Abstract
To discuss the value of “self-made ultrasonic scoring system” in predicting the different types of placenta accreta, and for predicting its associated risk of bleeding and hysterectomy.
A prospective study was performed in 137 patients who were suspiciously diagnosed with placenta accreta before delivery. All the patients were examined by the scoring system, and were classified into 3 groups according to their scores: score of ≤5 as N1, ≥6 and ≤9 as N2, and ≥10 as N3 groups. The accuracy and the Kappa values were calculated. Hemorrhage during the operation and the uterine resection rate were also compared.
There were 73 patients in N1, 36 in N2, and 28 in N3 groups. The prediction accuracy rates were 87.6% (64/73) and 92.0% (25/28), respectively in groups 1 and 3. The Kappa value was 0.75\0.77 for the prediction accuracy rate. The median quantities of hemorrhage during the operation were 400[100, 2000] mL, 1200[300, 9000] mL, and 4000[800, 13,000] mL, respectively. The uterine resection rates were 0.0%(0/73), 11.1%(4/36), and 39.3%(11/28), respectively. Comparison of hemorrhage and uterine resection rate among the 3 groups was significant (P < .001). Among them, statistically significant differences in hemorrhage and uterine resection rate were observed in every 2 groups (P < .05).
These results suggested that self-made ultrasonic scoring system remained an effective diagnostic tool for assessing the types of placenta accreta, and predicted the associated bleeding risk, indicating the possibility of hysterectomy.
Keywords: placenta accreta, prognosis prediction, prospective study, ultrasonic scoring system
With the commencement of the 2-children policy in China, the number of people acquiring pregnancy again after cesarean section has increased significantly, which subsequently increased the incidence of placenta accreta. The main risks included are fatal postpartum hemorrhage and high hysterectomy rates in women of reproductive age. The risk of bleeding during operation and hysterectomy was high for increta/percreta. Placenta accreta is mainly diagnosed using ultrasonography or magnetic resonance imaging, but these lack the prediction of the prognosis of placenta accreta, leading to severe hemorrhage and even maternal death due to inadequate preoperative evaluation. On the contrary, few hospitals are afraid of such type of disease due to the involvement of lot of blood preparation and abdominal aorta balloon hemostasis, but in fact not all patients with placenta accreta is extremely dangerous. This in turn leads to increased waste of medical resources including blood products, and increased risk of complications caused by unnecessary invasive operations. In recent years, several such events have occurred in succession where doctors after opening the abdomen found bulged blood vessels on the uterine surface and did not dare to continue or to complete the operation. The doctors took the direct closed abdomen, leaving the fetus still in the womb of pregnant women, and then referred the patient to the general hospital under anesthesia. This brings serious harm to the mother as well as the fetus. So, it is urgent for clinicians to predict the severity of placenta accreta before operation in order to prepare for the perioperative period and to minimize the risks of placenta accreta without wasting too much medical resources. However, the existing ultrasound technology can only diagnose placenta accreta, but due to its low sensitivity it is far from the needs of clinicians. The interpretation of ultrasonic images remained subjective. How to reduce the deviation that is caused by subjectivity and further quantification of the results of image reading predicts more directly the type of accreta and the prognosis from the images that remains a problem needs to be explored. Hence, a model that can predict the prognosis of placenta accreta by ultrasound examination, and to solve the above clinical problems is required.
At present, we have applied for international patents for “A method of processing B ultrasonic image and its device.” The invention relates to a noninvasive inspection information system, especially before the operation. This method includes the following steps: obtain data acquisition for ≥1 including the location of placenta, placental thickness, continuity of the clear space, bladder line, placental lacunae, condition of the subplacental vascularity, cervical morphology in cervical sinus, and calculate the score according to the predefined subscale. After that, deal with the data, output, and classify the placenta accordingly. Patent application number: PCT/CN2016/105842.
1. Introduction
Placenta accreta is a serious life-threatening obstetrical complication that refers to the penetration of placental villi into the uterine muscle layer to reach the uterine serous layer. It can either involve the bladder or rectum under serious conditions. According to the placental depth in the uterine muscle, placenta accreta is divided into the following 3 types: placenta accreta, placenta increta, and placenta percreta.[1] The major adverse outcomes include the high rate of hysterectomy and fatal postpartum hemorrhage among women of childbearing age, resulting in maternal and fetal death.[2,3] The total incidence of perinatal hysterectomy was reported to be 0.24% to 8.7%, and 43% of these were due to uterine atony and 73.3% were due to placenta accreta.[2] The incidence of placenta accreta has raised from 1:4027[4] in 1970's to 1:2510 in 1980's,[5] and currently it was evident in approximately 1:533 births.[4]
Ultrasound remains the major prenatal diagnostic method for placenta accreta. This increased the recognition of placenta accreta and continuously improved the diagnostic techniques, with increased sensitivity. The detection rate in the 1990s was only 1.9% to 62.5%.[6] In recent years, the sensitivity of ultrasound in diagnosing placenta accreta was 87% to 95%, specificity was 76% to 98%, and its positive predictive value was 82% to 93%.[6–11] Different types of placenta accreta involve different clinical treatment methods, and the perinatal outcomes remain very different. For patients with placental increta/percreta, the average quantity of blood loss during emergency surgery was 8600 mL,[12] and hence these patients need multidisciplinary consultation perioperatively including anesthesia and vascular surgery from the departments of general surgery, urology, pediatrics, and gynecologic oncology. We also need to prepare enough blood for the possibility of hysterectomy. However, for patients with adherent placenta, bleeding is often <1000 mL, and placenta can be delivered completely with no special treatment during the perioperative period in most of the patients. Therefore, we need ultrasound not only for diagnosing placenta accreta, but also to predict the type of placenta accreta, which can be more targeted to guide clinical work. However, few studies have addressed this need, including 2 relevant foreign studies. Cali et al[13] conducted a prospective study on 187 patients with pregnancy complicated by placenta previa after cesarean. The study screened for early placenta accreta based on 5 criteria of ultrasound, which included loss/irregularity of the echolucent area between the uterus and the placenta (“clear space”), thinning or interruption of the hyperechoic interface between the uterine serosa and the bladder wall, and the presence of turbulent with high-velocity flow, the hypervascularity of the uterine serosa–bladder wall interface and irregular intraplacental vascularization. Patients who met >2 criteria were considered to have severe placenta accreta (increta/percreta), making the final evaluation criteria by clinical outcomes and surgical pathology. Finally, 41 cases were confirmed to have placenta accreta by operation, while 146 cases did not have. All patients with placenta accreta had at least 2 of the 5 ultrasound signs mentioned above. The study also reported that ultrasound can be used to distinguish accreta or increta/percreta of the placenta. It was suggested that ultrasound demonstrated high positive and negative predictive values, and the accreta type could be evaluated to select the timing of termination and predict the intraoperative blood loss. In this paper, we tried to use ultrasound to predict the outcomes. Although the indicators were not new, it remains a pioneer study in the prediction of implantation types. Also, it lacks objectivity when used clinically, and presents inconvenience to the operation practically.
