Supplemental Digital Content is available in the text
Keywords: a body shape index, brachial ankle pulse wave velocity, cardio ankle vascular index, carotid intima media thickness, intermediate cardiovascular risk
Abstract
A body shape index (ABSI) has been introduced as a marker of the relationship between body composition and all-cause mortality. However, until now, the relationships between ABSI and vascular structure and function have not been evaluated. The aim of this study was to investigate the association of ABSI with vascular structure and function in Spanish adults with intermediate cardiovascular risk. This cross-sectional study analyzed the data of 2354 subjects [age, 35–74 years (median, 62.0 years [range, 56.0–67.0 years]), 61.9% men] enrolled into the MediAte Risk management (MARK) study. ABSI was calculated by using the following formula: ABSI = waist circumference (m)/[body mass index2/3 × height (m)1/2)]. Vascular function was assessed by measuring cardio-ankle vascular index (CAVI) with the VaSera device and brachial ankle pulse wave velocity (baPWV) by using a validated equation. Vascular structure was assessed by measuring carotid intima-media thickness (IMT) by ultrasonography. Median value of ABSI was 0.083 (range, 0.081–0.090), mean CAVI was (8.5 ± 1.2), and median IMT was 0.727 (range, 0.672–0.799). The values of ABSI and CAVI were higher in men. After adjusting for confounders, ABSI was positively associated with CAVI, baPWV, and average mean IMT. Thus, for each unit increase in ABSI, CAVI increased by 0.16 units, baPWV by 0.25 m/s, and IMT by 0.033 mm. In the logistic regression analysis, the odds ratio of ABSI was > 1 for high CAVI ≥ 9, baPWV ≥ 15 m/s, and IMT ≥ 0.90 mm in the overall subject group, and in the sex- and age-specific (> 62 years, ≤ 62 years) subgroups, after adjusting for confounders. The area under the receiver-operating characteristic curve of the ABSI was 0.631 (95% confidence interval [CI], 0.608–0.654) for CAVI ≥ 9, and 0.617 (95% CI, 0.593–0.641) for high baPWV ≥ 15 m/s. ABSI showed a positive association with vascular structure and function, independent of other confounders that might influence weight and fat mass distribution in Spanish subjects at intermediate cardiovascular risk.
Trial Registration: ClinicalTrials.gov Identifier: NCT01428934 (registered: September 2, 2011; last updated: September 8, 2016)
1. Introduction
Body mass index (BMI) is the most widely used measure to assess the presence of overweight and obesity in adults. An elevated BMI is an important risk factor for cardiovascular disease, diabetes mellitus, skeletal muscle disease, and some cancers in developed countries; moreover, it was found associated with increased all-cause mortality, cardiovascular disease mortality, and cancer mortality.[1] However, BMI has important limitations, as it does not distinguish between lean and fat mass, or between central and peripheral fat.[2] Waist circumference (WC) is a complementary index that assesses central obesity[3,4] and predicts mortality risk better than BMI. However, according to the World Health Organization, WC has certain limitations, mainly related to omission of the height or weight of subjects.[5]
To overcome these limitations, Krakauer and Krakauer[6] proposed in 2012 the A Body Shape Index (ABSI), which uses readily available clinical data (height, weight, and WC), and estimates visceral obesity and overall adiposity. Since then, several studies have shown that ABSI predicts mortality independently of BMI in the US[6] and European populations,[7] as well as in postmenopausal women.[8] Moreover, ABSI was found to be more strongly associated with all-cause mortality, cardiovascular mortality, and cancer mortality than other anthropometric measurements.[6–9] Since its description, several studies have analyzed its relationship with cardiovascular diseases and cardiovascular risk factors.[10–14]
Intima media thickness (IMT) is an independent predictor of the incidence of heart disease, coronary artery disease, and stroke.[15] Brachial ankle pulse wave velocity (baPWV) is an independent predictor of coronary artery disease and mortality in general population[16] and in patients with diabetes mellitus.[17] Cardio-ankle vascular index (CAVI) is associated with carotid and coronary atherosclerosis[18–20] and is a predictor of cardiovascular events in obese patients.[21]
Several studies have shown an association of central obesity (as estimated by WC) and peripheral obesity (as estimated by BMI) with IMT.[17,22–24] However, the relationship between adiposity and arterial stiffness remains controversial. Studies in the general population and in patients with type 2 diabetes mellitus[24–27] have shown conflicting results. The association of ABSI with vascular structure and function measures has not been studied. We have found only 1 recently published study showing an association between ABSI and baPWV in Japanese subjects with type 2 diabetes mellitus.[28]
Therefore, the aim of this study was to investigate the relationship between ABSI and structural (as estimated by IMT) and functional (as estimated by CAVI and baPWV) vascular measures in Spanish adults at intermediate cardiovascular risk.
2. Methods
2.1. Study design
This trial was a cross-sectional study of subjects recruited for the improving interMediAte RisK management (MARK) study (NCT01428934),[29] a longitudinal study designed to assess whether the ankle-brachial index, arterial stiffness (measured by CAVI), postprandial glucose, glycosylated hemoglobin, self-measured blood pressure, and the presence of comorbidities are independently associated with the occurrence of vascular events. It also investigates whether the predictive capacity of current risk equations can be improved in the intermediate risk population. The current study focuses on the data collected at initial visit of patients.
2.2. Study population
In this multicenter study, study population selection was performed by random sampling of individuals that attended general practitioners between July 2011 and June 2013 at 6 health care centers from 3 autonomic communities in Spain and matched the inclusion criteria. Subjects aged 35 to 74 years and with intermediate cardiovascular risk, defined as a 10-year coronary risk ranging from 5% to 15% according to the adapted Framingham risk equation,[30] 10-year vascular mortality risk ranging from 1% to 5% according to the scoring risk in the European equation,[31] or moderate risk according to the European Society of Hypertension guidelines for managing arterial hypertension, were included in the study.[32] Exclusion criteria (Fig. 1) included end-stage disease or institutionalization at the time of the visit, or a history of atherosclerotic disease. This study analyzed the data of 2354 of 2495 subjects included in the MARK study.
Figure 1.
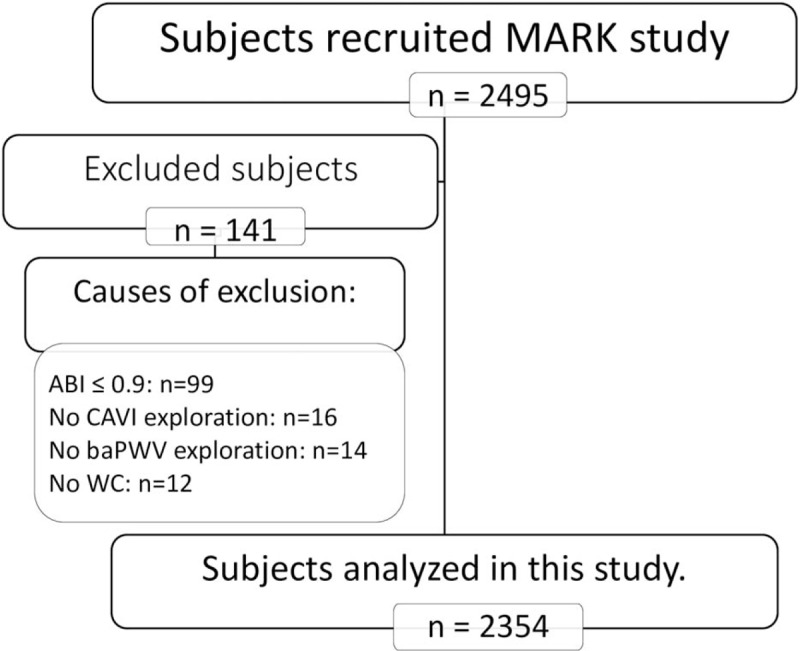
Flow chart of this MARK substudy. N = number, CAVI = cardio-ankle vascular index, baPWV = brachial-ankle pulse wave velocity, ABI = ankle-brachial index, WC = waist circumference.
