Abstract
Background:
Homed-based exercise training via telehealth is an effective method for cardiac rehabilitation in patients with heart failure (HF). However, little is known about the effects of telehealth exercise training among patients with HF in China.
Design:
A randomized controlled design with repeated measures was adopted in this study.
Objective:
To examine the effect of our telehealth exercise training program on health outcomes in patients with HF in China.
Methods:
A total of 98 participants were randomly allocated to an experimental group (n = 49) and control group (n = 49) from January 2014 to February 2015 in a teaching hospital in Chengdu, People's Republic of China. Participants in the experimental group underwent an 8-week home-based telehealth exercise training program, including 32 exercise training sessions, with regular telephone or instant messaging follow-ups and consultations. Participants in the control group received usual care. The outcome variables used in this study were the Minnesota Living with Heart Failure Questionnaire, 6-minute walking distance (6MWD), resting heart rate (HR), Hospital Anxiety and Depression Scale, left ventricular ejection fraction (LVEF), and the New York Heart Association (NYHA) classification. Data were collected at baseline, post-test (2 months after discharge), and 4 months post-test (6 months after discharge). Repeated measures ANOVA was used to examine the effects of groups, changes over time, and interaction of time and group with the above variables.
Results:
Statistically significant improvements were observed in the experimental group regarding quality of life (QOL) and 6MWD compared to the control group post-test. Significant improvements in QOL, 6MWD, and resting HR were sustained for 4 months post-test. However, no significant improvements were observed regarding the NYHA classification, LVEF, anxiety, and depression at either the post-test or 4-month post-test follow-ups. No patients experienced any significant complications or adverse outcomes during the program.
Conclusions:
The results reveal that telehealth exercise training is an effective alternative method for cardiac rehabilitation, especially under the conditions in China.
Keywords: exercise training, heart failure, home-based, telehealth
1. Introduction
In China, approximately 4.5 million people suffer from heart failure (HF).[1] The mortality rate of HF is 12.3%, which is higher than the average mortality of 2.6% for cardiovascular diseases.[2] With the increasing age of the population, the prevalence of chronic heart failure (CHF) has increased dramatically despite improvements in medical treatment. Therefore, HF has become a serious public health issue in China.
Exercise training is a critical component of cardiac rehabilitation. Previous studies have demonstrated positive effects of exercise training programs on clinical outcomes for medically stable outpatients with HF.[3–5] Despite the benefits of exercise training programs, many patients do not have access to hospital-based training due to distance, costs, and poor health. To address this problem, home-based exercise training may be an acceptable alternative method for patients. Compared with telehealth care, traditional outpatient cardiac rehabilitation has many disadvantages, such as travel requirements and higher costs. Home-based telehealth rehabilitation helps overcome these barriers and increases cardiac rehabilitation compliance because of its convenience and accessibility. Telehealth rehabilitation without regular clinical and home visits has resulted in positive effects on health outcomes in patients with HF.[6,7] Clark et al[6] conducted a meta-analysis including 14 randomized controlled trials of remote monitoring (structured telephone support or tele-monitoring) to investigate its effects in patients with HF and found decreased HF admissions, reduced all-cause mortality, improved quality of life (QOL), and reduced healthcare costs. Piotrowicz et al[7] demonstrated that both home-based telehealth cardiac rehabilitation and standard cardiac rehabilitation at a clinic significantly improved QOL, but home-based telehealth cardiac rehabilitation showed better adherence compared with standard cardiac rehabilitation.
Although many benefits have been observed with the use of telehealth among patients with HF in Western countries, little is currently known about the effect of telehealth in China. As a developing country with a large population, China's medical resources are unevenly distributed, with significant disparities between the supply and demand. Therefore, the telehealth system is critical for delivering care to patients who do not have access to hospital-based care. Recently, the Chinese government initiated a project called “Internet + healthcare” to expand the accessibility of healthcare via advanced technologies, such as mobile phones, wearable devices, and computer receivers. However, the project remains at an early stage of implementation due to a lack of feasible modes, available technology, necessary devices, and health professionals. In this context, the large-scale application and promotion of telemedicine has many barriers under the current Chinese conditions. In addition, different conditions and customs make it impossible for China to conform to Western telehealth systems. Therefore, a feasible telehealth program from a Chinese perspective is warranted. We used QQ and Wechat software (Tencent company, Shenzhen, Guangdong province, China), the most popular instant messaging service in China, to deliver home-based telehealth exercise training. The aim of the study was to examine the effects of a telehealth exercise training program on health outcomes in patients with HF. The primary outcome in this study was quality of life, which was measured by the Minnesota Living with Heart Failure Questionnaire (MLHFQ).
