Abstract
Prior research indicates that children of deployed parents are at risk for emotional problems, suggesting the utility of preventive efforts for military families. Effective parental socialization of children’s emotions is protective for children’s development, and parental experiential avoidance may impede parental emotion socialization, yet intervention studies in this area are lacking. This study examined the impact of a parenting program, After Deployment Adaptive Parenting Tools (ADAPT), on parental emotion socialization post-intervention (6 months post baseline) and whether intervention effects were moderated by parental experiential avoidance. The sample included 336 families (294 fathers and 313 mothers) with at least one deployed parent and a focal child aged 4–12. Families were randomized into either ADAPT (a 14-week group-based intervention) or control group. Self-reported data on parental emotion socialization and experiential avoidance were analyzed using structural equation modeling. Results showed that mothers who were assigned to the intervention had significant improved supportive emotion socialization and reduced non-supportive emotion socialization at post-intervention compared to controls. Mothers with higher levels of experiential avoidance assigned to the intervention group had higher levels of supportive emotion socialization at post-intervention. No significant intervention effects were found in fathers. This study provides support for the effects of the ADAPT program on maternal emotion socialization at 6-month post-baseline, and the role of experiential avoidance as a moderator. We discuss findings in relation to the different parental roles that mothers and fathers play in post-deployed families, as well as implications for personalized intervention programming.
Keywords: Emotion socialization, military families, parenting, intervention, experiential avoidance
Operations Enduring and Iraqi Freedom (OEF/OIF) have resulted in the deployments of large numbers of military personnel to Afghanistan and/or Iraq. The lives of about two million American children have been affected by the deployment of a parent (U.S. Department of Defense, 2014). The prevalence of posttraumatic stress disorder (PTSD) among the OEF/OIF veterans was found to be about 23.1% (ranged between 5.8% and 41.3%; Fulton et al., 2015). While most military parents do not show psychopathology, mental health problems associated with combat deployments can compromise parenting. Existing evidence shows that deployment-related stressors are associated with poor child adjustment via impaired parenting practices (Gewirtz, DeGarmo, & Zamir, 2018b). It is not surprising that children of deployed parents have been found to be at higher risk for emotional and behavioral problems compared to their civilian counterparts (Wadsworth, Bailey, & Coppola, 2017). Although research on military families has increased rapidly in the past decade, less research has focused on parenting in this population (Gewirtz & Youssef, 2016). Because effective parental socialization of children’s emotions is protective for children’s development (Eisenberg et al., 2001), and experiential avoidance may play an important role in parental emotion socialization (ES) (Brockman et al., 2016), this study investigated the effects of a parenting intervention designed for military families on parental ES practices and experiential avoidance as a moderator of intervention effects.
Parental emotion socialization practices
The stress associated with deployment and reintegration can result in the display of strong negative emotions, including anxiety, anger, and fear in the family (Drummet, Coleman, & Cable, 2003; Pincus, House, Christenson, & Alder, 2001). Combat-related physical injuries and/or mental health problems, and the at-home parent’s heightened distress or even secondary traumatization can complicate reintegration (Dirkzwager, Bramsen, Adèr, & van der Ploeg, 2005). And how parents react to children’s negative emotions and regulate those emotions can help or hinder children’s socio-emotional development (Baker, Fenning, & Crnic, 2011; Wong, McElwain, & Halberstadt, 2009). Indeed, the family is where children first become socialized in the world of emotions, and parents are critically important socializers (Grusec, 2011).
Parental reactions to children’s emotions (particularly negative emotions) are crucial indicators of parental emotion socialization/ES, which is distinguishable from more general parenting constructs such as parental warmth (Gottman, Katz, & Hooven, 1996). ES may be supportive or non-supportive, with each domain appearing to contribute unique variance to children’s adjustment (e.g., Baker et al., 2011; Gunzenhauser, Fäsche, Friedlmeier, & von Suchodoletz, 2014). Supportive parental ES practices include encouraging the discussion and expression of emotions, helping with problem-solving, and assisting to relieve distress. These behaviors have been labeled emotion-coaching (Gottman et al., 1996), which involve helping children to identify their feelings, showing validations and acceptance, and teaching effective emotion regulation strategies. On the other hand, non-supportive parental ES practices include dismissing children’s emotions, and using punishment to control children’s expression of negative emotions (Fabes, Poulin, Eisenberg, & Madden-Derdich, 2002).
Few evidence-based interventions have focused on ES, and no empirical studies have targeted post-deployed military families. While some parenting interventions address the topic of child emotion competence (Havighurst, 2003), existing evidence-based parent training programs predominantly take a behavior contingency approach with little attention to parental ES practices (e.g., Havighurst, Wilson, Harley, Prior, & Kehoe, 2010; Snyder et al., 2013). Recently, researchers have developed and evaluated the After Deployment Adaptive Parenting Tools (ADAPT) parent training program for post-deployed military families (Gewirtz, DeGarmo, & Zamir, 2018a), which includes skills to improve parental ES practices. ADAPT is a modification of the Parent Management Training – Oregon model (PMTO) (Forgatch & Patterson, 2010) with two key modifications in the areas of mindfulness exercises and parental ES skills (Pinna, Hanson, Zhang, & Gewirtz, 2017) as well as materials specific to the military context. Prior reports have documented program-related improvements in mothers’ and fathers’ parenting efficacy (Piehler, Ausherbauer, Gewirtz, & Gliske, 2016), couple parenting skills and children’s adjustment (Gewirtz et al., 2018a), parents’ mental health (Gewirtz, DeGarmo, & Zamir, 2016), and in dispositional mindfulness among engaged mothers (Zhang, Rudi, Zamir, & Gewirtz, 2018). However, no studies have yet tested whether the intervention was effective in improving parental ES. Therefore, this study evaluated the effects of ADAPT on parental ES practices.
Experiential avoidance as a moderator
In the current investigation, we also sought to understand how pre-existing parental emotional functioning (i.e., experiential avoidance) might predict (i.e., moderate) parents’ responsivity to ADAPT. Experiential avoidance refers to the inability to tolerate unwanted, distressing internal events (such as thoughts, feelings, memories, or bodily sensations), which results in attempts to avoid or change the context associated with those events (Hayes, Wilson, Gifford, Follette, & Strosahl, 1996). According to parental meta-emotion philosophy (Gottman et al., 1996), parents who find their own negative feelings painful or harmful (e.g., with high experiential avoidance) also may dismiss their children’s negative feelings. Indeed, experiential avoidance has been associated with depression, anxiety, and other types of emotion dysregulation problems (Tull, Gratz, Salters, & Roemer, 2004). It impedes emotional processing of traumatic events, at least in part facilitating the development and maintenance of PTSD symptoms (Erbes, Polusny, MacDermid, & Compton, 2008). In a prior study, Brockman et al. (2016) have also shown that male military service members’ experiential avoidance was associated with observed parenting practices above and beyond PTSD symptoms.