2.3. Variables and measurement instruments
A detailed description of collection of clinical data and measurement of anthropometric and analytical parameters has been published elsewhere.[29]
2.4. Anthropometric measurements
Body weight was determined twice by using an approved electronic scale (Seca 770, Medical scale and measurement systems, Birmingham, UK) after proper calibration (accuracy ± 0.1 kg). Readings were rounded to 100 g. Height was measured with a stadiometer (Seca 222, Medical scale and measurement systems, Birmingham, UK) and the average of 2 measures was recorded. BMI was calculated as weight (kg) divided by height squared (m2). A BMI > 30 kg/m2 was considered to define obesity.[32] WC was measured according to the 2007 recommendations of the Spanish Society for the Study of Obesity.[33]
ABSI was based on WC adjusted for height and weight using the following formula:[6]
 |
2.5. Office or clinical blood pressure
Office blood pressure measurement involved 3 measurements of the systolic blood pressure (SBP) and diastolic blood pressure (DBP), using the average of the last 2 measurements, by using a validated sphygmomanometer (OMRON M10-IT; Omron Health Care, Kyoto, Japan), according to the recommendations of the European Society of Hypertension.[34] Mean blood pressure (MBP) was calculated using the following formula
 |
2.6. Cardio-ankle vascular index (CAVI) and brachial-ankle pulse wave velocity (baPWV)
CAVI was measured using a VaSera VS-1500 device (Fukuda Denshi Co Ltd, Tokyo, Japan).[35,36] CAVI values were calculated automatically by estimating the stiffness parameter β by the following equation:
where ρ is blood density, Ps and Pd are SBP and DBP in mm Hg, and pulse wave velocity (PWV) is measured between the aortic valve and the ankle.[37] The mean coefficient of variation of the CAVI measurement was < 5%, small enough to allow for clinical use of this index, confirming that CAVI has a good reproducibility.[36]
baPWV was estimated by using the following equation:
where tba was the time interval between the arm and ankle waves).[38]
Measurements were performed with the patient in the supine position after resting for 10 minutes in a quiet room at a stable temperature. The patients should have not smoked or exercised within the hour prior to the test. The average values of CAVI and baPWV (calculated based on the highest and lowest values of these parameters) were considered for the study.
2.7. Carotid intima-media thickness (IMT):
IMT was measured in 448 subjects in the Salamanca cohort, using an ultrasound system (SonoSite Micromaxx; SonoSite Inc, Bothell, WA) with a 5 to 10 MHz high-resolution multifrequency linear transducer. Two researchers, blinded to patients’ clinical data and trained to perform this technique before starting the study, evaluated IMT according to previously published recommendations,[39] using the Sonocalc IMT software (SonoSite Inc, Bothell, WA) that performs automatic IMT measurements to optimize reproducibility. The measurement was performed with the patient supine, with the neck extended and the head slightly turned in the direction opposite to the carotid artery being examined, performing a longitudinal B-mode ultrasound. Measurements were performed on a 10 mm longitudinal section of the common carotid artery at a distance of 1 cm proximally to the bifurcation, performing measurements on the proximal and distal walls, in the lateral, anterior, and posterior projections, along a perpendicular axis of the artery. Sixty measurements were performed on the right carotid and another 60 on the left carotid artery, with 10 measurements in each segment analyzed. The average mean IMT was used, as calculated by the software.
2.8. Definition of cardiovascular risk factors
Patients were considered hypertensive if they were previously diagnosed with hypertension, were receiving antihypertensive drugs, or had blood pressure levels ≥ 140/90 mm Hg. Diabetic patients were those who were previously diagnosed with this disease, were receiving hypoglycemic drugs, or had fasting blood glucose levels ≥ 126 mg/dL or glycosylated hemoglobin level ≥ 6.5%. Dyslipidemia was defined as a prior diagnosis of this condition, use of lipid-lowering drugs, or fasting total cholesterol levels ≥ 250 mg/dL.
2.9. Lifestyle
2.9.1. Tobacco
Smoking history was assessed by asking questions about the participant's smoking status (smoker/nonsmoker). Those patients who were currently smoking or who have stopped smoking within the past year were considered smokers.
Alcohol consumption was assessed through a structured questionnaire and was expressed in grams per week.
2.9.2. Assessment of the diet quality index (DQI)
The diet was evaluated by the diet quality index (DQI),[40] which includes 3 food group categories: daily intake of 1 portion of food in the first food group category was scored as 2; lower and higher intakes were scored as 1 and 3, respectively. Daily consumption of 1 alcoholic drink (1 bottle of beer, 1 glass of wine, or 1 cup of liquor equivalent to approximately 12 g of alcohol) was scored as 3; lower and higher intakes were scored as 1. Consumption of foods from the second food group category considered detrimental was scored as 2, if reported as 4 to 6 times per week; more and less frequent consumption were scored as 1 and 3, respectively. High consumption (4 or more times per week) of food items from the third food group category considered beneficial was scored as 3; intakes of 2 to 3 a week times and less than twice a week were scored as 2 and 1, respectively. All food item scores were summed. The total possible score ranged from 18 to 54.[41]
2.9.3. Physical activity
Leisure time physical activity practice was collected using the Minnesota leisure time physical activity questionnaire that was validated for Spanish men and women.[42,43] The questionnaire was administered by trained interviewers and included detailed information about physical activity during the preceding year, the number of times this activity was performed, and the average duration of each activity on each occasion. Energy consumption in mean metabolic equivalents (METs) was estimated over 14 days by multiplying the METs of physical activity with the duration (in minutes) and cumulative frequency in the month before the interview.
All investigators that evaluated different tests were blinded to the clinical data of patients. All assessments were made within a period of 10 days.
2.10. Statistical analysis
Continuous variables were presented as means ± standard deviation for normally distributed variables or medians (interquartile ranges) for the skewed variables. The statistical normality was tested using the Kolmogorov–Smirnov test. The means of 2 groups were compared using Student t test or Mann–Whitney U test. All categorical variables were presented as numbers and proportions, whereas the χ2 test and Fisher exact test were used for qualitative variables. Rho de Spearman correlation (ρ) coefficients were calculated to evaluate the relationships among the ABSI, WC, and WC measures and CAVI, baPWV, and IMT. Multiple linear regression models were used to analyze the associations of ABSI with CAVI, baPWV, and IMT. The CAVI, baPWV, and IMT were the dependent variables, and ABSI was included as the independent variable. The following 3 models were developed: model 1 was unadjusted, model 2 was adjusted for age (years) and sex (0 = male and 1 = female), and model 3 was adjusted for age (years), sex (0 = male and 1 = female), smoking (0 = No and 1 = Yes), alcohol consumption (g/wk), physical activity (METs/h/wk), diet quality index score (DQI), mean blood pressure, glycosylated hemoglobin level, heart rate and atherogenic index, and the use of antihypertensive drugs (0 = No and 1 = Yes), lipid lowering drugs (0 = No and 1 = Yes), and antidiabetic drugs (0 = No and 1 = Yes). The exception was the analysis of age- and sex-specific subgroups, where age and sex were respectively not included as adjustment variables. To estimate the association of ABSI with the presence of arterial stiffness, 2 logistic regression models were fitted: unadjusted and adjusted for the variables used in the model 3 of the multiple regression analysis. To determine the status of arterial stiffness, the median values of CAVI (≥ 9) and baPWV (≥15 m/s), as well as the average mean IMT ≥ 0.09 mm were used. The analysis was performed with the overall sample, after grouping individuals by sex and age (for age, the median of 62 years was used as a cutoff). To improve the final interpretation, the ABSI was multiplied one hundred-fold. Receiver-operating characteristic (ROC) analyses were performed to examine the diagnostic ability of BMI, WC, and ABSI for CAVI (≥ 9) and baPWV (≥15). The area under the ROC curve (AUROC) and the 95% confidence intervals (CIs) were computed to compare the discriminative power of each anthropometric index. Data were analyzed using SPSS Statistics for Windows, Version 23.0 software (IBM Corp, Armonk, NY). P values < .05 were considered statistically significant.
