Supplemental Digital Content is available in the text
Keywords: meta-analysis, motivation, oral hygiene, orthodontic, systematic review
Abstract
Objective:
The aim of our study was to qualitatively and quantitatively synthesize the evidence regarding ways to improve motivation of oral hygiene among orthodontic patients with fixed appliances and identify the effects of motivational methods via comparing the oral hygiene condition before and after the motivations.
Methods:
An electronic search was conducted in PubMed, Ovid, Embase, and the Crochrane Library for relevant random controlled trials (RCT) and clinical controlled trial (CCT) published before May 1st, 2017 with manual search in addition. Search and selection of studies, quality assessment, data extraction and synthesis was completed by 2 reviewers independently. Plaque index (PI) and gingival index (GI) at 1, 3, 6-month were pooled with Review Manager 5.3. Bias of included studies was evaluated.
Results:
In total, 12 studies fulfilled the inclusion criteria of this systematic review, of which, 5 were included in the meta-analysis. Motivational methods had statistically significant advantage regarding PI in the experimental group over control group at 1, 3, 6-month, while GI was significantly better controlled in the study group at 3, 6-month. The quality of included studies was moderate.
Conclusion:
It is worthy for orthodontists to put in additional efforts to motivate patients to maintain good oral hygiene throughout the entire treatment process.
1. Introduction
During orthodontic treatment, fixed braces severely impede tooth brushing and thus create a favorable condition for plaque to rapidly adhere and accumulate.[1,2] The greater tooth surface area covered with brackets and the more complex appliance components used, the harder it gets for patients to appropriately clean their teeth.[3,4] As a result, enamel demineralization and gingivitis have been regarded as the most prevalent consequences of biofilm formation among orthodontic patients, affecting 50% to 70% of patients with fixed appliances.[5,6] Studies have shown that poor oral hygiene might prolong treatment duration and even jeopardize treatment outcomes.[2,6,7] Even worse, the progression of gingivitis lesions to periodontal diseases might lead to irreversible loss of supporting tissues.[8] These undesired potential side effects could lead to unsatisfactory results or even premature termination of orthodontic therapy. Scholars evaluated that 5% to 10% of orthodontic patients failed to complete their treatment because of oral hygiene issues.[9]
In general, clinicians provide routine oral hygiene instruction (OHI) to orthodontic patients but the efficacy of OHI might be limited.[5,6] Therefore, patients’ motivation plays a crucial and decisive role in maintaining favored oral hygiene. To date, hopefully, an increasing number of studies have focused on how orthodontists can motivate their patients on oral health, with extra motivational efforts made despite routine OHI.
However, these studies largely differ in terms of content, design, and duration and resulting in conflicting conclusions. Higgins and Green[10] had published a systematic review on interactions to improve adherence among orthodontic patients where they included oral hygiene as one of the 4 aspects of adherence. However, they involved only 4 articles published before March 1st, 2012 and had no quantitative synthesize. Therefore, the aim of our study was to qualitatively and quantitatively synthesize the evidence regarding ways to improve motivation of oral hygiene among orthodontic patients with fixed appliances and identify the effects of motivational methods.
2. Methods
This meta-analysis was carried out in accordance with Cochrane Handbook for Systematic Reviews of Interventions[11] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).[12] This work had not registered before it was conducted.
2.1. Literature search strategy
Studies on improving motivation on dental hygiene of orthodontic patients were searched in PubMed, Ovid, Embase, and the Cochrane Library. Moreover, additional relevant studies were obtained via manual searches and the reference lists of related articles. The last search conducted was at May 1st, 2017. The search strategy was formed for each database showed in Affiliated Table 1, with the example of PubMed as follows: (((oral health [MeSH Terms]) OR oral hygiene [MeSH Terms]) AND orthodontics [MeSH Terms]) AND (motivation∗ OR compliance OR adherence).
2.2. Inclusion and exclusion criteria
Based on the principles of participants; intervention; comparison; outcome; study design (PICOS), our inclusion criteria were as follows: random controlled trials (RCT) or clinical controlled trial (CCT) in patients with fixed orthodontic appliances; motivational methods were applied to improve patients’ motivation and compliance of oral hygiene; comparison was made between different motivational methods or between motivational group and control group; and availability of outcome of plaque accumulation or gingival status before and after motivation.