Given the extant literature that suggests a link between emotion regulation and parenting (for a review, see Crandall, Deater-Deckard, & Riley, 2015), we were interested in examining whether parents’ experiential avoidance (as an indicator of emotion regulation) would moderate the impact of the ADAPT program on parents’ emotion socialization practices. Parents with higher levels of experiential avoidance prior to the intervention likely have poorer emotion regulation skills and greater suppression of feelings and thoughts. These parents may learn better in part because they have more room for growth. Alternatively, because of their emotion regulation deficits, they may also face greater challenges in the intervention and show resistance to change, showing less improvement. Previously, Snyder et al. (2018) found that fathers in the ADAPT program who had higher (vs. lower) levels of experiential avoidance benefited more from the intervention in terms of reduced observed distress avoidance (a behavioral manifestation of experiential avoidance) which further led to improved parenting. We expected to see greater benefits to parents with higher baseline experiential avoidance in the ADAPT.
The current study
Researchers have mostly examined maternal ES, and only a few reports on this topic have included fathers. To what degree maternal and paternal ES practices within same family are correlated is, as yet, not understood, but many agree that mothers and fathers parent their children in different ways (Denham & Kochanoff, 2002; Stolz, Barber, & Olsen, 2005). Furthermore, evidence indicates gender differences in ES practices (Baker, Fenning, & Crnic, 2011; McElwain, Halberstadt, & Volling, 2007) as well as in intervention program engagement and satisfaction within the context of the ADAPT program (Pinna et al., 2017). Also, some participants in the ADAPT study were single parents. As such, we examined ES in mothers and fathers separately. The goals of the current study were to examine the effects of the ADAPT program on parental ES practices and the potential moderating effect of experiential avoidance on the intervention effects. We report pre- and post-intervention (6-month post-baseline) data from a randomized controlled trial (RCT) of the ADAPT program. Our hypotheses are as follows: 1) mothers and fathers who were randomly assigned to the ADAPT group would show significantly increased levels of supportive ES and decreased levels of non-supportive ES at post-intervention, compared to the controls; 2) mothers’ and fathers’ experiential avoidance would moderate these intervention effects, such that those with higher (vs. lower) levels of experiential avoidance will show greater improvements in parental ES outcomes.
Method
Participants.
The sample consisted of 314 mothers and 294 fathers from 336 families (87% married) who participated in an RCT of the ADAPT program. Because one of the families constituted two mothers, one mother from this family was randomly excluded to avoid nonindependence-related data issues, yielding 313 mothers. The mothers (n = 313; 18.2% deployed) were aged 35.69 years on average (SD = 5.89; range 23.08–51.15), primarily White (92.3%), with a small percentage being African American (2.2%), Native American (1.3%), Asian American (1.6%), and multi-racial (2.2%). The fathers (n = 294; 95.6% deployed) were aged 37.73 years on average (SD = 6.54; range 23.74–58.33), primarily White (88.5%) with a small percentage being African American (5.1%), Native American (0.3%), Asian American (2.4%), and multi-racial (2.0%). About half of the sample reported having a 4-year college degree or higher (52.1% mothers and 47.6% fathers). The majority reported annual household income between $40,000 to $79,999 (42.5% mothers and 42.7% fathers) or $80,000 to $119,999 (27.5% mothers and 31.1% fathers). Families included 2.34 children on average (SD = 0.96). These sample demographics are somewhat representative of the National Guard/Reserve parent population with school-aged children in the Midwest. Children in the study (one child per family) were 53.3% female and aged between 4 and 12 years, M = 8.39, SD = 2.52. Among the sample of 336 families, 81.0% (n = 272) were two-parent families (271 heterosexual couples). Within the two-parent families, 88.2% (n = 239) of the 271 couples consisted of a deployed father and a civilian mother, 7.4% (n = 20) consisted of dual-deployed couples, and 4.4% (n = 12) consisted of couples with a deployed mother and a civilian father. In addition, 64 families had only one deployed parent who participated in the study including 41 deployed mothers and 23 deployed fathers.
Procedure.
Families were eligible to participate in the study if at least one parent had been deployed to Afghanistan and/or Iraq since 2001, and at least one child was 4–12 years old. Participants were recruited using multiple strategies including presentations at events for NG/R families, a targeted mailing at Veterans Affairs Medical Center, the social media (e.g., Facebook), flyers or prints, and word of mouth. Interested families completed an online survey to screen for eligibility and consent to participate. Because participating parents may systematically choose a target child whom they were most or least concerned about if they had multiple children, during the first wave of recruitment process, the oldest child in the family was selected as the target child. To prevent oversampling older vs. younger children, for the families recruited after the first wave, the youngest child was selected. In a few cases when the oldest or youngest child was not willing or able to participate, parents made their own choice regarding target child. Families completed baseline online surveys and in-home assessment, and were randomized to participate in the ADAPT intervention (60%) or a control condition which consists of service-as-usual (40%). Families in the control condition were emailed a list of “tip sheets” and online parenting resources shortly after their completion of baseline assessment. The current study used data collected at baseline (T1) and 6-month post-baseline (T2); at both times, participants received email links to online surveys. For more details about the larger study, (see Gewirtz et al., 2016, 2018b). All study procedures were approved by University of Minnesota Institutional Review Board.
Intervention.
The intervention program consists of 14 2-hour sessions in total, delivered weekly in groups of 6 to 15 parents. Each group is led by 2–3 trained facilitators, who were military (National Guard/Reserve and veterans) or non-military professional service providers (e.g., social workers). Their training included 11 days of workshop training and biweekly ongoing supervision from the PI of the study and other certified trainers. The six domains of positive parenting practices taught are skill encouragement, positive involvement, problem-solving, monitoring, discipline, and emotion socialization (Gewirtz, Pinna, Hanson, & Brockberg, 2014). Two key innovations of the ADAPT program are the addition of mindfulness and emotion coaching to the ‘standard’ behavioral parent training skills, designed to enhance parental emotion regulation skills and effectively respond to children’s emotions. Parenting skills were taught each week building on previous topics. Mindfulness and emotion coaching components were infused into each session. All sessions were videotaped to measure fidelity of implementation. In addition to group sessions, online resources are accessible, which included videos demonstrating parenting principles, handouts summarizing each session, and mindfulness exercises.
Measures
Emotion socialization (ES) was measured with the Coping with Children’s Negative Emotions Scale (CCNES; Fabes, Eisenberg, & Bernzweig, 1990) at both T1 and T2. The CCNES is a widely-used instrument with good internal consistency and test-retest reliability (Fabes et al., 2002). The scale consists of 12 vignettes, describing possible situations where a child may experience negative emotions such as nervousness, fear, or sadness. An online survey administration error resulted in one of the vignettes not being delivered to a substantial proportion of the sample. Thus, that vignette was excluded at both T1 and T2, resulting in 11 vignettes1. Each vignette provided a scenario with 6 possible parental reactions; parents endorsed the likelihood of each reaction to their child on a 7-point scale (1 = very unlikely; 7 = very likely). The six reactions are: punitive reaction (PR; e.g., “send my child to his/her room to cool off”), minimization reaction (MR; e.g., “tell my child that he/she is over-reacting”), distress reaction (DR; e.g., “feel upset and uncomfortable because of my child’s reactions”), emotion-focused response, (EF; e.g., “do something fun with my child to help him/her forget about what scared him/her”), problem-focused response (PF; e.g., “suggest that my child think about something relaxing so that his/her nervousness will go away”), and expression encouragement (EE; e.g., “tell my child it’s OK to cry when he/she feels bad”). Scores for the six responses were calculated with a higher score indicating a greater tendency of endorsing that reaction. The internal consistency reliability (Cronbach’s α) of the six subscales were mostly between 0.74 to 0.90, except for mothers’ DR at both times (αs = .65 and .70 at T1 and T2, respectively) and PR at T1 (α = .67). In a psychometric study of the CCNES with predominantly mothers, Fabes et al. (2002) also reported relatively lower internal consistency reliability for these two subscales (αs = .70 and .69 for DR and PR respectively vs. αs > .78 for all other subscales). With mother samples, McElwain, Halberstadt, & Volling (2007) found lower α for PR ( .64). Hurrell, Hudson, & Schniering (2015) found low α for DR ( .54) and dropped this subscale. Considering that an α greater than .70 is satisfactory (Bland & Altman, 1997) and that latent constructs are used in the analyses, no subscales were dropped in our analyses.
