Abstract
Understanding the impact of evidence-based practice toward the rehabilitation of patients with knee osteoarthritis (PKOA) is possible with appropriate outcome measures. There is a definite need to summarize the available outcomes with reference to knee OA. This review summarizes the available outcome measures used in the diagnosis, prognosis, and rehabilitation of PKOA. Electronic searches of PubMed, Medline, CINAHL, PsycINFO, Google Scholar, and EBSCO were conducted using terms relating to outcome measures used in the diagnosis, prognosis, and rehabilitation of PKOA. Papers examining the relationship between psychosocial factors and pain and disability outcomes following physiotherapy were included. Two reviewers selected, appraised and extracted studies independently. The searched papers were classified under three classifications, radiological, arthroscopic, and functional knee OA outcome measures. 26 outcome measures used in the diagnosis, prognosis, and rehabilitation of PKOA were identified. Nine outcome measures were included under radiological, four under arthroscopic and remaining 13 under functional classification. Oxford knee score and WOMAC have excellent reliability and good validity among them. In developing countries, still, we use the scales validated and available from the developed countries. This will not reflect the actual treatment effect among PKOA. This review will assist in educating orthopedician, physiotherapist, academician, and researchers on the available in the diagnosis, prognosis, and rehabilitation of PKOA. This review highlight the need for patient-reported outcome measures from the developing countries to document actual treatment effect.
Keywords: Developing countries, knee, osteoarthritis, pain, radiography
Introduction
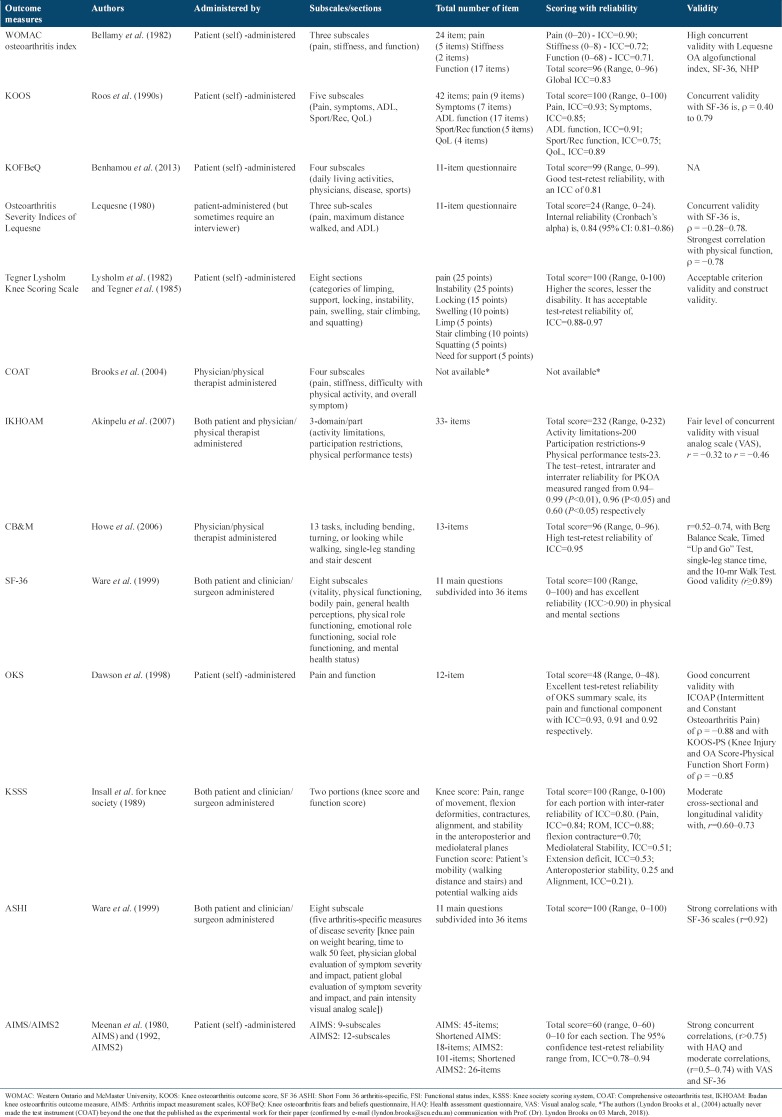
Among the world diseases, osteoarthritis (OA) ranked fourth for the contributing factor of disability.[1] OA is chronic, slowly progressive, degenerative disease of joint which affects articular cartilage and accompanied by pain, swelling, and loss of function.[2,3] OA affects various joints such as knee, hip, ankle, wrist, cervical, and lumbar. Out of 291 conditions globally, the 11th highest contributor to global disability is hip and knee OA.[4] 22%–39% of 1.252 billion population suffer from OA in India. Hip and knee OA is the most prevalent forms of OA with the overall prevalence of knee OA is 28.7%.[5] Among them, common is knee joint affecting one in two people over 85 years of age.[6] In India, many health-care professionals treat patients with various stages of OA. However, surprisingly many of them fails to use suitable scale or outcome measure to document their gained benefits. The health care professionals should be made aware about the importance of using proper scales for documenting patient progression. Measuring results of treatment in clinical setting has been an age long practice. The outcome measure in clinical practice provides the mechanism by which the health care provider, the patient, the public, and the payer are able to assess the end results of care and its effect upon the health of the patient and society. The measurement of clinical outcomes in the health care delivery system is mandatory in clinical decision making. We can classify the scale which is used in the PKOA under three categories namely, radiological, arthroscopic and functional, Figure 1.
