Supplemental Digital Content is available in the text
Keywords: fluoroscopy-guided, free-hand, pedicle screw, robot, spine surgery
Abstract
Background:
A miniature spine-mounted robot has recently been introduced to further improve the accuracy of pedicle screw placement in spine surgery. However, the differences in accuracy between the robotic-assisted (RA) technique and the free-hand with fluoroscopy-guided (FH) method for pedicle screw placement are controversial. A meta-analysis was conducted to focus on this problem.
Methods:
Several randomized controlled trials (RCTs) and cohort studies involving RA and FH and published before January 2017 were searched for using the Cochrane Library, Ovid, Web of Science, PubMed, and EMBASE databases. A total of 55 papers were selected. After the full-text assessment, 45 clinical trials were excluded. The final meta-analysis included 10 articles.
Results:
The accuracy of pedicle screw placement within the RA group was significantly greater than the accuracy within the FH group (odds ratio 95%, “perfect accuracy” confidence interval: 1.38–2.07, P < .01; odds ratio 95% “clinically acceptable” Confidence Interval: 1.17–2.08, P < .01).
Conclusions:
There are significant differences in accuracy between RA surgery and FH surgery. It was demonstrated that the RA technique is superior to the conventional method in terms of the accuracy of pedicle screw placement.
1. Introduction
As a common surgical procedure, the pedicle screw placement method has been widely employed to reconstruct local stability in spine surgery due to its great three-column control. However, the conventional free-hand pedicle screw placement method is prone to pedicle violation.[1] Although there is a low morbidity of clinically relevant complications, a misplaced screw can result in neurovascular damage, dural tearing, or visceral involvement because of the anatomical proximity of the vertebral pedicles to associated neurovascular structures.[2] Therefore, a variety of techniques have been introduced to assist screw insertion and to reduce the prevalence of pedicle violation.
Presently, the conventional free-hand with fluoroscopy-guided method (FH) is still the principal method performed for pedicle screw implantation. However, a consensus has developed that the image-guided navigation systems provide more accuracy over the conventional method in terms of pedicle screw insertion.[3] Recently, a miniature spine-mounted robot (Renaissance, Mazor Robotics, Caesarea, Israel) has been introduced to further reduce pedicle violation and relevant complications. Its advantages are powerfully supported by a number of studies.[4–10] Nevertheless, some hold opposite viewpoints, believing that the FH technique offers more accuracy than the robotic-assisted technology (RA) or that there are few differences between them.[11,12] A meta-analysis investigated this controversy and concluded that the superiority of RA in the accuracy of screw placement was indefinite, compared with FH,[13] but the results were unconvincing due to a lack of sufficient number of studies, and the evaluation method for determining accuracy demands were simplistic. Our review is an updated meta-analysis that used double evaluation methods (perfect and clinically acceptable measurement standards)[14] to focus on this controversy.
2. Methods
2.1. Search strategy
Several databases, including the Cochrane Library, Ovid, Web of Science, PubMed and EMBASE, were searched for studies published before January 2017 that focused on the accuracy of pedicle screw insertion involving RA and FH. We explored abstracts, titles and subtitles by searching for the term “pedicle screw” combined with the following Key words: “robot,” “robotic,” “robotics,” “spine,” and “accuracy”. The resulting abstracts were inspected to identify articles that should be excluded. Subsequently; the remaining full-text articles were reviewed to select publications that were suitable for inclusion. The study selection process conformed to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. As a meta-analysis; no ethics committee or institutional review board approval was necessary for the study.
2.2. Inclusion and exclusion criteria
Inclusion criteria were established before the search, and the following criteria were used: the article must involve pedicle screw insertion with spine robot, articles must conduct postoperative computed tomography (CT) scanning for accuracy assessment, and articles must present sufficient data in each arm to enable meaningful comparison (more than 10 pedicle screws in each study group). Excluded criteria were as follows: duplicated publications, no conventional FH pedicle screw insertion in the control group, and articles not containing screw accuracy data.
2.3. Data extraction
Two reviewers (YF and JPD) independently screened and extracted data by applying the same standard; discrepancies were resolved through discussion until a consensus was reached. The following basic information was extracted: first author's name, year of publication, study type, patient sizes, interventions, tool of assessment, key and secondary results. In this meta-analysis, the following 2 uniform measurement standards were used to collect primary data for further analysis: perfect (screw completely within pedicle), and clinically acceptable (a portion of the screw outside the pedicle ≤3 mm without relevant complications). To avoid potential bias due to the use of a single standard, these standards were applied to the results from 3 different evaluation methods.
