Abstract
The functions and clinical consequences of the fabella, a sesamoid bone found in the posterolateral aspect of the knee joint, are still a reason of intense debate in the scientific literature. Its incidence was reported to range between 20% and 87% and its presence was usually associated with the persistent pain in the posterolateral region of the knee. The aim of our study was to measure the prevalence, anatomic and clinical features of the fabella within a cross-sectional study, conducted in a Romanian orthopaedic center. Between 2015 and 2017, a consecutive series of 562 patients with knee injuries or persistent knee pain has been examined by radiographs and Magnetic Resonance Imaging and a set of anatomical and clinical parameters have been recorded. Collected data was evaluated with RadiANT DICOM Viewer and statistically analyzed with GraphPad Prism 7. The level of significance was set at P <.05. The incidence of the fabella in our study group was 16.93%, lower than previously reported for Caucasian populations. We found statistically significant differences regarding the possible association of the fabella with pain in the posterolateral corner of the knee (P = .04) and the 2 dimensions of the bone according to gender (P = .03 respectively P = .01), but the prevalence was not influenced by gender (P = .6). The anatomic characteristics could be important in differentiating this sesamoid bone from calcifications or loose bodies located in the knee joint region. Due to the high association with the posterolateral knee pain, the fabella should be recorded during knee examination as a differential diagnosis, before any surgical procedure.
Keywords: fabella, fabella syndrome, posterolateral knee pain, sesamoid bone
1. Introduction
The posterolateral corner (PLC) of the knee is a region with complex anatomy which was considered by many clinicians the dark side of the knee, due to the lack of understanding regarding its structures, biomechanics and treatment options.[1] The sesamoid bones found in this area, represented by patella, fabella, and cyamella (located within the popliteal tendon) raised more interest in recent years, due to their association with pathologic conditions such as fractures, dislocations, osteomyelitis, septic arthritis, osteoarthritis and even bone tumors.[2] The functions of these bones are to modify pressure, to diminish friction thereby to protect the tendons, to change the direction of a muscle pull and to assist muscle actions. The fabella is considered to be a normal anatomic variant, usually detected in routine lateral knee radiographs, which is sometimes confused with intra-articular loose bodies or osteophytes, especially in osteoarthritic knees and intra-meniscal calcifications. The development of the fabella begins as cartilaginous nodule and progressively undergoes enchondral ossification.[3] The association between local mechanical stress, locomotion, and muscular contraction might affect genetic factors that modulate the metaplasia of developing tissues, being responsible for larger dimensions of this sesamoid bone.[4,5] The association with the fabellofibular ligament, which is formed by the thickening of the distal part of the short head of the biceps femoris tendon, proves the role of the fabella in the stabilization of the posterolateral structures of the knee. It can also represent a source of pain and it is specifically considered responsible for discomfort in the PLC of the knee, known as fabella syndrome, a condition of extreme importance in orthopedic surgery and clinical routine.[6] Up to date there is little information in the scientific literature upon the prevalence of the fabella in various ethnic populations.[7] Few studies coming from Asia reported a prevalence of 66% to 68.6% in elderly Japanese patients and 31.25% in a Chinese population.[8,9] As there is no data in the literature regarding the prevalence of the fabella in the Romanian population, the purpose of our study was to examine, based on radiographic and Magnetic Resonance Imaging (MRI) films, the presence of the fabella and its anatomic features according to gender and its association with pain in the PLC of the knee in patients under 45 years of age. The null hypothesis to be tested is that there is no difference regarding the anatomic characteristics between genders and the presence of fabella has no influence on the occurrence of pain in the PLC of the knee in young patients.
2. Methods
2.1. Study design and patients
The medical records of a consecutive series of 562 patients who presented to the Clinic of Orthopaedics and Traumatology II Tirgu Mures had been examined between May 2015 and October 2017. The research protocol was conducted in accordance with the Declaration of Helsinki, within an appropriate ethical methodology; from each patient, a written informed consent was obtained which allowed us to use the medical data for scientific publication. In the study group patients under 45 years of age, with knee pathologies that required knee arthroscopy had been included. As exclusion criteria, we selected the radiographic and MRI findings of ligament and meniscus injuries in the PLC, loose bodies, synovitis, synovial tumors, and severe osteoarthritis. The age was also considered exclusion criteria, because increasing age is accompanied by ectopic ossification and increase in fabella dimensions.