Experiential Avoidance was assessed with the Acceptance and Action Questionnaire – II (AAQ-II; Bond et al., 2011). The AAQ-II is a unidimensional scale with 7 items (e.g., “I’m afraid of my feelings”); respondents rate each item on a 7-point scale (1 = never true, 7 = always true). Items include “Worries get in the way of my success” and “I worry about not being able to control my worries and feelings.” The Cronbach’s αs were .93 for both mother and father samples, showing an acceptable internal consistency reliability. A composite score was created such that higher score indicates higher level of experiential avoidance.
PTSD symptoms were measured using the military or civilian version of the Posttraumatic Stress Disorder Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993). The military version of the PCL asks about symptoms in response to stressful military experiences and the civilian version of the PCL asks about symptoms in response to stressful life experiences. The scale has shown good internal reliability and validity in previous research (Wilkins, Lang, & Norman, 2011). Parents were asked to rate 17 items on a 5-point scale 1 (not at all) to 5 (extremely). A composite score was calculated such that higher scores indicate greater symptom severity (αs = .91 and .95 for mothers and fathers, respectively). About 15% of fathers and 6.9% of mothers met clinical cutoff criteria for PTSD (Hoge et al., 2004).
Depression symptoms were measured by parents’ self-reports using the 25-item depression subscale of the Hopkins Symptom Checklist (HSCL-25; Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, 1974). Items were rated on a 4-point scale 1 (not at all) to 4 (extremely). An average score was created with higher scores indicating greater symptom severity (αs = .93 and .95, for mothers and fathers, respectively).
Demographic variables included parent’s self-reported education, annual household income, marital status (0 = not married; 1 = married), and the target child’s age.
Deployment-related variables included: times of deployment, cumulative length of deployments (scored on a scale ranging from 1 = 6 months or less to 7 = 37 months or more), and time interval between a parent’s T1 online survey date and date of the deployed parent’s most recent return home. For nondeployed parents, times and cumulative length were entered as zero in the data. For the time interval variable, when there was only one deployed parent in the family, that deployed parent’s last return date was used (in most cases, the father was the deployed parent); when there were two deployed parents in the family, the more recent return date was used. In mother sample, time since return M = 2.53 years, SD = 2.35; in father sample, time since return M = 2.53 years, SD = 2.34. The range of this variable was between 0 to 9.85.
Analysis Plan
Data analysis plan followed several stages. First, descriptive statistics and correlation matrices were computed and examined for key study variables. Second, mother and father measurement models were separately estimated including four latent constructs: supportive ES at T1/T2, and non-supportive ES at T1/T2. Third, intent-to-treat (ITT) intervention effects on outcome variables (i.e., supportive and nonsupportive ES T2) were estimated in two separate structural models for mothers and fathers without including a moderator of intervention effects. Lastly, experiential avoidance was included as a moderator of intervention outcomes in two separate structural models for mothers and fathers. In addition to supportive and nonsupportive ES T1, control variables included demographic and deployment-related variables, as well as parent PTSD and depression. If model fit is less than acceptable, nonsignificant control variables may be dropped. Of note, interclass correlations (ICCs) for parents within the same intervention groups were calculated for all subscales of the CCNES, and all ICCs at T1, T2, or changes scores (T1–T2) were lower than .020 with the exceptions of MR at T2 (.038), PF at T1 (.041), and EF at T1 (.077). Model fit was evaluated using recommended criteria (McDonald & Ho, 2002): a chi-square ratio (χ2 /df) below 2.0, a comparative fit index (CFI) above .95, a standardized root mean square residual (SRMR) below .08, and a root-mean-square error of approximation (RMSEA) below .06. Chi-square tests for overall model fit are sensitive to sample size, and the p-values tend to be significant in studies with large samples (Schumacker & Lomax, 2010). All structural equation modeling analyses were conducted in Mplus 7.4.
Missing data.
CCNES T2 data had nonnegligible missing data, particularly among families in the intervention group, due to delays in intervention delivery for some cohorts of families2. Fathers’ data had 3.1% missing on all subscales of the CCNES T1, 3.4% missing on the AAQ, and 35.7% missing on all subscales of the CCNES at T2. No difference was found regarding the CCNES T2 missingness among fathers in the intervention vs. control group, but it was associated with fathers who were assigned to the intervention but did not complete the intervention vs. those who completed (p < .001) (Completion of the intervention was defined as attending to 4 or more group sessions, in consistency with prior studies evaluating PMTO), as well as lower levels of annual household income and education (ps < .01). Mothers’ data had 2.2% missing on all subscales of the CCNES T1, 0.99% missing on the AAQ, and 25.9% missing on all subscales of the CCNES T2. Missing value analyses showed that CCNES T2 was more likely to be missing among mothers who were assigned to the intervention vs. control group (p < .01), who did not complete the intervention vs. those who completed the intervention (p < .001), and who reported lower levels of distress reaction at T1 as well as less marriage length than those who were not missing (ps < .05). Full information maximum likelihood (FIML) was used to handle missing data which is unbiased and efficient in model estimation (Enders & Bandalos, 2001). In particular, intervention completion was included in the final models as an auxiliary variable because it was found to be correlated with missing data. Following the approach by Graham (2003), the auxiliary variable was added to structural models in Mplus by 1) covarying the auxiliary variable with all exogenous manifest variables in the model and 2) covarying the auxiliary variable with the residuals for all the manifest variables that are predicted in the model.
Results
Bivariate correlations showed that the three indicators of the supportive ES construct and the three indicators of the non-supportive ES construct were moderately or strongly correlated with each other. Experiential avoidance was weakly associated with ES indicators. At family-level, ES practices of mothers and fathers within same family were mostly only weakly or nonsignificantly correlated among two-parent families (see Table 1). Paired-sample t-tests showed that other than distress reaction (t(247) = 0.95, p = .34), mothers and fathers within same family reported significantly different levels of ES practices at baseline. Specifically, within same family, mothers reported higher supportive ES practices including expression encouragement (t(248) = −7.64, p < .001), emotion-focused response (t(250) = −4.80, p < .001), and problem-focused response (t(250) = −5.92, p < .001), as well as lower nonsupportive ES practices including minimization reaction (t(246) = 9.47, p < .001) and punitive reaction (t(248) = 5.07, p < .001), relative to fathers. The tests were also performed for 6-month follow-up data, showing the same gender difference for ES practices.
Table 1.
