Abstract
All cases of prostate cancer exhibit the hallmark condition of marked decrease in zinc in malignancy compared to the high zinc levels in the normal and benign prostate. There exists no reported corroborated case of prostate cancer in which malignancy exhibits the high zinc levels that exist in the normal prostate acinar epithelium. The decrease in zinc is achieved by the downregulation of ZIP1 zinc transporter, which prevents the uptake and accumulation of cytotoxic zinc levels. Thus, prostate cancer is a “ZIP1-deficient” malignancy. Testosterone and prolactin are the major hormones that similarly regulate the growth, proliferation, metabolism, and functional activities of the acinar epithelial cells in the peripheral zone (the site of development and progression of malignancy). Testosterone regulation provides the basis for androgen ablation treatment of advanced prostate cancer, which leads to the development of terminal androgen-independent malignancy. Androgen-independent malignancy progresses under the influence of prolactin. These relationships provide the basis for the prevention and treatment of advanced prostate cancer. Clioquinol (zinc ionophore; 5-chloro-7-iodoquinolin-8-ol) is employed to facilitate zinc transport and accumulation in the ZIP1-deficient malignant cells and induce cytotoxic effects. Cabergoline (dopamine agonist) is employed to decrease prolactin production and its role in the progression of androgen-independent malignancy. We propose a clioquinol/cabergoline treatment regimen that will be efficacious for aborting terminal advanced prostate cancer. FDA policies permit this treatment regimen to be employed for these patients.
Keywords: Androgen-independent prostate cancer, cabergoline bromocriptine agonist, clioquinol zinc ionophore, testosterone and prolactin
INTRODUCTION
About 165,000 cases of prostate cancer and 30,000 deaths will occur in 2018 in the USA. For advanced prostate cancer, the 5-year survival rate is 30%.[1] The latter includes terminal androgen-independent malignancy (castration-resistant prostate cancer) that results from androgen ablation. Androgen independent cancer remains untreatable despite decades of research to develop a treatment to abort this malignancy. In this review, we will present the background for the development and progression of prostate malignancy, the role of testosterone and prolactin, and the basis for a proposed efficacious treatment that will abort the development and progression of terminal androgen-independent prostate cancer.
THE ORGANIZATION OF THE PROSTATE GLAND AND THE INITIATION AND DEVELOPMENT OF PROSTATE MALIGNANCY
The human prostate gland is a complex organ comprised different ontological and analogical regions. The structure of the normal prostate gland includes the peripheral zone (~75%), the central zone (~20%), and the transition zone/periurethral region (~5%). The peripheral zone is the major region where ~90% of malignancy is initiated and progresses. About 10% of malignancy develops in the transition zone but is a more indolent malignancy. The transition zone is the region where benign prostatic hyperplasia develops and then invades the central zone.[2]
These relationships must be recognized in describing functional relationships of the normal prostate gland and the implications in prostate pathology. Unfortunately, many (and likely most) reported physiological and pathophysiological reports do not recognize or identify these relationships and lead to inappropriate and misrepresented conclusions.
THE STATUS AND ROLE OF ZINC AND ZIP1 ZINC TRANSPORTER IN PROSTATE CANCER
In seventeen reported population studies,[3] collectively totally several hundred normal prostate versus prostate cancer cases, the zinc levels were decreased in all cases and stages of prostate cancer by 68% ± 3% standard error (P < 0.0001) as compared to normal and benign prostate. Figure 1 shows the high zinc level in the normal acinar epithelial cells, and the loss of zinc in the malignant cells. No corroborated case of prostate cancer exists in which the malignancy exhibits the higher zinc that exists in the normal acinar cells. “Why?”