2.4. Appraisal of evidence and statistical analysis
The odds ratios (OR) with 95% confidence intervals (CI) were summarized for the accuracy of pedicle screw placement. The level of significance was set at P < .05. A forest plot was generated to compare the accuracy of pedicle screw placement between the experimental and control groups; the point estimate on the right of the vertical line indicates the experimental group was significantly more accurate than the control group. Heterogeneity was assessed by the chi-square test. For P > .1 or I2 < 50%, no clear heterogeneity of results was assumed. Heterogeneity stems from a variety of different variations among several studies in systematic reviews, which may affect the synergistic effects of several studies and the explanation of the results of the meta-analysis; a strict evaluation is generally required. Although it is impossible to completely prevent heterogeneity, it can be controlled for by including high-quality studies that all have the same study objective. We selected a fixed-effect model for all analyses unless there was significant heterogeneity. To examine the stability of the outcomes and to identify important sources of slight heterogeneity, influence analyses and subgroup analyses were conducted. Funnel plots were examined for any evidence of publication bias if sufficient studies were included in the meta-analysis (n ≥ 10). The Cochrane Collaboration's Tool and Newcastle-Ottawa Quality Assessment Scale were used to appraise the quality of the included papers. Statistical analyses were performed using the statistical software Review Manager Version 5.0 (Cochrane Collaboration, Software Update, Oxford, UK).
3. Results
3.1. Literature search and basic characteristics
The primary search strategy resulted in 625 articles. After reading the titles, abstracts, and full texts, ultimately, 10 reviews[4–8,12,15–18] were included in this meta-analysis without identifying additional studies from the references of published papers. A flow diagram of the report selection is shown in Supplemental Digital Content (see Figure, Supplemental Content).
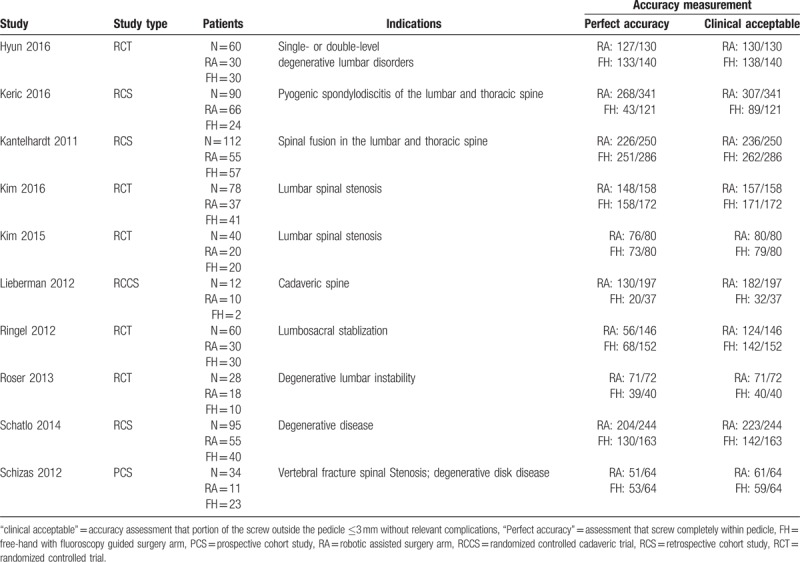
The studies were performed from 2011 to 2016 and included a total of 597 patients, 12 cadavers and 2937 screws. A total of 1255 pedicle screws were inserted using the FH technique, and 1682 pedicle screws were inserted using the RA technique. CT scanning was performed for the postoperative assessment of pedicle accuracy in all the trials. Table 1 provides the detailed characteristics and key results of the involved patients.
Table 1.
Characteristics of included studies.
3.2. Quality of included studies
A funnel plot was performed to test for possible publication bias. As shown in Fig. 1, the studies were nearly symmetrically distributed on both sides of the vertical line, indicating a relatively small publication bias. The results of the quality assessment that derived from the employment of the Cochrane Collaboration's Tool and the Newcastle-Ottawa Quality Assessment Scale can be found in Fig. 2, showing a small level of high risk of bias in the RCTs and evaluated scores of >5 stars in cohort studies; obviously, the included studies all expressed satisfactory quality. A controlled cadaveric study conducted by Lieberman et al,[16] which did not report a pre hoc power calculation but was otherwise well designed, met our inclusion criteria, and was included and assessed separately.