2.11. Ethics statement
All participants were informed about the objectives and procedures of the study and signed the informed consent form before inclusion. The study was approved by the Clinical Research Ethics Committee of the Primary Care Research Institute Jordi Gol, the Health Care Area of Salamanca and Palma of Mallorca. The study was conducted according to the recommendations of the Declaration of Helsinki .[44] The confidentiality of the information provided by the participants was ensured, complying with the rules established by Spanish Law 15/1999 on the Protection of Personal Data.
3. Results
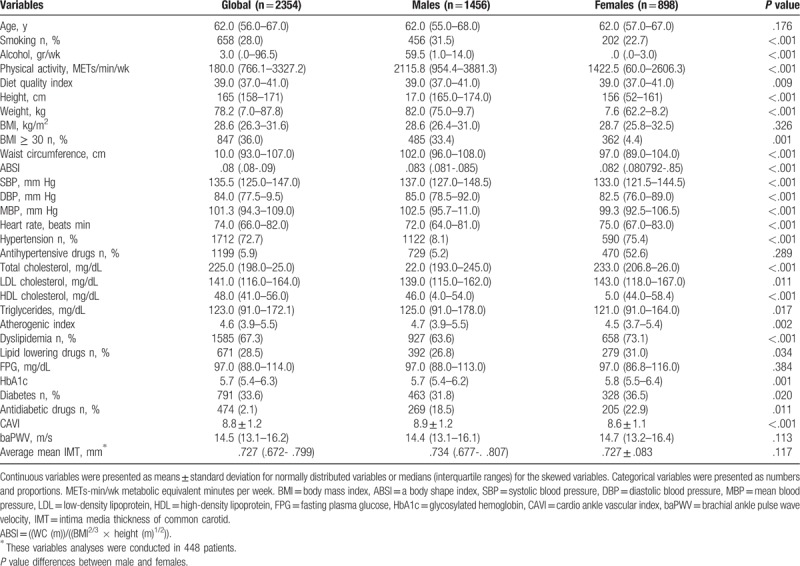
Anthropometric data, clinical characteristics, and vascular structure and function measures of the subjects are presented in Table 1. The median age of the patients was 62.0 (range, 56.0–67.0) years, and 61.9% of them were men. Male patients had a higher percentage of smokers (31.5% vs 22.7%) and hypertension (80.1% vs 75.4%). By contrast, women had a higher prevalence of obesity (40.4% vs 33.4%), dyslipidemia (73.1% vs 63.6%), and diabetes mellitus (36.5% vs 31.8%). The values of overall vascular structure and function measures were 0.727 (range, 0.672– 0.799) (IMT median), 8.81 ± 1.16 (CAVI mean), and 14.5 (range, 13.1–16.2) (baPWV median). ABSI median was 0.083 (range, 0.081–0.090). Male patients had higher values for all variables, except for baPWV and IMT, for which no significant differences were detected.
Table 1.
Characteristics of subjects global and stratified by gender.
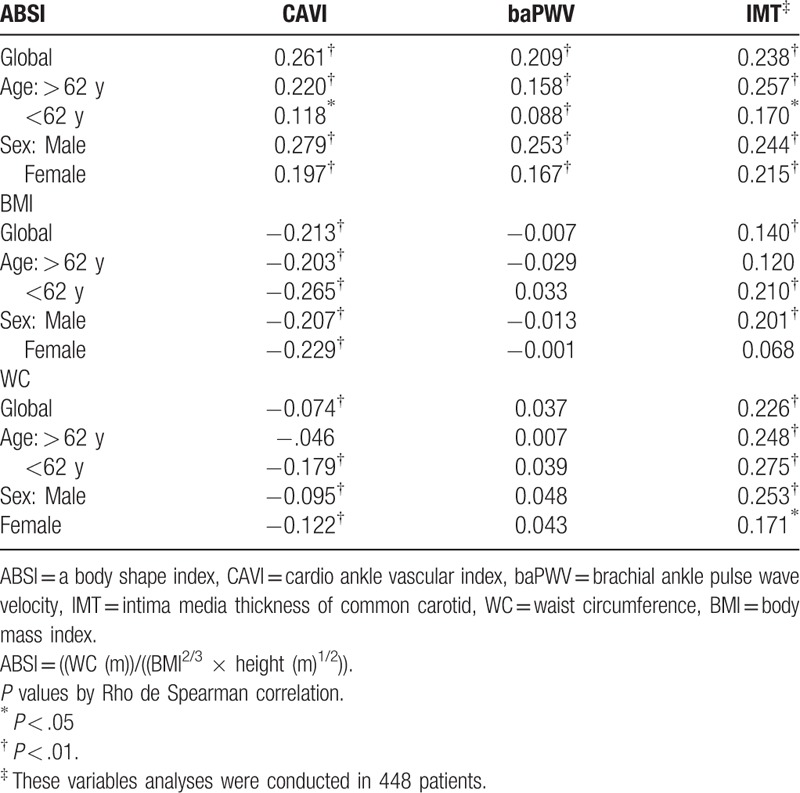
3.1. Correlation coefficients
The Rho de Spearman correlation coefficients of ABSI, WC, and BMI with the vascular structure and function parameters are described in Table 2.
Table 2.
Correlations coefficients between ABSI and vascular function and structure parameters.
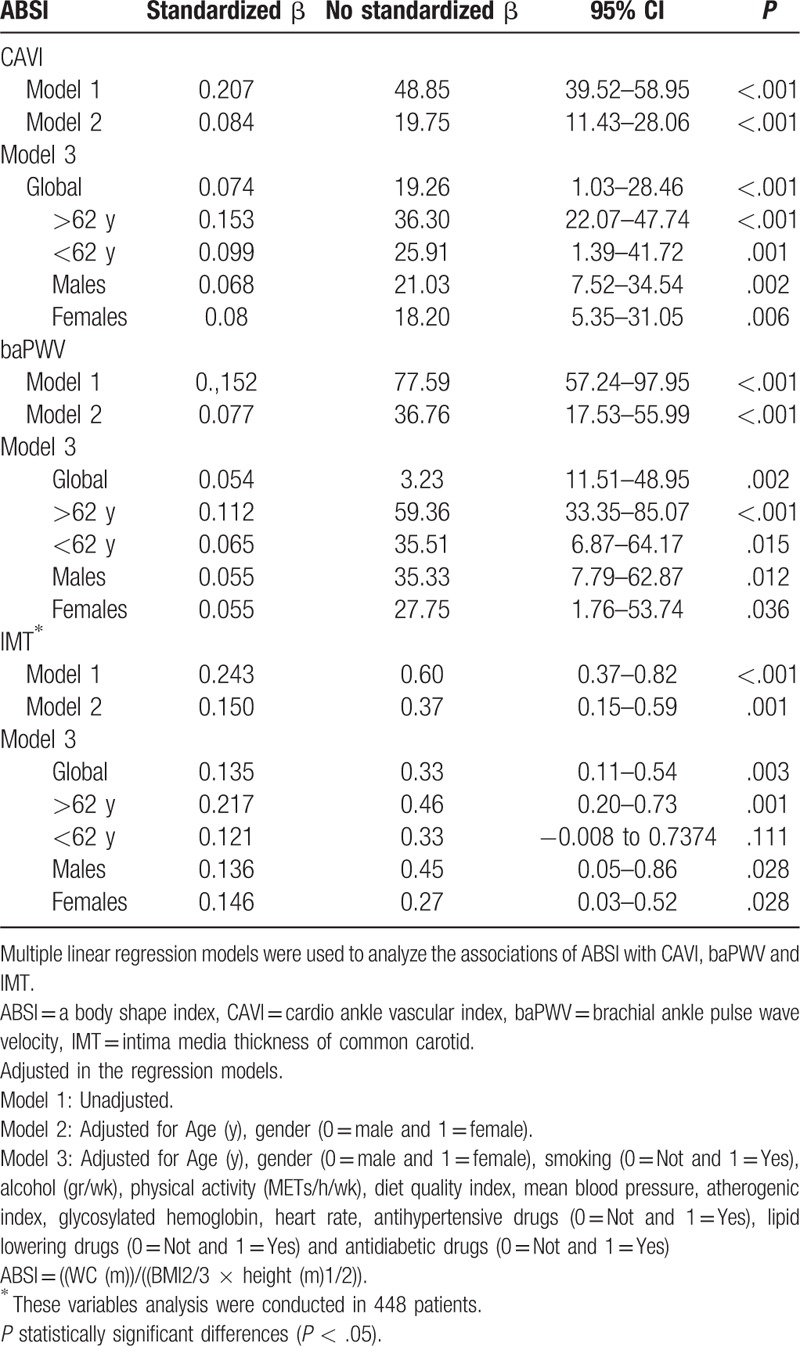
3.2. Multiple linear regression analysis
In the multiple linear regression analysis, after adjusting for various confounders, ABSI was positively associated with CAVI, baPWV, and IMT in all models (P < .01 for all, except for the IMT in the subgroup ≤ 62 years), as shown in Table 3, being stronger for subjects older than 62 years. For each unit increase in ABSI, CAVI increased by 0.16, baPWV by 0.25 m/s, and IMT by 0.033 mm.