Figure 1:
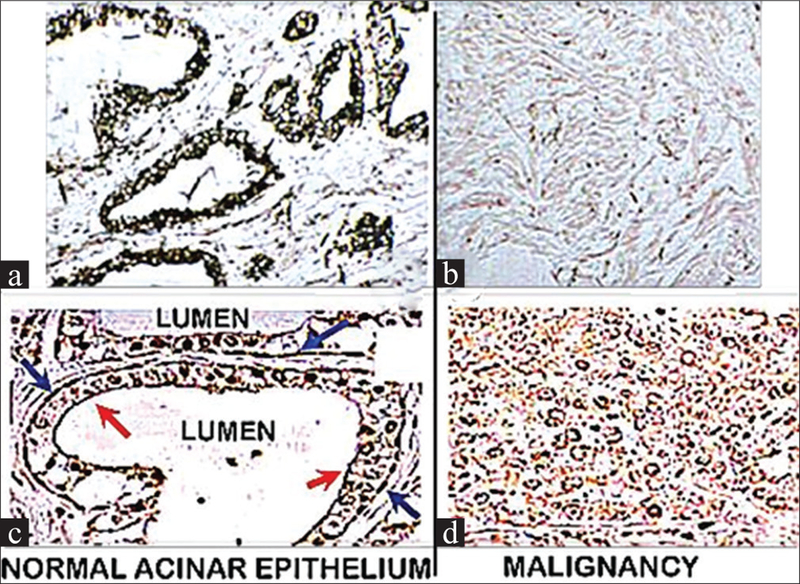
Zinc and ZIP1 transporter in normal acinar cells and malignant cells. (a) Black dithizone stain shows high zinc level in normal acinar epithelium and decreased zinc in malignant cells, (b) arrows show localized ZIP1 at the plasma membrane of the normal acinar cells and the absence of ZIP1 in the malignant cells
The high zinc level that exists in the normal peripheral zone acinar epithelial cells (the origin and development of malignancy) is cytotoxic in the malignant cells. Therefore, the malignant cell evolved with mechanisms that prevent the accumulation of the higher zinc levels that exist in the normal cells. A major factor is the downregulation of ZIP1 (Slc39A1) transporter that is responsible for the uptake and accumulation of zinc in the normal cells [Figure 1]. The ZIP1 downregulation and decreased zinc occurs in the development of malignancy and persists throughout the progression of the malignancy, leading to advanced prostate cancer.[4,5] Thus, prostate cancer is a “ZIP1-deficient” malignancy.
THE STATUS OF CITRATE IN NORMAL AND MALIGNANT PROSTATE PERIPHERAL ZONE
In addition to being zinc-accumulating cells, the acinar cells of the peripheral zone are also citrate-producing cells, due to zinc inhibition of m-aconitase activity and citrate oxidation through the Krebs cycle. In malignancy, the decreased zinc inhibition of citrate production is removed, and the malignant cells exhibit major decreased citrate.
This is the basis for in situ magnetic resonance spectroscopy imaging (MRSI) for the identification of normal and malignant loci in the peripheral zone [Figure 2].[6]
Figure 2:
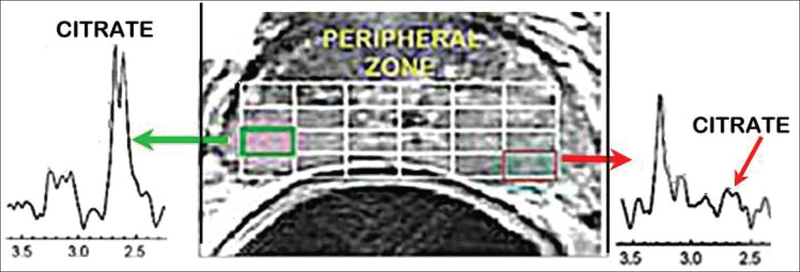
In situ magnetic resonance spectroscopy image shows high citrate in normal peripheral zone and marked decreased citrate in malignant loci
THE “GENETIC/METABOLIC TRANSFORMATION” IN THE DEVELOPMENT OF PROSTATE MALIGNANCY
It becomes apparent that the metabolism of the normal acinar epithelial cells undergoes “genetic/metabolic transformation” during the development of malignancy. The zinc-related metabolic pathway of citrate metabolism is represented in Figures 3 and 4[5] and reveals that the ZIP1 downregulation/decreased zinc is a genetic/metabolic transformation that occurs in premalignancy and progresses in the development of malignancy. Thus, we characterize prostate cancer as a ZIP1-deficient malignancy. This is an important relationship that should be represented in prostate biomedical research and clinical studies.