2. Methods
2.1. Design
Our study used a prospective, randomized controlled trial design. A total of 98 patients were recruited from January 2014 to February 2015 in a teaching hospital in Chengdu, China. Cardiac nurses identified potential participants via medical records and interviews. Simple randomization was used in this study. The 98 eligible patients were randomly assigned to either the experimental group (n = 49) or the control group (n = 49) prior to discharge by the researchers using a computer-generated random sequence. Allocation concealment was assured by enclosing the assignments in sequentially numbered, opaque envelopes. The patients in the control group received usual care that included simple discharge education and regular follow-up visits at the clinic. The patients in the control group in the usual care setting were not given any type of instruction regarding exercise, while the patients in the experimental group received usual care plus telehealth exercise training.
2.2. Participants
Patients with HF and their caregivers were recruited from January 2014 to February 2015. The inclusion criteria for the patients were: a primary diagnosis of chronic HF for at least 3 months; New York Heart Association (NYHA) classification I to III; more than 18 years of age; a clinically stable condition with a regular medication regimen for at least 4 weeks before enrolment in the study; the ability to use Wechat or QQ software via a smart phone; discharged to home; and the ability to understand and speak Chinese. The exclusion criteria for the patients included: myocardial infarction within the last month, unstable angina, uncontrolled hypertension, severe respiratory diseases, decompensated non-cardiac disease, malignancy, physical disability, mental disease, or other contraindications that affected participation in this studysurgical treatment within the last month; and previous participation in exercise cardiac rehabilitation programs.
The outcome variables in this study were QOL, 6-minute walking distance (6MWD), resting heart rate (HR), left ventricular ejection fraction (LVEF), NYHA classification, anxiety, and depression. The primary outcome was quality of life, which was measured by the MLHFQ. With a type I error of 5% and 80% power, assuming that the standard deviation of scores would be similar to that of a previous study of exercise among people with CHF,[8] a total of 52 participants were recruited to detect clinically significant improvement on the MLHFQ between the groups.[8] We recruited additional participants to allow for withdrawals, with a total sample of 98 participants.
2.3. Intervention
The patients in the experimental group participated in a telehealth exercise training program. The telehealth training exercise program included a 2-month intervention (a printed brochure developed for patients, exercise training education, and 32 sessions of exercise training) and a 4-month follow-up. The procedures of the intervention are presented in Table 1.
Table 1.
The proposal of telehealth exercise training program.
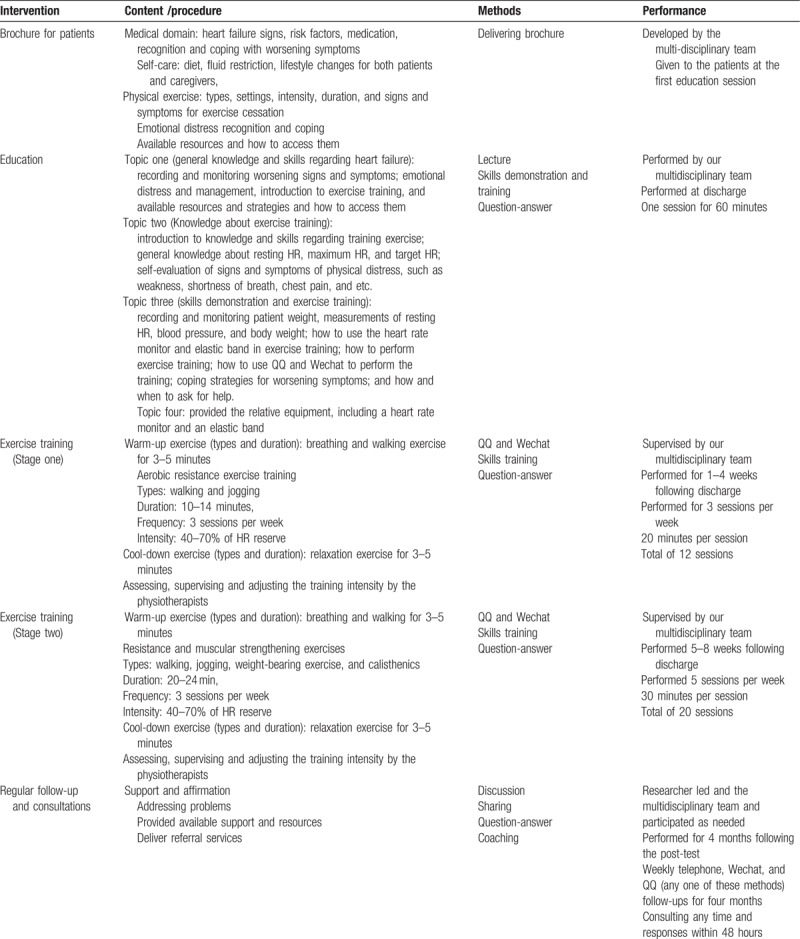
2.3.1. Exercise training
An instant messaging service provides a convenient and free means for people to exchange information online anywhere at any time via text-based, audio, or video conversations. Our telehealth exercise training program was conducted via online webcam communication and supervision using QQ and Wechat software. Prior to the intervention, a QQ group and a Wechat group were established to provide a platform for the patients and researchers to share information and interact with each other through instant messaging. Telehealth exercise training was performed by a multi-disciplinary team consisting of physiotherapists (exercise training), cardiac nurses (follow-up and self-care instruction), and psychiatric nurses (psychological instruction).