Table 3.
Multiple regression analysis of ABSI with CAVI, baPWV, and IMT.
3.3. Logistic regression analysis
Figure 2 shows the results of unadjusted logistic regression analysis and Fig. 3 shows the results of multiple regression analysis after adjusting for confounders used in the model 3. In the logistic regression analysis, the OR of the ABSI was 1.84 (95% CI, 1.17–2.51) for IMT ≥ 0.90 mm, 1.37 (95% CI, 1.13–1.67) for CAVI ≥ 9, and 1.48 (95% CI, 1.19–1.82) for high baPWV ≥ 15 m/s, in the overall subject group, and in sex- and age-specific (>62 years, ≤ 62 years) subgroups, after adjusting for confounders. The OR of the ABSI was also > 1 for all evaluated parameters, when the subjects were grouped by sex and age (> 62 years, < 62 years).
Figure 2.
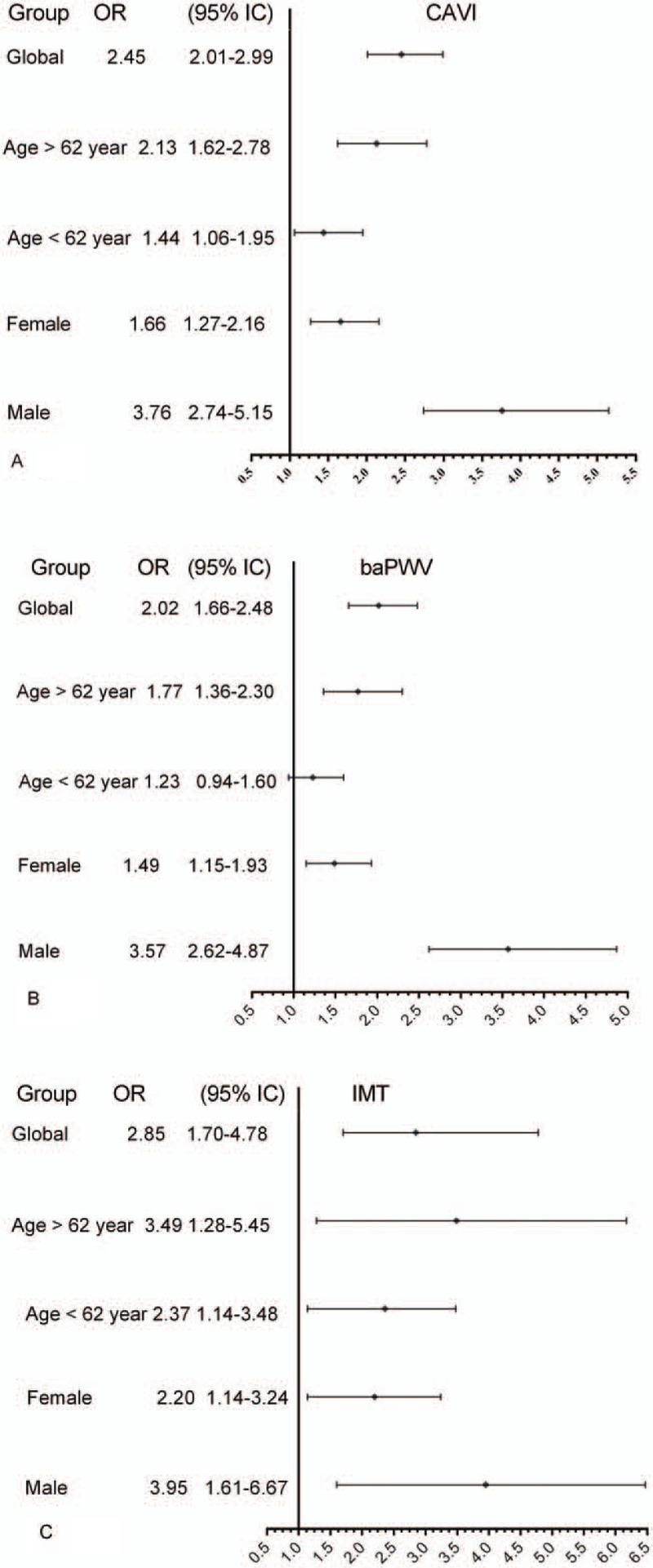
Logistic regression analysis showing unadjusted overall, sex-specific, and age-specific (≤62 and >62 years) OR of ABSI according to CAVI (A), baPWV (B), and average mean IMT (C). OR = odds ratio, CI = confidence interval, CAVI = cardio-ankle vascular index, baPWV = brachial-ankle pulse wave velocity, IMT = intima media thickness.
Figure 3.