Figure 3:
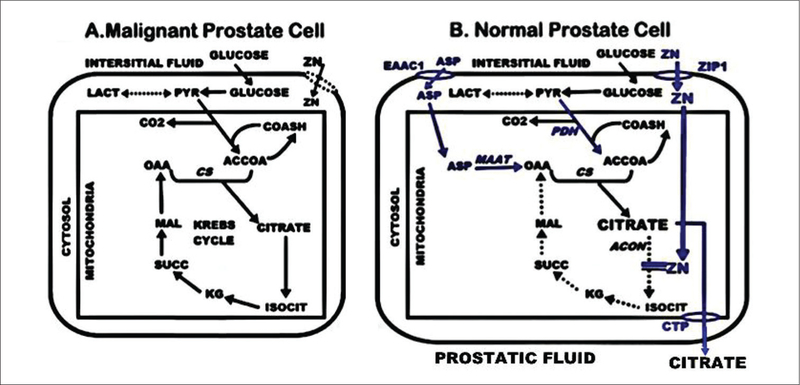
The citrate-related metabolic pathways in malignant and normal prostate epithelial cells
Figure 4:
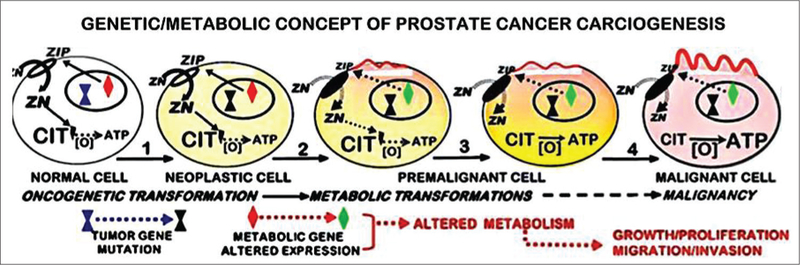
The genetic/metabolic transformation during the development of prostate malignancy
THE STATUS OF ZINC IN EXTRACELLULAR AND INTRACELLULAR FLUIDS
It must be recognized that zinc exists in extracellular and intracellular fluids as either mildly bound to ligands or as tightly bound to ligands, i.e., “Zn ligands.”[7] The former includes exchangeable (“mobile”) reactive Zn ligands such as Zn amino acids and Zn metallothioneins, and the latter includes most Zn proteins/Zn enzymes. The concentration of free Zn++ ion is in the fM-nM range, which is physiologically irrelevant. The mobile reactive Zn ligands have zinc-binding formation constants of logKf=~11 or lower. Zn ligands with logKf~12 and greater are tightly bound, non-exchangeable zinc compounds. In addition, Figure 5 shows that the effects of zinc are dependent on the total zinc concentration of the mobile Zn ligands and not on the free Zn++ ion concentration.
