Abstract
Nonshaven follicular unit extraction (NS-FUE) is the most state-of-the-art surgical technique in the field of follicular unit hair transplantation. It is particularly appealing because donor area shaving, one of the most serious impediments for the patient, can be omitted. In this article, we present our surgical approach for NS-FUE. We selectively used the direct or the pretrimming method of NS-FUE according to indication, determined by considering the location and purpose of transplantation, the condition of the recipient site, and the patient's preference. A total of 658 patients underwent NS-FUE. Of these, 17 had pubic atrichia, 2 had pubic atrichia and also received hairline correction surgery, 6 received eyebrow transplantation, 19 had female pattern hair loss, 362 had male pattern baldness (MPB), 2 had MPB and also required eyebrow transplantation, 3 received hair transplantation for MPB and scalp scar, 9 underwent male hairline correction surgery, 192 underwent female hairline surgery, and 46 received hair transplantation for scalp scar. The average numbers of transplanted grafts were 573 for atrichia, 1300 for atrichia and hairline correction performed successively, 240 for eyebrow transplantation, 996 for female pattern hair loss, 1408 for MPB (with a maximum of 3000), 1050 for MPB and eyebrow transplantation, 998 for female pattern hair loss (with a maximum of 1910), and 141 for scalp scar. On average, the total transection rate was 8.2%, and the calculated density was 2.2.
Key Words: follicular unit extraction, hair transplantation, nonshaven follicular unit extraction
The concept of donor dominance in male pattern baldness (MPB) introduced by Orentreich1 provided a firm theoretical basis upon which hair transplant surgery began. The follicular unit was first proposed by Headington2 as a histological term, describing a naturally occurring entity composed of 1 to 4 terminal hairs, an arrector pili muscle, sebaceous gland, and perifollicular tissue.
Follicular unit transplantation (FUT) is a technique first developed by Limmer3 in the 1990s. The follicular unit extraction (FUE) procedure was first reported in the literature by Rassman et al4 in 2002. The direct nonshaven FUE (NS-FUE) procedure was first introduced by Park.5 Follicular unit extraction is gaining popularity because it avoids a linear donor scar and reduces postoperative pain. However, the need for donor area shaving has been the biggest barrier for patients undergoing FUE. Nonshaven FUE provides a solution to this obstacle. Direct NS-FUE refers to a procedure of simultaneously cutting and punching hairs using a rotating punch tip, without cutting the hairs prior to surgery.5,6 On the other hand, the pretrimming method involves preoperative trimming of hairs that are about to be extracted during harvesting.7 This article presents the surgical approach and methods of NS-FUE for different indications.
MATERIALS AND METHODS
A total of 658 patients underwent hair transplantation by NS-FUE from December 1, 2015, to November 30, 2016. Minor touch-up procedures or cases where FUT was combined with NS-FUE were excluded. Patients were categorized by sex, age, type of baldness, recipient site, purpose of surgery, and history of previous hair transplantation. Medical charts and photographs were reviewed for transection rate and calculated density for each patient.
Surgical Planning
Surgical planning was meticulously undertaken through preoperative consultation with the patient. Both the occipital donor area and recipient site were thoroughly checked via examination by folliscope and visual inspection. In patients with a history of previous hair transplantation, the recipient site of prior surgery, the results of the surgery, and the donor scar position were carefully examined. Surgical design was confirmed with the patient looking into a mirror followed by marking with a surgical pen.
Preparation
In the pretrimming method, hairs were trimmed as short as 1 to 2 mm in length with the aid of highly magnifying loupes, using sharp iris scissors. The donor site was overtrimmed; that is, 10% to 20% more hairs were trimmed than were expected to be extracted. The surgical field was prepared with the patient in a sitting position, and sterile drapes were applied to both the recipient and donor sites.
Patient Position
Punching and extraction were performed with the patient in a sitting position. The forehead of the patient rested on a forehead support system, also known as graFUEt (Seson Medical Company, Seoul, Korea), which is easily moved by the surgeon using a foot pedal, to adjust the position of the patient's head (Fig. 1).
FIGURE 1.

Forehead support system for NS-FUE. A patient resting on an electrically powered forehead support. A foot pedal (not shown) is used by the surgeon to move the support in both horizontal and vertical planes.
Anesthesia
The donor area was prepared with a ring block of local anesthesia with 1:100,000 epinephrine mixed with lidocaine, along the inferior margin. A tumescent solution composed of 100 mL normal saline, 10 mL 2% lidocaine, and 0.3 mL epinephrine was injected incrementally into the punching site. Epinephrine at 1:50,000 mixed with lidocaine was used for the recipient site. Abbasi solution was used for tumescence (normal saline 100 mL + 2% lidocaine 8 mL + epinephrine 1 mL + triamcinolone 1 mL).8
NS-FUE Procedure
Punching
We used a motorized FUE machine with a 1-mm sharp punch (Folligraft; Lead M, Seoul, Korea). A 5.5× magnifying loupe was used intraoperatively.