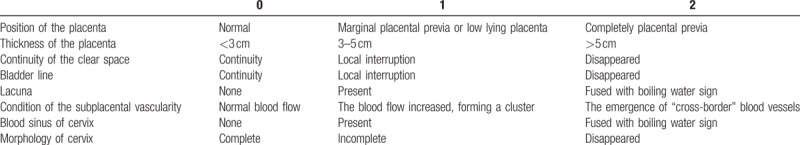
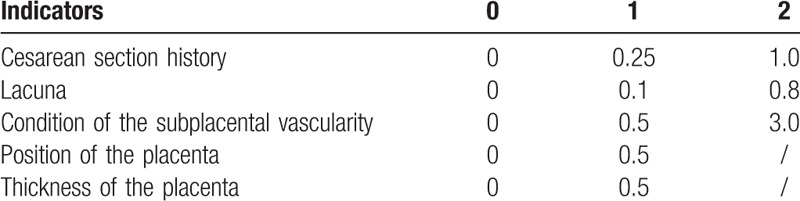
Another study by Chalubinski et al[9] monitored 232 patients with high-risk factors of placenta accreta by ultrasound over 10 years. Results revealed the types of placenta accreta according to the occurrence and severity of the signs of placenta accreta by ultrasound. Forty patients were predicted to have placenta accreta. Of these, 35 cases were clinically confirmed with placenta accreta, 7 cases with increta, and 17 cases with percreta. Its sensitivity was 91.4%, and specificity was 95.9%. Because none of the patients with increta/percreta were misdiagnosed as normal or accreta, they concluded that ultrasound had a high accuracy in the evaluation of the morbidly adherent placental types. These studies suggested that ultrasound can be used to diagnose placenta accreta, but also to distinguish the types of morbidly adherent placenta (accreta, increta, and percreta). However, they did not assess the prediction of intraoperative bleeding risk (including uterine resection rate and intraoperative blood loss), making it difficult to use due to the lack of objective criteria for interpretation. Yiwen Chong of the Third Hospital of Peking University designed the “placenta accreta scoring system” (Table 1) and confirmed that the scoring system has a certain value in predicting the type of morbidly adherent placenta, the quantity of bleeding during operation, and the rate of hysterectomy by retrospectively analyzing the imaging and clinical data of 180 placenta accreta patients and proposed the predictive value of ultrasound for placenta accreta.
Table 1.
Placenta accreta scoring system.
2. Methods
2.1. Sources of patients
From January 2015 to October 2016, 137 patients who met the following conditions in the Obstetrics Department of the Third Hospital of Peking University were prospectively studied: suspected with prenatal placenta accreta (the majority of whom were the patients with previous cesarean and placenta previa and the other patients were placenta previa with >2 times abortions); assessed by ultrasound scoring system before delivery; and delivered in the Third Hospital of Peking University. Patients with ≥1 of the following criteria were excluded: patients diagnosed as abnormal during early pregnancy were terminated; patients who have high risk complications, but her clinical data were incomplete; and pregnancy not terminated in our hospital. The study has been approved by the hospital ethics committee, and the committee approval number is 2015–155–2. All patients were informed regarding the relevant matters before study initiation. Patients voluntarily entered the study and signed the informed consent form.
2.2. Study design
We designed the “placenta accreta scoring system” (Table 1) and confirmed its feasibility in the prediction of placenta accreta by retrospectively analyzing 180 cases diagnosed with placenta accreta in the Third Hospital of Peking University from January 2005 to November 2014. We collected their clinical data and ultrasound images and scored them using the scoring system. There are 9 scoring items in this form, and among them, continuity of clear space, bladder line, lacuna, condition of subplacental vascularity are recognized as indicators for diagnosing placenta accreta in the literature. Based on our experience, placental position, placental thickness, blood sinus of cervix, and cervix morphology are formulated as indicators. In addition, history of cesarean section also remains essential for diagnosing placenta accreta, and so the 9 items were rated as 0, 1, and 2 according to the severity, while the total scores reflect the severity of placental accreta. Clinical observation revealed that patients with increta and percreta often have a blood loss >2000 mL, and the degree of danger was significantly higher than that of accreta. Therefore, we call these 2 types of patients as “severe placenta accrete.” The scores of these 3 types were compared in Table 2.
Table 2.
Three groups of patients with ultrasound score.
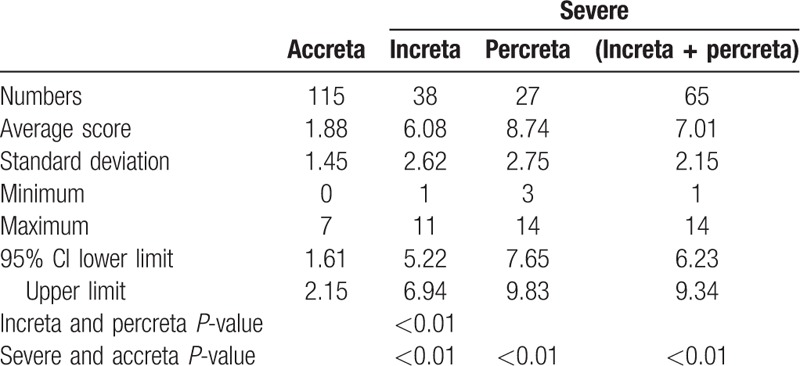
Receiver operating characteristic (ROC) curves were used to calculate the critical values of the patients in each group. According to the ROC curves, when the area under the curve was 94.3% and the score was ≥4.5, the sensitivity and specificity were 81.5% and 95.7%, respectively and therefore, the boundary value of accreta and increta/percreta was 5 (Fig. 1). When the area under the curve was 74.6% and the score was ≥9.5, the sensitivity and specificity were 55.6% and 89.5%, respectively and therefore, the boundary value of increta and percreta was 10 (Fig. 2).