Figure 5:
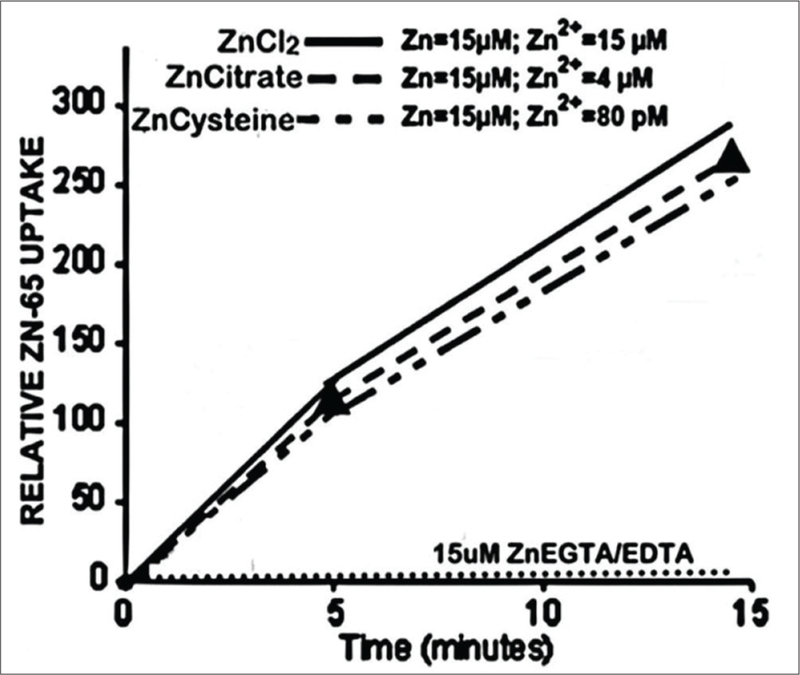
The effect of zinc concentrations of mobile Zn ligands on the cellular uptake of zinc in prostate PC-3 cells
EXPERIMENTAL EVIDENCE FOR ZINC IONOPHORE (CLIOQUINOL) EFFICACIOUS TREATMENT OF ADVANCED PROSTATE CANCER
The relationship of high zinc levels being cytotoxic in prostate malignancy provides a basis for zinc treatment regimen for prostate cancer. The ZIP1-deficient status of prostate malignancy dictates that a process and/or agent is required to deliver zinc from plasma into the ZIP1-deficient malignant cells and manifest the cytotoxic effects of zinc.
One such agent is an ionophore, which will bind zinc to provide a Zn ionophore ligand to facilitate the transport of zinc across the plasma membrane and into the cell. The ionophore must be capable of binding zinc in plasma, thus forming a Zn ionophore ligand. The binding affinity must result in a mobile. Zn ionophore ligand, which is delivered to the malignant site, and facilitates the transport of zinc into the cell. Within the cell, the mobile Zn ionophore will provide the exchangeable Zn that will then exhibit the cytotoxic effects of the increased concentration of zinc. Consequently, this is a complex process that is required for a zinc ionophore to be an efficacious regimen for the treatment of prostate malignancy.
The above zinc ionophore requirements are exhibited by clioquinol, which has a logKf~7–8.[8,9] We achieved successful results with clioquinol treatment of xenograft mice implanted with human ZIP1-deficient PC3 cells that we developed.[10] Subcutaneous administration of clioquinol resulted in ~85% suppression of the ZIP1-deficient tumor growth [Figure 6].
Figure 6:
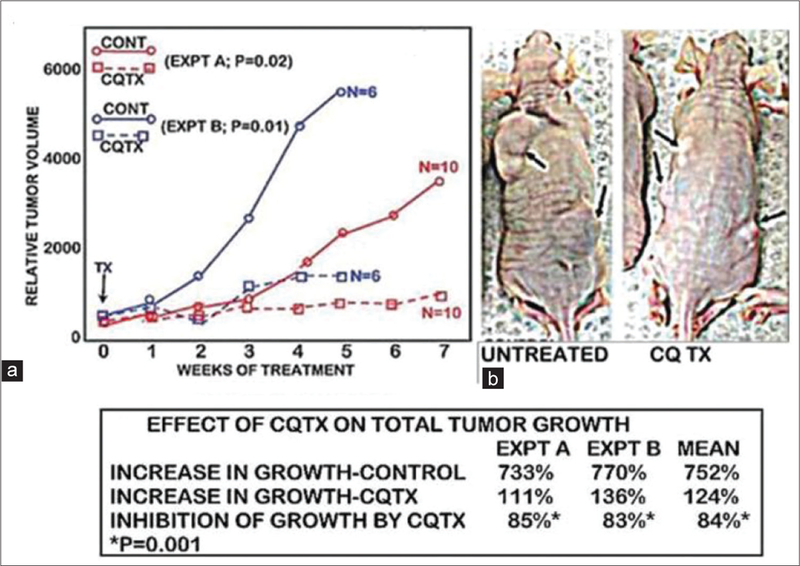
The effects of the clioquinol treatment of mice with xenograft human ZIP1-deficient tumors. (a) Results of two experiments showing the tumor suppression effects of clioquinol treatment, (b) shows the marked decrease in tumor size in treated mice
TESTOSTERONE AND PROLACTIN DUAL ROLE IN THE DEVELOPMENT AND PROGRESSION OF ADVANCED PROSTATE CANCER
It is well established and recognized that testosterone is a major hormone for the regulation of growth, proliferation, metabolism, and functional activities of peripheral zone acinar epithelial cells.[11] Testosterone regulation is through androgen receptor pathway [Figure 7].