Figure 1.
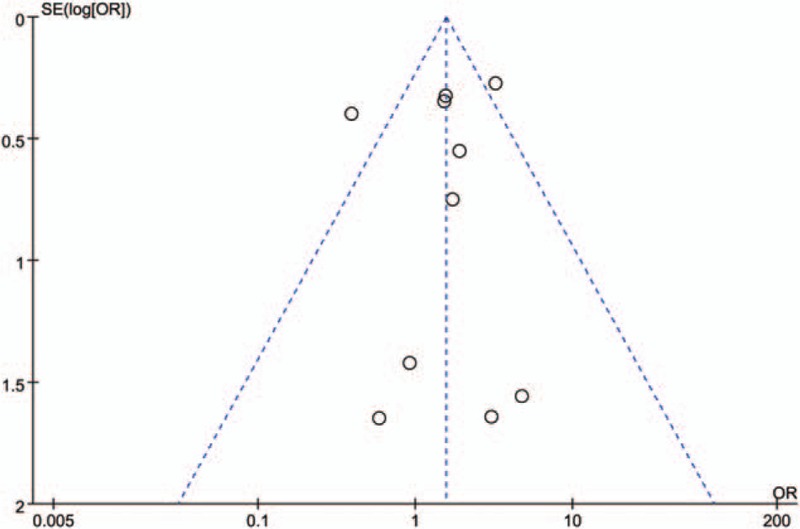
Funnel plot of included studies.
Figure 2.
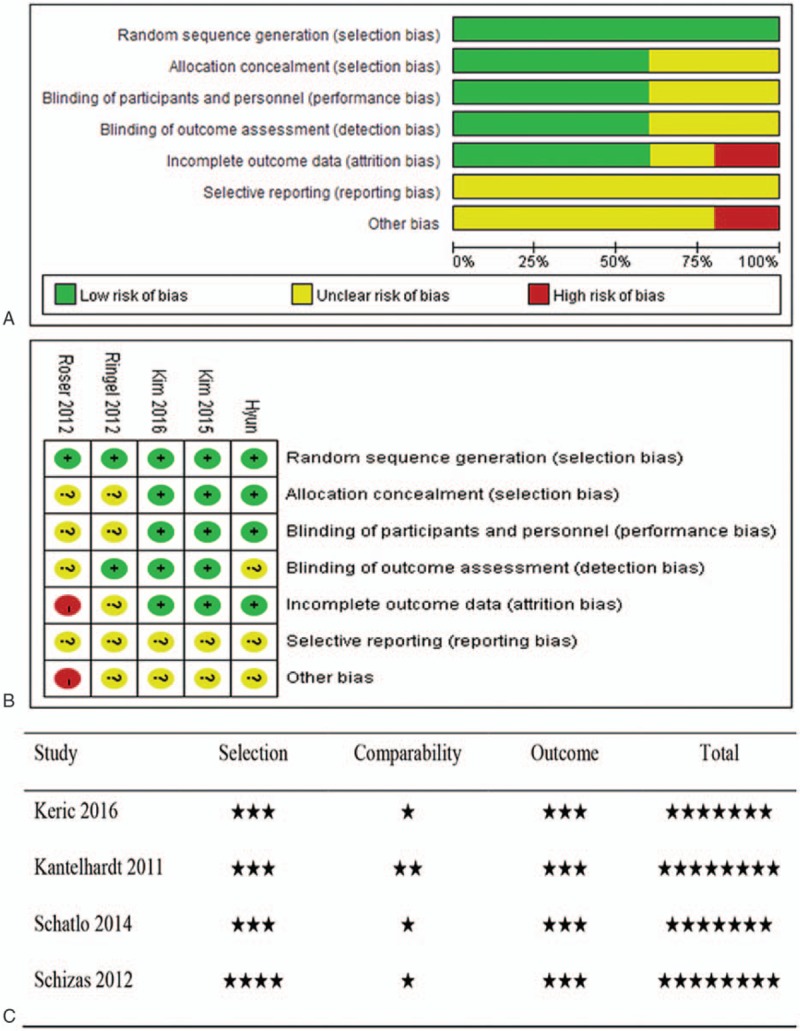
(A) Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies. (B) Risk of bias summary: review authors’ judgements about each risk of bias item for each included study. (C) Scores of the Newcastle-Ottawa Quality Assessment Scale for 4 cohort studies.