Figure 1.
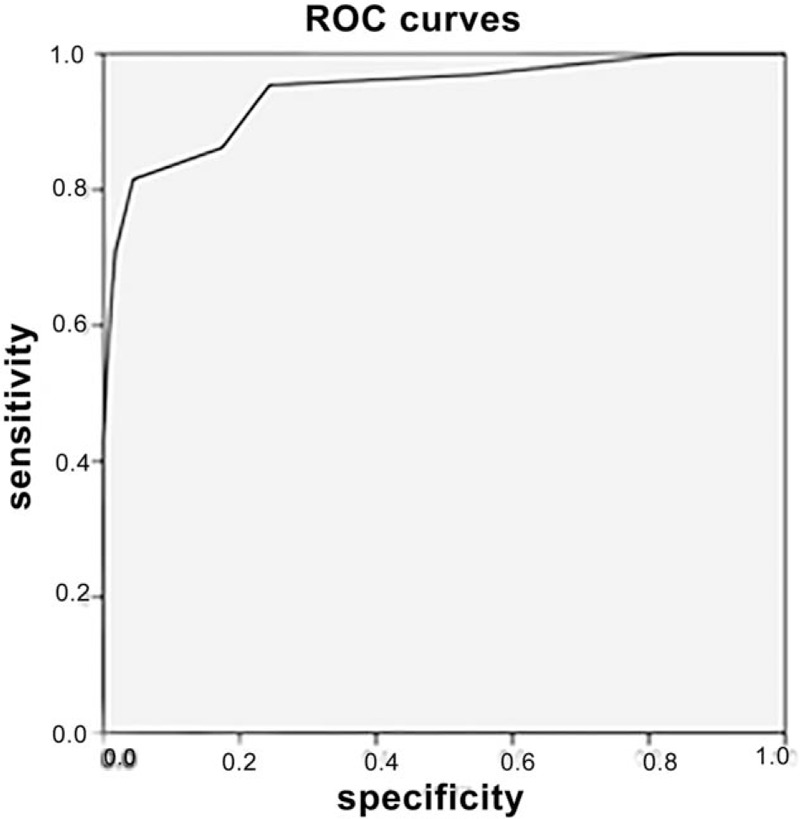
Placenta accreta and severe ROC curves. ROC = receiver operating characteristic.
Figure 2.
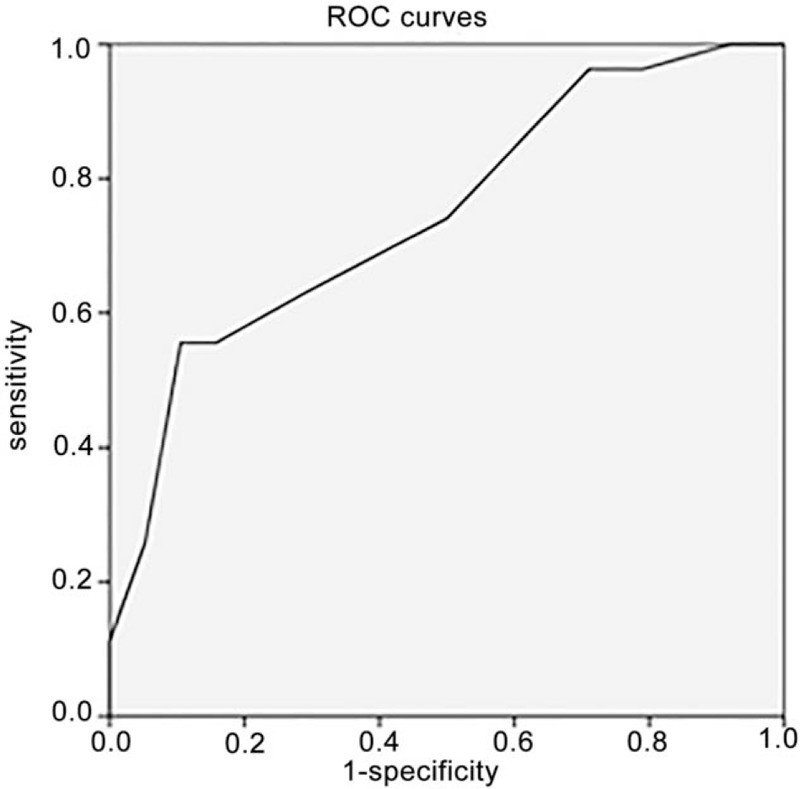
Placenta increta and percreta ROC curves. ROC = receiver operating characteristic.
To further verify the feasibility of this model, we designed the following prospective study. Hence, we defined a score of ≤5 as N1 group, which predicted that the patients would neither not haveplacenta accreta nor have only accreta type. A score of ≥6 and ≤9 was defined as N2 group, which predicted the patients with placenta increta. Finally, a score of ≥10 was defined as N3 group, which predicted that patients would have placenta percreta. We sought to confirm the value of ultrasonic scoring system in the prediction of the degree of risk of placenta accreta in a prospective study in order to guide the perioperative treatment of placenta accreta (Figs. 3–9).
Figure 3.
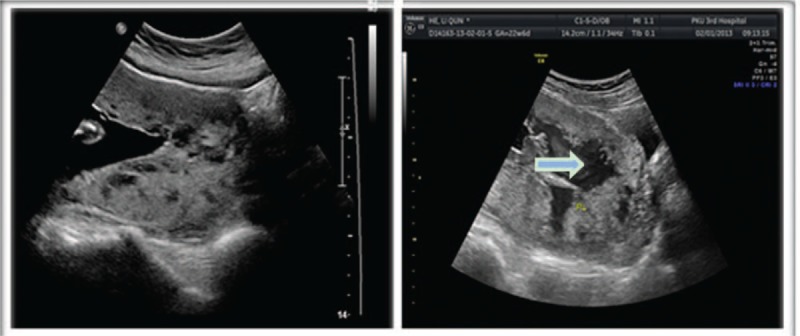
The white arrow was shown as the “boiling water sign” in the placenta. The two-dimensional ultrasound showed boiling water in it, which was actually the blood flow.