Figure 7:
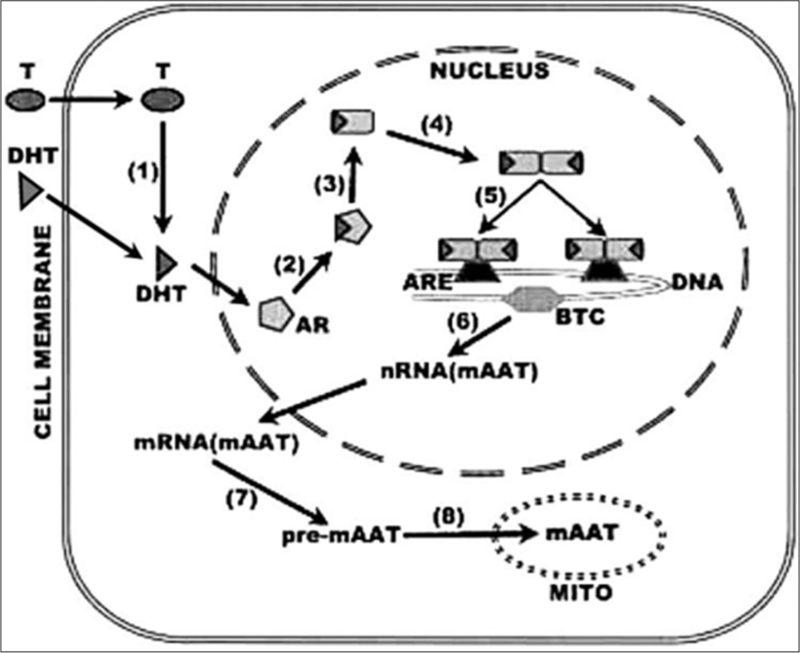
The pathway of testosterone regulation of metabolic genes as represented by mAAT. Testosterone (T); dihydrotestosterone (DHT); androgen receptor (AR); (3) androgen response elements (ARE 1 and 2); basal transcription complex (BTC); mito aspartate aminotransferase (mAAT)
In contrast, the important role of prolactin in males has been largely ignored and/or misrepresented by contemporary investigators and clinicians. Most reported studies (such as[12]) relate to the well-known growth promoting and differentiation effects (cytokine effects) of prolactin, which are mediated predominantly through the tyrosine kinase-associated pathway.
In contrast, prolactin regulation of the metabolic genes in prostate cells is mediated through the direct hormone receptor activation of the phospholipase-diacylglycerol pathway, leading to the direct activation of PKC [Figure 8].[13] This metabolic relationship is the major function of prolactin in the human and animal prostate glands.