Figure 1.
Classification of knee osteoarthritis scales
Abbreviations: K and L: Kellgren and Lawrence; IKDC: International knee documentation committee; OARSIJSN: Osteoarthritis Research Society International Joint Space Narrowing; WORMS: Whole-Organ Magnetic Resonance Imaging Score; UGSSPKOA: Ultrasonographic Grading Scale for Severity of Primary Knee Osteoarthritis; SFA: French Society of Arthroscopy; WOMAC: Western Ontario and McMaster University; KOOS: Knee Osteoarthritis Outcome Score; SF 36 ASHI: Short Form 36 Arthritis Specific; FSI: Functional Status Index; KSSS: Knee Society Scoring System; LEQUESNE: Osteoarthritis Severity Indices of Lequesne; COAT: Comprehensive osteoarthritis test; IKHOAM: Ibadan Knee Osteoarthritis Outcome Measure; CBM: Community Balance and Mobility Scale; AIMS: Arthritis Impact Measurement Scales; KOFBeQ: Knee Osteoarthritis Fears and Beliefs Questionnaire; and MOS SF-36: Medical Outcomes Study Questionnaire Short Form 36 Health Survey
Information Source
The articles are searched academic databases from inception to February 23, 2018. In addition, the reference sections of the extracted articles were manually searched for any articles missed by the electronic search. Academic databases, including PubMed, Medline, CINAHL, PsycINFO, and EBSCO, were used to extract relevant studies. The primary author conducted the electronic search using the keywords encompassed within five primary key terms: “knee,” “OA,” “outcome,” “physiotherapy,” “exercise,” and “India.” These keywords were combined using the Boolean operators “AND,” “OR,” and “NOT.”
Radiological Classification
Radiological classification OA scales being the pioneer of all OA scales, which are used in diagnosis.
Kellgren and Lawrence classification system
Kellgren and Lawrence system proposed in 1957 and accepted by the WHO in 1961, grades the severity of knee OA.[7] They classified the radiographic grading of OA under five-point ordinal scale. They are, Grade 0 - no radiographic findings of OA knee joint; Grade I - minute osteophytes of doubtful clinical significance and possible osteophytic lipping; Grade II - definite osteophytes with unimpaired joint space; Grade III - definite osteophytes with moderate joint space narrowing (JSN) and possible bony deformity; and Grade IV - definite large osteophytes with severe JSN, subchondral sclerosis, and definite bony deformity. They demonstrate a wide range of interobserver reliability (0.51–0.89).[8]
Ahlbäck classification of OA of the knee joint
In 1968, Ahlbäck et al. proposed the classification system for radiological grading of OA of the knee joint. According to them, there were six grades, Grade 0 - no radiographic findings of OA; Grade I - JSN <3 mm; Grade II - joint space obliteration; Grade III - minor bone attrition <5 mm; Grade IV - moderate bone attrition (5–15 mm); and Grade V - severe bone attrition (>15 mm). Ahlback system has poor interobserver reliability (0.11–0.23)[9] because it gives more importance to the bone loss and it becomes difficult to extrapolate among the individual in their early stages of OA.