Figure 9.
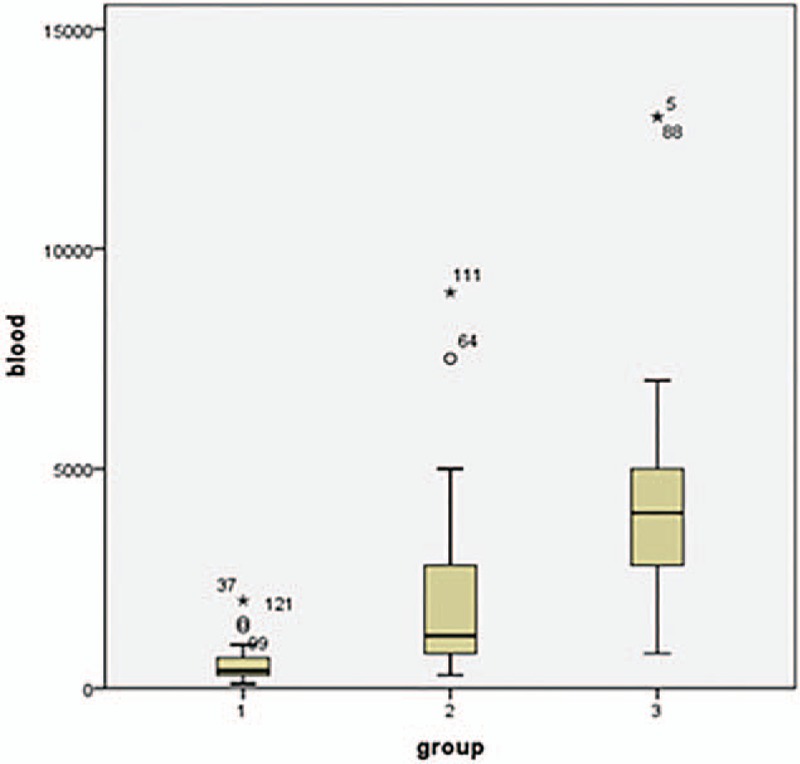
Box diagram representation of bleeding volume in the 3 groups of patients.
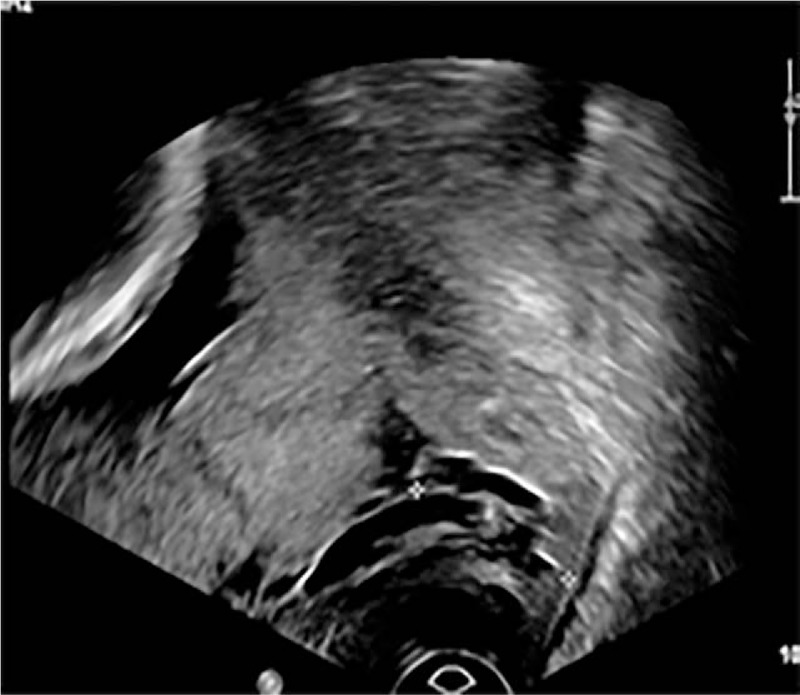
Figure 4.
The white arrow shows the interruption of clear space.
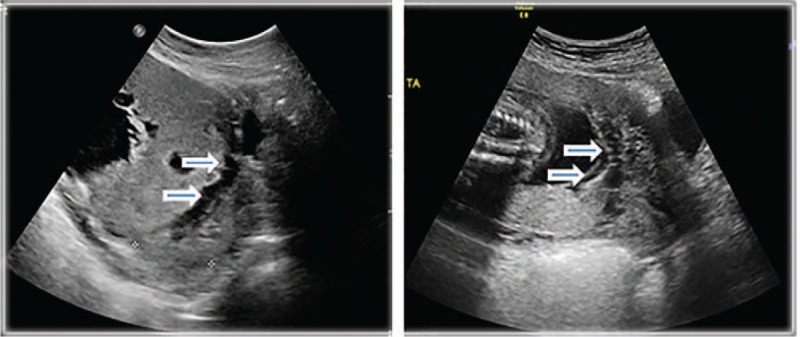
Figure 5.
The arrow head was described as bladder line, and shown discontinuity in bladder line.
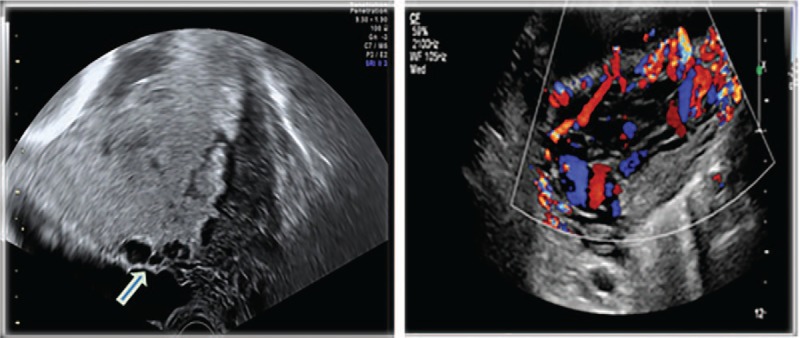
Figure 6.
