (Phila Pa 1976). 2000;25:3140–51. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 35.Hudak PL, Wright JG. The characteristics of patient satisfaction measures. Spine (Phila Pa 1976). 2000;25:3167–77. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 36.Ware JE Jr. SF-36 health survey update. Spine (Phila Pa 1976). 2000;25:3130–9. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 37.Wiens BL. Choosing an equivalence limit for noninferiority or equivalence studies. Control Clin Trials. 2002;23:2–14. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 38.Bombardier C, Hayden J, Beaton DE. Minimal clinically important difference. Low back pain: outcome measures. J Rheumatol. 2001;28:431–8. [PMID: ] [PubMed] [Google Scholar]
- 39.Jordan K, Dunn KM, Lewis M, Croft P. A minimal clinically important difference was derived for the Roland-Morris Disability Questionnaire for low back pain. J Clin Epidemiol. 2006;59:45–52. [PMID: 16360560] [DOI] [PubMed] [Google Scholar]
- 40.Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976). 2008;33:90–4. [PMID: ] doi: 10.1097/BRS.0b013e31815e3a10 [DOI] [PubMed] [Google Scholar]
- 41.Heapy AA, Higgins DM, LaChappelle KM, Kirlin J, Goulet JL, Czlapinski RA, et al. Cooperative pain education and self-management (COPES): study design and protocol of a randomized non-inferiority trial of an interactive voice response-based self-management intervention for chronic low back pain. BMC Musculoskelet Disord. 2016;17:85 [PMID: ] doi: 10.1186/s12891-016-0924-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. New York: J Wiley; 2004. [Google Scholar]
- 43.Hausmann LR, Gao S, Lee ES, Kwoh CK. Racial disparities in the monitoring of patients on chronic opioid therapy. Pain. 2013;154:46–52. [PMID: ] doi: 10.1016/j.pain.2012.07.034 [DOI] [PubMed] [Google Scholar]
- 44.Chibnall JT, Tait RC, Andresen EM, Hadler NM. Race and socioeconomic differences in post-settlement outcomes for African American and Caucasian Workers’ Compensation claimants with low back injuries. Pain. 2005;114:462–72. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 45.Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl Health Stat Report. 2015:1–16. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
- 46.Saper R Integrative medicine and health disparities. Glob Adv Health Med. 2016;5:5–8. [PMID: ] doi: 10.7453/gahmj.2015.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Freburger JK, Holmes GM, Carey TS. Physician referrals to physical therapy for the treatment of musculoskeletal conditions. Arch Phys Med Rehabil. 2003;84:1839–49. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 48.American Physical Therapy Assocation. Fair Physical Therapy Copays. Accessed at www.apta.org/StateIssues/FairCopays/ on 16 February 2017.
- 49.Keosaian JE, Lemaster CM, Dresner D, Godersky ME, Paris R, Sherman KJ, et al. “We’re all in this together”: a qualitative study of predominantly low income minority participants in a yoga trial for chronic low back pain. Complement Ther Med. 2016;24:34–9. [PMID: ] doi: 10.1016/j.ctim.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beinart NA, Goodchild CE, Weinman JA, Ayis S, Godfrey EL. Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: a systematic review. Spine J. 2013;13:1940–50. [PMID: ] doi: 10.1016/j.spinee.2013.08.027 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