International knee documentation committee IKDC
IKDC was formed in 1987, to identify and document the prognosis or deterioration in symptoms, function, and sports activities due to knee impairment. Originally, it was designed for the individual with an injury to the knee ligament. Later other knee impairments such as articular cartilage lesions, patellofemoral pain, ligament injuries, and meniscal injuries were described by them. They classified OA into four ordinal scale grading being, Grade A - No JSN; Grade B - joint space >4 mm with the presence of small osteophytes, slight sclerosis, or femoral condyle flattening; Grade C - joint space between 2 and 4 mm; and Grade D - joint space <2 mm. The IKDC system, which incorporates JSN is more informative had good reliability (0.6–0.8) and superior to all other classification system.[10]
OA research society international (OARSI) JSN grading system
OARSI JSN[11] grading system describes the severity of OA knee joint on four-point ordinal scale based on the percentage of JSN. They are, Grade I - normal (0% JSN); Grade II - mild (1–33% JSN); Grade III - moderate (34–66% JSN) and the last being, and Grade IV - severe (67–100% JSN).
Whole-organ magnetic resonance imaging
Whole-organ magnetic resonance imaging score (WORMS), semi-quantitative scoring system published by Peterfy et al., in 2004. It examines the five features related to the articular surfaces. They are marginal osteophytes (eight-point scale, based on size and the extent of bone spur margin involvement), subarticular bone attrition (four-point scale, based degree of flattening or depression), cartilage signal and morphology (eight-point scale), subarticular bone marrow abnormality (three-point scale, based on the extent of regional marrow involvement), and subarticular cysts (three-point scale, based on focal bone loss).[12] The final WORMS scores are calculated as cumulative surface feature (osteophytes, bone attrition, cartilage, marrow abnormality, and subarticular cysts) scores in each compartments, patellofemoral joint (PFJ), the medial femorotibial joint, and the lateral femorotibial joint of knee joint. It has excellent interrater reliability (Intraclass Correlation Coefficient (ICC) >0.9, P < 0.01) in all the five features except bone attrition feature (ICC = 0.61, P < 0.01 [MTFJ], ICC = 0.78, P < 0.01 (PFJ)].[12]
Ultrasonographic grading scale for severity of primary knee OA
Ultrasonographic grading scale for severity of primary knee OA was proposed by Mortada et al., in 2016.[13] They graded the knee of PKOA into five grades (0–4) depended on the shape of distal femoral osteophytes. In which, Grade 0 being no osteophytes and Grade 4 has osteophytes which are superior and parallel to femoral bone with or without an inferior part in the joint space. Grade 4 is the advanced grade of KOA while Grade 0 means no OA. The interreader and intrareader reliability is good with kappa > 0.81, P ≤ 0.001.
Brandt radiographic grading scale
Brandt radiographic grading scale of OA of the knee joint classifies the severity based on five-point ordinal scale. According to them, Grade 0 - no radiographic findings of OA; Grade I - < 25% JSN with secondary features; Grade II - 50–75% JSN without secondary features; Grade III - 50–75% JSN with secondary features, and Grade IV - > 75% JSN with secondary features. The secondary features are subchondral sclerosis, osteophyte formation, and subchondral cysts. This system is also based on JSN and demonstrated moderate interobserver reliability.
Fairbank classification of OA
Fairbank classified OA into five grades. They are, Grade 0 - normal; Grade I - squaring of tibial margin; Grade II - flattening of femoral condyle, squaring and sclerosis of tibial margin; Grade III - JSN, hypertrophic changes, or both, and Grade IV - 75% JSN with the secondary feature.
Jager-Wirth classification system
Similarly, Jager-Wirth used five-point ordinal scale to classify the severity of knee OA. According to them, Grade 0 - no arthrosis; Grade I - initial arthrosis, small osteophytes, and minimal JSN; Grade II - moderate arthrosis, approximately 50% JSN; Grade III - medium-grade arthrosis and the last is, and Grade IV - heavy arthrosis. To the best of author knowledge, no reliability studies are available for Fairbank and Jager-Wirth classification system.
Arthroscopy Classification
Arthroscopic classification provides detailed chondropathy such as depth consistency, size, and location of lesion of the knee joint. Arthroscopy classification includes three scales, Outerbridge,[14,15] Modified Outerbridge,[16] and French society of arthroscopy (FSA)[17] and a modified Collins classification.[18] These scales grade OA knee based on cartilage lesions.
Outerbridge arthroscopy classification
Based on patellar chondral lesions, in 1961 Outerbridge classified into four grades, Grade I - softening; Grade II - fragmentation/fissure of 1.25 cm or less; Grade III - fragmentation/fissure >1.25 cm; and Grade IV - bone erosion.