Correlations, means, and standard deviations of key study variables by parent gender.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. EE T1 | .03 | .53 | .48 | −.33 | −.25 | −.28 | .67 | .41 | .34 | −.29 | −.29 | −.28 | −.13 | |
| 2. PF T1 | .59 | .05 | .65 | −.27 | −.08 | −.17 | .32 | .51 | .42 | −.23 | −.18 | −.17 | −.19 | |
| 3. EF T1 | .54 | .78 | .21 | −.19 | .09 | −.09 | .31 | .46 | .62 | −.24 | −.05 | −.18 | −.00 | |
| 4. DR T1 | −.37 | −.45 | −.41 | .14 | .35 | .46 | −.21 | −.18 | −.11 | .58 | .32 | .38 | .32 | |
| 5. MR T1 | −.15 | −.20 | −.12 | .54 | .12 | .69 | −.19 | −.04 | .04 | .23 | .69 | .50 | .08 | |
| 6. PR T1 | −.24 | −.31 | −.23 | .63 | .74 | .21 | −.21 | −.09 | −.03 | .31 | .59 | .63 | .09 | |
| 7. EE T2 | .61 | .39 | .33 | −.26 | −.17 | −.26 | .18 | .62 | .51 | −.35 | −.32 | −.28 | −.05 | |
| 8. PF T2 | .31 | .52 | .44 | −.31 | −.16 | −.27 | .58 | .09 | .73 | −.34 | −.20 | −.22 | −.15 | |
| 9. EF T2 | .26 | .42 | .52 | −.35 | −.12 | −.25 | .55 | .83 | .21 | −.24 | −.07 | −.15 | −.03 | |
| 10. DR T2 | −.22 | −.33 | −.29 | .60 | .30 | .40 | −.41 | −.52 | −.55 | .18 | .45 | .57 | .21 | |
| 11. MR T2 | −.15 | −.18 | −.10 | .22 | .52 | .36 | −.26 | −.24 | −.18 | .45 | .13 | .67 | .12 | |
| 12. PR T2 | −.18 | −.28 | −.15 | .39 | .54 | .56 | −.30 | −.40 | −.37 | .59 | .72 | .12 | .17 | |
| 13. EA | −.12 | −.15 | −.15 | .21 | .15 | .12 | −.13 | −.28 | −.28 | .29 | .04 | .20 | .17 | |
| M | Mother | 5.12 | 5.85 | 5.60 | 2.82 | 2.56 | 2.46 | 5.11 | 5.81 | 5.50 | 2.75 | 2.42 | 2.34 | 16.82 |
| Father | 4.52 | 5.53 | 5.31 | 2.89 | 3.13 | 2.74 | 4.54 | 5.43 | 5.23 | 2.84 | 2.91 | 2.64 | 16.76 | |
| SD | Mother | 0.91 | 0.66 | 0.78 | 0.69 | 0.79 | 0.67 | 1.01 | 0.74 | 0.82 | 0.69 | 0.76 | 0.71 | 8.23 |
| Father | 1.02 | 0.78 | 0.85 | 0.81 | 0.86 | 0.84 | 1.04 | 0.80 | 0.86 | 0.77 | 0.80 | 0.79 | 8.09 | |
| N | Mother | 306 | 306 | 306 | 306 | 306 | 306 | 232 | 232 | 232 | 232 | 232 | 232 | 309 |
| Father | 285 | 285 | 285 | 285 | 285 | 285 | 189 | 189 | 189 | 189 | 189 | 189 | 284 | |
Note. EE = expression encouragement; PF = problem-focused response; EF = emotion-focused response; DR = distress reaction; MR = minimization reaction; PR = punitive reaction; T1 = baseline; T2 = 6-month post-baseline; EA = experiential avoidance.
Correlations in the upper right of the diagonal are for mothers and those in the lower left are for fathers. Correlations between mothers and fathers from the same family were calculated and the coefficients are shown on the diagonal. Statistically significant correlation coefficients are bolded (α = .05).
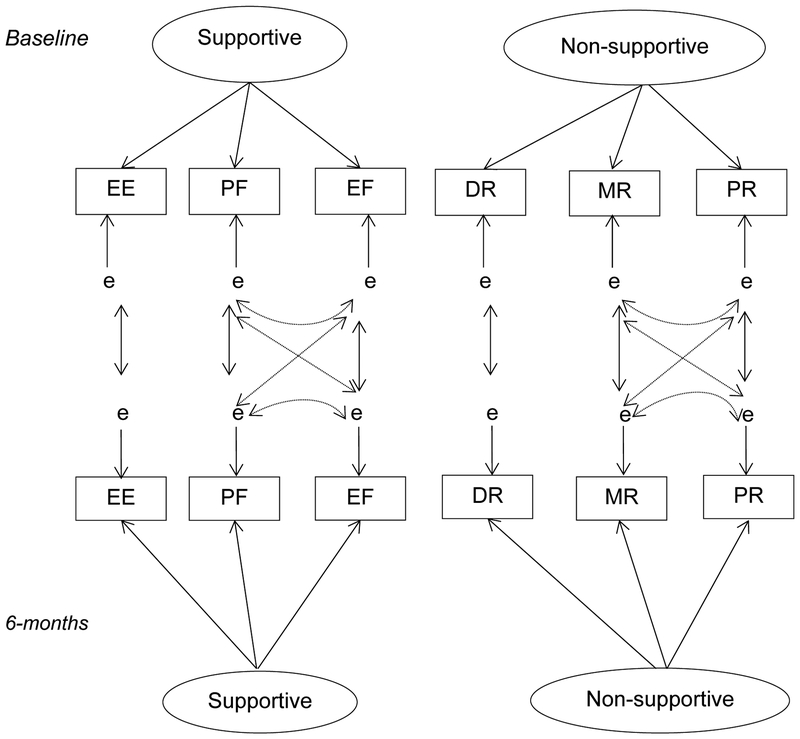
A basic measurement model (Figure 2) was estimated prior to conducting a structural model. The measurement model included four latent constructs: supportive ES T1 and T2, non-supportive ES at T1 and T2. According to the original six-factor structure of the scale (Fabes, Eisenberg, & Bernzweig, 1990), supportive ES has three indicators: emotion-focused response (EF), problem-focused response (PF), and expression encouragement (EE); non-supportive ES also has three indicators: punitive reaction (PR), minimization reaction (MR), and distress reaction (DR). The measurement model based on these six factors was evaluated and the model fit was acceptable but not optimal: fathers, χ2 (42) = 119.39, p < .001, χ2 /df > 2.0, CFI = .96, RMSEA = .08, SRMR = .08; mothers, χ2 (42) = 119.05, p < .001, χ2 /df > 2.0, CFI = .96, RMSEA = .08, SRMR = .08. This led to the testing of a possible four-factor structure for the CCNES, supported by a prior study showing that PF and EF may be combined into a single factor and PR and MR may be combined into a single factor (Fabes et al., 2002). Then, a second measurement model was tested in which the concurrent and longitudinal correlations between PF and EF, as well as between MR and PR were specified in the model (see dotted lines in Figure 2). The results showed acceptable fit to the data: fathers, χ2 (34) = 40.97, p = .19, χ2 /df = 1.21, CFI = 1.00, RMSEA = .03, SRMR = .03; mothers, χ2 (34) = 60.91, p < .01, χ2 /df = 1.79, CFI = .98, RMSEA = .05, SRMR = .04. Chi-square difference tests supported the second measurement model as a better-fitting model (ps < .001), which was chosen for further structural model analysis. The standardized factor loadings of DR, PR, and MR ranged between 0.49 to 1.00, whereas those of EF, PF, EE ranged between .56 to .86, except for MR T1 (0.39).
Figure 2.