2.2. Radiological and clinical examination
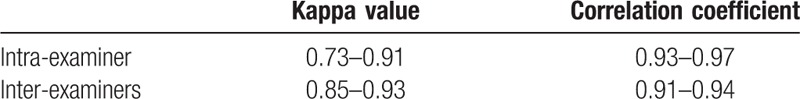
The identification of fabella was based on both radiographic and MRI films. (Fig. 1) However, for assessing the size of the bone, MRI films were exclusively used. Two specialists measured twice the length and width as the largest diameters on 2 perpendicular axes on sagittal view and in uncertain cases, the final decision was reached by consensus. For this analysis, RadiAnt DICOM Viewer (version 4.2.1. for Windows, Medixant, Poland) was used. (Fig. 2 and Fig. 3) In order to eliminate possible sources of bias related to the individual diagnosis and measurements, intra-observer and inter-observer validity were estimated using the intra-class correlation and Kappa coefficients.
Figure 1.
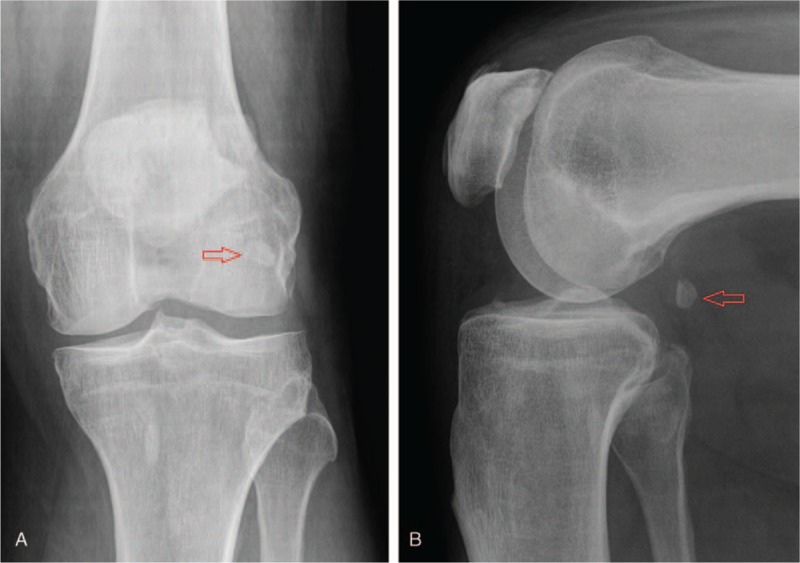
A. Anteroposterior incidence of a radiographic film, showing the presence of fabella (arrow) behind the posterolateral femoral condyle. B. On lateral incidence the fabella (arrow) is aligned with the articular space in knee flexion. Male patient, 42 years, left knee.
Figure 2.
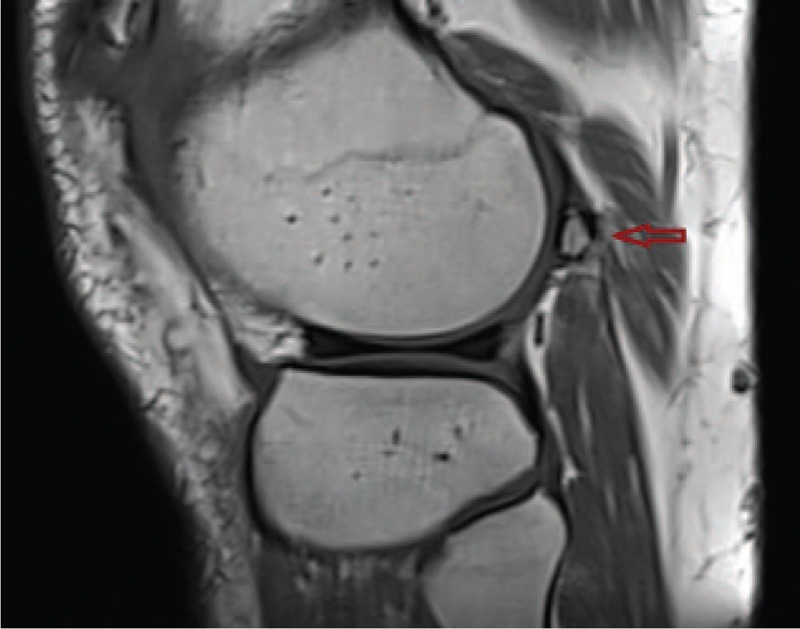
The sagittal section of the MRI film from the same patient confirms the proximity of the fabella (arrow) to the posterolateral femoral condyle. MRI = magnetic resonance imaging.