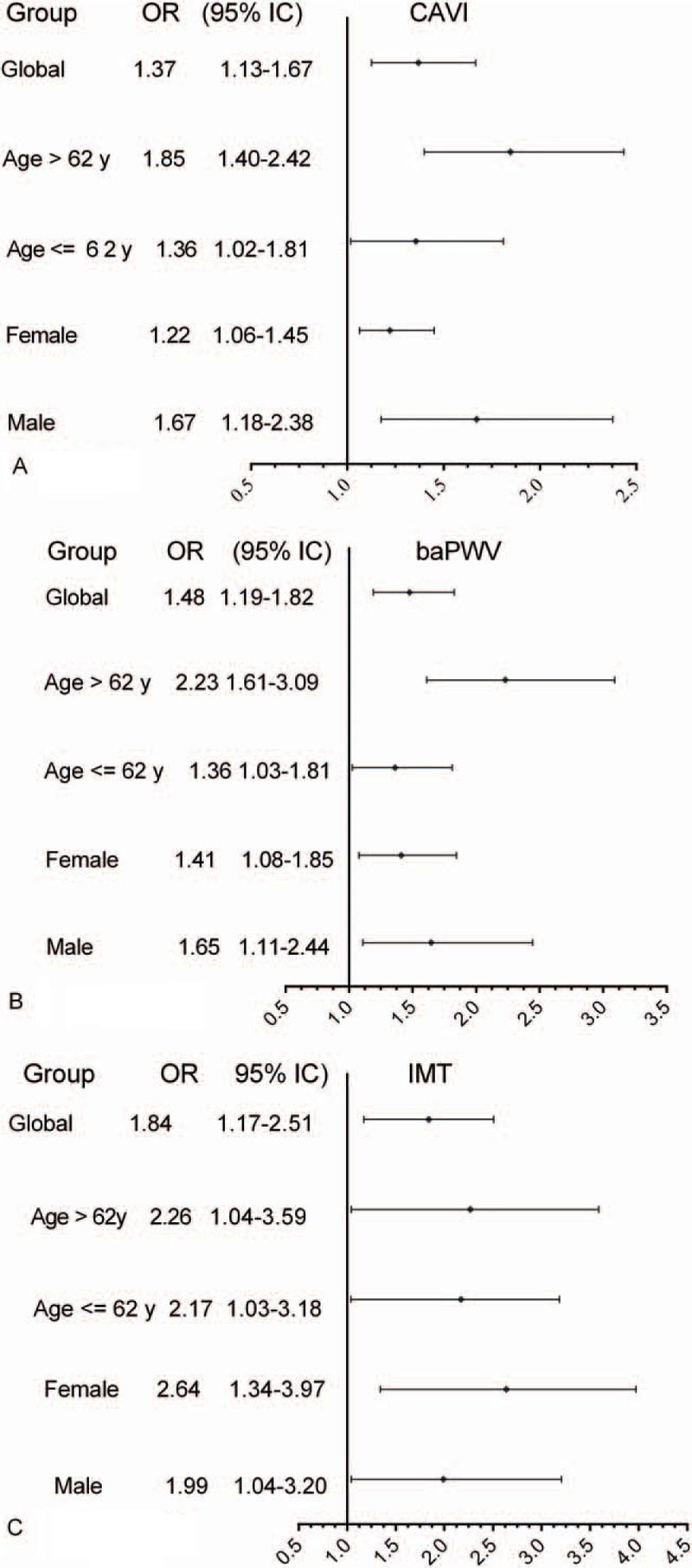
Logistic regression analysis showing, overall, sex-specific, and age-specific (≤62 and >62 years) adjusted OR of ABSI according to CAVI (A), baPWV (B), and average mean IMT (C). Adjustment was performed for age (years), sex (0 = male and 1 = female), smoking (0 = No and 1 = Yes), amount of alcohol intake (g/wk), physical activity (METs/h/wk), diet quality index, BMI, mean blood pressure, glycosylated hemoglobin level, heart rate and atherogenic index, and use of antihypertensive drugs (0 = No and 1 = Yes), lipid lowering drugs (0 = No and 1 = Yes), and antidiabetic drugs (0 = No and 1 = Yes). OR = odds ratio, CI = confidence interval, CAVI = cardio-ankle vascular index, baPWV = brachial-ankle pulse wave velocity, IMT = intima media thickness.
3.4. Curves ROC analysis
The AUROC of the ABSI was 0.631 (95% CI, 0.608–0.654) for CAVI ≥ 9, and 0.617 (95% CI, 0.593–0.641) for high baPWV ≥ 15 m/sec. The AUROC of the BMI was 0.414 (95% CI, 0.391–0.436) for CAVI ≥ 9, and 0.497 (95% CI, 0.472–0.521) for high baPWV ≥ 15 m/s. The AUROC of the WC was 0.483 (95% CI, 0.459–0.506) for CAVI ≥ 9, and 0.504 (95% CI, 0.472–0.536) for high baPWV ≥ 15 m/s (Supplementary Figure 1S).
4. Discussion
Our study revealed a positive association between ABSI and used vascular structure and function measures. This association was independent of drugs used to treat hypertension, diabetes mellitus, and dyslipidemia, and of the cardiovascular risk factors and lifestyle. These findings suggest that ABSI might be a good anthropometric measurement to predict vascular structure and function in Spanish subjects at intermediate cardiovascular risk.
Some studies found that IMT and increased arterial stiffness are associated with an increased number of cardiovascular events and mortality, both in general population and in diabetic patients.[20,45–48] On the other hand, ABSI is more associated with all-cause mortality and cardiovascular and cancer mortality than are other anthropometric measurements, and it predicts all-cause mortality independently of BMI.[6–8] Therefore, finding an association between ABSI and vascular structure and function may provide new approaches to evaluate the risk of cardiovascular events in people at intermediate cardiovascular risk.
In this study the mean value of CAVI was higher in men, which is in agreement with published data indicating that CAVI increases linearly with age according to the following formulas: CAVI = 5.0 + 0.048 × age (years) in men, and CAVI = 4.8 + 0.045 × age (years) in women,[49] and that the values of CAVI are higher in men than in women (approximately by 0.2, which is equivalent to 4–5 years old).[49–51] We found no sex differences in the median values of baPWV, which is consistent with data published by Tomiyama et al[52] who showed that the effect of age on baPWV is different according to sex category. Prepubertal women have a higher arterial stiffness than men, and this increases after menopause. However, men show a linear increase in arterial stiffness from puberty. This suggests that women have large arteries that are intrinsically more rigid compared with those of men. However, in women of reproductive age, the effects are offset by sex steroids.[53,54]
Therefore, the relationship between ABSI and the analyzed arterial stiffness parameters may be modified by the influence of age and sex upon arterial aging.
Bouchi et al[55] found that increased visceral fat, with a normal weight, is associated with increased arterial stiffness. Kim et al[56] in turn showed that increased visceral fat, with a normal WC, is associated with increased carotid atherosclerosis. Therefore, elevated ABSI values might indicate low skeletal muscle mass with increased visceral adiposity, together implying an accelerated progression of arterial stiffness. In this regard, ABSI could be an important addition to BMI for identifying subjects at intermediate cardiovascular risk and with an increased risk of arterial stiffness.
This study is the first to show that ABSI may be an important marker of IMT and arterial stiffness, assessed by CAVI and baPWV, in a large sample of Spanish subjects at intermediate cardiovascular risk. Moreover, this association is maintained in the analysis of those subjects when grouped by sex and age (>62 years, ≤62 years). The results of this study suggest that the association between ABSI and arterial stiffness is greater beyond the age of 62 years and in men. On the other hand, age is known to influence arterial stiffness—the latter increasing after 60 years of age.[49,52]
We have found 2 studies that analyzed the relationship between ABSI and arterial stiffness, measured by baPWV, in patients with type 2 diabetes mellitus[28] and in Chinese adults.[57] Their results agree with those found in our investigation. ABSI is positively associated with arterial stiffness assessed by baPWV, independently of visceral adiposity.[28,57] A noteworthy aspect of this study is that the association is maintained after adjusting for different lifestyles that could affect the distribution of body fat and nonfat mass, such as exercise, diet, smoking, and alcohol drinking, and act as confounders in the association of ABSI with arterial stiffness.
However, several studies have analyzed the association of other anthropometric measurements (BMI and WC) with arterial stiffness. In the general population without cardiovascular disease,[25–27] carotid femoral pulse wave velocity (cfPWV) showed a moderately positive relationship with WC (correlation coefficient r, 0.16–0.40) and BMI (r, 0.12–0.35). Nevertheless, in the study by Rodrigues et al,[25] when performing multiple regression analysis adjusted for age, mean arterial pressure, and heart rate, BMI showed a negative association (β = −0.103, P = .12), and the observed relationship with WC was lost. Only Strasser et al[27] confirmed the association of these anthropometric measurements with baPWV, obtaining similar results with for (r = 0.26) and BMI (r = 0.23). Studies conducted on diabetic patients[58–61] showed a weaker relationship between cfPWV and anthropometric measurements, obtaining r coefficients between 0.08 and 0.15, both for WC and BMI. Furthermore, in some cases, the relationship with WC[59] or BMI[60] disappeared after adjusting for potential confounders. Finally, the study conducted by Recio-Rodrigues et al[24] in healthy subjects and in hypertensive and diabetic patients concluded that, independently of the presence of diabetes mellitus or hypertension, abdominal obesity correlates better than peripheral obesity with cfPWV and IMT.