Hypothesized measurement model.
Note: EE = expression encouragement; PF = problem-focused response; EF = emotion-focused response; DR = distress reaction; MR = minimization reaction; PR = punitive reaction
To estimate the ITT intervention effects, in two models with fathers and mothers separately, outcomes (nonsupportive ES and supportive ES at T2) were predicted by intervention condition (ADAPT = 1, control = 0) and corresponding ES scores at T1, as well as control variables while including intervention completion as an auxiliary variable. Control variables were also used to predict outcomes and covaried with each other which included child age, parent education, income, marital status, times and length of deployment, time since return, parent PTSD and depression. The model for fathers’ ES showed good fit to the data: χ2 (116) = 128.29, p = .21, χ2 /df = 1.11, CFI = 0.99, RMSEA = .02, SRMR = .04. Intervention condition did not significantly predict outcomes (ps > .05). The model for mothers’ ES showed good fit to the data: χ2 (116) = 195.42, p < .001, χ2 /df = 1.74, CFI = 0.97, RMSEA = .05, SRMR = .04. The ADAPT condition significantly predicted increased supportive ES T2 (B = 0.21, SE = 0.10, β = 0.13, p < .05, Cohen’s d = 0.13) and decreased non-supportive ES T2 (B = −0.26, SE = 0.07, β = −0.24, p < .001, Cohen’s d = −0.24) in mothers. That is, mothers who were randomly assigned to the ADAPT intervention condition relative to the control condition showed significant increases in supportive ES, and decreases in non-supportive ES at 6-month post-baseline. For fathers, there were non-significant treatment effects on supportive ES and non-supportive ES.
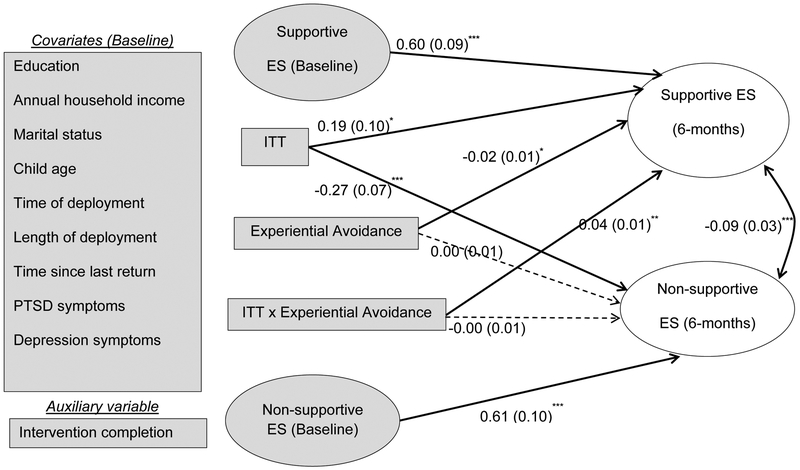
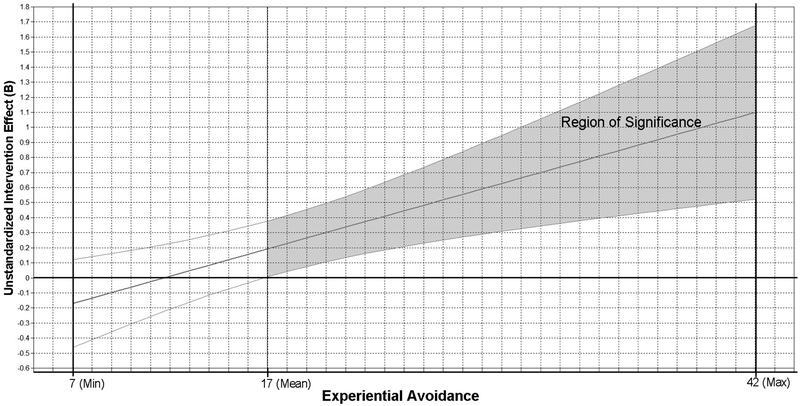
To test the moderation effects of experiential avoidance, in two models with fathers and mothers separately, outcomes were predicted by intervention condition (ADAPT = 1, control = 0), mean-centered experiential avoidance, and moderation (mean-centered experiential avoidance multiplied by intervention condition), and corresponding ES scores at T1, as well as control variables while including intervention completion as an auxiliary variable. Control variables were also used to predict outcomes and covaried with each other which included child age, parent education, income, marital status, times and length of deployment, time since return, parent PTSD and depression. The structural equation model for fathers included all control variables and showed an acceptable fit to the data: χ2 (132) = 152.49, p = .11, χ2 /df = 1.12, CFI = .99, RMSEA = .02, SRMR = .04. The results showed that intervention condition did not significantly predict ES outcomes at T2 (ps > .05). Experiential avoidance predicted decreased supportive ES T2 significantly, B = −0.04, SE = 0.01, β = −.44, p < .01, and increased nonsupportive ES T2 with a trend towards significance, B = 0.02, SE = 0.01, β = .26, p = .06. Marital status was associated with nonsupportive ES T2 such that married fathers showed higher nonsupportive ES T2 compared to those who were not married, B = 0.29, SE = 0.15, β = .14, p < .05. The structural model for mothers showed a good fit to the data: χ2 (132) = 229.82, p < .001, χ2 /df = 1.74, CFI = .97, RMSEA = .05, SRMR = .05. Among mothers, experiential avoidance did not moderate the ITT effect on decreased nonsupportive ES T2, but it moderated the ITT effect on increased supportive ES T2, B = 0.04, β = .30, bootstrapped 95% CIs [0.01, 0.06], p < .01. The moderation effect and its region of significance revealed that mothers with higher levels of experiential avoidance had significantly greater improvement in supportive ES from T1 to T2 if they were randomized into the ADAPT group, relative to those with lower levels of experiential avoidance.
Discussion
Using an RCT research design, the current study evaluated the ITT intervention effects of ADAPT on parental ES in mothers and fathers in post-deployed military families at 6-month post-baseline, and whether the effects were moderated by experiential avoidance. Mothers in the intervention reported significantly increased supportive ES (although effect size was small) and decreased non-supportive ES (with a modest effect size) relative to controls. Mothers with higher vs. lower levels of experiential avoidance benefited more from the intervention by reported increased supportive ES. Our data did not reveal significant improvements in ES practices for fathers who were in the intervention group (vs. control) group at 6-months post-baseline.
Effective parents provide not only behavioral support to their children, but also emotional support and assistance; this is particularly important when families are experiencing stressful transitions. The ADAPT program addresses six core parenting skills: teaching through encouragement, discipline, problem-solving, monitoring, positive involvement with children, and emotion socialization (ES). While ES is a key theme throughout, two out of 14 sessions especially focus on some of the effective ways in coping with children’s negative emotions. Strategies including in-group role-play, discussions, and online educational resources (e.g., video) are utilized to train parents to effectively recognize, validate, and help regulating children’s negative emotions. Parents learn that frequent punitive or minimizing reactions can be maladaptive for children’s emotional development. Finally, by coaching parents to attend and regulate their own emotions, ADAPT can assist parents in interrupting the cycle of negative escalating emotional expression that emanates from the distress parents experience when faced with their children’s displays of negative emotions. These components are consistent with the conceptualizations of supportive and non-supportive ES in the measurement we used. As we anticipated, mothers in the intervention group showed significant increased supportive ES and decreased non-supportive ES at 6-month post-baseline.