The 2-month exercise training program consisted of 2 stages: the first stage (1–4 weeks) was focused on endurance exercises, with 3 20-minute sessions per week. The training modalities included walking and jogging. Walking was the most common modality performed by patients in the first stage because of its simplicity. The patients received a total of 12 20-minute sessions of exercise training in the first stage, with 3 sessions per week. The second stage (5–8 weeks) included resistance and muscular strengthening exercises in 5 30-minute sessions per week. The patients performed endurance exercises before progressing to resistance exercises. The training modalities included walking, jogging, and calisthenics for muscular training. The muscular strengthening exercises included multiple weight-bearing calisthenics, such as single-leg squats, deep squats and partial squats, which were demonstrated by the physiotherapists at the education session at discharge. Resistance exercises were performed using the elastic band that was given to the patients at discharge. The patients received a total of 20 30-minute sessions of exercise training in the second stage, with five sessions per week.
In both stages, the physiotherapists were responsible for monitoring, assessing, and adjusting the training intensity according to an individual's condition. Exercise intensity was the main priority of the exercise prescription. In this study, exercise intensity was evaluated by target HR, which was calculated using the method known as HR reserve.[7] The target training HR was 40% to 70% of the HR reserve plus the resting HR.[7] Each training session in both stages started with a warm-up and ended with a cool-down exercise. The details of the exercise training program are presented in Table 1.
2.3.2. Regular follow-up and consultations
Cardiac nurses provided regular follow-ups every week during the exercise training program via dedicated telephone or Wechat and QQ instant messaging conversations. The follow-up included the following domains: discussions about the current situation and problems; support and resources; answers to questions; and referral services as needed. The participants could interact with the cardiac nurses at any time via telephone or Wechat as necessary. All questions and concerns received a response within 48 hours. The cardiac, rehabilitative, and psychiatric nurses in our multi-disciplinary team participated in consultations via telephone or Wechat groups as needed.
2.4. Data collection
The participants in each group completed 3 surveys at baseline (discharge), post-test (2 months following discharge) and 4 months post-test (6 months following discharge). Data were collected by blinded independent collectors. Data analysts and outcome assessors were blinded to the group assignments. The baseline data were collected at the hospital prior to discharge, including patients’ demographic characteristics, QOL, 6MWD, resting HR, LVEF, NYHA classification, and levels of anxiety and depression. The post-test and 4-month post-test data were collected during a clinic visit, including QOL, 6MWD, resting HR, LVEF, NYHA classification, and anxiety and depression levels. We scheduled appointments with the patients via telephone or Wechat prior to the data collection.
2.4.1. Demographic questionnaire
The demographic and clinical data of the patients included: gender, age, education level, marital status, employment, financial resources for treatment, monthly income, NYHA classification, duration of HF, number of comorbidities, and LVEF.
2.4.2. Hospital Anxiety and Depression Scale (HADS)
Psychological status was measured by the 14-item HADS, including 2 7-item subscales for anxiety and depression.[9,10] Both the English and Chinese versions of the HADS show adequate reliability and validity.[9–11]
2.4.3. Minnesota Living With Heart Failure Questionnaire (MLHFQ)
Health-related quality of life was measured by the 21-item MLHFQ.[12] Both the English and Chinese versions of the MLHFQ show adequate reliability and validity.[12–14]
6MWD The 6MWD was used to measure patients’ functional exercise capacity (6MWD) according to the guidelines of the American Thoracic Society.[15]
2.4.4. Resting HR
Resting HR reflects general functioning of the heart. The resting HR were measured and collected by the researchers at three follow-up times.
2.4.5. LVEF
The LVEF was measured using the conventional Simpson technique with 2-dimensional echocardiography at 3 follow-up points.[7]
2.5. Safety of the telehealth exercise training program
Safety is the main priority in the home-based telehealth exercise training program. The following strategies were considered to ensure safety: the patients recruited for our study were clinically stable, with mild to moderate HF according to the NYHA classification; a 60-minute education session on exercise training was held prior to discharge; the intensity of exercise training was low to moderate in terms of safety and protocols were designed by rehabilitation physicians based on patients’ personal conditions; patients’ caregivers was asked to accompany them during the training sessions in case of an emergency; each patient was given a HR monitor and was instructed to wear it during exercise and to report his or her real-time heart rate so that the rehabilitation doctors could adjust the training intensity accordingly; and the patients were asked to report to the doctor and stop the exercises immediately if they experienced signs or symptoms of physical distress, such as weakness, shortness of breath, chest pain, and nausea.