The exclusion criteria were as follows: recruitment of patients with removable appliances; no motivational methods were applied; reports of outcomes that did not illustrate oral health status; review, case report, letter, or conference paper; articles with no English abstract available.
2.3. Primary and secondary outcomes
Plaque index (PI) and gingival index (GI) were collected as primary outcomes. Bleeding index and white spots were collected as secondary outcomes.
2.4. Study selection
Two review authors (JH and YXY) individualistically screened the titles and abstract of search results to select potential relevant studies. After that, by reading the full-text of potential researches, the 2 reviewers independently selected the articles which met the inclusion criteria. A third reviewer (CYL) was consulted whenever there was any doubt about the eligibility of articles. The reviewers had contacted the authors of the included articles when essential for any further details of additional or unpublished results.
2.5. Bias assessment
The risk of bias of the included studies was independently evaluated by 2 review authors (JH and YXY) according to the “risk of bias” tool of Cochrane Collaboration in Chapter 8 in the Cochrane Handbook for Systematic Reviews of Information.[11] Any disagreement was solved through discussion with the third reviewer (CYL). The following aspects were assessed as at a high, low, or unclear risk of bias: random sequence generation, allocation concealment, blinding of outcome assessment, blinding of participants, incomplete outcome data, selective reporting, and other bias including but not limited at reliability testing and confounders analyzed. However, considering the nature of motivational studies, blinding of participants was almost impossible in most study design. Thus, this aspect had not been taken into account when evaluating the quality of involved articles.
After considering the additional essential details provided by the original authors of the articles, trials were classified into the following categories:
High quality (the bias was unlikely to seriously affect the results) if no aspect, except blinding of participants, was identified as unclear or at high risk.
Moderate quality (the bias would produce doubt regarding the results) if only 1 to 2 key aspects were identified to be unclear or at high risk, except blinding of participants.
Low quality (the bias would seriously weaken the confidence of the results) if >2 key aspects were identified to be unclear or at a high risk, except blinding of participants.
2.6. Data extraction
Two review authors (JH and YXY) independently extracted the data, outcomes at 1, 3, 6-month were collected, reports with other time intervals were not included in meta-analysis. Disagreement was then resolved by discussion with the third reviewer (CYL). Reviewers were not blinded to the information of included studies, including authors, interventions, and results. The original authors were contacted when any information was missed.
2.7. Data synthesis
Meta-analysis was conducted for continuous outcomes measured in the included studies with Review Manager software 5.3; Cochrane Community, London, UK. As various indices had been used to measure were regarded as the same basic item (PI or GI), mean difference (MD) combined with 95% confidence interval (CI) was used to analyze the outcomes.
Heterogeneity between researches was assessed using the Cochrane test (P < .05 was considered significant) and the I2. The I2 statistical cutoffs of 25%, 50%, and 75% were regarded as low, moderate, and high heterogeneity, respectively. Because the studies selected in the meta-analysis were conducted in different countries and populations, the between-study variations were assumed as a priori; thus, when I2 was >75%, random effect models were used indicating the results should be considered with caution, otherwise fixed effect models would be applied.
3. Results
Figure 1 presents a flow chart of study selection. Our search strategy yielded 370 records from electronic and manual search. After removal of 259 duplicates, 2 reviewers separately screened the titles and abstract of the remained 111 identical studies. Eighteen potential studies were selected to obtain the full-text for further consideration of eligibility. The kappa score of interviewers’ agreement while identifying titles and abstract was 0.95. Disagreements were resolved by consulting the third reviewer (CYL). Finally, 12 studies were included in this review while 5 studies were involved in meta-analysis, while the other 7 were not included due to the lack of available data at 1, 3, 6-month after the begin of intervention. Excluded studies were explained with reasons in affiliated Table 2.
Figure 1.