This negative association of BMI with CAVI has already been described in previous studies. In a studio realized in 23,257 healthy Japanese subjects showed that after adjusting for confounders, the CAVI correlated negatively with BMI in both sexes (r = −0.119).[51] These findings are consistent with our own observations. Furthermore, this negative correlation has also been reported in other population groups, such as children [62] and hypertensive and type 2 diabetic patients.[63] Similarly, waist circumference has shown a negative association with CAVI in subjects with metabolic syndrome.[64,65] However, not all studies have found a negative association. Consequently, the relationship between weight gain and arterial stiffness involves complex mechanisms, and vascular adaptation to fat accumulation remains the subject of controversy. Likewise, the physiopathological mechanisms explaining how obesity increases the incidence of cardiovascular disease complementary to the classical risk factors have not been fully clarified.[66] On the other hand, it must be remembered that arterial stiffness depends on arterial wall elasticity and diameter, and a positive correlation has been found between BMI and aortic diameter measured by nuclear magnetic resonance.[67] This could partially explain the negative association of BMI with arterial stiffness.
The results of our study suggest that ABSI is an anthropometric parameter that offers advantages over BMI in the analysis of the association between adiposity and the vascular structure and function measures in subjects with intermediate cardiovascular risk. This could be explained by the fact that ABSI takes BMI, WC, and height into account, mitigating the limitations of these parameters considered separately.[2,5] In our study, ABSI was positively correlated to CAVI and baPWV, while BMI showed a negative correlation to CAVI and no correlation to baPWV. We therefore consider that ABSI is a measure that offers complementary clinical information beyond the mere mathematical effect derived from its calculation, since it shows a direct correlation to the two used stiffness measures, thereby facilitating clinical interpretation.
Our results suggest that the association of arterial stiffness with measures of central obesity (WC) and peripheral obesity (BMI) is unclear both in general population and in patients with diabetes mellitus. Therefore, based on this study, it is necessary to promote new research on large samples, examining various anthropometric measurements and stiffness measures of the central and peripheral vascular system.
In summary, the results of our investigation are novel and may have important clinical relevance, showing the association of ABSI, which includes measures of both general and abdominal obesity, with vascular structure and function in patients at intermediate cardiovascular risk. It also provides information to conduct prospective studies and to analyze whether its use would improve cardiovascular risk equations. Therefore, because it is easy to determine and has a low cost, ABSI can be useful in clinical practice.
The main limitation of our study is its cross-sectional design, which did not allow us to establish causal relations or the direction of the influence of the vascular structural and functional parameters on ABSI and vice versa. Second, the population of this study was ethnically homogeneous (all subjects were Spanish at intermediate cardiovascular risk), and therefore, the extrapolation of our findings may be limited. Another limitation that should be kept in mind is that carotid ultrasound measurements were only performed in 448 subjects.
In conclusion, the results of this study indicate that ABSI is positively associated with vascular structure and function, independently of BMI and other confounders that may influence weight and fat mass distribution in subjects at intermediate cardiovascular risk. Therefore, ABSI, because of easy calculation and low cost, can be a useful clinical tool to detect individuals at high risk of presenting abnormalities in vascular structure and function.
Acknowledgments
The authors are grateful to all professionals participating in the MARK study.
Lead author of this group: Rafel Ramos, Research Unit, Primary Health Care, Girona, Jordi Gol Institute for Primary Care Research (IDIAP Jordi Gol), Catalonia, Spain
E-mail: rramos.girona.ics@gencat.net.
Coordinating persons and centers: Rafel Ramos, Ruth Martí, Dídac Parramon, Anna Ponjoan, Miquel Quesada, Maria Garcia-Gil, Martina Sidera, and Lourdes Camós, Research Unit, Primary Health Care, Jordi Gol Institute for Primary Care Research (IDIAP Jordi Gol), C/Maluquer Salvador, 11, Girona 17002, Catalonia, Spain
Fernando Montesinos, Ignacio Montoya, Carlos López, Anna Agell, Núria Pagès of the Primary Care Services, Girona, Catalan Institute of Health (ICS), Catalonia, Spain
Irina Gil, Anna Maria-Castro of the Primary Care Services, Girona, Institut d’Assistència Sanitaria (IAS), Catalonia, Spain
Fernando Rigo, Guillermo Frontera, Antònia Rotger, Natalia Feuerbach, Susana Pons, Natividad Garcia, John Guillaumet, Micaela Llull, and Mercedes Gutierrez of the Health Center Primary Care San Augustín, Ibsalut Balears, Spain
Cristina Agudo-Conde, Leticia Gómez-Sanchez, Carmen Castaño-Sanchez, Carmela Rodriguez-Martín, Benigna Sanchez-Salgado, Angela de Cabo-Laso, Marta Gómez-Sánchez, Emiliano Rodriguez-Sanchez, Jose Angel Maderuelo-Fernandez, Emilio Ramos-Delgado, Carmen Patino-Alonso, Jose I Recio-Rodriguez, Manuel A Gomez-Marcos, and Luis Garcia-Ortiz, Primary Care Research Unit of The Alamedilla, Castilla and León Health Service (SACYL), Salamanca, Spain
Author contributions
LG-S and MAGG-M prepared the manuscript draft, participated in fund raising and interpretation of results, and corrected the final version of the manuscript. LG-O participated in the study design, interpretation of results, and manuscript review. CA-C, ER-S, and FR participated in data collection and manuscript review. MCP-A and AM performed all analytical methods, interpretation of results, and manuscript review. RR, RM, LG-O, MG-S, and MAG-M participated in the protocol design, fund raising, analysis of results, and final review of the manuscript. All authors reviewed and approved the final version of the manuscript.
Conceptualization: Manuel A Gomez-Marcos, Rafel Ramos, Luis Garcia-Ortiz.
Data curation: Jose I Rodriguez-Sanchez, Fernando Rigo, Rhut Marti, Cristina Agudo-Conde, Rafel Ramos.
Formal analysis: Manuel A Gomez-Marcos, Maria C Patino-Alonso, Luis Garcia-Ortiz.
Funding acquisition: Manuel A Gomez-Marcos, Marta Gomez-Sanchez, Fernando Rigo, Rhut Marti, Rafel Ramos.
Investigation: Manuel A Gomez-Marcos, Leticia Gomez-Sanchez, Marta Gomez-Sanchez, Cristina Agudo-Conde, Rafel Ramos, Emiliano Rodriguez-Sanchez, Jose A Maderuelo-Farnandez, Luis Garcia-Ortiz.
Methodology: Manuel A Gomez-Marcos, Leticia Gomez-Sanchez, Maria C Patino-Alonso, Marta Gomez-Sanchez, Fernando Rigo, Rhut Marti, Rafel Ramos, Emiliano Rodriguez-Sanchez, Jose A Maderuelo-Farnandez, Luis Garcia-Ortiz.
Project administration: Manuel A Gomez-Marcos, Leticia Gomez-Sanchez, Fernando Rigo, Rhut Marti.
Supervision: Manuel A Gomez-Marcos, Leticia Gomez-Sanchez, Maria C Patino-Alonso, Rhut Marti, Cristina Agudo-Conde, Rafel Ramos, Emiliano Rodriguez-Sanchez, Jose A Maderuelo-Farnandez.
Validation: Jose I Rodriguez-Sanchez.
Writing – original draft: Manuel A Gomez-Marcos, Jose I Rodriguez-Sanchez, Emiliano Rodriguez-Sanchez, Jose A Maderuelo-Farnandez, Luis Garcia-Ortiz.