2.6. Ethical consideration
This study was approved by the Medical Ethics Committees of Sichuan University and the relevant hospital. The patients were informed about the study, including the purpose, procedure, and the right to withdraw at any time. Written informed consent was obtained from all patients.
2.7. Data analysis
The SPSS 17.0 statistical analysis package was used to perform the statistical analyses. Descriptive statistics were used to describe patients’ demographic and clinical variables. The comparison of patients’ baseline demographic and clinical data between the groups was performed by χ2 analysis and Fischer exact test as appropriate. The effects of differences between groups, changes within groups over time, and the interaction of group and time on 6MWD, resting HR, LVEF, NYHA classification, QOL, anxiety, and depression were examined by the general linear model (GLE) with repeated measures (ANOVA). P < .05 was considered statistically significant.
3. Results
3.1. Inclusion procedure of the participants
Of the 140 individuals who were screened for eligibility, 32 did not meet the inclusion criteria and 10 declined participation. A total of 98 participants were randomly allocated to the experimental group (n = 49) and the control group (n = 49). A total of 15 participants (7 in the experimental group and 8 in the control group) did not complete the 4-month follow-up. The attrition rates of the experimental and control groups at 4 months post-test were 14.3% and 16.3%, respectively. The flowchart of the inclusion procedure is presented in Figure 1. No patient had any significant complications or adverse outcomes during the program.
Figure 1.
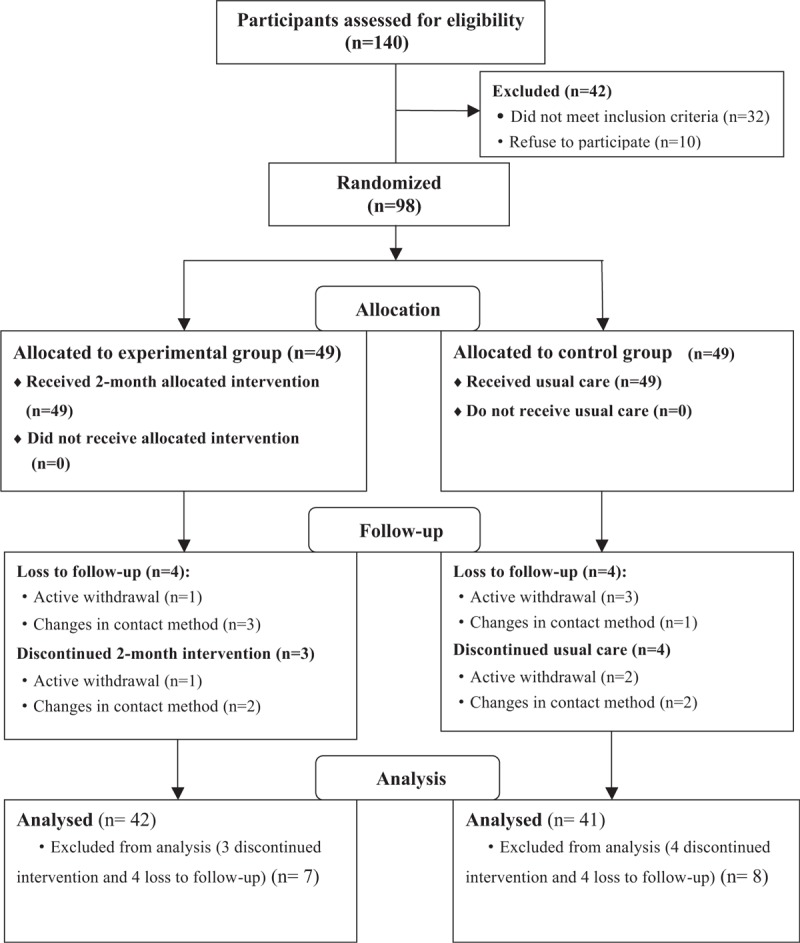
Participant flow chat in this study. Simple randomization was used in this study. The 98 eligible patients were randomly assigned to either the experimental group (n = 49) or the control group (n = 49) prior to discharge by the researchers using a computer-generated random sequence. The patients in the control group received usual care without any type of instruction regarding exercise, while the patients in the experimental group received usual care plus telehealth exercise training. All patients in both the experimental and control group received a 4-month follow-up. A total of 83 participants completed the follow-up (42 in the experimental group and 41 in the control group).