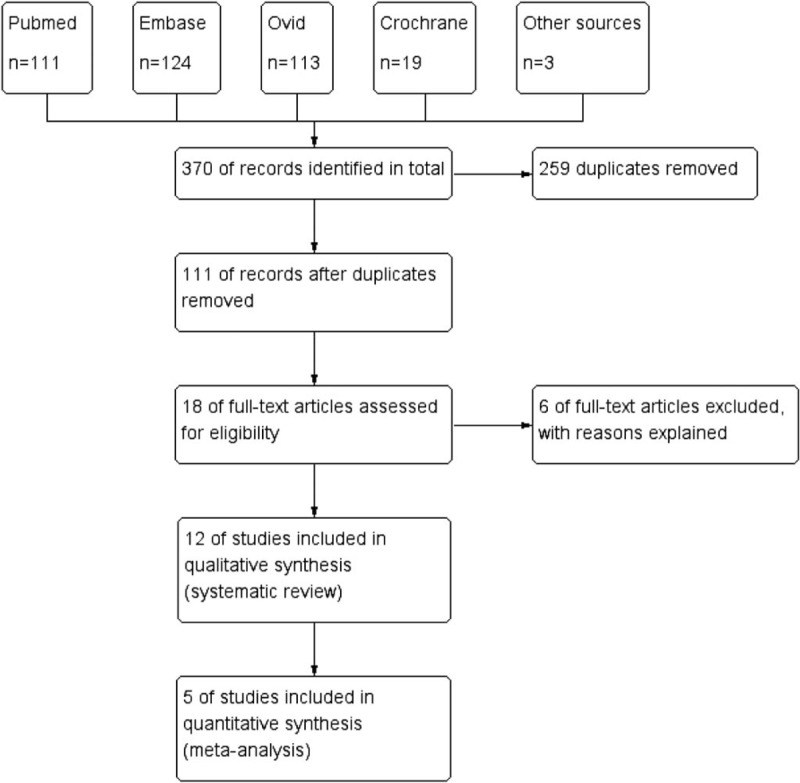
Study flow diagram. 18 articles were involved in this review, while among them, 12 were included in meta-analysis.
3.1. Characteristics of included studies
Characteristics of included studies were illustrated in Table 1 for 5 studies included in meta-analysis, and Table 2 for the other 7 studies involved in qualitative analysis. Detailed information mainly included sample features, intervention approaches, measurements, and main results.
Table 1.
Characteristics of 6 articles involved in meta-analysis.
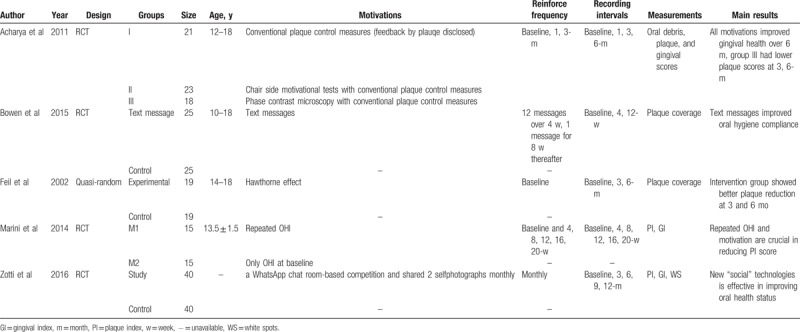
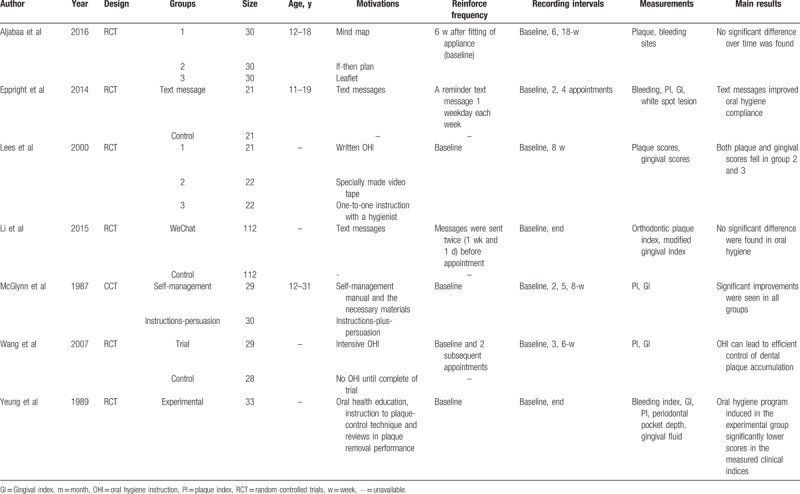
Table 2.
Characteristics of 6 articles included in systematic review but not involved in meta-analysis.