Figure 3.
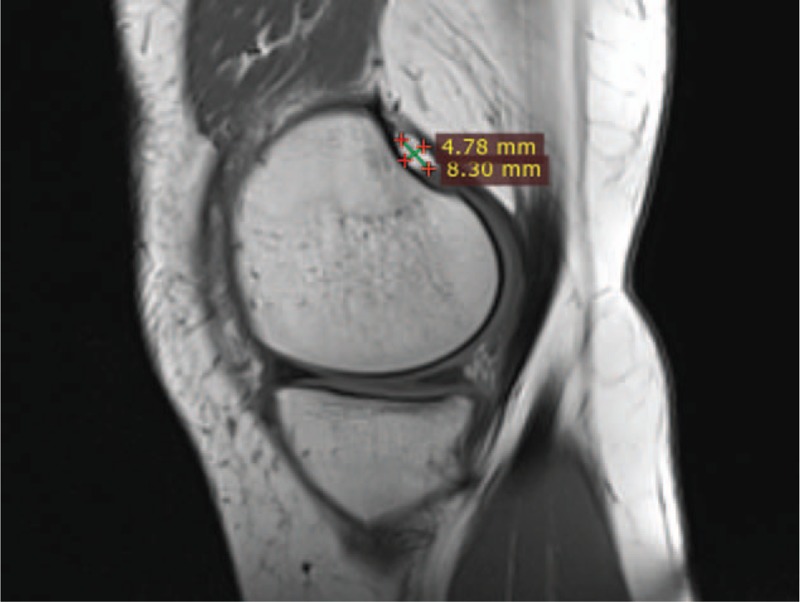
Measurements of the fabella on a sagittal section of the MRI film from the left knee of a female patient, suggesting the presence of an articular facet with the posterolateral femoral condyle. MRI = magnetic resonance imaging.
The pain in the PLC of the knee was evaluated based on the following clinical aspects: click sound and/or crepitation during knee flexion and extension, pain with active flexion, which could be reproduced by palpation of the lateral head of the gastrocnemius muscle.
2.3. Statistical analysis
Statistical analysis of all recorded data was accomplished with GraphPad Prism 7 for Windows (GraphPad Software, CA), using Fisher exact test and Welch t test. The continuous variables were presented as mean ± standard deviation (SD) and categorical variables as percentages and frequency distribution. The level of statistical significance was set at a value of P <.05 (2-tailed).
3. Results
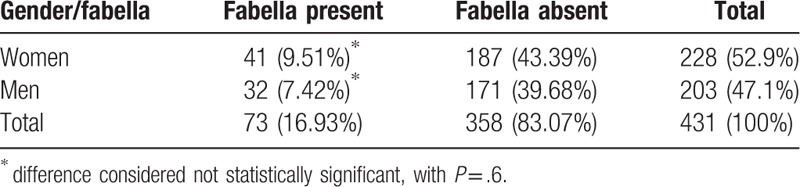
After the exclusion criteria were applied, 431 patients were evaluated, 228 women and 203 men aged between 21 and 43 years (36.8 ± 4.19). The fabella was identified in 73 cases corresponding to an overall prevalence of 16.93%. The distribution of the fabella within the study group according to gender is presented in a contingency table (Table 1). The sesamoid bone was identified in 41 women (17.98% of 228 female patients, 9.51% of the entire study group) and in 32 men (15.76% of 203 male patients, 7.42% of the entire study group). According to Fisher's exact test, the 2-sided P value is .6 which is not significant. The calculated odds ratio of 1.172 (0.7132–1.972), with 95% confidence interval, shows that there is no causal relationship between gender and the presence of the fabella.
Table 1.
The distribution of fabella within the study group according to gender.
The correlation between the presence of the fabella and pain in the PLC of the knee is presented in Table 2. The concomitant presence of fabella and pain was noticed in 46 cases (20.54% of 224 patients with pain, 10.67% of the entire study group). The Fisher exact test reported a 2-sided P value of .04 considered statistically significant; the odds ratio was 1.723 (1.038–2.903) with 95% confidence interval. The calculated parameters show that the patients with fabella had higher odds of experiencing pain in the PLC of the knee, compared with patients without fabella.