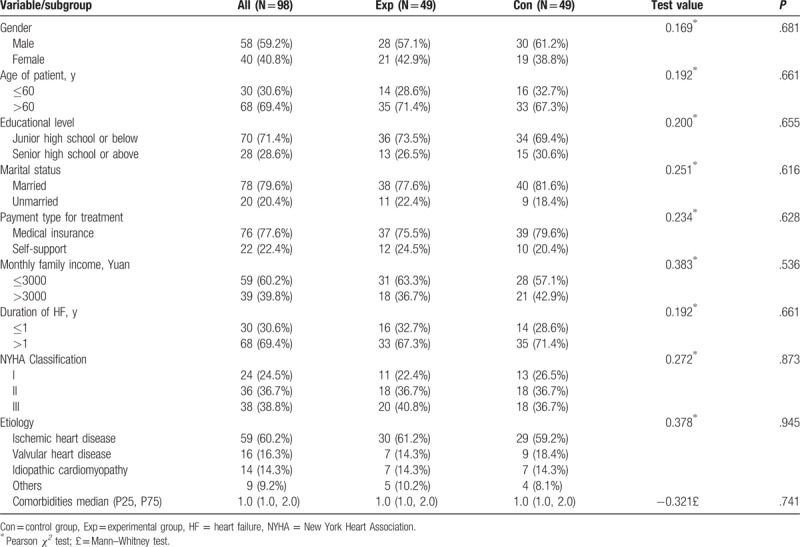
3.2. Characteristics of the participants
The characteristics of the patients at baseline are presented in Table 2. There were no significant differences between the experimental and control groups with respect to patients’ demographic and clinical variables (Table 2). The mean age of the patients was 66.3 years (SD = 10.50). Most of the patients were men (59.2%) and were married (79.6%). More than half of the patients (71.4%) had a junior high school education or below. Most patients (77.6%) had medical or other insurance. Most patients (69.4%) had HF for more than one year. The NYHA Classification ranged from Class I to Class III, including 24 Class I patients (24.5%), 36 Class II patients (36.7%), and 38 Class III patients (38.8%). The main aetiology of HF was ischaemic heart disease, which accounted for 60.2% of all cases.
Table 2.
Characteristics of the patients at baseline (N = 98).
3.3. Effects of the exercise training program
The data for the outcome variables at baseline, post-test (2 months after discharge) and 4 months post-test (6 months after discharge) are shown in Table 3.
Table 3.
Comparison of outcomes at three time points (n = 98).
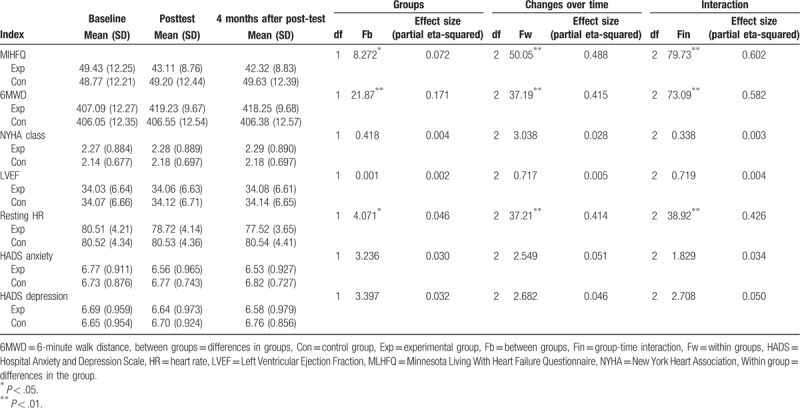
3.3.1. Effects on QOL
The MLHFQ was used to measure patients’ QOL, with higher scores indicating better health. Significant differences between the groups were found in terms of MLHFQ scores (Fb = 8.272, P = .005). Significant changes in MLHFQ scores were observed over time (Fw = 50.05, P = .000), and a significant interaction of group and time for MLHFQ scores was observed (Fin = 79.73, P = .000). The results indicated that the home-based telehealth exercise training program improved patient QOL significantly, with sustained improvement for 4 months after the post-test.
3.3.2. Effects on anxiety and depression
The HADS was used to measure anxiety and depression, with higher scores indicating higher levels of anxiety and depression. No statistically significant differences were observed between the groups regarding scores for either anxiety or depression (Fb = 3.236, P = .075; Fb = 3.397, P = .117). No significant changes in scores for either anxiety or depression were observed within the groups over time (Fw = 2.549, P = .87; Fw = 2.682, P = .97). No significant interaction of group and time for scores for anxiety and depression were observed (Fin = 1.829, P = .166; Fin = 2.708, P = .050). The results indicated that the home-based telehealth exercise training program had no significant effect on anxiety or depression.