3.3. Meta-analyses of primary endpoints
3.3.1. “Perfect” pedicle screw insertion
Accuracy assessment that the screw was completely within the pedicle was considered “Perfect” accuracy. Fig. 3A shows that the RA group was significantly more accurate (OR 95% CI: 1.38–2.07 P < .01) than the FH group for pedicle screw placement. However, we found that the RA group had a huge heterogeneity (χ2 = 51.28 P < .1 I2 = 82%), which may lead to an unconvincing result. Then, an influence analysis (Fig. 4) was employed to identify potential sources of serious heterogeneity. Surprisingly, Keric et al[15] and Ringel et al[12] deviated tremendously in the total confidence interval. The recalculated forest plot (OR 95% CI: 1.02–1077 P = .03) shows that the heterogeneity reduced to 0% after the removal of those 2 papers (Fig. 3B), indicating that the studies of Keric et al and Ringel et al may be a great source of heterogeneity.
Figure 3.
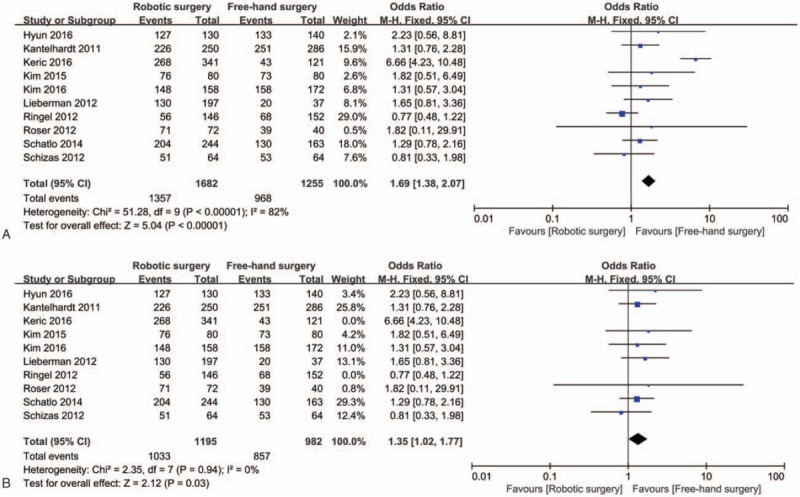
Forest plot of “Perfect” pedicle screw insertion; (A): RA surgery versus FH surgery. (B): RA versus FH after removal of Keric et al[15] and Ringel et al[12]. RA = robotic-assisted; FH = fluoroscopy-guided.
Figure 4.
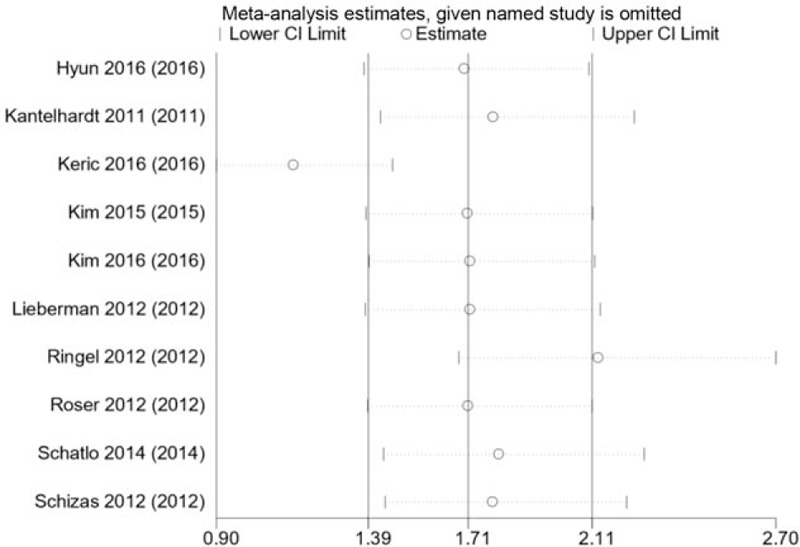
Influence analysis of “Perfect” pedicle screw insertion.