Punching in the Pretrimming NS-FUE Procedure
In patients with long hair, 0.7- to 1.0-cm sections of the scalp were exposed using multiple hair clips (Fig. 2). In order to obtain a better visual field and minimize hindrance caused by long hairs, punch insertion was performed within the 0.7- to 1.0-cm-long zone exposed at the proximal end of hairs fixed with the lowermost clip. As the harvest of hairs progressed, the clips were released one at a time, proceeding from the bottom to the top of the donor site, to expose additional pretrimmed hairs. In patients with relatively short hair, the surgery was performed by holding fine jeweler's forceps in the left hand and the motorized punch handpiece in the right. Hair was moved aside with the forceps while punching; an assistant helped to move the hair aside using a narrow sterile stick or upward traction. Pretrimmed hairs were located for punching, working from the bottom of the donor site and proceeding upwards. Direct punching was occasionally used in between the punching of pretrimmed hairs, depending on the recipient site, purpose of surgery, and indication.
FIGURE 2.
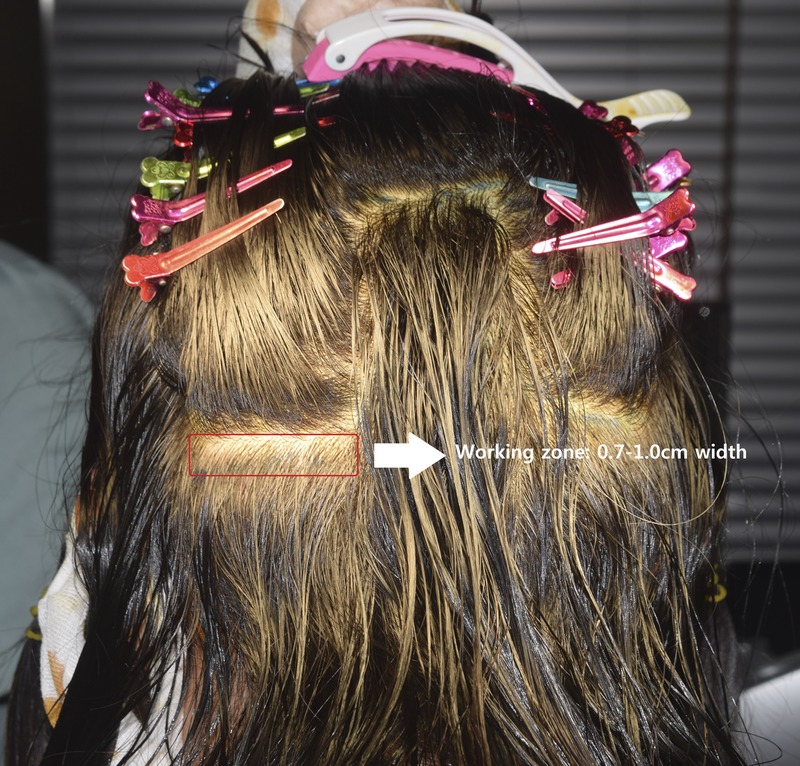
Multiple clips used to expose the scalp in a female patient with long hair. To minimize hindrance to the surgeon and the tangling of long hairs, punch insertion should be performed within the exposed 0.7- to 1.0-cm working zone.
Punching in the Direct NS-FUE Procedure
Target hairs to be harvested were selected, and the punch tip was positioned over them. Rotation of the punch was started by stepping on the foot pedal. As the punch rotated, the tip cut the hair and simultaneously entered the skin to rapidly punch out the follicular unit.
Extraction
After either punching method, aid-to-extraction forceps were used for extraction. The operator moved from left and right when punching. To reduce the duration of the procedure, assistants stood on both sides of the operator; when punching on the right side, the assistant on the right applied upward traction to the scalp and swept up the hairs, while the assistant on the left proceeded with extraction. When a portion of donor area had been scored with the punch, the operator moved to the left, the assistant on the right performed simultaneous extraction, and the assistant on the left swept up the hairs while applying upward traction.
Graft Inspection
One hundred extracted follicular units were randomly selected and examined under a microscope.
Graft Insertion
A sharp implanter (Rainbow implanter; Seson Medical Company) was used for transplantation. The patient was placed in a supine position. To minimize the grafts' out-of-body time, punching was limited within 1 hour, and grafts extracted first were implanted first. The purpose of such rules is to reduce the grafts' out-of-body time to within 2 hours. Two or 3 assistants loaded implanters, while another assistant stood immediately next to the operator to circulate the implanters.