3.3.3. Effects on the 6MWD, resting HR, NYHA classification, and LVEF
Statistically significant differences were observed between the groups (Fb = 21.87, P = .000; Fb = 4.071, P = .046), within group over time (Fw = 37.19, P = .000; Fw = 37.21, P = .000), and in group-time interaction (Fin = 73.09, P = .000; Fin = 38.92, P = .000) regarding the 6MWD and resting HR. There were no statistically significant differences between the groups (Fb = 0.418, P = .519; Fb = 0.001, P = . 984), within group over time (Fw = 3.038, P = .084; Fw = 0.717, P = .472), and in group-time interaction (Fin = 0.338, P = .562; Fin = 0.719, P = .471) regarding the NYHA Classification and LVEF, respectively.
4. Discussion
The present telehealth exercise rehabilitation program for patients with HF improved their health-related QOL and increased their functional exercise capacity and no adverse events were reported. The effects of the program were sustained at the 4-month post-test follow-up. No significant differences in anxiety, depression, NYHA classification, or LVEF were observed.
4.1. Effects of the telehealth exercise training program
A significant improvement in QOL was found following telehealth exercise training in patients with HF. The results were consistent with previous studies.[4,8] Giannuzzi et al[4] investigated the long-term effects of a 6-month moderate exercise training program among patients with stable HF and found significant improvements in their QOL and functional exercise capacity. They suggested that exercise training was a safe and effective method to improve QOL and exercise capacity.[4] Chien et al[8] found that an 8-week home-based exercise training program significantly improved functional exercise capacity and QOL in patients with HF. In our study, a positive effect on QOL may be related to several factors. Exercise training may improve QOL by ameliorating edema, fatigue, shortness of breath, and other uncomfortable symptoms in patients with HF. In addition, improved QOL may be related to increased exercise capacity, which may have a positive effect on patients’ self-perceived health status. Moreover, QOL could have increased due to consultations via the instant messaging service, which provided early symptom monitoring and recognition, timely medical treatment, and instant emotional support.
Our study showed a significant improvement in the 6MWD following telehealth exercise training in patients with HF. Significant benefits in exercise capacity were sustained for 4 months after the post-test. These results were consistent with previous studies.[4,7,8] Piotrowicz et al[7] compared the effects of a new model of home-based tele-monitored cardiac rehabilitation with those of an outpatient-based standard cardiac rehabilitation and found that the two cardiac rehabilitation programs both significantly improved QOL and functional exercise capacity. However, home-based tele-monitored cardiac rehabilitation resulted in better adherence compared with the outpatient-based standard rehabilitation. In China, there are no outpatient-based standard cardiac rehabilitation programs for patients with HF. The current study examined whether a telehealth home-based cardiac rehabilitation program was feasible and effective in China.
Our study showed a significant reduction in resting HR following telehealth exercise training in patients with HF. This significant reduction in resting HR was sustained for 4 months after the post-test. The results were consistent with previous studies.[16,17] Resting HR is one of the important determinants of myocardial oxygen consumption. A high resting HR is associated with a high cardiovascular risk.[17] Previous evidence has shown that a reduced HR can improve contractility and energy supply while reducing expenditure.[18,19] In addition, the risk of death decreased by 18% with every HR reduction of 5 beats/min.[20] Therefore, HR is an important target in the treatment of heart failure, and a reduced HR may improve cardiovascular outcomes in HF.[17] However, since the goal of HF treatment is to improve the long-term prognosis, blindly lowering HR could worsen HF.[21] As a result, exercise training for patients with HF should be conducted under the monitoring and supervision of specialists to ensure safety, and the training HR should be determined according to the specific conditions of a patient with HF.
Our study showed no significant improvements in NYHA classification or LVEF following telehealth exercise training in patients with HF. The results of previous studies in this area were inconsistent with our findings.[4,7,22] Piotrowicz et al[7] found that an 8-week home-based tele-monitored walking training program resulted in a significant reduction in NYHA classification in patients with HF. The study suggested that a well-designed home-based tele-monitored exercise training was effective in terms of improved cardiac functional capacity in patients with HF. Belardinelli et al[22] showed that a 10-year supervised exercise training program with moderate intensity in patients with NYHA Classification II to III HF did not significantly improve LVEF in the experimental group until the fifth year, with sustained improvement until the completion of the program. The results indicated that a long period is required to elicit positive training-induced effects on LVEF. In this study, our lack of significant improvement in NYHA classification and LVEF may be related to our 2-month period of exercise training, which was too short to detect an effect.
Depression is prevalent in patients with HF, and addressing depression improves symptoms in patients with HF.[23] Our study showed no significant improvements in anxiety or depression following telehealth exercise training or at 4 months after the program in patients with HF. The results of prior studies in this area are inconsistent.[8,24] For example, Kulcu et al[24] reported that an 8-week aerobic exercise program showed significant reductions in anxiety and depression among HF patients. In contrast, Chien et al[8] found that an individualized home-based exercise training program did not improve anxiety and depression. In our study, anxiety and depression scores at baseline were low, with little room for improvement. In addition, the lack of significant improvements in anxiety and depression may be related to a lack of face-to-face social interaction in the program. Therefore, further and longer interventions are warranted to examine the effects of home-based telehealth exercise training on the psychological status of patients with HF.