Figure 8:
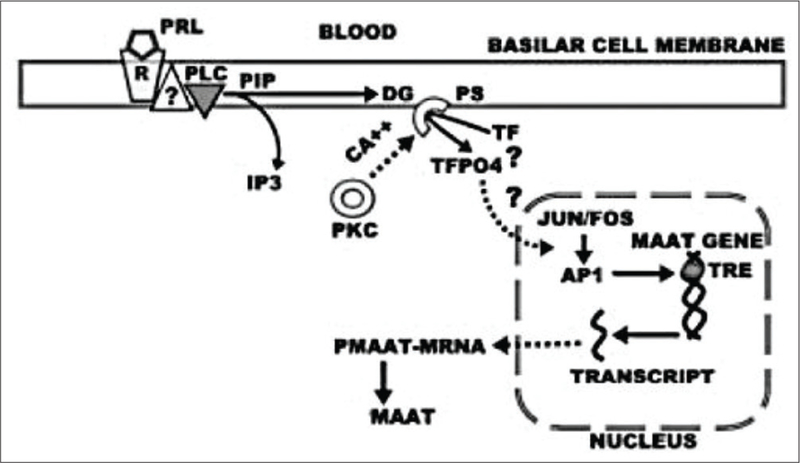
Protein kinase C pathway for prolactin regulation of metabolic gene expression in prostate epithelial cells as represented by mitochondrial aspartate aminotransferase. Prolactin receptor complex (PRL-R); phospholipase C (PLC); diacylglycerol (DG); inositol triphosphate (IP3); protein kinase C (PKC); transcription factor (TF); TPA response element (TRE)
It is important to note that prolactin regulation occurs specifically in the acinar epithelial cells of the posterior peripheral zone, whereas testosterone regulates these and other cells in the prostate gland. Nevertheless, both hormones are involved in the development and progression of advanced prostate cancer. This relationship must be considered in relation to the development and progression of advanced prostate cancer and in the application of treatment regimens for prostate cancer.
A PROPOSED REGIMEN THAT INCLUDES CLIOQUINOL TREATMENT AND CABERGOLINE TREATMENT (PROLACTIN DOPAMINE AGONIST) FOR TERMINAL ANDROGEN-INDEPENDENT PROSTATE CANCER
We propose to employ the topical cutaneous application of 3% clioquinol cream to deliver zinc from plasma to the malignant site and into the ZIP1-deficient cells to manifest its cytotoxic effects. The topical cutaneous application of 3% clioquinol cream (also with 1% hydrocortisone) is employed for the treatment of bacterial and fungal skin infections and exhibits little or no adverse local or systemic effects so that the benefit/risk consideration favors its treatment for terminal prostate cancer.
The effective transdermal absorption of clioquinol into plasma and delivery to other tissue sites is evident from its increase in protein-bound iodine and the recovery of clioquinol glucuronide in urine.[14,15] Thus, it is plausible to expect that sufficient Zn clioquinol in circulation will be delivered to primary site prostate malignancy and to metastatic sites, thereby resulting in zinc transport into the ZIP1-deficient malignant cells and manifesting zinc cytotoxicity and abortion of malignancy. This is well supported by the tumor suppression effects of subcutaneous clioquinol treatment in mice [Figure 3].
Its typical treatment protocol for skin disorders is to apply a thin layer of the medication to the affected area and gently rub in, up to 3–4 times daily. For advanced prostate cancer, the cream could be initially applied to ~2 inch area of skin, perhaps once a day. If no adverse side effects become apparent, the treatment might be increased.
The presence of prolactin receptors and prolactin dependency in prostate cancer[16–20] dictates that treatment to decrease its production and plasma level is advisable. To achieve this, we propose that cabergoline (dopamine agonist; Dostinex) to decrease the plasma level of prolactin be employed in combination with clioquinol. It has been shown to be more effective than bromocriptine for decreasing the production and plasma level of prolactin and with less adverse side effects.[21–23] The treatment should be in accord with the recommended dosage for Dostinex (https://www.centerwatch.com/drug-information/fda-approved-drugs/drug/209/dostinex-tablets-cabergoline-tablets.).
The possible adverse effects and the efficacy of the combined testosterone and prolactin ablation treatment should be monitored by the levels of PSA, plasma testosterone, and prolactin and imaging of malignancy (e.g., PSMA PET and MRSI).