3.3.2. “Clinically acceptable” pedicle screw insertion
“Clinically acceptable” means that the portion of the screw outside the pedicle is ≤3 mm without relevant complications. Fig. 5 shows a statistically significant difference between the RA group and FH group; obviously, the RA arm is significantly more accurate (OR 95% CI: 1.17–2.08 P = .003) than the FH arm, but a moderate heterogeneity (χ2 = 20.12 P < .1 I2 = 55%) was found in the forest plot. Clinically acceptable accuracy was concurrently evaluated using 3 slightly different evaluation methods. RA technology can be divided into 2 categories, an open RA approach and a percutaneous RA approach. A new tool named Peterson, which was used with an upgraded version of the robots to prevent skidding of the guiding cannula on a slanted or sloped anatomy,[6] also exists. Therefore, considering this potential risk of bias before the design of the meta-analysis, subgroup analyses were conducted to identify possible sources of heterogeneity. Figure 6 shows the reduction of heterogeneity (Gertzbein and Robbins scale: χ2 = 8.76 P > .1 I2 = 43%; Rampersaud scale: χ2 = 0.01 P > .1 I2 = 0%) to varying degrees in the 2 subgroups, and tests for subgroup differences were significant (χ2 = 8.48 P < .1 I2 = 76.4%). The remainder of the subgroups show an increase in heterogeneity (Wiesner and Schizas scale: χ2 = 2.83 P < .1 I2 = 65%), which may result from the article of Keric et al[15] Furthermore, the subgroup that applied the Peterson technique showed a clear reduction of heterogeneity (55%–0%), and the subgroup differences were very large. The open or percutaneous subgroup analysis shows that the subgroup differences were 0% (χ2 = 0.04 P > .1 I2 = 0%). Overall, the differences in the evaluation scale and the application of the Peterson tool may be 2 potential sources of statistical heterogeneity instead of reflecting differences in the RA operative approach.
Figure 5.
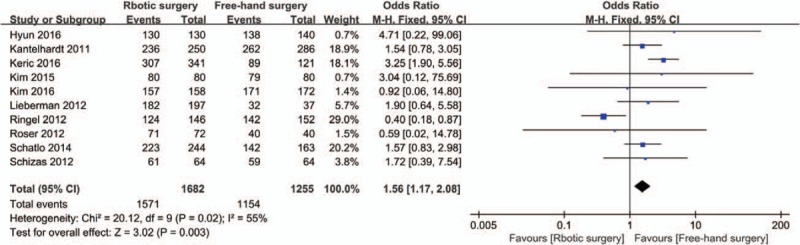
Forest plot of “Clinically acceptable” pedicle screw insertion.
Figure 6.
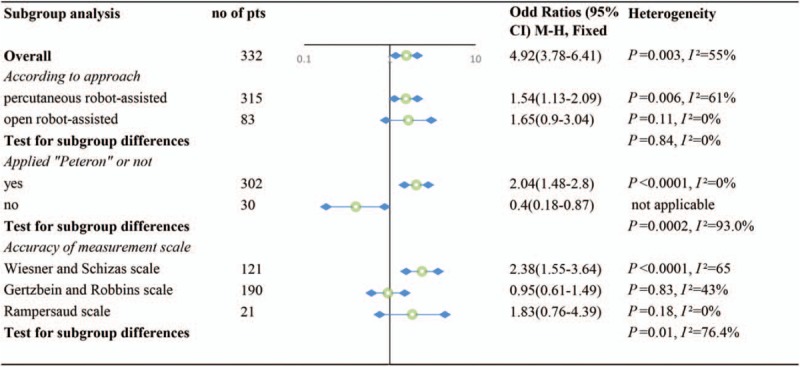
Forest plot of sub-analysis of “Clinically acceptable” pedicle screw insertion.
4. Discussion
4.1. Characteristics of the new technique
The accuracy of pedicle screw placement is a major concern for many spine surgeons. Although the accuracy of screw insertion could be improved with constant practice and an increase in experience in FH surgery, the misplaced rates for conventional techniques have definitely been shown to cover the range of from 5% to 41% in the lumbar spine and from 3% to 55% in the thoracic spine.[19] Except for limitations of the fluoroscopy guided technique itself, one of the important reasons may be that the accuracy is partially limited by the surgeon's freehand motion. Long-duration operations lead to fatigue of the operator and his muscles, which may decrease the accuracy of screw implantation.[20–22]
The introduction of Renaissance, a spinous process-mounted miniature robot, holds great potential. Although RA spine surgery is an emerging field and seems to be in its infancy,[21] its advantages of minimal access and high accuracy of screw placement are vital reasons why some “pioneering” surgeons are entering into this field. The miniature robot has the beneficial characteristics of ergonomics and great dexterity that augments the surgeon's hands and eliminates physiological tremor. Additional benefits include image-based semi-active guidance for screw insertion, the ability to hold tools for long periods of time and for repetitive motions, quick response to change in commands, excellent three-dimensional visualization, and reduction of intraoperative dosage of radiation exposure.[23]
The robot platform is used as a computerized mechanical positioning system that assists surgeons on the placement of implants along the planned trajectory. The system consists of two units: a cylindrically shaped, miniature robot with an end-effector that can be moved in 6 degrees-of-freedom, and a connected workstation that runs a graphical user interface software to take responsibility for intraoperative real-time robot motion monitoring and control, preoperative planning, image acquisition, registration for matching and calculations.[9] Basic steps in the robot operation are summarized as follows: preoperative planning, attachment to bony anatomyimage acquisition and registration, Robot assembly and motion, and Pedicle preparation and screw insertion. Then, the robot motion and the screw placement are consecutively repeated for other planned implants.