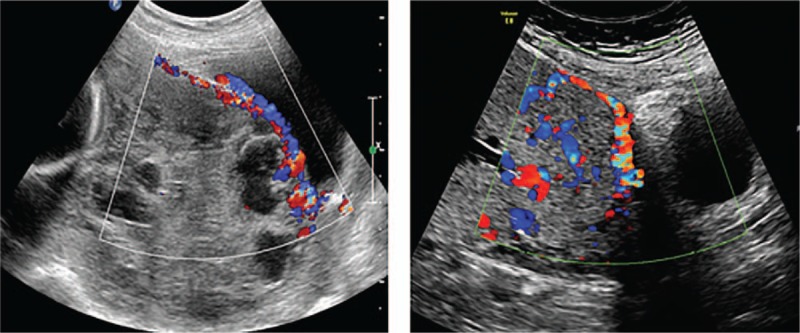
Increased blood flow in the basement of the placenta, and a “transboundary” blood vessel.
Figure 7.
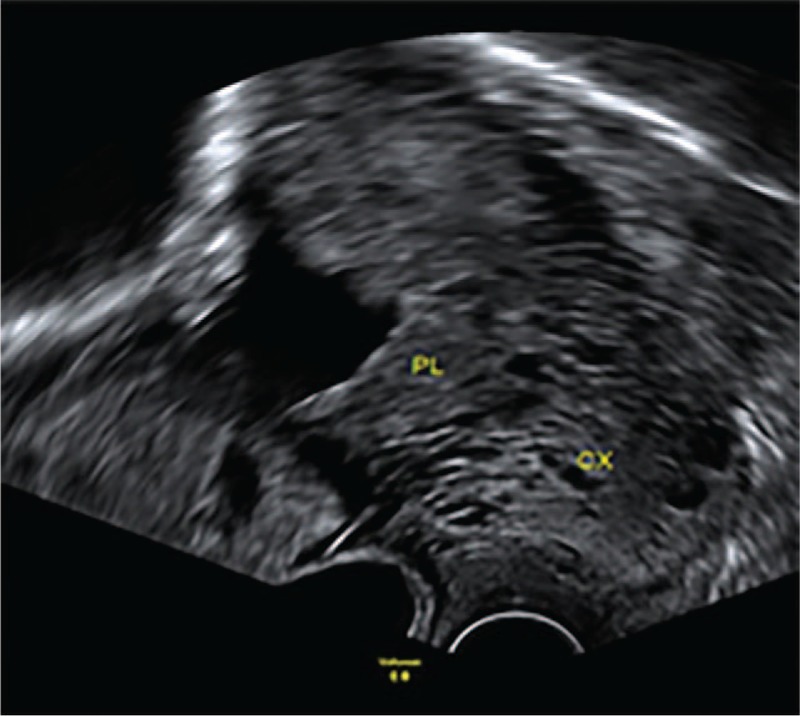
Cervical blood sinus.
Figure 8.
Incomplete cervical morphology.
The above patients were examined by ultrasound at 11 to 13 weeks add 6 days, 20 to 24 weeks, 28 to 32 weeks, 34 to 36 weeks, and 1 week before delivery, and scored according to the scoring system presented in Table 1. The color Doppler ultrasound—Philips Iu22 (made by Philips Ultrasound, Inc. in Bothell Everett Highway Bothell, WA) and GE Volusion E8 (made by GE Healthcare Austra Gmbh in Tiefenbach 15, 4871 Zipf, Germany) were used for examination. The probe frequency was 3.5 Hz. As a routine position, patients were initially placed in the supine position and lateral position when necessary. The bladder was moderately filled before the examination. We took the placental images by longitudinal, transverse, or crown scanning approach, and paid attention to the placental position, placental thickness, the clear space continuity, the bladder line continuity, the relationship between the posterior wall of the bladder and the anterior wall of the uterus, whether placental lacunae were present, and whether a boiling water sign was present in the lacunae. We observed the cervix and the lower uterine segment, and paid attention to the integrity of the cervical morphology and its internal as well as peripheral blood flow. We gave each of the above items a score of 0, 1, or 2 points according to their severity. Prior cesarean section added 1 point, and >2 prior cesarean sections added 2 points. Based on this, we calculated the total score. All ultrasonic physicians received unified training and evaluation before examination of placental accreta scoring, and only after the evaluation is passed it can do the examination. We compared the results from different doctors on ultrasound “back to back,” and the consistency reached to 0.701.
We divided the patients into 3 groups. We defined a score of ≤5 as N1 group, which predicted that the patients would neither not have placenta accreta nor have only accreta type. A score of ≥6 and ≤9 was defined as N2 group, which predicted the patients with placenta increta. Finally, a score of ≥10 was defined as N3 group, which predicted that patients would have placenta percreta. As the degree of placental accreta changes during pregnancy, the final evaluation criteria are based on the last ultrasound score that is performed before delivery. The final type of accreta is clearly diagnosed according to the patient's birth and intraoperative clinical conditions. This pathological type can be added to the diagnosis, but does not remain a necessary diagnostic method. For patients with hysterectomy, pathological examination of the myometrium with the placental tissue after the operation was set to make clear evaluation regarding the depth of the accreta.
2.3. Clinical data collection and examination method
A total of 137 patients with suspected placenta accreta were followed up. We collected their prenatal ultrasound images and clinical data including age, number of deliveries, number of cesarean sections, whether the patient has placenta previa or not, gestational age, intraoperative blood loss, whether the patient had undergone hysterectomy, etc. The type of accreta on what was seen during the operation was considered as the final criterion. If pathological examination was performed, then diagnosis can be combined with pathology.
2.4. Statistical methods
Statistical analysis was calculated by using SPSS18.0 (made in IBM, NY).
The measurement data that conform to the normal distribution was expressed by ( ). Analysis of variance was performed among the groups to compare the uterine resection rate. Measurement data of non-normal distribution were expressed by M (min–max), rank sum test was used for comparison among the groups, and the quantity of bleeding during the operation in the 3 groups was compared. Count data were expressed in frequency and rate, and compared using X2 test. ROC curve was used to calculate each type of scoring boundary value.
). Analysis of variance was performed among the groups to compare the uterine resection rate. Measurement data of non-normal distribution were expressed by M (min–max), rank sum test was used for comparison among the groups, and the quantity of bleeding during the operation in the 3 groups was compared. Count data were expressed in frequency and rate, and compared using X2 test. ROC curve was used to calculate each type of scoring boundary value.