Modified Outerbridge arthroscopy classification
Modified Outerbridge classification grade the knee OA into five grades based on cartilage lesion, namely Grade 0 - normal articular cartilage, Grade I - articular cartilage softens, Grade II - superficial fissures and fibrillation appears over the cartilage, Grade III - deep fissures appears over the cartilage without exposing bone, and Grade IV - bone gets exposed.
FSA classification
In 1994 another grading system of classification was proposed by the FSA for grading chondropathy. They are Grade I - softening; Grade II - superficial fissure; Grade III - deep fissure; and Grade IV - bone exposure.
Collins classification
Based on cartilage destruction, Collins classified into four grades, Grade I - destruction of superficial cartilage; Grade II - more extensive cartilage destruction; Grade III - loss of cartilage in one or more pressure areas; and Grade IV - complete cartilage loss.
The intraobserver kappa (k) index of Outerbridge, FSA, and Collins were 0.29, 0.61, and 0.42, respectively, while interobserver kappa (k) index was 0.47, 0.49, and 0.45.[19,20] FSA classification system was moderately accurate in grading arthroscopic lesion when compared to other system.[20]
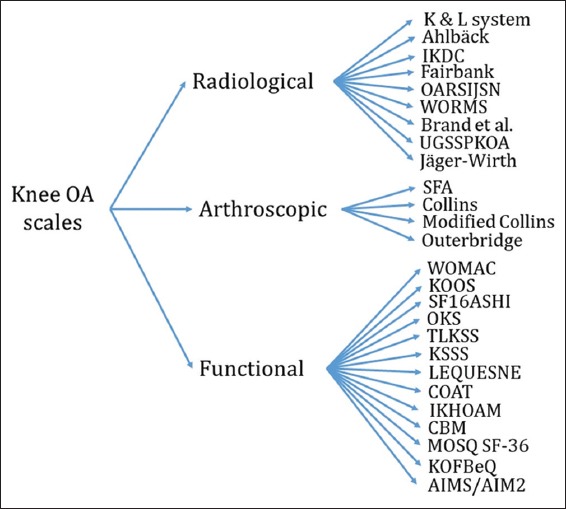
Functional Classification
The scales under functional classification are used to document the functional benefit among PKOA is tabulated in Table 1.
Table 1.
Functional classification of outcome measures used in the rehabilitation of PKOA
Western Ontario and Mcmaster university (WOMAC) OA index
WOMAC OA index was developed by Bellamy et al.[21] in 1982 for assessing their activities of daily living (ADL), functional mobility, gait, general health and quality of life (QoL) in PKOA and validated in 1988. It has total 24 items and three subscales, namely pain (5 items), stiffness (2 items), and function (17 items), scored on five-point ordinal scale, 0 - none, 1 - mild, 2 - moderate, 3 - severe, and 4 - extremely severe. Higher WOMAC scores indicate worse pain, stiffness, and functional limitations. The test-retest reliability for pain, stiffness, and function is ICC = 0.74, 0.58, and 0.92, respectively.[22] It would take approximately 12 min to complete the whole WOMAC directly or indirectly over telephone or online.
Knee injury and OA outcome score (KOOS)
KOOS was developed by Roos et al., in the 1990s, as a patient self-reported opinion regarding their knee and associated problems.[23] It is an extension of WOMAC OA index. It has 42 items and scored under five subscales, namely pain, other symptoms, ADL, function in sport and recreation (Sport/Rec), and knee-related QoL. It has the acceptable reliability of ICC >0.8 in all subscales, except ADL in sport and recreation having ICCs between 0.45 and 0.65. The main intention for the development of KOOS is to document the clinical changes following knee injuries such as knee ligament injury, meniscal tears, knee cartilage lesions, osteochondritis dissecans, and knee OA that can result in posttraumatic knee OA or secondary knee OA.