4.2. Accuracy of pedicle screw insertion using robots is still controversial
Although the robot was invented with several inherent advantages, a major controversy comes with it. A cadaveric study conducted by Lieberman et al[16] to investigate the accuracy of pedicle screw placement using a robotic guidance system showed that the RA arm had fewer screw placement deviations (average, 2.6 ± 0.7 mm vs 1.1 ± 0.4 mm; P < .0001) relative to the FH group, and it concluded that robotic guidance systems may make the surgeon more comfortable with implanting pedicle-based fixation by choosing percutaneous surgery or minimally invasive options for patients in general. Other studies also clearly indicate a support for the RA technique in the accuracy of pedicle screw placement;[1,4,5,7,8,18] however, some authors hold the opposite opinion.[11,12] The randomized controlled trial by Ringel et al[12] demonstrated significantly poor screw insertion in the RA group compared with the FH group (85% vs 93%); furthermore, 10 screws implanted using RA required intraoperative revision compared with only 1 in the control group. Nevertheless, a meta-analysis by Liu et al[13] pooled 3 RCTs and 2 cohort studies to address this controversy and demonstrated that no significant difference was found between the 2 techniques in terms of accuracy; therefore, it would require further studies to determine the unresolved clinical equipoise in this field. This paper had several distinct limitations, including a lack of sufficient RCTs and comparative studies, an unclear appraisal of evidence, and the use of a single evaluation criterion to collect data for primary endpoints. Accordingly, we conducted an updated meta-analysis to address these previous limitations and focused on the present contradiction.
Clearly, the meta-analysis result of a “Perfect” standard reveals that the RA group was statistically more accurate than the FH group for pedicle screw placement; in addition, the funnel plot and risk of bias graphs all indicated great reliability of the pooled results. However, there was serious statistical heterogeneity (χ2 = 51.28 P < .1 I2 = 82%). Influence analyses indicated that studies by Keric et al[15] and Ringel et al[12] may have brought an enormous risk of bias. However, the analysis showed a positive outcome with no statistical heterogeneity when these 2 articles were removed, which indicates the reliability of the total result. The meta-analysis result of the “Clinically acceptable” standard demonstrated a conclusion consistent with the “Perfect” standard, but its moderate heterogeneity cannot be overlooked. Some potential risk of bias was considered before the plan of analysis, and then the 2 subgroup analyses were made, which implies that the variance of assessment scale and the application of the Peterson tool may have generated a potential risk of bias.
The high risk of bias needs further analysis. A retrospective cohort by Keric et al[15] reported the “Perfect” accuracy that the screw position classified as GRADE 0 in the FH arm was much lower (35.5%) than in the other included papers, and over the full-text review, no obvious reasons were found to cause such an unusual condition. However, it received 6 out of 9 stars after an appraisal using the Newcastle-Ottawa Quality Assessment Scale, which indicates that the relatively low quality may be one of the reasons for the significant heterogeneity. Other limitations are as follows: a total of 90 patients were included, but only 24 patients were treated by free-hand fluoroscopy-guided surgery (121 screws), making it an unmatched control group; and an unclear independent blind assessment. Another randomized controlled trial by Ringel et al[12] reported remarkable deviation from the CI as shown on the influence analysis graph, which may have resulted from the following greatly important reasons: the patients likely have not been blinded to the procedure they underwent, the method of generation of randomization was not described, and He attributed the inaccuracy of the RA pedicle screw implantation to the application of the bed mount platform. However, 85% of the screws were inserted with the same platform in another RCT by Kim et al[6] which was not considered a real reason. Instead, it might be that the employment of the first generation of the robot (SpineAssist, Mazor Robotics, Caesarea, Israel) caused lateral slippage because no entry point preparation was conducted. The remainder of the articles mainly utilized the Peterson technique, in which a manual percussive tool was passed through the robotic arm to flatten the surfaces at the docking area of the cannulated tools to prevent such skidding,[17] which flattens and smooths the screw entry point before pedicle drilling. An earlier report discussed the importance of valid preoperative planning of entry, which is the point of successful screw placement when using a robot.[24] Moreover, they chose a lateral to medial pedicle screw trajectory, which could also have reduced lateral skidding.