P < .05 was considered to be statistically significant. The accuracy and Kappa values of the 3 groups of patients were calculated, and compared whether there were differences in the amount of bleeding during the operation and hysterectomy rate among the 3 groups.
3. Results
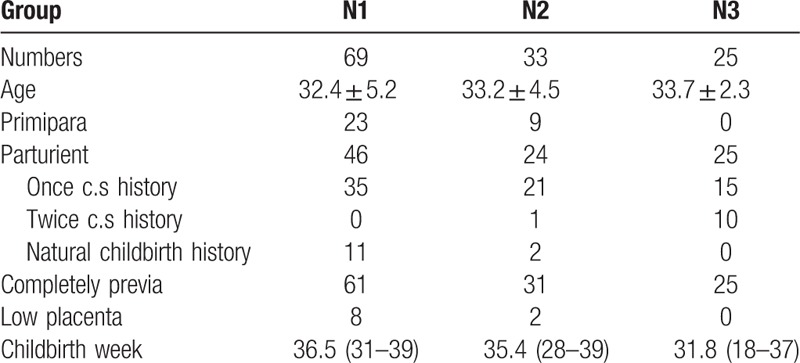
A total of 69 patients were included in N1 group with a score ≤5; 33 patients were included in N2 group with a score of ≥6 and ≤9; and 25 patients in N3 group with a score of ≥10. All patients underwent complete prenatal placental ultrasonic imaging. We scanned the placenta by longitudinal, transverse, or crown cut approach, including the image of the lower cervical segment and cervix. We scored every patient according to the scoring system presented in Table 1, and collected their clinical data. The general information of the patients was presented in Table 3. Some of the typical ultrasound signs are shown in charts 3 to 8.
Table 3.
General information.
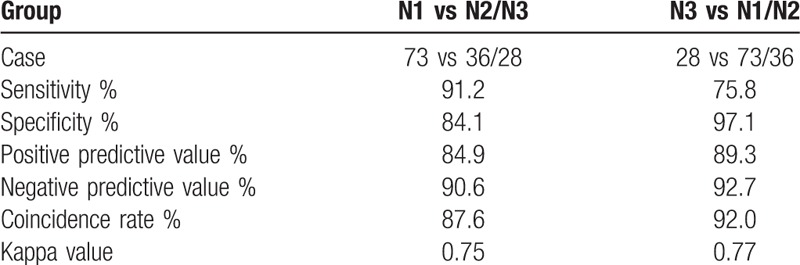
3.1. Prediction of the 3 groups with pathological type
Of the 137 patients, 68 were accreta, 36 were increta, and 33 were percreta type, as confirmed by operation and pathology. The prognosis of patients in group N1 was shown in Table 4. Patients in group N1 were predicted to have no accreta/accreta type, and 62 cases of these were consistent with the actual pathological results, while 8 cases in N2/N3 group had no accreta/accrete type. The prognosis of patients in group N1 was shown in Table 5. In N3 group, 28 patients had scores ≥10, and they were predicted to have percreta type. Of these, 25 cases were consistent with the actual pathological results, while 3 cases in N1/N2 group had percreta type. The prediction accuracy of each group was shown in Table 6.
Table 4.
N1 versus N2/N3 group.
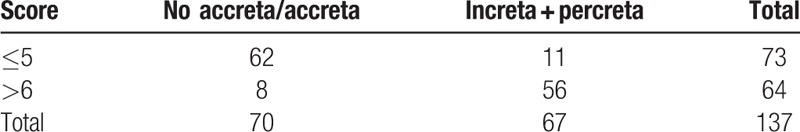
Table 5.
N3 versus N1/N2 group.
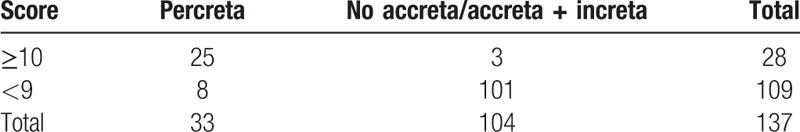
Table 6.
Pathological prediction of 3 groups of patients.
3.2. The quantity of bleeding during the operation in the 3 groups
Blood loss during operation was compared among the 3 groups by rank sum test. Differences of P < .001 was considered to be significant. Results showed differences in the intraoperative blood loss among the 3 groups. The median quantities of hemorrhage during the operation in the 3 groups were 400[100,2000] mL, 1200[300,9000] mL, and 4000[800,13,000] mL, respectively. Comparison of N1/N2 showed P < .001; N1/N3 showed P < .001; and N2/N3 showed P = .007. P < .05 was found for all values, showing statistically significant differences. There were significant differences in the quantity of bleeding between each pair of groups. The quantity of bleeding in the 3 groups was shown in chart 9.
3.3. The uterine resection rate in 3 groups
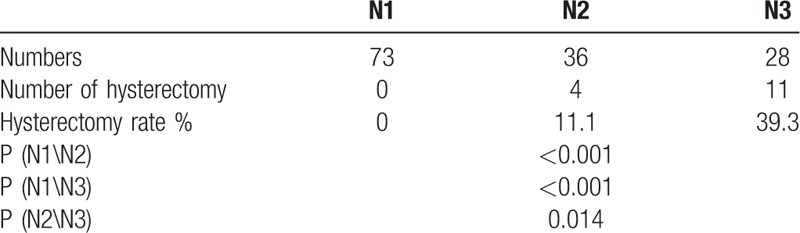
We compared the uterine resection rate in the 3 groups using Chi squared test, and demonstrated statistically significant differences (P < .001) among the 3 groups. Comparison of N1/N2 (P < .001), N1/N3 (P < .001), and N2/N3 (P = .014) showed statistically significant differences among the groups. There were significant differences in the uterine resection rate among each pair of group. Hysterectomy rate of the 3 groups of patients was shown in Table 7.
Table 7.
Hysterectomy rate in 3 groups.