Writing – review & editing: Manuel A Gomez-Marcos, Leticia Gomez-Sanchez, Marta Gomez-Sanchez, Luis Garcia-Ortiz.
Supplementary Material
Footnotes
Abbreviations: ABSI = a body shape index, AUROC = area under the ROC curve, baPWV = brachial-ankle pulse wave velocity, BMI = body mass index, CAVI = cardio-ankle vascular index, cfPWV = carotid femoral pulse wave velocity, DBP = diastolic blood pressure, DQI = diet quality index, IMT = intima-media thickness, MARK = MediAte Risk management, MBP = mean blood pressure, METs = mean metabolic equivalents, ROC = receiver-operating characteristic, SBP = systolic blood pressure, WC = waist circumference.
JAM-F and LG-O contributed equally to this work.
This work was supported by grants from the Spanish Ministry of Science and Innovation (MICINN), the Carlos III Health Institute/European Regional Development Fund (ERDF) (MICINN, ISCIII/FEDER) (Red RedIAPP RD06/0018, Research Groups: RD16/0007/0003, RD16/0007/0004, RD16/0007/0008), the Health Research Fund (PI10/01088, PI10/02077, PI10/02043; PI13/01930), and the Regional Health Management of Castile and León (GRS 635/A/11; GRS 906/B/14).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Forouzanfar MH, Alexander L, Anderson HR, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:2287–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Nevill AM, Stewart AD, Olds T, et al. Relationship between adiposity and body size reveals limitations of BMI. Am J Phys Anthropol 2006;129:151–6. [DOI] [PubMed] [Google Scholar]
- [3].Patel AV, Hildebrand JS, Gapstur SM. Body mass index and all-cause mortality in a large prospective cohort of white and black U.S. Adults. PLoS One 2014;9:e109153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med 2006;355:763–78. [DOI] [PubMed] [Google Scholar]
- [5].Nishida C, Ko GT, Kumanyika S. Body fat distribution and noncommunicable diseases in populations: overview of the 2008 WHO Expert Consultation on Waist Circumference and Waist-Hip Ratio. Eur J Clin Nutr 2010;64:2–5. [DOI] [PubMed] [Google Scholar]
- [6].Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One 2012;7:e39504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Dhana K, Kavousi M, Ikram MA, et al. Body shape index in comparison with other anthropometric measures in prediction of total and cause-specific mortality. J Epidemiol Community Health 2016;70:90–6. [DOI] [PubMed] [Google Scholar]
- [8].Thomson CA, Garcia DO, Wertheim BC, et al. Body shape, adiposity index, and mortality in postmenopausal women: findings from the Women's Health Initiative. Obesity (Silver Spring) 2016;24:1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Rahman SA, Adjeroh D. Surface-based body shape index and its relationship with all-cause mortality. PLoS One 2015;10:e0144639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Cheung YB. A Body Shape Index” in middle-age and older Indonesian population: scaling exponents and association with incident hypertension. PLoS One 2014;9:e85421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Fujita M, Sato Y, Nagashima K, et al. Predictive power of a body shape index for development of diabetes, hypertension, and dyslipidemia in Japanese adults: a retrospective cohort study. PLoS One 2015;10:e0128972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].He S, Chen X. Could the new body shape index predict the new onset of diabetes mellitus in the Chinese population? PLoS One 2013;8:e50573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Legleye S, Beck F, Spilka S, et al. Correction of body-mass index using body-shape perception and socioeconomic status in adolescent self-report surveys. PLoS One 2014;9:e96768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Maessen MF, Eijsvogels TM, Verheggen RJ, et al. Entering a new era of body indices: the feasibility of a body shape index and body roundness index to identify cardiovascular health status. PLoS One 2014;9:e107212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Chambless LE, Heiss G, Folsom AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993. Am J Epidemiol 1997;146:483–94. [DOI] [PubMed] [Google Scholar]
- [16].Turin TC, Kita Y, Rumana N, et al. Brachial-ankle pulse wave velocity predicts all-cause mortality in the general population: findings from the Takashima study. Japan Hypertens Res 2010;33:922–5. [DOI] [PubMed] [Google Scholar]
- [17].Maeda Y, Inoguchi T, Etoh E, et al. Brachial-ankle pulse wave velocity predicts all-cause mortality and cardiovascular events in patients with diabetes: the Kyushu Prevention Study of Atherosclerosis. Diabetes Care 2014;37:2383–90. [DOI] [PubMed] [Google Scholar]
- [18].Izuhara M, Shioji K, Kadota S, et al. Relationship of cardio-ankle vascular index (CAVI) to carotid and coronary arteriosclerosis. Circ J 2008;72:1762–7. [DOI] [PubMed] [Google Scholar]
- [19].Okura T, Watanabe S, Kurata M, et al. Relationship between cardio-ankle vascular index (CAVI) and carotid atherosclerosis in patients with essential hypertension. Hypertens Res 2007;30:335–40. [DOI] [PubMed] [Google Scholar]
- [20].Nakamura K, Tomaru T, Yamamura S, et al. Cardio-ankle vascular index is a candidate predictor of coronary atherosclerosis. Circ J 2008;72:598–604. [DOI] [PubMed] [Google Scholar]
- [21].Satoh-Asahara N, Kotani K, Yamakage H, et al. Cardio-ankle vascular index predicts for the incidence of cardiovascular events in obese patients: a multicenter prospective cohort study (Japan Obesity and Metabolic Syndrome Study: JOMS). Atherosclerosis 2015;242:461–8. [DOI] [PubMed] [Google Scholar]
- [22].Gentile M, Iannuzzi A, Iannuzzo G, et al. Relation of body mass index with carotid intima-media thickness and diameter is independent of metabolic syndrome in postmenopausal Mediterranean women. Menopause 2012;19:1104–8. [DOI] [PubMed] [Google Scholar]
- [23].Rashid SA, Mahmud SA. Correlation between carotid artery intima-media thickness and luminal diameter with body mass index and other cardiovascular risk factors in adults. Sultan Qaboos Univ Med J 2015;15:e344–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Recio-Rodriguez JI, Gomez-Marcos MA, Patino-Alonso MC, et al. Abdominal obesity vs general obesity for identifying arterial stiffness, subclinical atherosclerosis and wave reflection in healthy, diabetics and hypertensive. BMC Cardiovasc Disord 2012;12:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Rodrigues SL, Baldo MP, Lani L, et al. Body mass index is not independently associated with increased aortic stiffness in a Brazilian population. Am J Hypertens 2012;25:1064–9. [DOI] [PubMed] [Google Scholar]
- [26].Wohlfahrt P, Somers VK, Cifkova R, et al. Relationship between measures of central and general adiposity with aortic stiffness in the general population. Atherosclerosis 2014;235:625–31. [DOI] [PubMed] [Google Scholar]
- [27].Strasser B, Arvandi M, Pasha EP, et al. Abdominal obesity is associated with arterial stiffness in middle-aged adults. Nutr Metab Cardiovasc Dis 2015;25:495–502. [DOI] [PubMed] [Google Scholar]
- [28].Bouchi R, Asakawa M, Ohara N, et al. Indirect measure of visceral adiposity ’A Body Shape Index’ (ABSI) is associated with arterial stiffness in patients with type 2 diabetes. BMJ Open Diabetes Res Care 2016;4:e000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Marti R, Parramon D, Garcia-Ortiz L, et al. Improving interMediAte risk management. MARK study. BMC Cardiovasc Disord 2011;11:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Marrugat J, D’Agostino R, Sullivan L, et al. An adaptation of the Framingham coronary heart disease risk function to European Mediterranean areas. J Epidemiol Community Health 2003;57:634–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Conroy RM, Pyorala K, Fitzgerald AP, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003;24:987–1003. [DOI] [PubMed] [Google Scholar]