Knee OA fears and beliefs questionnaire
Knee OA fears and beliefs questionnaire (KOFBeQ) was developed by Benhamou et al., in 2013, for assessing the unrealistic fears and beliefs of PKOA.[24] It has four subscales, namely daily living activities (3 items), physicians (4 items), disease 9 (2 items), and sports (2 items), totaling 11 items and scored in 10-point numeric scale (0–9). It helps in identifying the potential barriers to treatment adherence and planning better management. Test-retest reliability of KOFBeQ was good with an ICC of 0.81 (95% confidence interval [CI] 0.64–0.90).[24]
OA severity indices of lequesne
The OA severity indices of lequesne, algofunctional index for OA knee is devised by rheumatologists, Lequesne in late 1980 and validated in 1981 to assess the severity for OA of knee and hip in an elderly population.[25,26] It is an 11-item questionnaire of subjective nature used as a part of interview to obtain information from patients, about their diseased hip. Patients’ responses with references to pain, maximum distance walked and ADL are recorded to generate a single composite scale.[25]
Tegner lysholm knee scoring scale (TLKSS)
TLKSS was initially published as a physician-administered score in 1982 to document the functional outcome of knee ligament surgery. But later TLKSS was extended to measure the patient with, meniscal tears, patellofemoral pain, traumatic knee dislocation, knee cartilage lesions, osteochondritis dissecans, patellar instability, and knee OA. 3 years later, the Tegner activity scale was published by the addition of work and sport activities. Now, TLKSS is validated as patient-administered scores for the responsiveness after the treatment of anterior cruciate ligament tears. The total score is 100 (range, 0–100) which is scored under eight sections; pain (25 points), instability (25 points), locking (15 points), swelling (10 points), limp (5 points), stair climbing (10 points), squatting (5 points), and need for support (5 points). It has the acceptable test-retest reliability of, ICC = 0.88–0.97.
Comprehensive OA test (COAT)
COAT is a simple index to measure the severity of symptom among the patients with hip and knee OA.[27] COAT was constructed to assess the three main components of OA, pain, stiffness, and physical dysfunction both WOMAC and COAT are highly reliable (WOMAC alpha = 0.98; COAT alpha = 0.97) when measured over weeks among the patient with hip and knee OA. However, this scale was developed beyond its infancy.
Ibadan knee OA outcome measure (IKHOAM)
IKHOAM, measures both self/patient- and clinician/observer-measured items among PKOA, was developed by Akinpelu et al., in 2007.[28] It has three domain, activity limitations, participation restrictions, and physical performance test.[29] Activity limitations domain composed of 25 ADL items that are being performed by PKOA. The degree of difficulty and assistance required in carrying out the activities are rated on a 5 point (0–4) ordinal scale. Second, participation restriction domain has three restricted activities in societal participation due to knee/hip OA. The activities restrictions experienced in carrying out the activities are rated on a 4 point (0–3) ordinal scale. Third, physical performance tests domain which includes five tests that are rated by the clinician. These tests are; (1) 250m walk test rated on a 6 point (0–5) ordinal scale, (2) one leg stance test rated on a 6 point (0–5) ordinal scale, (3) stairs climbing test rated on a 5 point (0–4) ordinal scale, (4) squat test rated on a 5 point (0–4) ordinal scale, and (5) balance test rated on a 6 point (0–5) ordinal scale. The maximum obtainable score on IKHOAM is 232 (200+9+23).[29] The minimal clinically important difference for IKHOAM among PKOA (23 males and 101 females) aged 59.2 ± 11.5 years was 12.8. The score for PKOA was calculated in percentage as individual’s score/total possible score × 100. The test-retest, intrarater, and interrater reliability for PKOA measured ranged from 0.94 to 0.99 (P < 0.01), 0.96 (P < 0.05), and 0.60 (P < 0.05), respectively.[29] It takes about 15 min to complete the test.
Community balance and mobility scale (CB and M)
The CB and M was developed by Howe et al., in 2006, to assess functional deficits in both dynamic balance and mobility at their community level.[30] The scale was originally designed to assess advanced balance and mobility activities such as rapid direction changes and dual tasking in young patients after traumatic brain injury.[30] The CB and M comprises 13 tasks includes, unilateral stance (R and L), tandem walk, 180° tandem pivot, lateral foot scooting (R and L), hopping forward (R and L), crouch and walk, lateral dodging, walking and looking (R and L; over an 8-m distance), running with controlled stop, forward to backward walking, walk (over an 8-m distance), look and carry (R and L), and descending stairs and step-ups (R and L; performance of 5 step-ups onto a stair).[31] The maximum score is 96, with a minimum score of 0. It has concurrent validity of 0.52, 0.74, 0.71, 0.61, and 0.69 with Berg Balance Scale, Timed up and go test, single-leg stance, self-selected gait speed, and fast gait speed, respectively. It has excellent test-retest reliability ICC = 0.95 (95% CI = 0.70–0.99), SEM = 3 (95% CI = 2.68–4.67) with 95% minimal detectable change value is 10.[31]
QoL in PKOA
QoL in PKOA (QoL-PKOA) can be assessed with medical outcomes study questionnaire short form 36 health survey (MOS SF-36) was developed by Ware et al., in 1992.[32] It estimates overall health status under eight sections; vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning, and mental health status. The total score is 100 (range, 0–100) with higher scores lesser disability.[32,33]
Oxford knee score (OKS)
The OKS was developed by Dawson et al., to document patients perceptions on replacement surgeries, in 1996 for hip and 1998 for knee.[34,35] It is a 12-item knee joint-specific patient-reported outcome measures for the assessment of function and pain in PKOA.[35] The OKS has proven to be valid, reliable, and responsive to document clinical changes following intervention to knee. Recommended revised scoring system scores each item in 5-point ordinal scale, 0 (worst) to 4 (best) and with summed up total score range from, 0 to 48.[36] Minimum detectable change and minimal clinical important change for OKS are 5 and 9 points, respectively.[37] The 12-item questionnaire has been used in several clinical studies and translated into various languages with cross-cultural adaptation.