THE FDA “COMPASSIONATE USE” (EXPANDED ACCESS) POLICY: APPLIED FOR THE CLIOQUINOL TREATMENT OF TERMINAL CANCERS
FDA “Expanded access” policy for the use of investigational drugs outside the clinical trial setting for treatment purposes described as: “Patient has a serious disease or condition, or whose life is immediately threatened by their disease or condition; there is no comparable or satisfactory alternative therapy to diagnose, monitor, or treat the disease or condition; patient enrollment in a clinical trial is not possible; potential patient benefit justifies the potential risks of treatment; providing the investigational medical product will not interfere with investigational trials that could support a medical product’s development or marketing approval for the treatment indication.” (https://www.fda.gov/NewsEvents/PublicHealthFocus/ExpandedAccessCompassionateUse/default.htm). In addition, the “right to try” legislation provides terminally ill patients an option to try an experimental drug that has met FDA requirement of being a safe drug for human use but need not been shown to be therapeutically effective. This permits the terminally ill patients, who have exhausted all FDA-approved treatments, to proceed with an experimental treatment that could eliminate or improve their terminal condition. Also, the FDA “off-label use” and “right to try” policies should be employed for the combined 3% clioquinol cream and cabergoline treatment regimen for the treatment of terminal prostate cancer patients with androgen-independent prostate cancer.
CONCLUSIONS
Terminal androgen-independent prostate is prolactin dependent, decreased zinc, ZIP1- deficient malignancy in which conditions that will increase zinc uptake and accumulation will exhibit cytotoxic/tumor suppressor effects.
Experimental studies demonstrate that the topical cutaneous application of 3% clioquinol cream will provide transdermal absorption of clioquinol into blood, which will result in mobile ZnCQ that is delivered to malignant sites, transports zinc into the ZIP-deficient malignant cells, and induces cytotoxic/tumor suppression effects. Treatment with the dopamine agonist, cabergoline, will decrease plasma prolactin level, thereby preventing prolactin-induced progression of androgen-independent malignancy.
FDA “Compassionate use” policies should permit clioquinol and cabergoline treatment of terminal androgen-independent cancer and without unnecessary delay.
ACKNOWLEDGMENT
Studies of LC Costello and RB Franklin cited herein were supported by NIH grants CA79903, DK076783, and DK42839.
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin 2016;66:7–30. [DOI] [PubMed] [Google Scholar]
- 2.Timms BG, Mohs TJ, Didio LJ. Ductal budding and branching patterns in the developing prostate. J Urol 1994;151:1427–32. [DOI] [PubMed] [Google Scholar]
- 3.Zaichick VYe Sviridova TV, Zaichick SV. Zinc in the human prostate gland: Normal, hyperplastic and cancerous. Int Urol Nephrol 1997;29:565–74. [DOI] [PubMed] [Google Scholar]
- 4.Franklin RB, Feng P, Milon B, Desouki MM, Singh KK, Kajdacsy-Balla A, et al. HZIP1 zinc uptake transporter down regulation and zinc depletion in prostate cancer. Mol Cancer 2005;4:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costello LC, Franklin RB. A comprehensive review of the role of zinc in normal prostate function and metabolism; and its implications in prostate cancer. Arch Biochem Biophys 2016;611:100–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Costello LC, Franklin RB, Narayan P. Citrate in the diagnosis of prostate cancer. Prostate 1999;38:237–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costello LC, Fenselau CC, Franklin RB. Evidence for operation of the direct zinc ligand exchange mechanism for trafficking, transport, and reactivity of zinc in mammalian cells. J Inorg Biochem 2011;105:589–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferrada E, Arancibia V, Loeb B, Norambuena E, Olea-Azar C, Huidobro-Toro JP, et al. Stoichiometry and conditional stability constants of Cu(II) or Zn(II) clioquinol complexes; implications for Alzheimer’s and Huntington’s disease therapy. Neurotoxicology 2007;28:445–9. [DOI] [PubMed] [Google Scholar]