Although a higher accuracy has been demonstrated in this review, and other advantages were shown in other papers, such as low intraoperative adverse events rate, low fluoroscopic times, short length of stay, small skin incision, minimal bleeding and infection, and a considerable learning curve,[4,6–8,10,18,19] there are still weaknesses in the use of the robotic system. For example, in one situation, an operation failed to match the preoperative CT scan with intraoperative fluoroscopy images in severe degenerative scoliosis, which wasted some time, and the surgeon had to change the surgical planning to free-hand. Although there was good registration, it still is possible that a cannula sliding off an angled bone surface could result in a most difficult-to-prevent lateral screw inaccuracy. Normally, this inaccuracy occurs lateral to the facet joint, demanding care when using the robot. Currently robots are used for spine surgery except at the cervical level because there is no appropriate place to mount the bridge for robot positioning at the cervical level.
In conclusion, this study demonstrates that the RA technique is superior to the conventional method in terms of accuracy of pedicle screw placement. Spine robots will be another available tool for surgeons to improve the accuracy of pedicle placement.
Author contributions
Data curation: Ji Jun Liu, Jia Nan Zhang.
Formal analysis: Jin Peng Du.
Investigation: Jin Peng Du, Ding Jun Hao.
Methodology: Jin Peng Du, Huan Huan Qiao.
Resources: Ding Jun Hao.
Software: Jin Peng Du, Jia Nan Zhang.
Validation: Ji Jun Liu, Ding Jun Hao.
Writing – original draft: Yong Fan.
Writing – review & editing: Jin Peng Du, Shi Chang Liu, Ding Jun Hao.
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, FH = free-hand with fluoroscopy-guided, RA = robotic-assisted.
YF and JPD have contributed equally to this study and should be considered co-first authors.
Funding: This study was funded by grants from the National Natural Science Foundation of China (grant numbers 81772357). We would like to thank all of the patients who participated in this study.
The authors declare that they have no competing interests.
Supplemental Digital Content is available for this article.
References
- [1].Lau D, Terman SW, Patel R, et al. Incidence of and risk factors for superior facet violation in minimally invasive versus open pedicle screw placement during transforaminal lumbar interbody fusion: a comparative analysis. J Neurosurg Spine 2013;18:356–61. [DOI] [PubMed] [Google Scholar]
- [2].Aoude AA, Fortin M, Figueiredo R, et al. Methods to determine pedicle screw placement accuracy in spine surgery: a systematic review. Eur Spine J 2015;24:990–1004. [DOI] [PubMed] [Google Scholar]
- [3].Tian NF, Huang QS, Zhou P, et al. Pedicle screw insertion accuracy with different assisted methods: a systematic review and meta-analysis of comparative studies. Eur Spine J 2011;20:846–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Roser F, Tatagiba M, Maier G. Spinal robotics: current applications and future perspectives. Neurosurgery 2013;72(suppl):12–8. [DOI] [PubMed] [Google Scholar]
- [5].Hyun SJ, Kim KJ, Jahng TA, et al. Minimally invasive, Robotic-vs. Open Fluoroscopic-guided spinal instrumented fusions-a randomized, controlled trial. Spine (Phila Pa 1976) 2017;42:353–8. [DOI] [PubMed] [Google Scholar]
- [6].Kim H-JMD, Lee SHMD, Chang B-SMD, et al. Monitoring the quality of robot-assisted pedicle screw fixation in the lumbar spine by using a cumulative summation test. Spine (Phila Pa 1976) 2015;40:87–94. [DOI] [PubMed] [Google Scholar]
- [7].Schatlo B, Molliqaj G, Cuvinciuc V, et al. Safety and accuracy of robot-assisted versus fluoroscopy-guided pedicle screw insertion for degenerative diseases of the lumbar spine: a matched cohort comparison. J Neurosurg Spine 2014;20:636–43. [DOI] [PubMed] [Google Scholar]