Table 2.
The association between the presence of the fabella and the occurrence of posterolateral knee pain.

We measured the mean and standard deviation of the fabella dimensions in millimeters (mm) according to gender: in men, the length had a mean value of 8.82 mm ± 0.44 SD and a mean width of 5.02 mm ± 0.73 SD. For the female patients, we calculated a mean length of 8.62 mm ± 0.35 and a mean width of 4.65 ± 0.29 SD. For the entire group, the mean length was 8.71 mm ± 0.41 SD and the mean width 4.81 mm ± 0.56 SD. The comparison of size distribution according to gender was assessed using the unpaired t-test, Welch corrected, which confirmed a statistically significant difference with a value of P = .03 for length and P = .01 for width (Table 3). The intra-class correlation coefficient and Kappa values confirmed that the measurements of the fabella were reliable, without significant differences between the 2 observers (Table 4).
Table 3.
The distribution of fabella dimensions according to gender.
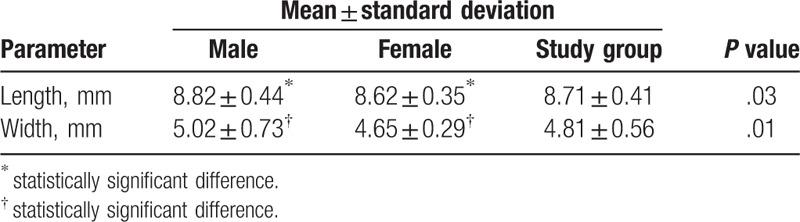
Table 4.
Reliability of the measurements performed by the 2 examiners.
4. Discussion
The location of the fabella, at the terminal part of the tendon of gastrocnemius muscle, the arcuate ligament and the oblique popliteal and fabellofibular ligaments, represents a point of confluent forces. Most of the studies place this sesamoid bone on the lateral head of the gastrocnemius muscle, but some reports found it in the medial head.[10,11] The differentiation between osseous fabella and ectopic calcifications or intra-articular loose bodies was best achieved on lateral radiographs, which show the intra-tendinous and fixed position of this bone during knee dynamic examination.[12] MRI is considered the gold standard for the investigation of the internal architecture of the knee. It allows an improved visualization of small structures and avoidance of over-investigation and misdiagnosis.[13] The irregular appearance of fabella may be confused with foreign body and MRI helps to locate it within the muscle. The structures that belong to the lateral aspect of the knee can be examined with routine spin-echo magnetic resonance imaging sequences, using sagittal, coronal and axial planes. The studies that measured the prevalence of the fabella in different ethnic groups used radiographs, MRI or cadaver dissection and showed great variability, as values ranged between 9% and 31% for western populations to 66% and 86% measured in Asian ethnics.[4,14]
Our study was based on radiographic and MRI examination, in order to detect both bony and cartilaginous fabellae. We measured an overall prevalence of 16.93% with no significant differences between genders which are in accordance to previous reported data of 10% to 30% for most European countries.[6,10] In their anatomical study on cadavers, Kawashima et al[4] found a prevalence of 66% in Japanese population, most of the fabellae and their surrounding structures being in contact with the lateral femoral condyle with which a small articular cavity was formed. A similar investigation was conducted by Chew et al[9] in a Chinese population, reporting a prevalence of 31.25%. They found that 52% of the fabellae had an articulating facet, associated with the increased dimensions but not with the distance between the fabella and its insertion on the lateral head of the gastrocnemius muscle. The reason for a higher prevalence in Asian countries was thought to originate from the daily routine of these populations in which kneeling is more frequent.[15]
Previously reported data considered that the fabella might have variable size, increasing in patients with osteoarthritis, with a length that can reach 22 mm and a mean of 15 mm, the larger dimensions being recorded in male patients, which supported the idea that it has a biomechanical function. In patients without osteoarthritis the length of the fabella was reported to have a mean of 8 mm ± 3 mm and a width of 5 mm ± 2 mm.[7,9] We measured mean values of 8.71 mm length and 4.81 mm width for the entire study group, with slightly higher values reported in male patients, which proved to be statistically significant. This is in contradiction with the study of Chew et al,[9] that found no association between gender and fabella dimensions. Even though we examined a suitable sized sample for statistical analysis, in order to draw a clear conclusion, more investigations are required on a larger population.