Knee society scoring system (KSSS)
The KSSS is a simple, but objective scoring system developed by Insall et al.[38] for knee society to document the knee and patient’s functional abilities such as walking and stair climbing before and after TKA due to OA knee. It has two portions, first being, clinician/surgeon-rated portion (Knee Score) of KSS, which covers pain, range of movement, flexion deformities, contractures, alignment, and stability in the anteroposterior, and mediolateral planes. Second, patient-reported portion (Function Score) of KSS which covers the patient’s mobility (walking distance and stairs) and potential walking aids in PKOA before and after TKA.[39,40] The total score of each portion, knee score and function score range from 0 to 100 points with higher scores indicating a better outcome.
SF-36 arthritis-specific health index (ASHI)
The SF-36 ASHI, published in 1999 was developed by John E Ware for studying the changes in clinical severity of knee OA and rheumatoid arthritis.[41] It measures the impact of knee OA/rheumatoid arthritis on, bodily pain, physical role, physical functioning, social functioning, vitality, and clinical measures such as 50ft walk test.
Arthritis impact measure (AIM)
AIM was developed by Meenan et al., in 1980, to measure 55 health status items under 9 scale groups. They are mobility (5 status items), physical Activity (5 status items), social Role (7 status items), social activity (9 health status items), pain (5 status items), dexterity (5 status items), activities of daily living (5 status items), anxiety (8 status items), and depression (6 status items).[42] AIM was revised in 1992 and renamed as AIM2 by the addition of three scale groups; arm function, social support, and work. Thus, the original AIM has 55-items while the revised version, AIM2 has 101-items with 95% confidence test-retest reliability range from, ICC = 0.78–0.94.[43]
Discussion
We have summarized the outcome measures used in PKOA and hope; this review would highlight the names of various scales used in PKOA. From Table 1, it was evident that Oxford knee score has excellent test-retest reliability (ICC >0.9) and good concurrent validity with Intermittent and constant OA pain of ρ = −0.88 and with KOOS-physical function short form of ρ = −0.85. WOMAC has excellent reliability with pain subscale (ICC = 0.90) and high concurrent validity with Lequesne OA algofunctional index, SF-36 and NHP. OA Severity Indices of Lequesne has good internal reliability but have fair to strong concurrent validity with SF-36. IKHOAM, KOOS (pain and ADL function) and CB and M have excellent test-retest reliability but non-acceptable level of concurrent validity with criterion measures. Available evidence on the scales used in the diagnosis, prognosis, and rehabilitation of PKOA, confirms that both Oxford knee score and WOMAC have excellent reliability and good validity. All the available scales are from the developed countries, except IKHOAM. We hope, this collection of outcome measure used in the diagnosis, prognosis, and rehabilitation of PKOA would encourage the development of new scales by combining the items of the above in a single scale, CKOI in PKOA to facilitate the patient-centered outcome research. In developing countries like India, still, we use the scales validated and available from the developed countries. This will not reflect the actual treatment effect among PKOA due to cross-cultural variation. None of the scale is available from India. There is real need to develop the outcome measures to be used in diagnosis, prognosis, and rehabilitation of PKOA.
Conclusion
The collection of outcome measure used in the diagnosis, prognosis, and rehabilitation of PKOA is summarized. We hope this review will assist in educating orthopedician, physiotherapist, and academician and researchers on the available in the diagnosis, prognosis, and rehabilitation of PKOA. This review highlights the need for patient-reported outcome measures from the developing countries to document actual treatment effect.