4.2. Acceptability of the telehealth exercise training program
Our program delivered telehealth cardiac rehabilitation by instant messaging, which provided an easy and acceptable way for people to have real-time interactions anywhere at any time. No participant showed any problems with the use of QQ and Wechat software during the program. In addition, the attrition rates of the experimental and control groups at 4 months post-test were 14.3% and 16.3%, respectively. Although there were no significant differences between the two groups in attrition rate (P > .05), the findings showed that more participants in the experimental group completed the telehealth program in contrast to those in the control group. Therefore, the findings indicated that our telehealth exercise training program is acceptable among the Chinese HF population.
5. Limitations
The representativeness of the sample was limited by the participants having been recruited from only one hospital in Chengdu. A multi-centre sampling study is recommended to expand the sample beyond this hospital. In addition, this study was also limited by the use of simple randomization, and we did not use block and stratified randomization to ensure equality between the groups. Another limitation was the short intervention and follow-up periods. Therefore, further studies are needed to examine the long-term and sustained effects of telehealth exercise training. Moreover, the generalizability of this study was limited by the requirement of owning a smart phone. Furthermore, other outcome measures should be considered to provide more objective information on health status, such as peak VO2, the cardiopulmonary exercise treadmill test, and pulmonary ventilation.
6. Implications for practice
As there is a significant lack of data regarding telehealth cardiac rehabilitation, this study provided important information about specific aspects of a home-based telehealth cardiac rehabilitation program and the required resources based on Chinese conditions, including discharge education, physician supervision and follow-ups via instant messaging.
7. Conclusions
In summary, we developed an acceptable telehealth exercise training program for patients with HF and found that it improved QOL and functional exercise capacity. A telehealth exercise training program is a feasible and effective method for cardiac rehabilitation. The home-based platform is specifically used in China, where medical resources are limited. Future long-term studies are warranted in China to examine the effective implications of home-based telehealth cardiac rehabilitation.
Acknowledgments
We would like to thank the executives and participating staff of the hospital for their support and assistance. Special thanks give to all participants for their understanding and cooperation.
Author contributions
Conceptualization: Xiaolin Hu, Yonglin Su, Xingchen Peng, Xiaoping Li.
Data curation: Moying Qu, Zhonghua Hu, Xiye Sun, Xiaoping Li.
Formal analysis: Xiaolin Hu, Xingchen Peng, Xiye Sun, Xiaoping Li.
Funding acquisition: Xiaolin Hu.
Investigation: Xiaolin Hu, Yonglin Su, Moying Qu, Zhonghua Hu, Xiye Sun, Xiaoping Li.
Methodology: Yonglin Su, Moying Qu, Xiye Sun, Xiaoping Li.
Project administration: Xiaolin Hu, Yonglin Su, Xiaoping Li.
Resources: Xiaolin Hu, Yonglin Su, Moying Qu, Zhonghua Hu, Xiye Sun, Xiaoping Li.
Software: Yonglin Su, Xingchen Peng, Zhonghua Hu.
Supervision: Xiaolin Hu, Mary Dolansky, Xingchen Peng.
Writing – original draft: Xiaolin Hu, Yonglin Su, Xingchen Peng.
Writing – review & editing: Mary Dolansky.
Footnotes
Abbreviations: 6MWD = 6-minute walking distance, CPET = cardiopulmonary exercise testing, HADS = Hospital Anxiety and Depression Scale, HF = heart failure, HR = heart rate, LVEF = left ventricular ejection fraction, MLHFQ = Minnesota Living with Heart Failure Questionnaire, NYHA = New York Heart Association, QOL = quality of life, SD = standard deviation.
This study was approved by the Ethics Committees of Sichuan University (K2014021). The study is funded by the National Natural Science Foundation of China (81803104), the Science and Technology Department of Sichuan Province (2016FZ0087 and 2017KZ0033), the health and family planning commission of Sichuan province (16PJ344 and 17PJ394), the Sichuan Medical Association (S16055), the China Scholarship Council (201706245002), and the initial Science Fund of Sichuan University for the Young Teachers (2017SCU11012).
The authors declare no conflicts of interest.