The ADAPT intervention improved both supportive and non-supportive ES in mothers, and the program’s impact was larger on non-supportive ES. Parents who habitually engage non-supportive ES practices have been described as if “they preferred a happy child and often found these negative states in their child quite painful” (Gottman et al., 1996, p.245). Non-supportive parental ES practices may be particularly stressful for children. Biological data suggested that children who live in a stressful environment would show increased physiological activation (i.e., stress hormones), and if the hyper-activation is maintained over time, they may be unable to return to a normal physiological baseline (Grusec, 2011). It is possible that supportive ES practices might require a more sophisticated skill set and thus take a longer time to consolidate. In parallel, somewhat, previous research showed that parents who received the PMTO intervention relative to control group showed reduced coercive parenting first, which in turn led to increased positive parenting (Patterson, Forgatch, & DeGarmo, 2010).
Unlike the opposite of non-supportive ES (which is to restrain from punishing, minimizing or feeling distress), supportive ES involves an active and motivated approach to parenting. Although mothers likely in general feel distress for what their children are feeling in stressful situations (Manini et al., 2013), those who habitually engage in experiential avoidance may feel more such distress (Tiwari et al., 2008), which poses difficulties for engaging supportive parental ES practices. Research has suggested that mothers tend to exhibit more supportive parenting if their emotions are child-oriented (Dix, Gershoff, Meunier, & Miller, 2004). That is, the more mothers are oriented to their own emotions (typically observed in mothers with poor emotion regulation), the more they tend to disengage from or resist their children’s negative emotions. Our analysis showed that mothers with higher vs. lower levels of experiential avoidance had greater gains in supportive ES practices from the ADAPT intervention. This indicated that mothers with greater risk of experiential avoidance (i.e., emotion regulation deficits) had greater gains in supportive ES practices at 6-month follow-up. Given the evidence that the ADAPT program indirectly improved maternal emotion regulation (Gewirtz et al., 2016), it is conceivable that the program may also indirectly reduced experiential avoidance, because experiential avoidance is a correlate of emotion dysregulation (Aldao, Nolen-Hoeksema, & Schweizer, 2010). The ADAPT curriculum has infused mindfulness exercises into all sessions, cultivating skills that allow parents to be aware of their feelings and thoughts without getting caught up by them, which are essential for parenting (Zhang et al., 2017). Thus, mothers with higher vs. lower levels of emotion dysregulation (can be measured through experiential avoidance) may have become more equipped to regulate their own emotions and thus showed greater gains in supportive parental ES in the intervention.
The ADAPT condition did not improve fathers’ ES at 6-months post-baseline. Our first speculation is that fathers may need more time to show desirable outcomes. Researchers found evidence supporting significant improvements in some fathers’ parenting in the ADAPT program only at 1–2 years post-baseline (Snyder et al., 2018). During the intervention, fathers reported lower levels of satisfaction with the ADAPT group sessions than mothers did (Pinna et al., 2017), suggesting that fathers may find group materials less relevant to their parenting experiences. This is perhaps due to the fact that fathers had fewer opportunities to practice parenting than mothers - especially those who were absent and just returned home after deployment. Parenting-related outcomes, including parental ES, may be detectable at a later time point as fathers have more parenting practice after participating in an intervention. We also speculate that our null findings for fathers may be related to differences between fathering and mothering in the domains of emotion. For example, fathers do not engage in emotion-related conversations with children as frequently as mothers (Fivush, Brotman, Buckner, & Goodman, 2000), which gives them fewer opportunities to practice emotion-related parenting. Lastly, gender and deployment status are confounded in our sample, as most fathers in our sample were post-deployed military service members. Deployed service members may have been trained to suppress or “turn off” their emotions because emotions may endanger their survival or hinder mission completion in combat zones (Lorber & Garcia, 2010). Thus, emotion-related parenting may turn out to be a relatively strange, or at least difficult topic for these fathers. It is unclear whether civilian fathers may benefit from the ADAPT intervention. Future studies may oversample civilian fathers and deployed mothers to address this question.
The current study has some limitations. First, primary outcome variables were assessed via self-reports which are subject to biases. Using observational or multi-informant data in future studies would address these concerns. Second, as mentioned above, 6-months post-baseline may not provide sufficient time for some parents (e.g., fathers) to strengthen parental ES practices. Data collected at later time points will allow for other analytical methods such as linear growth modeling in examining prospective changes in these desirable outcomes. Third, there was nonnegligible missing data at 6-months post-baseline, although we included the variables associated with missingness while using FIML to reduce the potential biases. Last but not least, given the uniqueness of post-deployed families, any generalization of the findings to other stressed or distressed families should be made with caution. In particular, our findings should not be extrapolated to families from non-Euro-American cultures due to the influences of culture on caregivers’ ES strategies (Friedlmeier, Corapci, & Cole, 2011; Grusec, 2011).
The current study has contributed to the literature by demonstrating the effects of a parent training program on maternal ES in a sample of post-deployed military families. Structural equation modeling allowed us to examine unobserved variables beyond the specific CCNES subscales, and thus strengthen the validity of the measures. Finally, our findings on experiential avoidance as a moderator of improvements in maternal supportive ES have important implications for personalized preventive interventions. For example, targeting different subgroups of mothers according to their baseline levels of experiential avoidance may improve the efficiency and effectiveness of parenting and mental health interventions.
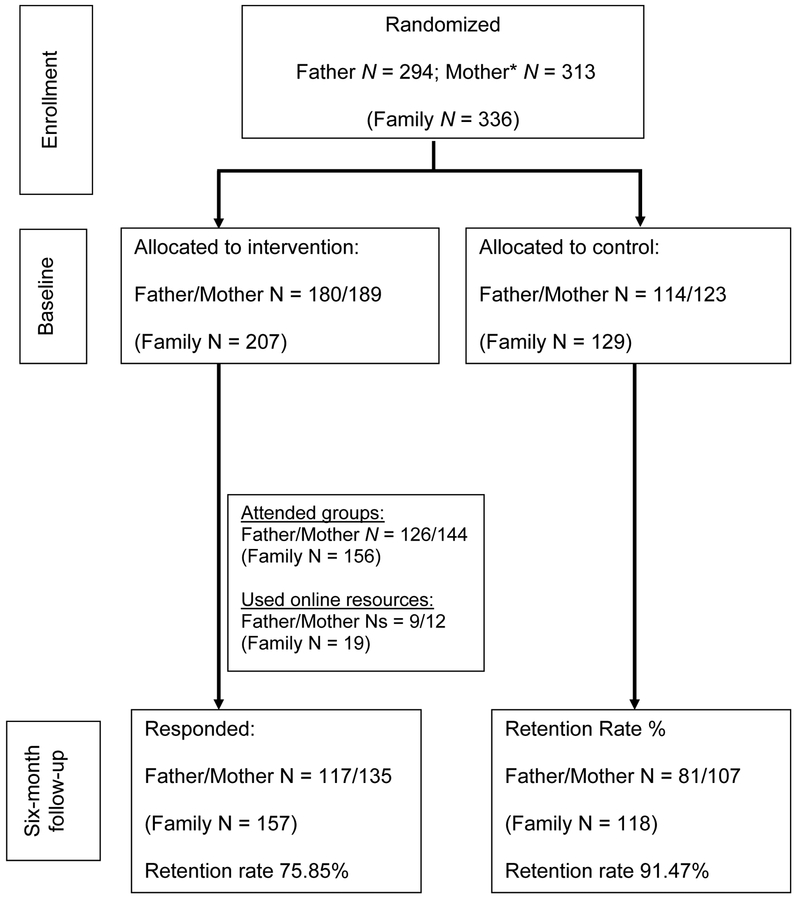
Figure 1.