Of the 73 patients in group N1, 62 were predicted accurately and 11 were predicted wrongly. The 11 patients were analyzed as follows: 8 patients with a score of 5 had actually increta type with a bleeding volume of 700 to 1000 mL during operation, and all had preserved the uterus. Two cases scored 4 points, where 1 case scored 3 points was actually increta type, with a bleeding volume of 800 to 1000 mL, and all have preserved the uterus. Of the 36 patients in group N2, 25 were predicted accurately and 11 were wrongly predicted. The 11 patients were analyzed as follows: 6 patients with score of 6 were actually accreta type, their bleeding volume was 300 to 1500 mL, and all have preserved the uterus. Five patients with a score of 8 to 9 were actually percreta type, with an intraoperative bleeding of 800 to 7500 mL, and 1 patient underwent hysterectomy. Among the 28 patients in group N3, 25 cases were accurately predicted, 3 cases were wrongly predicted. All the wrong patients with 10 to 11 scores were increta type, and the amount of bleeding during operation was 800 to 3500 mL, and preserved the uterus.
4. Discussion
4.1. Analysis for prediction results
Chong et al of the third hospital of Peking university designed the “placenta accreta scoring system” and used this model to predict the type of placenta accreta, intraoperative blood loss, and hysterectomy rate. Results proved that the model has a certain predictive value by conducting a retrospective analysis of imaging and clinical data of 180 placenta accreta patients. On this basis, we conducted a prospective study to further verify the feasibility of this model.
The study indicated that the accuracy of the scoring system for predicting the pathologic types of placenta accreta as 83.9% to 92%, demonstrating a relatively high accuracy. Most of the mispredicted cases had scores closer to the critical value. The error rate in N2 group was slightly higher and the coincidence rate remained the lowest because it was adjacent to N1 and N3 groups. Despite the errors in predicting pathological types, intraoperative bleeding and hysterectomy in these mispredicted cases were basically consistent with the predictions. Patients with misprediction in group N1 showed blood loss of <1000 mL and preserved the uterus. In group N2, 6 patients with low scores had blood loss of <1500 mL, and preserved the uterus, and 5 patients with higher scores had larger blood loss, and 1 of them underwent hysterectomy. Three patients in group N3 demonstrated a larger amount of blood. Regardless of their actual pathological type, the 3 groups of patients showed significant differences in the quantity of bleeding and hysterectomy rate.
4.2. Application of ultrasound scoring system in the prediction of placenta accreta
The above-mentioned data showed that we can rely on the scoring system for predicting the type of accreta and the degree of risk. According to different scoring levels, a customized follow-up and treatment options for patients can be made. It demonstrated a great clinical significance for the timing of termination of pregnancy, preoperative preparation, selection of surgical methods, and organization of experienced teams. This in turn avoided insufficient or excessive waste of blood preparation, reducing the potential maternal and children morbidity and mortality.[14] Evidences suggested that preoperative diagnosis of placental accreta can decrease intraoperative blood loss and blood transfusion in patients.[15,16]
For example, we can organize an experienced team, including the departments of obstetrics, pediatrics, urology, vascular surgery, anesthesiology and laboratory doctors to perform corresponding treatment measures and blood preparation, reducing the potential for maternal morbidity and mortality. According to our experience, a patient with a score of ≤5 points should undergo repeat ultrasound examination every 3 to 4 weeks before delivery and try to deliver after 37 weeks, depending on whether the patients had vaginal bleeding, abdominal pain, and other symptoms. If there was no other method of delivery for patients with prior cesarean section (e.g., scarred uterus, placenta previa), they can choose to undergo vaginal delivery. For this, we should prepare 2 units of red blood cells before delivery without consultation from other departments. With scores of ≥6 and ≤9, ultrasound examination should be performed every 2 to 3 weeks before delivery and try to deliver between 35 and 36 weeks according to the patient's symptoms. C-section is the most preferred method, for which we should make sure to set 6 units of red blood cells and plasma before the delivery and consult the department of urology. Additionally, cystoscopy and stent placement should be performed before undergoing the operation if any. With a score of ≥10, a repeat ultrasound examination should be performed every 1 to 2 weeks before delivery and try to deliver between 33 and 34 weeks according to the patient's symptoms. Cesarean section should be the preferred method, where 25 units of red blood cells, plasma, and coagulation factor should be set before the operation. The departments of urology, vascular surgery, and ICU should be called for consultation before performing the operation. During the operation, cystoscopy, stent placement, femoral artery isolation, and preparations to place an abdominal aorta balloon and hysterectomy can be performed. In this study, a prenatal ultrasound model was established to predict the severity of placenta accreta, and there were only few reports regarding this topic. Accurate preoperative evaluation of accreta types, prediction of intraoperative bleeding risk, targeted completion of preoperative preparation were of great significance in the reduction of the incidence of fatal postpartum hemorrhage, the rate of hysterectomy in young pregnant women, maternal mortality, avoid the wastage of blood, and reduce the economic burden.
4.3. Advantages and limitations of research
This study further verified the clinical application value of the model through prospective studies. The prediction accuracy of this model was high, which opened the way for the prediction of placenta accreta. But there are some limitations to this study: the sample size was relatively small, this was a single-center study, and this model was relatively complex. Therefore, simplification of the scoring items in this model by logistic regression was necessary to screen out the items that have a more differentiated effect on accreta/severe placental accreta to facilitate the primary hospitals for referral. Currently, we are conducting this research and have got some initial results. Of the 9 previously listed indicators, the following 5 have been selected by nomogram to distinguish between accreta and severe placental accreta only, including position of the placenta, thickness of the placenta, lacuna, condition of the subplacental vascularity, and cesarean section history. Figure 10 and Table 8 present the above data. In Table 8, the numbers are the weights of the indications, and which the placental position was divided into 0 and 1 points according to whether it was a complete placenta previa, and the placental thickness was divided into 0 and 1 points by the boundary of 5 cm. This is still an undergoing study, and we look forward to a simpler and more effective model.
Figure 10.