Acknowledgments
The authors are very thanks full to Dr. Vencita Priyanka Aranha, MPT (Pediatrics), Assistant Professor, Maharishi Markandeshwar Institute of Physiotherapy and Rehabilitation, Maharishi Markandeshwar (Deemed-to-be University), Mullana, India, for providing logistic and technical support in editing Figure 1. This review article is a partial fulfillment for the completion of structured Doctorate of Philosophy / Philosophiae Doctor (PhD) programme by the first author Asir John Samuel (Roll No. 20160001 / Regn No. 15-Ph.D-006).
References
- 1.Fransen M, Bridgett L, March L, Hoy D, Penserga E, Brooks P, et al. The epidemiology of osteoarthritis in Asia. Int J Rheum Dis. 2011;14:113–21. doi: 10.1111/j.1756-185X.2011.01608.x. [DOI] [PubMed] [Google Scholar]
- 2.Arthritis-India. [[Last cited on 2017 Jul 27]]. Available from: http://www.arthritis-india.com/osteoarthritis.html .
- 3.What Is Osteoarthritis?Who Gets Osteoarthritis?What Causes Osteoarthritis?How Is Osteoarthritis Diagnosed? 2014. [[Last cited 2017 Jul 27]]. pp. 301–495. Available from: http://www.niams.nih.gov .
- 4.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis:Estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:1323–30. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 5.Pal CP, Singh P, Chaturvedi S, Pruthi KK, Vij A. Epidemiology of knee osteoarthritis in India and related factors. Indian J Orthop. 2016;50:518–22. doi: 10.4103/0019-5413.189608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alarming Osteoarthritis Stats in India. [[Last cited on 2017 Jul 27]]. Available from: http://www.thehansindia.com/posts/index/Health/2016-03-07/Alarming-osteoarthritis-stats-in-India/211848 .
- 7.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scott WW, Jr, Lethbridge-Cejku M, Reichle R, Wigley FM, Tobin JD, Hochberg MC, et al. Reliability of grading scales for individual radiographic features of osteoarthritis of the knee. The Baltimore longitudinal study of aging atlas of knee osteoarthritis. Invest Radiol. 1993;28:497–501. [PubMed] [Google Scholar]
- 9.Galli M, De Santis V, Tafuro L. Reliability of the ahlbäck classification of knee osteoarthritis. Osteoarthritis Cartilage. 2003;11:580–4. doi: 10.1016/s1063-4584(03)00095-5. [DOI] [PubMed] [Google Scholar]
- 10.Wright RW. MARS Group. Osteoarthritis classification scales:Interobserver reliability and arthroscopic correlation. J Bone Joint Surg Am. 2014;96:1145–51. doi: 10.2106/JBJS.M.00929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15(Suppl A):A1–56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 12.Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, et al. Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12:177–90. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Mortada M, Zeid A, Al-Toukhy MA, Ezzeldin N, Elgawish M. Reliability of a proposed ultrasonographic grading scale for severity of primary knee osteoarthritis. Clin Med Insights Arthritis Musculoskelet Disord. 2016;9:161–6. doi: 10.4137/CMAMD.S38141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–7. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 15.Outerbridge Classification, Collins Classification, SFA Classification. Orthopaedic Surgery. [[Last cited on 2017 Oct 02]]. Available from: http://www.orthofracs.com/general/osteoarthritis/oa-grading.html .
- 16.Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG, et al. Cartilage injuries:A review of 31,516 knee arthroscopies. Arthroscopy. 1997;13:456–60. doi: 10.1016/s0749-8063(97)90124-9. [DOI] [PubMed] [Google Scholar]
- 17.Dougados M, Ayral X, Listrat V, Gueguen A, Bahuaud J, Beaufils P, et al. The SFA system for assessing articular cartilage lesions at arthroscopy of the knee. Arthroscopy. 1994;10:69–77. doi: 10.1016/s0749-8063(05)80295-6. [DOI] [PubMed] [Google Scholar]
- 18.Collins D. The Pathology of Articular and Spinal Diseases. London: Edward Arnold Co; 1949. [Google Scholar]
- 19.Brismar BH, Wredmark T, Movin T, Leandersson J, Svensson O. Observer reliability in the arthroscopic classification of osteoarthritis of the knee. J Bone Joint Surg Br. 2002;84:42–7. doi: 10.1302/0301-620x.84b1.11660. [DOI] [PubMed] [Google Scholar]
- 20.Lasmar NP, Lasmar RC, Vieira RB, de Oliveira JR, Scarpa AC. Assessment of the reproducibility of the outerbridge and FSA classifications for chondral lesions of the knee. Rev Bras Ortop. 2011;46:266–9. doi: 10.1016/S2255-4971(15)30193-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC:A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]