RESULTS
Nonshaven FUE was applied to a total of 658 patients, of which 234 were female and 324 were male. Seventeen patients with atrichia underwent pubic transplantation, 2 patients underwent pubic transplantation for pubic atrichia and hairline correction surgery successively, 362 underwent hair transplantation for MPB, 2 patients with MPB also received eyebrow transplantation successively, 3 patients with MPB also underwent hair transplantation for scalp scar, 9 patients had male hairline correction surgery, 192 patients had female hairline correction surgery, and 46 patients had hair transplantation for scalp scar. Of the patients with MPB, 14 (3.8%) showed a Norwood type II pattern, 122 (33.2%) showed type III, 102 (33%) showed type IV, 100 (27.2%) showed type V, 21 (5.7%) showed type VI, and 8 (2.2%) showed type VII pattern hair loss.
The average age of the patients was 36.5 years, with the youngest being 20 and the oldest 73 years old. There was a great difference in age by type of surgery. The average age of patients with pubic atrichia was 45.9 years (range, 28–62 years). Patients with female pattern hair loss, comprising the oldest age group, averaged 48.9 years of age (range, 25–68 years). Average age was 37.3 years (range, 24–73 years) for patients with MPB, 30.8 years (range, 25–37 years) for male hairline correction, 33.7 years (range, 20–66 years) for female hairline correction surgery, and 40.0 years (range, 20–60 years) for scalp scar.
The pretrimming technique was adopted for pubic hair transplantation, female hairline correction surgery, and eyebrow transplantation. The direct method was applied for hair transplantation for MPB alone and for a portion of the male hairline correction cases. For cases of hair transplantation for MPB and eyebrow transplantation and for a portion of patients undergoing male hairline correction surgery, the direct method was used in conjunction with pretrimming.
Using NS-FUE, 1 cycle of the whole procedure took approximately 3 hours: 1.5 hours for punching and extraction and another 1.5 hours for implantation, taking into account some spare time for changing the patient's position and other minor delays. In total, transplantation of 1600 to 1800 grafts took approximately 6 hours, and 2400 to 2700 grafts took 9 hours. The maximum number of grafts transplanted in a day was approximately 3000. On average, the total transection rate was 8.2%, and the calculated density was 2.2.
The average numbers of grafts required were 573 for atrichia, 1300 for the 2 patients with atrichia also receiving hairline correction surgery, 240 for the 6 patients undergoing eyebrow transplantation, 996 for the 19 patients with female pattern hair loss, 1408 with a maximum of 3000 for the 362 patients with MPB, 1002 for the 2 patients with MPB also receiving eyebrow transplantation, 1050 for the 9 patients undergoing male hairline surgery, 998 with a maximum of 1910 for the 192 patients receiving female hairline correction surgery, and 131 for the 141 patients undergoing transplantation for scalp scar.
DISCUSSION
Donor area shaving poses a serious impediment for patients undergoing hair transplantation by the FUE method. Several solutions can be provided to alleviate the impact of shaving (Fig. 3).
FIGURE 3.
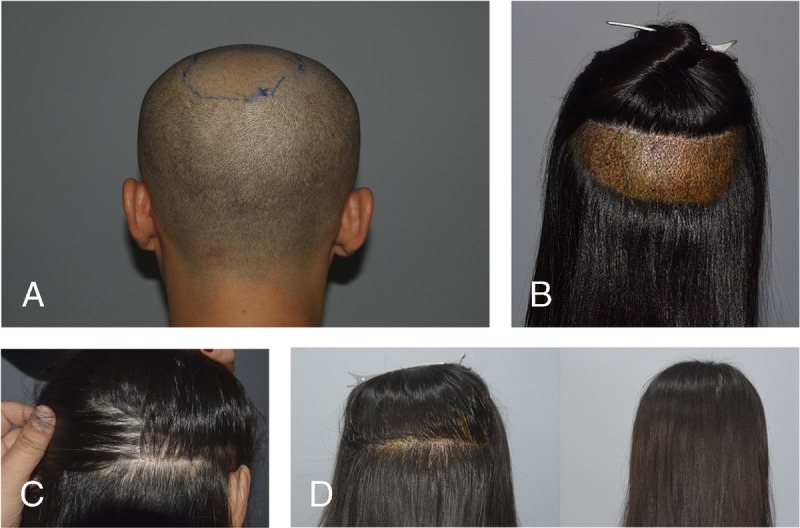
Various shaving patterns. A, Total shaving, postoperative day 1. B, Partial shaving, postoperative day 1. C, Harvesting a large number of grafts in a microstrip shaving pattern can result in multiple linear scars. D, Nonshaven FUE, postoperative day 1.