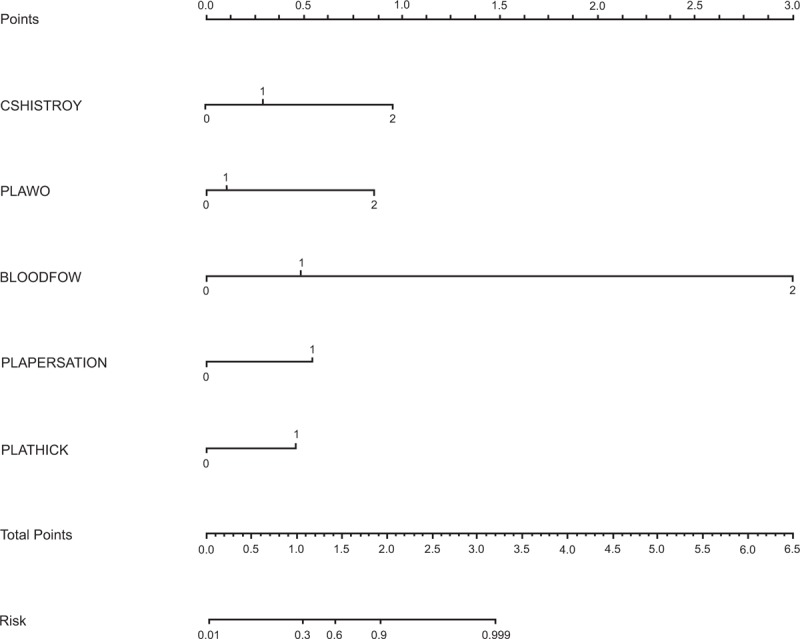
Nomogram of indicators used to distinguish between accreta and severe placenta accreta.
Table 8.
Weighted coefficient of indicators used to distinguish between accreta and severe placenta accreta.
5. Conclusions and prospects
The model of “placenta accreta scoring system” can be used to evaluate the type of accreta before operation, predict the risk of intraoperative bleeding, and has a certain significance in the reduction rate of fatal postpartum hemorrhage, hysterectomy rate of young women, and maternal mortality. These subsequently make a reasonable preoperative preparation and avoidance of waste of blood, and reduce the economic burden of patients and countries. In the future, we hope to use the simple and easy-to-operate ultrasound scoring system to guide junior hospitals in performing a timely referral, reduce maternal mortality, and ensure maternal and fetal health.
Acknowledgments
First of all, the authors would like to express their heartfelt thanks to their tutor, professor Zhao Yangyu. From the initial topic selection to the collection of data to the final paper writing, including the design of the subject, these are inseparable from professor Zhao's help and guidance. Secondly, thanks to the department of obstetrics and gynecology ultrasound and obstetrics teachers, help them to complete the collection of ultrasound images and clinical data, Finally, they would like to thank the teachers of the epidemiology research center for their guidance and assistance in writing papers and statistical analysis.
Author contributions
Investigation: Yan Wang.
Methodology: Aiqing Zhang.
Project administration: Yunshan Chen.
Writing – original draft: Yiwen Chong.
Writing – review & editing: Yangyu Zhao.
Footnotes
Abbreviations: PA = placenta accreta, PASS = placenta accreta scoring system.
The study was supported by the special clinical application research (Z131107002213089) and the capital health development research project (2016-1-4091).
The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this study.
References
- [1].Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol 1997;177:210–4. [DOI] [PubMed] [Google Scholar]
- [2].Machado LS. Emergency peripartum hysterectomy: incidence, indications, risk factors and outcome. N Am J Med Sci 2011;3:358–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Angstmann T, Gard G, Harrington T, et al. Surgical management of placenta accreta: a cohort series and suggested approach. Am J Obstet Gynecol 2010;202:38.e1–9. [DOI] [PubMed] [Google Scholar]
- [4].Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol 2005;192:1458–61. [DOI] [PubMed] [Google Scholar]
- [5].Read JA, Cotton DB, Miller FC. Placenta accreta: changing clinical aspects and outcome. Obstet Gynecol 1980;56:31–4. [PubMed] [Google Scholar]
- [6].Gielchinsky Y, Rojansky N, Fasouliotis SJ, et al. Placenta accreta–summary of 10 years: a survey of 310 cases. Placenta 2002;23:210–4. [DOI] [PubMed] [Google Scholar]
- [7].Palacios Jaraquemada JM, Bruno CH. Accuracy of ultrasonography and magnetic resonance imaging in the diagnosis of placenta accreta. Obstet Gynecol 2007;109:203author reply 203. [DOI] [PubMed] [Google Scholar]
- [8].Shih JC, Palacios Jaraquemada JM, Su YN, et al. Role of three-dimensional power Doppler in the antenatal diagnosis of placenta accreta: comparison with gray-scale and color Doppler techniques. Ultrasound Obstet Gynecol 2009;33:193–203. [DOI] [PubMed] [Google Scholar]
- [9].Chalubinski KM, Pils S, Klein K, et al. Prenatal sonography can predict degree of placental invasion. Ultrasound Obstet Gynecol 2013;42:518–24. [DOI] [PubMed] [Google Scholar]
- [10].Chou MM, Ho ES, Lee YH. Prenatal diagnosis of placenta previa accreta by transabdominal color Doppler ultrasound. Ultrasound Obstet Gynecol 2000;15:28–35. [DOI] [PubMed] [Google Scholar]
- [11].Riteau AS, Tassin M, Chambon G, et al. Accuracy of ultrasonography and magnetic resonance imaging in the diagnosis of placenta accreta. PLoS One 2014;9:e94866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Sumigama S, Itakura A, Ota T, et al. Placenta previa increta/percreta in Japan: a retrospective study of ultrasound findings, management and clinical course. J Obstet Gynaecol Res 2007;33:606–11. [DOI] [PubMed] [Google Scholar]
- [13].Cali G, Giambanco L, Puccio G, et al. Morbidly adherent placenta: evaluation of ultrasound diagnostic criteria and differentiation of placenta accreta from percreta. Ultrasound Obstet Gynecol 2013;41:406–12. [DOI] [PubMed] [Google Scholar]
- [14].Committee on Obstetric Practice. Committee opinion no. 529: placenta accrete. Obstet Gynecol 2012;120:207–11. [DOI] [PubMed] [Google Scholar]
- [15].D’Antonio F, Bhide A. Ultrasound in placental disorders. Best Pract Res Clin Obstet Gynaecol 2014;28:429–42. [DOI] [PubMed] [Google Scholar]
- [16].Tikkanen M, Paavonen J, Loukovaara M, et al. Antenatal diagnosis of placenta accreta leads to reduced blood loss. Acta Obstet Gynecol Scand 2011;90:1140–6. [DOI] [PubMed] [Google Scholar]