The fabella syndrome is defined as a condition resulting in pain in the PLC of the knee, which increases in full extension. According to Zipple et al,[16] possible mechanisms of pain in fabella syndrome include compression on adjacent structures such as fabellofibular ligament, gastrocnemius tendon, femoral condyle, posterior capsule, and common fibular nerve. The fabella syndrome is characterized by the presence of pain due to mechanical irritation of local soft tissues during knee extension, as the pressure of fabella causes tension on the lateral femoral condyle.[17] This syndrome is diagnosed based on a combination of clinical and physical examination, radiography, ultrasound, radionucleotide scanning, and MRI. Pain syndromes that may mimic this condition include primary pathologic conditions of the knee, like gout, occult fractures, bursitis, and tendinitis. Patients with knee pain secondary to fabella report tenderness and pain in the PLC of the knee and a grating sensation during knee motion.[18,19]
In our study, the association between the presence of fabella and pain in PLC was considered statistically significant based on the measured P value and odds ratio. However, in order to strength this observation, a cohort study would be appropriate, which may certify the causal relationship. For the statistical analysis, we used the Fisher exact test which is more suitable in evaluating study groups less than 500 participants, compared to chi-square test, more suitable for larger samples. Pritchett et al[20] proposed that the presence of the fabella increases the risk of knee osteoarthritis. It may lead to peroneal nerve compression due to their close anatomical association in the PLC of the knee. In addition, Ando[21] reported popliteal artery compression induced by the fabella. The PLC of the knee has a complex arrangements of tendons, ligaments, and muscles, extremely important during physiological functions. The untreated lesions and as a consequence, the insufficient support of the posterior knee prolongs the healing process and may cause postsurgical failure after cruciate ligament reconstruction.[22] Injuries of the cruciate ligament may mask secondary posterolateral pathology which may remain unrecognized. Although the presence or absence of fabella is accepted as a normal variant, the specialists should have a thorough knowledge of the anatomical characteristics and frequency of the fabella in the population they practice. The presence of fabella needs to be kept in mind during knee examination and any surgical procedures and should be included as one of the differential diagnosis in posterolateral knee pain.
4.1. Strengths and limitations
The methodology of a cross-sectional study allowed a quick and inexpensive examination of the prevalence of the fabella in a clinic-based sample, useful before planning a cohort study. Even though it is the first study to address the number of symptomatic fabella in a young population without osteoarthritis, a limitation of our research protocol is that we could not have a follow-up of the cases with concomitant presence of fabella and posterolateral knee pain, regarding the development of osteoarthritis or enlargement of fabella dimensions.
Author contributions
Conceptualization: Tudor Sorin Pop, Peter Olah, Cristian Trambitas.
Data curation: Tudor Sorin Pop, Cristian Trambitas.
Formal analysis: Anca Maria Pop, Peter Olah.
Investigation: Tudor Sorin Pop, Anca Maria Pop, Cristian Trambitas.
Methodology: Tudor Sorin Pop, Peter Olah, Cristian Trambitas.
Resources: Anca Maria Pop.
Software: Anca Maria Pop, Peter Olah.
Supervision: Tudor Sorin Pop, Cristian Trambitas.
Validation: Tudor Sorin Pop, Peter Olah, Cristian Trambitas.
Writing – original draft: Tudor Sorin Pop, Anca Maria Pop.
Writing – review & editing: Tudor Sorin Pop, Anca Maria Pop, Cristian Trambitas.
Footnotes
Abbreviations: DICOM = digital imaging and communications in medicine, MRI = magnetic resonance imaging, PLC = posterolateral corner, SD = standard deviation.
The authors have no conflicts of interest to disclose.