3.2. Risk of bias
As presented in Fig. 2, in the 12 studies included in systematic review, only 2 of the included studies provided high-quality evidence, 8 were unclear, and the remaining 2 had only low-quality evidence. In general, the quality of the included studies was relatively moderate.
Figure 2.
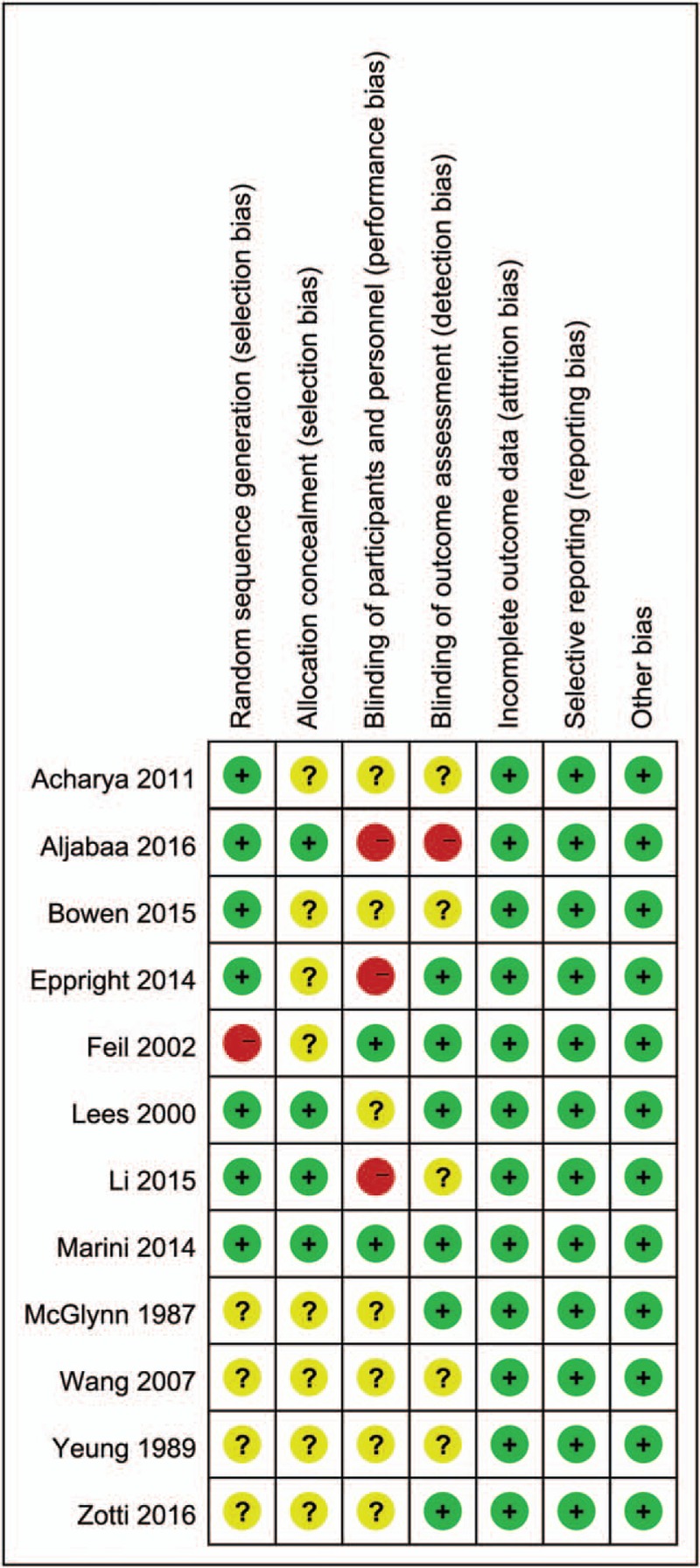
Bias assessment of 12 studies involved in systematic review.
3.3. Synthesis of data
PI and GI at 1, 3, 6-month were separately synthesized in forest plots as Figs. 3 and 4, respectively.
Figure 3.