A CONSORT diagram of the ADAPT study.
Note: * One participating family had two female parents and only one mother was included here.
Figure 3.
Unstandardized model estimates of the moderation model (mothers). *p < .05. **p < .01. ***p < .001. Standard errors are shown in the parentheses. ES = emotion socialization. ITT = intent-to-treat intervention. Nonsignificant paths are shown as dotted line. Model fit: χ2 (132) = 229.82, p < .001, χ2 /df = 1.74, CFI = .97, RMSEA = .05, SRMR = .05. R2 (Nonsupportive ES) = .52 (p < .001). R2 (Supportive ES) = .45 (p < .001). All baseline control variables (shaded in grey) were specified to covary with each other.
Figure 4.
Experiential avoidance moderated intervention effect on Supportive Emotion Socialization at 6-months among mothers.
Note: The band indicates the 95% Confidence Intervals of the unstandardized treatment effect (intent-to-treat analysis). X-axis: Raw scores of the experiential avoidance measure. In the mother sample, 43.4% were within the region of significance (α = .05).
Footnotes
The findings reported in this article were presented at the 25th Annual Meeting of the Society for Prevention Research (SPR) in 2017.
The excluded vignette was: “if my child is participating in some group activity with his/her friends and proceeds to make a mistake and then looks embarrassed and on the verge of tears, I would …”.
Some families in the intervention group missed T2 assessment because they were nearly ready for T3 (1-year post-baseline) assessment by the time of their completion of the intervention, which are not included in this report.
Contributor Information
Abigail H Gewirtz, Department of Family Social Science and Institute of Child Development, University of Minnesota – Twin Cities.
Timothy F Piehler, Department of Family Social Science, University of Minnesota – Twin Cities.
References
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30, 217–237. 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- Baker JK, Fenning RM, & Crnic KA (2011). Emotion socialization by mothers and fathers: Coherence among behaviors and associations with parent attitudes and children’s social competence. Social Development, 20, 412–430. 10.1111/j.1467-9507.2010.00585.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, … Zettle RD (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42, 676–688. 10.1016/j.beth.2011.03.007 [DOI] [PubMed] [Google Scholar]
- Bland J, & Altman D (1997). Statistics Notes: Cronbach’s Alpha. BMJ: British Medical Journal, 314(7080), 572–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockman C, Snyder J, Gewirtz A, Gird SR, Quattlebaum J, Schmidt N, … DeGarmo D (2016). Relationship of service members’ deployment trauma, PTSD symptoms, and experiential avoidance to postdeployment family reengagement. Journal of Family Psychology, 30, 52–62. 10.1037/fam0000152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crandall A, Deater-Deckard K, & Riley AW (2015). Maternal emotion and cognitive control capacities and parenting: A conceptual framework. Developmental review, 36, 105–126. 10.1016/j.dr.2015.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denham S, & Kochanoff AT (2002). Parental contributions to preschoolers’ understanding of emotion. Marriage & Family Review, 34, 311–343. 10.1300/J002v34n03_06 [DOI] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, & Covi L (1974). The Hopkins Symptom Checklist (HSCL): A self‐report symptom inventory. Systems Research and Behavioral Science, 19, 1–15. 10.1002/bs.3830190102 [DOI] [PubMed] [Google Scholar]
- Dirkzwager AJ, Bramsen I, Adèr H, & van der Ploeg HM (2005). Secondary traumatization in partners and parents of Dutch peacekeeping soldiers. Journal of Family Psychology, 19, 217–226. 10.1037/0893-3200.19.2.217 [DOI] [PubMed] [Google Scholar]
- Dix T, Gershoff ET, Meunier LN, & Miller PC (2004). The affective structure of supportive parenting: Depressive symptoms, immediate emotions, and child-oriented motivation. Developmental Psychology, 40, 1212–1227. 10.1037/0012-1649.40.6.1212 [DOI] [PubMed] [Google Scholar]
- Drummet AR, Coleman M, & Cable S (2003). Military families under stress: Implications for family life education. Family Relations, 52, 279–287. 10.1111/j.1741-3729.2003.00279.x [DOI] [Google Scholar]
- Eisenberg N, Losoya S, Fabes RA, Guthrie IK, Reiser M, Murphy B, … & Padgett SJ (2001). Parental socialization of children’s dysregulated expression of emotion and externalizing problems. Journal of family Psychology, 15, 183–205. 10.1037/0893-3200.15.2.183 [DOI] [PubMed] [Google Scholar]
- Enders CK, & Bandalos DL (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural equation modeling, 8, 430–457. 10.1207/S15328007SEM0803_5 [DOI] [PubMed] [Google Scholar]
- Erbes CR, Polusny MA, MacDermid S, & Compton JS (2008). Couple therapy with combat veterans and their partners. Journal of Clinical Psychology, 64, 972–983. 10.1002/jclp.20521 [DOI] [PubMed] [Google Scholar]
- Fabes RA, Eisenberg N & Bernzweig J (1990). Coping with Children’s Negative Emotions Scale (CCNES): Description and scoring. Tempe, AZ: Arizona State University. [Google Scholar]
- Fabes RA, Poulin RE, Eisenberg N, & Madden-Derdich DA (2002). The Coping with Children’s Negative Emotions Scale (CCNES): Psychometric properties and relations with children’s emotional competence. Marriage & Family Review, 34, 285–310. 10.1300/J002v34n03_05 [DOI] [Google Scholar]
- Fivush R, Brotman MA, Buckner JP, & Goodman SH (2000). Gender differences in parent–child emotion narratives. Sex Roles, 42, 233–253. 10.1023/A:1007091207068 [DOI] [Google Scholar]
- Forgatch MS, & Patterson GR (2010). Parent Management Training—Oregon Model: An intervention for antisocial behavior in children and adolescents In Weisz JR & Kazdin AE (Eds.), Evidence-based psychotherapies for children and adolescents (pp. 159–177). New York: Guilford Press. [Google Scholar]
- Friedlmeier W, Corapci F, & Cole PM (2011). Emotion socialization in cross‐cultural perspective. Social and Personality Psychology Compass, 5, 410–427. 10.1111/j.1751-9004.2011.00362.x [DOI] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, … & Beckham JC (2015). The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans: A meta-analysis. Journal of Anxiety Disorders, 31, 98–107. 10.1016/j.janxdis.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, DeGarmo DS, & Zamir O (2016). Effects of a military parenting program on parental distress and suicide ideation: After Deployment Adaptive Parenting Tools. Suicide and Life Threatening Behavior, 46, S23–S31. 10.1111/sltb.12255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, DeGarmo DS, & Zamir O (2018a). After Deployment, Adaptive Parenting Tools: 1-year outcomes of an evidence-based par- enting program for military families following deployment. Prevention Science, 19, 589–599. 10.1007/s11121-017-0839-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, DeGarmo DS, & Zamir O (2018b). Testing a military family stress model. Family Process, 57, 415–431. 10.1111/famp.12282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, Pinna KLM, Hanson S, Brockberg D (2014). Promoting parenting to support reintegrating military families: After Deployment, Adaptive Parenting Tools. Psychological Services, 11, 31–40. 10.1037/a0034134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, & Youssef AM (2016). Parenting and children’s resilience in military families: A twenty-first century perspective In MacDermid Wadsworth S (Ed.), Parenting and children’s resilience in military families (pp. 1–9). New York, NY: Springer. [Google Scholar]