- 22.Roos EM, Klässbo M, Lohmander LS. WOMAC osteoarthritis index. Reliability, validity, and responsiveness in patients with arthroscopically assessed osteoarthritis. Western Ontario and macMaster universities. Scand J Rheumatol. 1999;28:210–5. doi: 10.1080/03009749950155562. [DOI] [PubMed] [Google Scholar]
- 23.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and osteoarthritis outcome score (KOOS) –development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 24.Benhamou M, Baron G, Dalichampt M, Boutron I, Alami S, Rannou F, et al. Development and validation of a questionnaire assessing fears and beliefs of patients with knee osteoarthritis:The knee osteoarthritis fears and beliefs questionnaire (KOFBeQ) PLoS One. 2013;8:e53886. doi: 10.1371/journal.pone.0053886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lequesne MG, Mery C, Samson M, Gerard P. Indexes of severity for osteoarthritis of the hip and knee. Validation –value in comparison with other assessment tests. Scand J Rheumatol Suppl. 1987;65:85–9. doi: 10.3109/03009748709102182. [DOI] [PubMed] [Google Scholar]
- 26.Lequesne MG. The algofunctional indices for hip and knee osteoarthritis. J Rheumatol. 1997;24:779–81. [PubMed] [Google Scholar]
- 27.Brooks LO, Rolfe MI, Cheras PA, Myers SP. The comprehensive osteoarthritis test:A simple index for measurement of treatment effects in clinical trials. J Rheumatol. 2004;31:1180–6. [PubMed] [Google Scholar]
- 28.Akinpelu AO, Odole AC, Adegoke BOA, Adeyini AF. Development and initial validation of the Ibadan knee/hip osteoarthritis outcome measure. S Afr J Physiother. 2007;63:3–8. [Google Scholar]
- 29.Odole AC, Odunaiya NA, Akinpelu AO. Ibadan knee/hip osteoarthritis outcome measure:Process of development. Ann Ib Postgrad Med. 2013;11:71–6. [PMC free article] [PubMed] [Google Scholar]
- 30.Howe JA, Inness EL, Venturini A, Williams JI, Verrier MC. The community balance and mobility scale –a balance measure for individuals with traumatic brain injury. Clin Rehabil. 2006;20:885–95. doi: 10.1177/0269215506072183. [DOI] [PubMed] [Google Scholar]
- 31.Takacs J, Garland SJ, Carpenter MG, Hunt MA. Validity and reliability of the community balance and mobility scale in individuals with knee osteoarthritis. Phys Ther. 2014;94:866–74. doi: 10.2522/ptj.20130385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 33.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item short-form health survey (SF-36):III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–90. [PubMed] [Google Scholar]
- 35.Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80:63–9. doi: 10.1302/0301-620x.80b1.7859. [DOI] [PubMed] [Google Scholar]
- 36.Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, et al. The use of the Oxford hip and knee scores. Bone Jt Surg. 2007;89B:1010–4. doi: 10.1302/0301-620X.89B8.19424. [DOI] [PubMed] [Google Scholar]
- 37.Beard DJ, Harris K, Dawson J, Doll H, Murray DW, Carr AJ, et al. Meaningful changes for the oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol. 2015;68:73–9. doi: 10.1016/j.jclinepi.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop Relat Res. 1989;???:13–4. [PubMed] [Google Scholar]
- 39.Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN, et al. The new knee society knee scoring system. Clin Orthop Relat Res. 2012;470:3–19. doi: 10.1007/s11999-011-2135-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, Lonner JH, et al. Development of a new knee society scoring system. Clin Orthop Relat Res. 2012;470:20–32. doi: 10.1007/s11999-011-2152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ware JE, Jr, Keller SD, Hatoum HT, Kong SX. The SF-36 arthritis-specific health index (ASHI):I. Development and cross-validation of scoring algorithms. Med Care. 1999;37:MS40–50. doi: 10.1097/00005650-199905001-00004. [DOI] [PubMed] [Google Scholar]
- 42.Meenan RF, Gertman PM, Mason JH. Measuring health status in arthritis. The arthritis impact measurement scales. Arthritis Rheum. 1980;23:146–52. doi: 10.1002/art.1780230203. [DOI] [PubMed] [Google Scholar]
- 43.Meenan RF, Mason JH, Anderson JJ, Guccione AA, Kazis LE. AIMS2. The content and properties of a revised and expanded arthritis impact measurement scales health status questionnaire. Arthritis Rheum. 1992;35:1–0. doi: 10.1002/art.1780350102. [DOI] [PubMed] [Google Scholar]