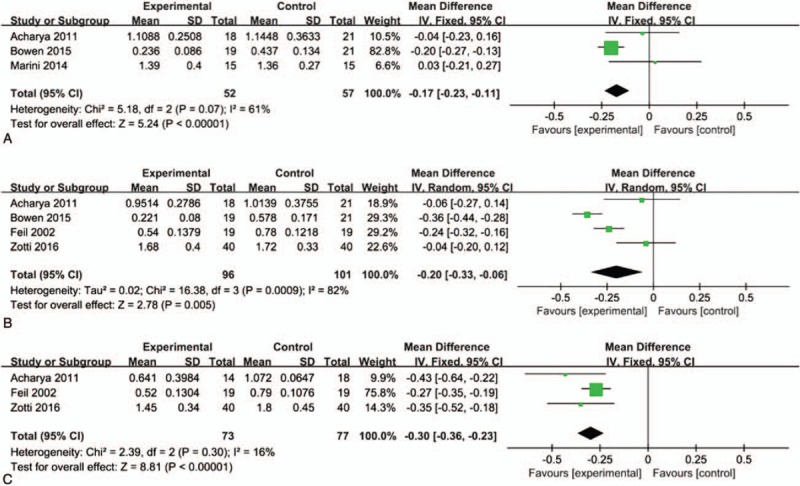
Forest plot of PI, ∗P < .05. A. 1 month, B. 3 months, C. 6 months. PI = plaque index.
Figure 4.
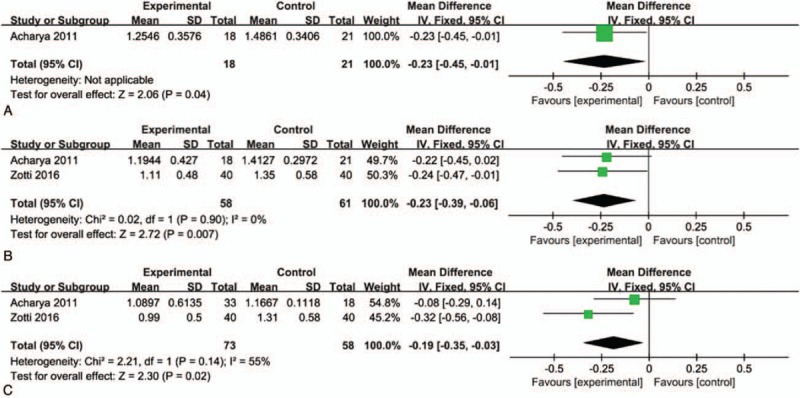
Forest plot of GI, ∗P < .05. A. 1 month, B. 3 months, C. 6 months. GI = gingival index.
For plaque index, experimental groups demonstrated significant advantage over control group at all selected time intervals, namely 1-month (MD: −0.17, 95% CI: −0.23, −0.11, P < .05), 3-month (MD: −0.20, 95% CI: −0.33, −0.06, P < .05), and 6-month (MD: −0.30, 95% CI: −0.36, −0.23, P < .05).
While in terms of gingival index, no synthesis was available at 1-month, significant difference revealed at 3-month (MD: −0.23, 95% CI: −0.39, −0.06, P < .05) and 6-month (MD: −0.19, 95% CI: −0.35, −0.03, P < .05), illustrating experimental group had better gingival condition over control group at the 2 time intervals.
Bleeding index and white lesion were unavailable to be synthesized due to limited reports.
4. Discussion
The aforementioned results demonstrated that extra efforts made by orthodontists or oral hygientists could effectively motivate orthodontic patients to enhance their oral hygiene. PI was significantly reduced in the experimental group than the control group at all 3 time intervals, while GI showed statistical advantage in study group at 3, 6-month.
Motivational approaches applied in included studies could be generally classified as chair-side education, message reminders, behavioral modification, and Hawthorne effect. Chair-side modified OHI was the most broadly used method to enhance the motivation of oral hygiene among orthodontic patients. In detail, verbal and written information, photos or catalogs, videos,[13] and visual demonstration with models or experimental equipment were used by scholars to explain the composition and mechanism of plaque formation,[14] warn the risk of poor oral hygiene, recommend brushing techniques,[15,16] and provide personalized counseling.[17] The modified and enhanced OHI were primarily performed by hygienists and orthodontist.
Despite being time-consuming, professional education required materials and equipment prepared in advance in the clinics. In spite of plaque disclosure with tablets, which was relatively easily accessed, Lalic et al[14] showed the participants color changes of dyed acid of plaque and showed live motile bacteria under microscope. These educational demonstration might not be easily taken broadly in routine orthodontic practice worldwide, due to its high cost and the limited space in clinics or hospitals especially in developing and undeveloped countries.