First, the strip method can be recommended to patients, excluding those with insufficient scalp laxity or an aversion to this method. Second, partial shaving can be a solution when the patient's own hair is long enough to hide the shaved areas.5 However, it is not applicable when the patient's hair is cut too short, a large number of grafts are required, or occupational or personal reasons do not allow any type of shaving. Moreover, harvesting takes place only in the shaved area; thus, the area with decreased hair density is clustered in a specific portion of the donor area.
We generally use the palm of the hand to help patients estimate the size of the area to be shaved (Fig. 4).
FIGURE 4.
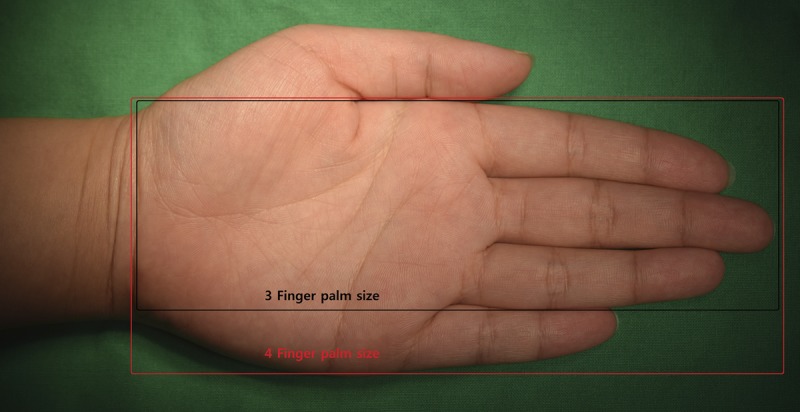
Patient's palm is used for understanding of the extent of shaving.
This lets the patient easily visualize the area about to be shaved on the back of the head. In female patients, the width of 3 fingers is approximately 5 cm, and that of 4 fingers is approximately 6.5 cm. The distance from the fingertip to the wrist is approximately 15 cm. With the use of a 1-mm-diameter punch, approximately 13 to 15 follicular units can be harvested in a 1-cm2 area, avoiding any clustering of white spots. Therefore:
a 3-finger palm size = 5 × 15 cm = 75 cm2, and 75 cm2 × 13 (or 15) = 975 (or 1125) follicular units;
a 4-finger palm size = 6.5 × 15 cm = 97.5 cm2, and 97.5 cm2 × 13 (or 15) = 1267.5 (or 1462.5) follicular units.
For female patients with good hair density, approximately 900 grafts can be obtained from an area covered by 3 fingers and 1200 grafts from a palm size area of approximately 4 finger-widths. In a patient with lower hair density in the donor area, approximately 700 grafts can be obtained from an area of approximately 3 finger-widths and approximately 900 to 1000 grafts from an area of approximately 4 finger-widths. More grafts can be obtained with a smaller punch.9
Male patients, of course, have hands of larger size and have greater follicle density, allowing a higher number of grafts to be obtained from a 1-cm2 area. An estimation of the number of grafts obtainable from male patients is as follows:
a 3-finger palm size = 6.5 × 15 cm = 97.5 cm2, and 97.5 cm2 × 13 (or 15) = 1267.5 (or 1462.5) follicular units;
a 4-finger palm size = 8 × 15 cm = 120 cm2, and 120 cm2 × 13 (or 15) = 1560 (or 1800) follicular units.
The above rule is very useful during preoperative consultation with the patient. He/she can have an understandable estimate of the size of the area that needs shaving. The surgical method can be chosen with more ease as well.
A third solution is microstrip shaving. However, this method is not recommended in a case requiring more than 400 to 600 grafts because multiple linear scars can be created as a result.
A fourth solution is NS-FUE. Nonshaven FUE necessitates longer operation hours and requires more time to acquire the necessary skills. An extremely long operation time can be physically and mentally exhausting for the patient as well as the surgeon.10 The longer the follicle out-of-body time is, the lower the rate of engraftment. However, the entire donor area can be evenly punched without the need for any shaving. If the surgeon is capable of successfully performing this procedure, it can be the best possible technique to adopt. Therefore, a proper understanding of the patient's position, ergonomics, equipment, and surgical skills required for NS-FUE is crucial.
Patient Position
A sitting position is preferred to a prone position for FUE harvesting. However, this varies, depending on the operator's experience and preference. Obtaining a clear visual field is a crucial matter in NS-FUE, and the visual field can be poor if not properly managed. As the blood clots, hairs can stick together, making it more difficult to sweep them up, out of the visual field. Because blood flows downward, working from the bottom of the surgical area upward helps to gain a better visual field when the patient is in a sitting position.