- 9.Cherny RA, Atwood CS, Xilinas ME, Gray DN, Jones WD, McLean CA, et al. Treatment with a copper-zinc chelator markedly and rapidly inhibits beta-amyloid accumulation in Alzheimer’s disease transgenic mice. Neuron 2001;30:665–76. [DOI] [PubMed] [Google Scholar]
- 10.Costello LC, Franklin RB, Zou J, Naslund MJ. Evidence that human prostate cancer is a ZIP1-deficient malignancy that could be effectively treated with a zinc ionophore (Clioquinol) approach. Chemotherapy (Los Angel) 2015;4:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Costello LC, Franklin RB. Testosterone and prolactin regulation of metabolic genes and citrate metabolism of prostate epithelial cells. Horm Metab Res 2002;34:417–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goffin V Prolactin receptor targeting in breast and prostate cancers: New insights into an old challenge. Pharmacol Ther 2017;179:111–26. [DOI] [PubMed] [Google Scholar]
- 13.Costello LC, Franklin RB. Effect of prolactin on the prostate. Prostate 1994;24:162–6. [DOI] [PubMed] [Google Scholar]
- 14.Fischer T, Fagerlund C, Hartvig P. Absorption of 8-hydroxyquinolines through the human skin. Acta Derm Venereol 1978;58:407–11. [PubMed] [Google Scholar]
- 15.Stohs SJ, Ezzedeen FW, Anderson AK, Baldwin JN, Makoid MC. Percutaneous absorption of iodochlorhydroxyquin in humans. J Invest Dermatol 1984;82:195–8. [DOI] [PubMed] [Google Scholar]
- 16.Kadar T, Ben-David M, Pontes JE, Fekete M, Schally AV. Prolactin and luteinizing hormone-releasing hormone receptors in human benign prostatic hyperplasia and prostate cancer. Prostate 1988;12:299–307. [DOI] [PubMed] [Google Scholar]
- 17.Verhelst J, Abs R, Maiter D, van den Bruel A, Vandeweghe M, Velkeniers B, et al. Cabergoline in the treatment of hyperprolactinemia: A study in 455 patients. J Clin Endocrinol Metab 1999;84:2518–22. [DOI] [PubMed] [Google Scholar]
- 18.Colao A, Di Sarno A, Landi ML, Scavuzzo F, Cappabianca P, Pivonello R, et al. Macroprolactinoma shrinkage during cabergoline treatment is greater in naive patients than in patients pretreated with other dopamine agonists: A prospective study in 110 patients. J Clin Endocrinol Metab 2000;85:2247–52. [DOI] [PubMed] [Google Scholar]
- 19.Sabuncu T, Arikan E, Tasan E, Hatemi H. Comparison of the effects of cabergoline and bromocriptine on prolactin levels in hyperprolactinemic patients. Intern Med 2001;40:857–61. [DOI] [PubMed] [Google Scholar]
- 20.Colao A, Di Sarno A, Landi ML, Cirillo S, Sarnacchiaro F, Facciolli G, et al. Long-term and low-dose treatment with cabergoline induces macroprolactinoma shrinkage. J Clin Endocrinol Metab 1997;82:3574–9. [DOI] [PubMed] [Google Scholar]
- 21.Arduc A, Gokay F, Isik S, Ozuguz U, Akbaba G, Tutuncu Y, et al. Retrospective comparison of cabergoline and bromocriptine effects in hyperprolactinemia: A single center experience. J Endocrinol Invest 2015;38:447–53. [DOI] [PubMed] [Google Scholar]
- 22.Webster J, Piscitelli G, Polli A, Ferrari CI, Ismail I, Scanlon MF, et al. A comparison of cabergoline and bromocriptine in the treatment of hyperprolactinemic amenorrhea. Cabergoline comparative study group. N Engl J Med 1994;331:904–9. [DOI] [PubMed] [Google Scholar]
- 23.Boguszewski CL, dos Santos CM, Sakamoto KS, Marini LC, de Souza AM, Azevedo M, et al. A comparison of cabergoline and bromocriptine on the risk of valvular heart disease in patients with prolactinomas. Pituitary 2012;15:44–9. [DOI] [PubMed] [Google Scholar]