- [8].Kantelhardt SR, Martinez R, Baerwinkel S, et al. Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur Spine J 2011;20:860–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Devito DP, Kaplan L, Dietl R, et al. Clinical acceptance and accuracy assessment of spinal implants guided with spineassist surgical robot: retrospective study. Spine (Phila Pa 1976) 2010;35:2109–15. [DOI] [PubMed] [Google Scholar]
- [10].van Dijk JD, van den Ende RPJ, Stramigioli S, et al. Clinical pedicle screw accuracy and deviation from planning in Robot-guided spine surgery. Spine (Phila Pa 1976) 2015;40:E986–91. [DOI] [PubMed] [Google Scholar]
- [11].Laudato PA, Pierzchala K, Schizas C, et al. Switzerland. Pedicle screw insertion accuracy using O-arm, robotic guidance or freehand technique: a comparative study. Eur Spine J 2014;23(suppl):S481–2. [DOI] [PubMed] [Google Scholar]
- [12].Ringel F, Stuer C, Reinke A, et al. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: a prospective randomized comparison to conventional freehand screw implantation. Spine (Phila Pa 1976) 2012;37:E496–501. [DOI] [PubMed] [Google Scholar]
- [13].Liu H, Chen W, Wang Z, et al. Comparison of the accuracy between robot-assisted and conventional freehand pedicle screw placement: a systematic review and meta-analysis. Int J Comput Assist Radiol Surg 2016;11:2273–81. [DOI] [PubMed] [Google Scholar]
- [14].Fujishiro TMD, Nakaya YMD, Fukumoto SMD, et al. Accuracy of pedicle screw placement with robotic guidance system: a Cadaveric Study. Spine (Phila Pa 1976) 2015;40:1882–9. [DOI] [PubMed] [Google Scholar]
- [15].Keric N, Eum DJ, Afghanyar F, et al. Evaluation of surgical strategy of conventional vs. percutaneous robot-assisted spinal trans-pedicular instrumentation in spondylodiscitis. J Robot Surg 2017;11:17–25. [DOI] [PubMed] [Google Scholar]
- [16].Lieberman IHMD, Hardenbrook MAMD, Wang JCMD, et al. Assessment of pedicle screw placement accuracy, procedure time, and radiation exposure using a miniature Robotic guidance system. J Spinal Disord Tech 2012;25:241–8. [DOI] [PubMed] [Google Scholar]
- [17].Schizas C, Thein E, Kwiatkowski B, et al. Pedicle screw insertion: robotic assistance versus conventional C-arm fluoroscopy. Acta Orthopaedica Belgica 2012;78:240–5. [PubMed] [Google Scholar]
- [18].Kim HJ, Jung WI, Chang BS, et al. A prospective, randomized, controlled trial of robot-assisted vs freehand pedicle screw fixation in spine surgery. Int J Med Robot 2016;13:3. [DOI] [PubMed] [Google Scholar]
- [19].Mason A, Paulsen R, Babuska JM, et al. The accuracy of pedicle screw placement using intraoperative image guidance systems. J Neurosurgery Spine 2014;20:196–203. [DOI] [PubMed] [Google Scholar]
- [20].Lieberman IH, Togawa D, Kayanja MM, et al. Bone-mounted miniature robotic guidance for pedicle screw and translaminar facet screw placement: Part I–Technical development and a test case result. Neurosurgery 2006;59:641–50. discussion 641-650. [DOI] [PubMed] [Google Scholar]
- [21].Barzilay Y, Kaplan L, Libergall M. Robotic assisted spine surgery–a breakthrough or a surgical toy? Int J Med Robot 2008;4:195–6. [DOI] [PubMed] [Google Scholar]
- [22].Togawa D, Kayanja MM, Reinhardt MK, et al. Bone-mounted miniature robotic guidance for pedicle screw and translaminar facet screw placement: part 2–Evaluation of system accuracy. Neurosurgery 2007;60(2 suppl 1):ONS129–39. discussion ONS139. [DOI] [PubMed] [Google Scholar]
- [23].Matis GK, Silva D, Chrysou OI, et al. Robotics for spinal operations: reality or Alice in Wonderland? Int J Med Robot 2012;8:125–6. [DOI] [PubMed] [Google Scholar]
- [24].Hu X, Lieberman IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res 2014;472:1839–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