Ergonomics
Adequate ergonomics is important not only to the patient but also to the operator, as NS-FUE demands extremely long operative hours. Maintaining the prone position for a prolonged period is much more challenging to the patient compared with the sitting position. However, it is more comfortable for the surgeon than having the patient sitting upright. The GraFUEt system, an FUE apparatus that is currently used by the authors, provides an arm border that supports the elbow and is vertically adjustable via a foot pedal to diminish the surgeon's muscle fatigue. Occasional leaning of the elbow on the rest very effectively reduces muscle fatigue (Fig. 5).
FIGURE 5.

Motorized elbow rest. An elbow rest allows the operator to occasionally rest the arm during surgery.
Tumescent Injection
Tumescent infiltration into the donor area lessens intraoperative bleeding, creates tense turgor of the scalp, and changes the hair angle to be more obtuse. Na et al11 previously reported that the vasoconstrictive effect rises in parallel with the proportion of epinephrine in local injection or tumescent solution. Also, the tense turgor of the scalp tissue brought by tumescent injection lasts only 5 to 10 minutes. Therefore, we prefer to use the solution frequently and incrementally, according to the pace of progress in punching.
Upward Traction
As Zontos and colleagues12 have described, the average FUE punching angle is approximately 45 degrees, and the more acute this angle is, the larger the resulting wound surface. Moreover, the angle of a hair follicle is more acute above the scalp tissue than below. Thus, changing the angle of hair follicles to be more obtuse generally provides a great significant during surgery. There are 2 principal ways of achieving a more obtuse punching angle. One is tumescent injection, and the other is upward traction. Upward traction first changes the hair angle to be more upright. Second, this maneuver helps to keep the scalp tissue tense and prevents graft torsion by inhibiting the punch tip from being pushed away from the follicle axis by its initial rotating movement. Third, manual upward traction literally sweeps up the hairs that may block the surgical field, at the same time preventing hairs from tangling around the rotating punch tip.
Extraction
Extraction is the most important and time-consuming process in NS-FUE. Existing hairs should be set aside to accurately locate punched grafts, requiring utmost focus, skill, and know-how. With the patient in a sitting position, aid-to-extraction forceps are more useful than jeweler's forceps. As for the punching process, extraction begins at the bottom and moves upward. The operator needs to change places with the assistant for simultaneous punching and extraction, to minimize operation time. When the operator is finished with punch insertion, 2 assistants extract hair follicles from both sides (Fig. 6).
FIGURE 6.
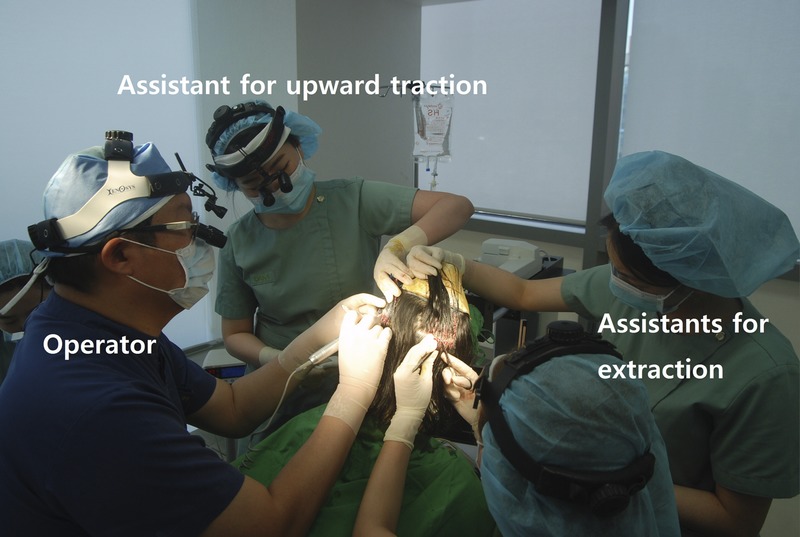
Operator-assistant cooperation system during NS-FUE.
Graft Loading Into the Implanter Tip
We use sharp implanters for graft insertion. There are 2 methods of graft loading. One involves hair follicles protruding through the slitting gap, and the other involves completely placing grafts into the lumen of the implanter tip (Fig. 7).
FIGURE 7.
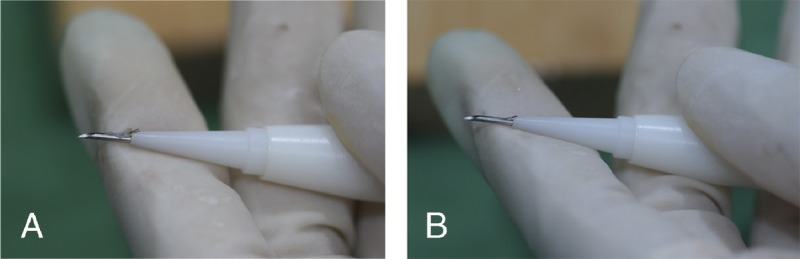
Two methods of loading grafts into the implanter. A, A graft protruding through the slitting gap after loading. B, A graft placed entirely in the tip lumen when loaded.