References
- [1].Wang W, Zhu ML, Wang YJ, et al. Report on cardiovascular diseases in China. Chin Circulation J 2012;28:408–12. [Google Scholar]
- [2].The Chinese society of Cardiology. Guidelines for the diagnosis and treatment of chronic heart failure. Chin J Cardiol 2007;35:1076–95. [Google Scholar]
- [3].Tol BA, Huijsmans RJ, Kroon DW, et al. Effects of exercise training on cardiac performance, exercise capacity and quality of life in patients with heart failure: a meta-analysis. Eur J Heart Fail 2006;8:841–50. [DOI] [PubMed] [Google Scholar]
- [4].Giannuzzi P, Temporelli PL, Corrà U, et al. Antiremodeling effect of long-term exercise training in patients with stable chronic heart failure results of the exercise in left ventricular dysfunction and chronic heart failure (ELVD-CHF) trial. Circulation 2003;108:554–9. [DOI] [PubMed] [Google Scholar]
- [5].O’Connor CM, Whellan DJ, Lee KL, et al. HF-ACTION Investigators. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 2009;301:1439–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Clark RA, Inglis SC, McAlister FA, et al. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ 2007;334:942–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Piotrowicz E, Baranowski R, Bilinska M, et al. A new model of home-based telemonitored cardiac rehabilitation in patients with heart failure: effectiveness, quality of life, and adherence. Eur J Heart Fail 2010;12:164–71. [DOI] [PubMed] [Google Scholar]
- [8].Chien CL, Lee CM, Wu YW, et al. Home-based exercise improves the quality of life and physical function but not the psychological status of people with chronic heart failure: a randomised trial. J Physiother 2011;57:157–63. [DOI] [PubMed] [Google Scholar]
- [9].Zigmond AS, Snaith R. The hospital anxiety and depression scale. Acta Psychiat Scand 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- [10].Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res 2002;52:69–77. [DOI] [PubMed] [Google Scholar]
- [11].Qian J, Bian CD, Cui HD, et al. Comparative study of reliability and validity between several screening scales of anxiety. J Int Med Concepts Pract 2011;6:176–9. [Chinese]. [Google Scholar]
- [12].Rector TS, Cohn JN. Assessment of patient outcome with the Minnesota Living with Heart Failure questionnaire: reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. Am Heart J 1992;124:1017–25. [DOI] [PubMed] [Google Scholar]
- [13].Middel B, Bouma J, de Jongste M, et al. Psychometric properties of the Minnesota living with heart failure questionnaire (MLHF-Q). Clin Rehabil 2001;15:489–500. [DOI] [PubMed] [Google Scholar]
- [14].Zhu YB, Hideki Q, Zheng J, et al. Evaluation on the reliability and validity of Chinese version of the Minnesota living with heart failure questionnaire. Chin J Behav Med Sci 2004;13:337–9. [Google Scholar]
- [15].ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Resp Crit Care 2002;166:111–7. [DOI] [PubMed] [Google Scholar]
- [16].Koukouvou G, Kouidi E, Iacovides A, et al. Quality of life, psychological and physiological changes following exercise training in patients with chronic heart failure. J Rehabil Med 2004;36:36–41. [DOI] [PubMed] [Google Scholar]
- [17].Böhm M, Swedberg K, Komajda M, et al. Heart rate as a risk factor in chronic heart failure (SHIFT): the association between heart rate and outcomes in a randomised placebo-controlled trial. Lancet 2010;376:886–94. [DOI] [PubMed] [Google Scholar]
- [18].Mulder P, Barbier S, Chagraoui A, et al. Long-term heart rate reduction induced by the selective if current inhibitor ivabradine improves left ventricular function and intrinsic myocardial structure in congestive heart failure. Circulation 2004;109:1674–9. [DOI] [PubMed] [Google Scholar]
- [19].Colin P, Ghaleh B, Monnet X, et al. Effect of graded heart rate reduction with ivabradine on myocardial oxygen consumption and diastolic time in exercising dogs. J Pharmacol Exp Ther 2004;308:236–40. [DOI] [PubMed] [Google Scholar]
- [20].McAlister FA, Wiebe N, Ezekowitz JA, et al. Meta-analysis: beta-blocker dose, heart rate reduction, and death in patients with heart failure. Ann Intern Med 2009;150:784–94. [DOI] [PubMed] [Google Scholar]
- [21].Li LW, Yi SX. Reduction of heart rate is not the target of heart failure treatment. Chin J Cardiol 2015;433:197–9. [PubMed] [Google Scholar]
- [22].Belardinelli R, Georgiou D, Cianci G, et al. 10-year exercise training in chronic heart failure: a randomized controlled trial. J Am Coll Cardiol 2012;60:1521–8. [DOI] [PubMed] [Google Scholar]
- [23].Gottlieb SS, Kop WJ, Ellis SJ, et al. HF-ACTION Investigators. Relation of depression to severity of illness in heart failure (from Heart Failure And a Controlled Trial Investigating Outcomes of Exercise Training [HF-ACTION]). Am J Cardiol 2009;103:1285–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kulcu DG, Kurtais Y, Tur BS, et al. The effect of cardiac rehabilitation on quality of life, anxiety and depression in patients with congestive heart failure. A randomized controlled trial, short-term results. Eura Med Phys 2007;43:489–97. [PubMed] [Google Scholar]