- Gottman JM, Katz LF, & Hooven C (1996). Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology, 10, 243–268. 10.1037/0893-3200.10.3.243 [DOI] [Google Scholar]
- Graham JW (2003). Adding missing-data-relevant variables to FIML-based structural equation models. Structural Equation Modeling, 10, 80–100. doi: 10.1207/S15328007SEM1001_4 [DOI] [Google Scholar]
- Grusec JE (2011). Socialization processes in the family: Social and emotional development. Annual Review of Psychology, 62, 243–269. 10.1146/annurev.psych.121208.131650 [DOI] [PubMed] [Google Scholar]
- Gunzenhauser C, Fäsche A, Friedlmeier W, & von Suchodoletz A (2014). Face it or hide it: Parental socialization of reappraisal and response suppression. Frontiers in psychology, 4, 1–14. 10.3389/fpsyg.2013.00992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havighurst S (2003). Improving Children’s Emotional Competence: Parenting Interventions In Denham SA & Burton R (Eds.), Social and emotional prevention and intervention programming for preschoolers. Boston, MA: Springer. [Google Scholar]
- Havighurst SS, Wilson KR, Harley AE, Prior MR, & Kehoe C (2010). Tuning in to Kids: Improving emotion socialization practices in parents of preschool children–findings from a community trial. Journal of Child Psychology and Psychiatry, 51, 1342–1350. 10.1111/j.1469-7610.2010.02303.x [DOI] [PubMed] [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, & Strosahl K (1996). Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64, 1152–1168. 10.1037/0022-006X.64.6.1152 [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, & Koffman RL (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351, 13–22. 10.1056/NEJMoa040603 [DOI] [PubMed] [Google Scholar]
- Hurrell KE, Hudson JL, & Schniering CA (2015). Parental reactions to children’s negative emotions: Relationships with emotion regulation in children with an anxiety disorder. Journal of anxiety disorders, 29, 72–82. 10.1016/j.janxdis.2014.10.008 [DOI] [PubMed] [Google Scholar]
- Lorber W, & Garcia HA (2010). Not supposed to feel this: traditional masculinity in psychotherapy with male veterans returning from Afghanistan and Iraq. Psychotherapy: Theory, Research, Practice, Training, 47, 296–305. 10.1037/a0021161 [DOI] [PubMed] [Google Scholar]
- Manini B, Cardone D, Ebisch SJ, Bafunno D, Aureli T, & Merla A (2013). Mom feels what her child feels: Thermal signatures of vicarious autonomic response while watching children in a stressful situation. Frontiers in Human Neuroscience, 7, 1–10. 10.3389/fnhum.2013.00299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald RP, & Ho MHR (2002). Principles and practice in reporting structural equation analyses. Psychological Methods, 7, 64–82. 10.1037/1082-989X.7.1.64 [DOI] [PubMed] [Google Scholar]
- McElwain NL, Halberstadt AG, & Volling BL (2007). Mother‐and father‐reported reactions to children’s negative emotions: Relations to young children’s emotional understanding and friendship quality. Child Development, 78, 1407–1425. 10.1111/j.1467-8624.2007.01074.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, Forgatch MS, & DeGarmo DS (2010). Cascading effects following intervention. Development and Psychopathology, 22, 949–970. 10.1017/S0954579410000568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piehler TF, Ausherbauer K, Gewirtz A, & Gliske K (2018). Improving child peer adjustment in military families through parent training: The mediational role of parental locus of control. The Journal of early adolescence, 38, 1322–1343. 10.1177/0272431616678990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pincus SH, House R, Christenson J, & Adler LE (2001). The emotional cycle of deployment: A military family perspective. US Army Medical Department Journal, 4(5), 6 Retrieved from http://www.hooah4health.com/deployment/familymatters/emotionalcycle2.htm [Google Scholar]
- Pinna KLM, Hanson S, Zhang N, & Gewirtz AH (2017). Fostering resilience in National Guard and Reserve families: A contextual adaptation of an evidence-based parenting program. American Journal of Orthopsychiatry, 87, 185–193. 10.1037/ort0000221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacker RE and Lomax RG (2010). A beginner’s guide to structural equation modeling (3rd ed.). New York, NY: Routledge Academic. [Google Scholar]
- Snyder J, Gewirtz AH, Zamir O, Gird S, Elish K, Quattlebaum J, … Pauline M (2018). Effects of the After Deployment: Adaptive Parenting Tools (ADAPT) Intervention on distress avoidance and parenting behavior of male military service members deployed to middle east conflicts. Manuscript in preparation. [Google Scholar]
- Snyder J, Low S, Bullard L, Schrepferman L, Wachlarowicz M, Marvin C, & Reed A (2013). Effective parenting practices: Social interaction learning theory and the role of emotion coaching and mindfulness In Larzelere RE, Morris AS, & Harrist AW (Eds.), Authoritative parenting: Synthesizing nurturance and discipline for optimal child development (pp. 189–210). Washington, DC, US: American Psychological Association. [Google Scholar]
- Stolz HE, Barber BK, & Olsen JA (2005). Toward disentangling fathering and mothering: An assessment of relative importance. Journal of Marriage and Family, 67, 1076–1092. 10.1111/j.1741-3737.2005.00195.x [DOI] [Google Scholar]
- Tiwari S, Podell JC, Martin ED, Mychailyszyn MP, Furr JM, & Kendall PC (2008). Experiential avoidance in the parenting of anxious youth: Theory, research, and future directions. Cognition and Emotion, 22, 480–496. 10.1080/02699930801886599 [DOI] [Google Scholar]
- Tull MT, Gratz KL, Salters K, & Roemer L (2004). The role of experiential avoidance in posttraumatic stress symptoms and symptoms of depression, anxiety, and somatization. The Journal of Nervous and Mental Disease, 192, 754–761. 10.1097/01.nmd.0000144694.30121.89 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Defense. (2014). Demographics 2014: Profile of the military community. Retrieved from http://www.militaryonesource.mil/12038/MOS/Reports/2014-Demographics-Report.pdf
- Wadsworth SM, Bailey KM, & Coppola EC (2017). US military children and the wartime deployments of family members. Child Development Perspectives, 11, 23–28. 10.1111/cdep.12210 [DOI] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, & Keane TM (1993, October). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- Wilkins KC, Lang AJ, & Norman SB (2011). Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and anxiety, 28, 596–606. 10.1002/da.20837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MS, McElwain NL, & Halberstadt AG (2009). Parent, family, and child characteristics: Associations with mother-and father-reported emotion socialization practices. Journal of Family Psychology, 23, 452–463. 10.1037/a0015552 [DOI] [PubMed] [Google Scholar]
- Zhang N, Rudi JH, Zamir O, & Gewirtz AH (2017). Parent engagement in online mindfulness exercises within a parent training program for post-deployed military families. Mindfulness, 9, 725–736. 10.1007/s12671-017-0810-2 [DOI] [PMC free article] [PubMed] [Google Scholar]