When using a 1-mm punch at the average punching angle of 45 degrees, the diameter of the graft would be greater than 1 mm at the level of the epidermis, but approximately 1 mm at a lower level. The slitting gap varies by manufacturing company but is usually 0.2 to 0.35 mm in width. It is, of course, narrower in implanters of smaller size (0.9, 0.8, 0.7, or 0.6 mm). The most commonly used implanter used for 2- or 3-hair grafts is 1-mm outer diameter and 0.8-mm inner diameter. Thus, without graft trimming, loading grafts such that they are protruding causes injury by strangling the grafts in the process of insertion. In particular, damage to the bulge area, which is located 2 to 3 mm below the skin surface, would adversely affect engraftment. Lorenzo and Vila13 introduced the method of loading grafts into implanter tip with partially protruding through slitting gap. They used a punch that had diameter of 0.75 to 0.80 mm. In whites, with thinner and shorter hair follicles and softer scalp skin, the use of such a smaller-sized punch is more efficient. To transplant larger follicles, we prepared grafts by trimming only the side of the epidermis that protrudes more, to minimize manipulation at the same time as facilitating the process of loading. Assistants were thoroughly educated and trained to precisely dissect only the epidermis with one clean cut, avoiding any injury to bulge area (Fig. 8).
FIGURE 8.
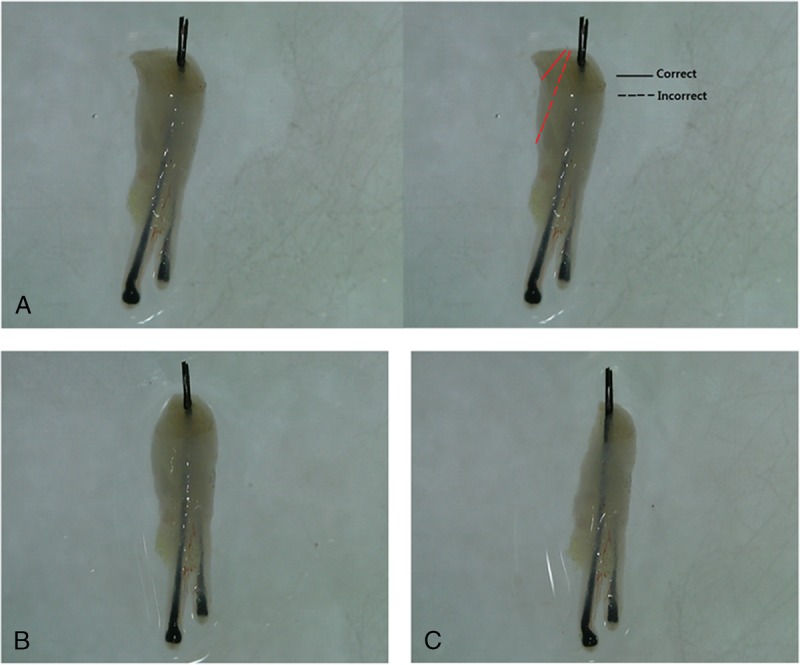
Unilateral trimming of the epidermis. A, An extracted FUE graft, showing prospective trimming planes. B, A graft after unilateral trimming of the epidermis with one clean cut. C, A graft trimmed with the blade directed downward too much, which can cause damage to the bulge area.
Graft Placement With a Sharp Implanter
Grafts are implanted by a 4- or 5-person team composed of 2 to 3 loaders, 1 passer, and the operator (Fig. 9).
FIGURE 9.

The 2(3)-1-1 system. The passer withdraws the used implanter from the operator's hand, immediately replacing it with another loaded implanter in a very precise manner, allowing the operator to work with quick, small vertical movements within a range of 5 cm. Graft insertion thereby takes place swiftly and accurately, without soft tissue damage.
In comparison with FUT grafts, FUE grafts are more slender toward the bottom (Fig. 10). Follicular unit extraction grafts are therefore more prone to physical trauma, such as desiccation. Thus, we prefer an implanter technique that enables the most atraumatic and swift graft insertion. This technique embodies much higher responsibility for the surgeon, as he/she directly implants all grafts himself/herself. It allows real-time monitoring of the surgery result. On the other hand, the high cost of sharp implanters and the intensive labor for the physician can be considered downsides of this technique.
FIGURE 10.