- [32].Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013;31:1281–357. [DOI] [PubMed] [Google Scholar]
- [33].Salas-Salvado J, Rubio MA, Barbany M, et al. [SEEDO 2007 Consensus for the evaluation of overweight and obesity and the establishment of therapeutic intervention criteria]. Med Clin (Barc) 2007;128:184–96. [DOI] [PubMed] [Google Scholar]
- [34].O’Brien E, Asmar R, Beilin L, et al. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens 2005;23:697–701. [DOI] [PubMed] [Google Scholar]
- [35].Satoh N, Shimatsu A, Kato Y, et al. Evaluation of the cardio-ankle vascular index, a new indicator of arterial stiffness independent of blood pressure, in obesity and metabolic syndrome. Hypertens Res 2008;31:1921–30. [DOI] [PubMed] [Google Scholar]
- [36].Shirai K, Utino J, Otsuka K, et al. A novel blood pressure-independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI). J Atheroscler Thromb 2006;13:101–7. [DOI] [PubMed] [Google Scholar]
- [37].Shirai K, Hiruta N, Song M, et al. Cardio-ankle vascular index (CAVI) as a novel indicator of arterial stiffness: theory, evidence and perspectives. J Atheroscler Thromb 2011;18:924–38. [DOI] [PubMed] [Google Scholar]
- [38].Yamashina A, Tomiyama H, Takeda K, et al. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res 2002;25:359–64. [DOI] [PubMed] [Google Scholar]
- [39].Gomez-Marcos MA, Recio-Rodriguez JI, Patino-Alonso MC, et al. Protocol for measuring carotid intima-media thickness that best correlates with cardiovascular risk and target organ damage. Am J Hypertens 2012;25:955–61. [DOI] [PubMed] [Google Scholar]
- [40].Schroder H, Benitez Arciniega A, Soler C, et al. Validity of two short screeners for diet quality in time-limited settings. Public Health Nutr 2012;15:618–26. [DOI] [PubMed] [Google Scholar]
- [41].Schroder H, Covas MI, Marrugat J, et al. Use of a three-day estimated food record, a 72-hour recall and a food-frequency questionnaire for dietary assessment in a Mediterranean Spanish population. Clin Nutr 2001;20:429–37. [DOI] [PubMed] [Google Scholar]
- [42].Elosua R, Marrugat J, Molina L, et al. Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish men. The MARATHOM Investigators. Am J Epidemiol 1994;139:1197–209. [DOI] [PubMed] [Google Scholar]
- [43].Elosua R, Garcia M, Aguilar A, et al. Validation of the Minnesota Leisure Time Physical Activity Questionnaire In Spanish Women. Investigators of the MARATDON Group. Med Sci Sports Exerc 2000;32:1431–7. [DOI] [PubMed] [Google Scholar]
- [44].World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194. [DOI] [PubMed] [Google Scholar]
- [45].Chung CM, Tseng YH, Lin YS, et al. Association of brachial-ankle pulse wave velocity with atherosclerosis and presence of coronary artery disease in older patients. Clin Interv Aging 2015;10:1369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 2010;55:1318–27. [DOI] [PubMed] [Google Scholar]
- [47].Mitchell GF, Hwang SJ, Vasan RS, et al. Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 2010;121:505–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Lorenz MW, Markus HS, Bots ML, et al. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation 2007;115:459–67. [DOI] [PubMed] [Google Scholar]
- [49].Choi SY, Oh BH, Bae Park J, et al. Age-associated increase in arterial stiffness measured according to the cardio-ankle vascular index without blood pressure changes in healthy adults. J Atheroscler Thromb 2013;20:911–23. [DOI] [PubMed] [Google Scholar]
- [50].Brunner EJ, Shipley MJ, Ahmadi-Abhari S, et al. Adiposity, obesity, and arterial aging: longitudinal study of aortic stiffness in the Whitehall II cohort. Hypertension 2015;66:294–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Nagayama D, Imamura H, Sato Y, et al. Inverse relationship of cardioankle vascular index with BMI in healthy Japanese subjects: a cross-sectional study. Vasc Health Risk Manag 2017;13:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Tomiyama H, Yamashina A, Arai T, et al. Influences of age and gender on results of noninvasive brachial-ankle pulse wave velocity measurement—a survey of 12517 subjects. Atherosclerosis 2003;166:303–9. [DOI] [PubMed] [Google Scholar]
- [53].Marlatt KL, Kelly AS, Steinberger J, et al. The influence of gender on carotid artery compliance and distensibility in children and adults. J Clin Ultrasound 2013;41:340–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Bartok CJ, Marini ME, Birch LL. High body mass index percentile accurately reflects excess adiposity in white girls. J Am Diet Assoc 2011;111:437–41. [DOI] [PubMed] [Google Scholar]
- [55].Bouchi R, Minami I, Ohara N, et al. Impact of increased visceral adiposity with normal weight on the progression of arterial stiffness in Japanese patients with type 2 diabetes. BMJ Open Diabetes Res Care 2015;3:e000081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Kim SK, Park SW, Kim SH, et al. Visceral fat amount is associated with carotid atherosclerosis even in type 2 diabetic men with a normal waist circumference. Int J Obes (Lond) 2009;33:131–5. [DOI] [PubMed] [Google Scholar]
- [57].Zhang J, Fang L, Qiu L, et al. Comparison of the ability to identify arterial stiffness between two new anthropometric indices and classical obesity indices in Chinese adults. Atherosclerosis 2017;263:263–71. [DOI] [PubMed] [Google Scholar]
- [58].Martin V, Davila-Batista V, Castilla J, et al. Comparison of body mass index (BMI) with the CUN-BAE body adiposity estimator in the prediction of hypertension and type 2 diabetes. BMC Public Health 2016;16:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Moh MC, Sum CF, Lam BC, et al. Evaluation of body adiposity index as a predictor of aortic stiffness in multi-ethnic Asian population with type 2 diabetes. Diab Vasc Dis Res 2015;12:111–8. [DOI] [PubMed] [Google Scholar]
- [60].Teoh WL, Price JF, Williamson RM, et al. Metabolic parameters associated with arterial stiffness in older adults with Type 2 diabetes: the Edinburgh Type 2 diabetes study. J Hypertens 2013;31:1010–7. [DOI] [PubMed] [Google Scholar]
- [61].Dahlen EM, Bjarnegard N, Lanne T, et al. Sagittal abdominal diameter is a more independent measure compared with waist circumference to predict arterial stiffness in subjects with type 2 diabetes—a prospective observational cohort study. Cardiovasc Diabetol 2013;12:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Philip R, Alpert BS, Schwingshackl A, et al. Inverse relationship between cardio-ankle vascular index and body mass index in healthy children. J Pediatr 2015;167:361–5. e1. [DOI] [PubMed] [Google Scholar]
- [63].Yeboah K, Antwi DA, Gyan B, et al. Arterial stiffness in hypertensive and type 2 diabetes patients in Ghana: comparison of the cardio-ankle vascular index and central aortic techniques. BMC Endocr Disord 2016;16:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Al-Daghri NM, Al-Attas OS, Wani K, et al. Sensitivity of various adiposity indices in identifying cardiometabolic diseases in Arab adults. Cardiovasc Diabetol 2015;14:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Gomez-Sanchez L, Garcia-Ortiz L, Patino-Alonso MC, et al. Association of metabolic syndrome and its components with arterial stiffness in Caucasian subjects of the MARK study: a cross-sectional trial. Cardiovasc Diabetol 2016;15:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2006;113:898–918. [DOI] [PubMed] [Google Scholar]
- [67].Danias PG, Tritos NA, Stuber M, et al. Comparison of aortic elasticity determined by cardiovascular magnetic resonance imaging in obese versus lean adults. Am J Cardiol 2003;91:195–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