References
- [1].Chahla J, Moatshe G, Dean CS, et al. Posterolateral corner of the knee: current concepts. Arch Bone Jt Surg 2016;4:97–103. [PMC free article] [PubMed] [Google Scholar]
- [2].Singh J, James SL, Kroon HM, et al. Tumor and tumor-like lesions of the patella—a multicenter experiment. Eur Radiol 2009;19:701–12. [DOI] [PubMed] [Google Scholar]
- [3].Sarin VK, Erickson GM, Giori NJ, et al. Coincident development of sesamoid bones and clues to their evolution. Anat Rec 1999;257:174–80. [DOI] [PubMed] [Google Scholar]
- [4].Kawashima T, Takeishi H, Yoshitoni S, et al. Anatomical study of the fabella, fabellar complex and its clinical implications. Surg Radiol Anat 2007;29:611–6. [DOI] [PubMed] [Google Scholar]
- [5].Franceschi F, Longo VG, Ruzzini L, et al. Dislocation of an enlarged fabella as uncommon cause of knee pain: a case report. Knee 2007;14:330–2. [DOI] [PubMed] [Google Scholar]
- [6].Driessen A, Balke M, Offerhans C, et al. The fabella syndrome—a rare case of posterolateral knee pain: a review of the literature and two case reports. BMC Muskuloskelet Disord 2014;15:100–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hauser NH, Hoechel S, Toranelli M, Klaws J, Muller-Gerbl M. Functional and structural details about the Fabella: what the important stabilizer looks like in the central European population. BioMed Research International. Vol. 2015, Article ID. 343728. 8 pages. 2015. 10.1155/2015/343728 Accessed on March 26, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Tabira Y, Saga T, Takahashi N, et al. Influence of the fabella in the gastrocnemius muscle on the common fibular nerve in Japanese subjects. Clin Anat 2013;26:893–902. [DOI] [PubMed] [Google Scholar]
- [9].Chew CP, Lee KH, Koh JS, et al. Incidence and radiological characteristics of fabellae in an Asian population. Singapore Med J 2014;55:198–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Egerci OF, Kose O, Turan A, et al. Prevalence and distribution of the fabella: a radiographis study in Turkish subjects. Folia Morphol 2017;76:478–83. [DOI] [PubMed] [Google Scholar]
- [11].Raheem O, Philpott J, Ryan W, et al. Anatomical variations in the anatomy of the postero-lateral corner of the knee. Knee Surg Sports Traumatol Arthrosc 2007;15:895–900. [DOI] [PubMed] [Google Scholar]
- [12].Zhou F, Zhang F, Deng G, et al. Fabella fracture with radiological imaging: a case report. Trauma Case Rep 2017;12:19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Tyler P, Datir A, Saifuddin A. Magnetic resonance imaging of anatomical variations in the knee. Part 1: ligamentous and musculotendinous. Skeletal Radiol 2010;39:1161–73. [DOI] [PubMed] [Google Scholar]
- [14].Phukubye P, Oyedele O. The incidence and structure of the fabella in a South African cadaver sample. Clin Anat 2011;24:84–90. [DOI] [PubMed] [Google Scholar]
- [15].Zeng SX, Dong XL, Dang RS, et al. Anatomic study of the fabella and its surrounding structures in a chinese population. Surg Radiol Anat 2012;34:65–71. [DOI] [PubMed] [Google Scholar]
- [16].Zipple JT, Hammer RL, Loubert PV. Treatment of fabella syndrome with manual therapy: a case report. J Orthop Sports Phys Ther 2003;33:33–9. [DOI] [PubMed] [Google Scholar]
- [17].Okono E, Yoshyoka T, Yanai T, et al. Fabella syndrome as an uncommon cause of posterolateral pain after total knee arthroplasty: a case report and review of the literature. Case Rep Orthop 2016;2016: Article ID 4328462, 5 pages, 10.1155/2016/4328462. Accessed March 24, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kim T, Chung H, Lee H, et al. A case report and literature review on fabella syndrome after high tibial osteotomy. Medicine 2018;97:4Available at: 10.1097/MD.0000000000009585. Accessed March 9, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Merolla G, Dave AC, Paladini P, et al. Ossifying tendinitis of the rotator cuff after arthroscopic excision of calcium deposits: report of two cases and literature review. J Orthop Traumatol 2015;16:67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Pritchett JW. The incidence of fabella in osteoarthrosis of the knee. J Bone Joint Surg Am 1984;66:1379–80. [PubMed] [Google Scholar]
- [21].Ando Y, Miyamoto Y, Tokimura F, et al. A case report on a very rare variant of popliteal artery entrapment syndrome due to an enlarged fabella associated with severe knee osteoarthritis. J Orthop Sci 2017;22:164–8. [DOI] [PubMed] [Google Scholar]
- [22].Ehara S. Potentially symptomatic fabella: MR imaging review. Japanese J of Radiol 2014;32:1–5. [DOI] [PubMed] [Google Scholar]