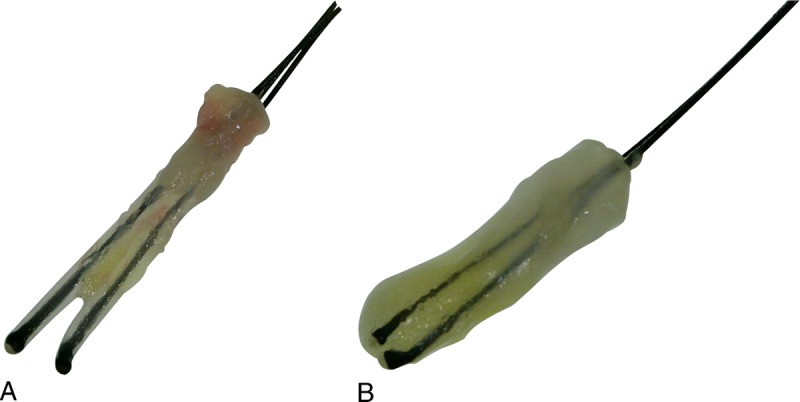
Follicular unit extraction grafts differ from FUT grafts in shape. A, An FUE graft. B, Two FUT grafts.
We can perform 700 to 900 punches per hour using the above techniques. Nonshaven FUE can be used for transplanting 2500 grafts in a day on average, with a maximum of 3000 grafts a day. When we began using this method, it took 1 hour to complete punch insertion for 200 to 300 grafts, which was followed by an additional hour to extract the punched grafts. Nonshaven FUE is time consuming, demands high concentration, and is physically exhausting. It also requires substantial time to acquire the necessary skills. Performing surgery on a female patient with long hair is even more difficult. Therefore, less experienced practitioners should attempt only a small number of grafts at once. To reach a high standard (Figs. 11, 12), not only the operator but also the staff should be involved with ongoing education and quality control.
FIGURE 11.
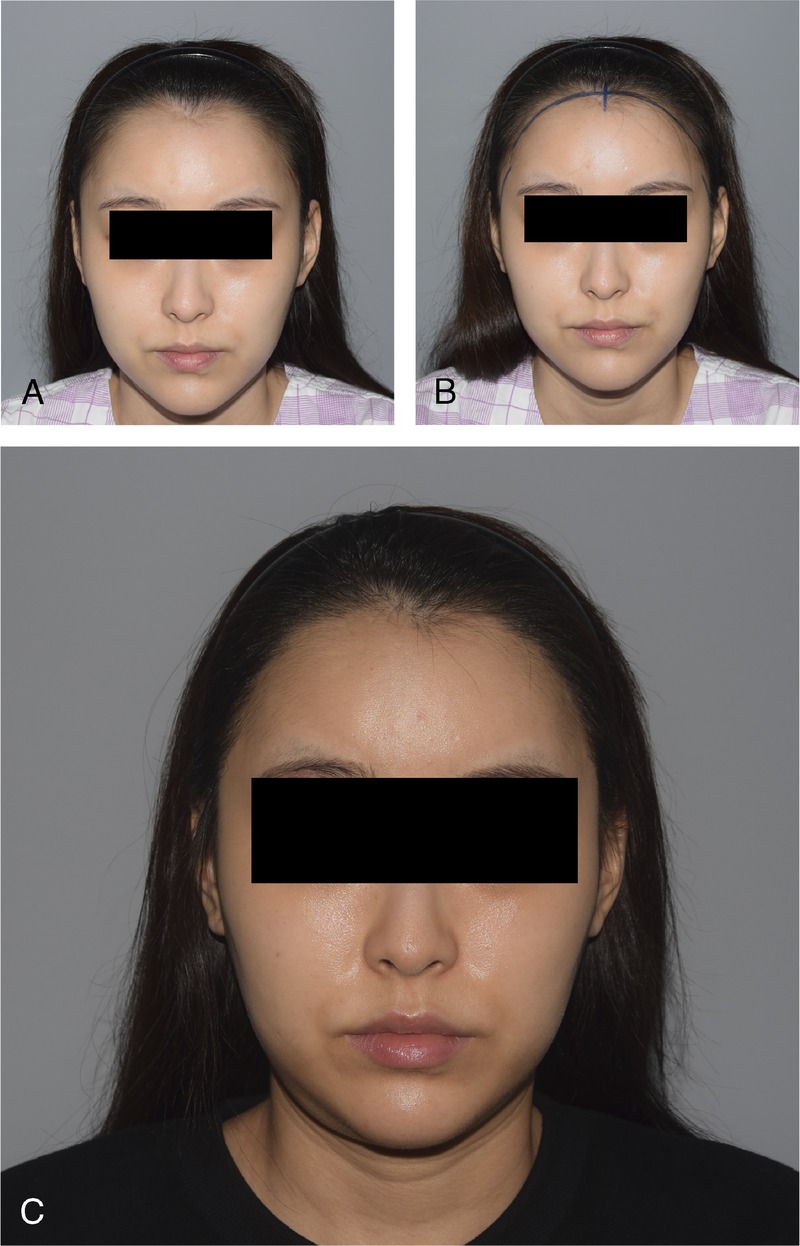
Female hairline correction with NS-FUE, 1400 grafts. A, Preoperative photographs. B, Surgical design. C, One year postoperation.
FIGURE 12.
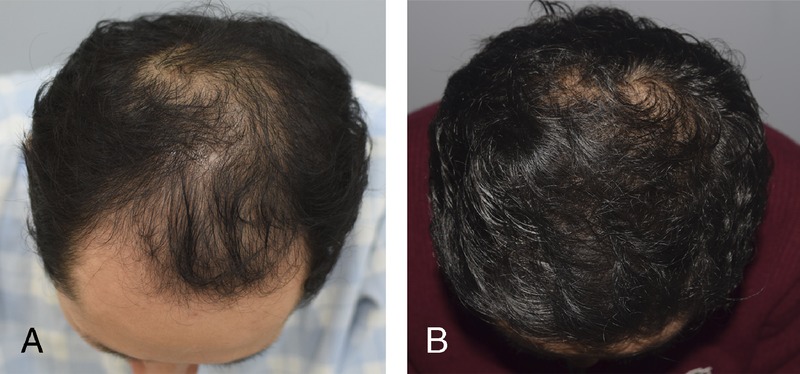
Male pattern baldness patient, 2000 grafts with direct NS-FUE technique. A, Preoperative photograph. B. Hair growth after 1 year.
The major objective of hair transplantation is to deliver the required number of grafts in adequate density and with natural appearance. It is also important to provide both the patient and the physician with maximal comfort and convenience, at the same time minimizing any negative personal and social effects for the patient. In conclusion, we consider that the surgical techniques described in this article fulfill these objectives.
Footnotes
Conflicts of interest and sources of funding: J.H.P. has patent pending, ownership interest of Seson medical company. The other authors have none declared.
REFERENCES
- 1.Orentreich N. Autografts in alopecias and other selected dermatological conditions. Ann N Y Acad Sci. 1959;83:463–479. [DOI] [PubMed] [Google Scholar]
- 2.Headington JT. Transverse microscopic anatomy of the human scalp: a basis for a morphometric approach to disorders of the hair follicle. Arch Dermatol. 1984;120:449–456. [PubMed] [Google Scholar]
- 3.Limmer BL. Elliptical donor stereoscopically assisted micrografting as an approach to further refinement in hair transplantation. J Dermatol Surg Oncol. 1994;20:789–793. [DOI] [PubMed] [Google Scholar]
- 4.Rassman WR, Bernstein RM, McClellan R, et al. Follicular unit extraction: minimally invasive surgery for hair transplantation. Dermatol Surg. 2002;28:720–728. [DOI] [PubMed] [Google Scholar]
- 5.Park JH. Direct non-shaven FUE technique. Hair Transplant Forum Int. 2014;24:103–104. [Google Scholar]
- 6.Park JH. Re: state-of-the-art FUE: non-shaven technique. Hair Transplant Forum Int. 2015;25:82–83. [Google Scholar]
- 7.Cole JP. State of the art FUE: advanced non-shaven technique. Hair Transplant Forum Int. 2015;25:82–83. [Google Scholar]
- 8.Gholamali A, Sepideh P, Susan E. Hair transplantation: preventing post-operative oedema. J Cutan Aesthet Surg. 2010;3:87–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park JH. FUE round table questions and answers. Hair Transplant Forum Int. 2016;26:139–140. [Google Scholar]
- 10.Williams KL., Jr Ergonomics in hair restoration surgeons. J Cosmet Dermatol. 2016;15:66–71. [DOI] [PubMed] [Google Scholar]
- 11.Na YC, Park R, Jeong HS, et al. Epinephrine vasoconstriction effect time in the scalp differs according to injection site and concentration. Dermatol Surg. 2016;42:1054–1060. [DOI] [PubMed] [Google Scholar]
- 12.Zontos G, Williams KL, Jr, Nikiforidis G. Minimizing injury to the donor area in follicular unit extraction (FUE) harvesting. J Cosmet Dermatol. 2017;16:61–69. [DOI] [PubMed] [Google Scholar]
- 13.Lorenzo J, Vila X. Introduction to the use of implanters. Hair Transplant Forum Int. 2011;21:121–122. [Google Scholar]