Besides, interactions out of clinics could make a close connection between orthodontists and their patients at the typical 4 to 6-week interval of appointments, as patients would feel that they were concerned by their orthodontists throughout the entire treatment process. In 4 included studies, the participants were motivated with message reminder. The approaches of reminder included sending short text messages to patients or their parents to emphasize the importance of good oral hygiene,[18,19] using apps to push orthodontic related messages and remind before appointments,[20] and setting a WhatsApp-based chatting room for participants to share tooth selfies.[21]
Studies have demonstrated that active reminder used in medicine and dentistry could improve appointment attendance, compliance to medication schedules, and positive behavioral changes.[20,22–24] Accompanied with the popularization of smartphones and various software, technical means including short message service and messaging apps have been broadly attempted in medical fields, particularly being helpful in patients’ education and outpatients’ management.[23] However, most smartphones have developed the function of shielding junk messages so such texts frequently sent from the clinics might be shielded by certain patients when feeling annoyed.
Compared with chair-side motivation conducted in clinic, which was supposed to be more formal and professional, daily reminder, was more like regular and automatic greetings sent from dentists. Besides, the content of reminder primarily focused on encouragement, emphasizing the advantages of clean teeth. Unlike chair-side instruction, which was relatively more serious, mainly focused on warning about unwanted outcomes of improper oral hygiene, to create a sense of being threatened if the participants did not follow the instruction.
Nevertheless, the cost of interventions performed out of clinics was much lower in terms of both price and time, and would not be limited by the space of the clinics, the number of dental chairs, or the schedule of hygienists, which could thus be more convenient to be broadly practiced among orthodontic patients.
In addition, 2 studies applied self-management of behavior to modify the habits of oral hygiene,[25,26] including self-monitoring, goal-setting, self-evaluation, and self-reward. These measurements were taken to have an effect on participants’ behavior with psychologic-related disciplinary principles. Another study offered the participants an ordinary toothpaste but labeled as “experimental,” which simulated being enrolled in a study, intentionally produced a sense of been observed for participants through Hawthorne effect.[27] All the 3 studies reported positive results in the management of oral hygiene which revealed that in spite of instruction and remind, psychologic-related approaches might also be a potential and effective way in maintaining patients’ compliance.
Several researchers have reinforced the process not only at the commencement of the study or treatment but also at subsequent visits. Seven studies had reinforcement of motivation along the treatment, 5 studies had conducted motivation only at baseline, including 3 studies which provide material to take home so actually work and reinforce daily throughout the observational period.
It was noticeable that size and observational period were relatively limited in each individual study, only 2 studies had reported the PI and GI at the end of treatment,[20,28] but the results had not been synthesized because different measurement methods led to high heterogeneity between the 2 studies.
The positive result of this meta-analysis had demonstrated the value and effect of motivation on oral hygiene. Motivation could be applied not only among orthodontic patients but also among patients with periodontal diseases or implant plans, who would probably have multiple visits to dentists and long treatment duration. On the other hand, it gave a brand-new idea for future studies in this field, because the effects of chair-side motivation in clinic, reminder sent during intervals between visits, behavioral modification and Hawthorn effects might be simultaneously conducted in an individual study, so that their efficacy could be directly compared in a single study in the future.
5. Limitations
This meta-analysis had not registered online before it was conducted. Besides only articles with English abstract had been included, this might cause bias as studies reported in other languages had not been included.
6. Conclusion
It is worthwhile for orthodontists to take additional attainments to improve dental hygiene motivation of their patients. PI revealed statistically significant advantages in the experimental groups at 1, 3, 6-month while GI improved significantly at 3, 6-month.
It is highly recommended for orthodontists to take at least one method, or ideally use a combination, to improve the oral hygiene motivation among their patients, with reinforcement along the treatment period.
Acknowledgments
The authors appreciated the help of the Department of Orthodontics of the Peking University, School of Stomatology.
Author contributions
Conceptualization: Jing Huang, Jiuhui Jiang.
Data curation: Jing Huang, Yunxia Yao, Cuiying Li.
Formal analysis: Jing Huang, Yunxia Yao, Cui-Ying Li.
Funding acquisition: Jiuhui Jiang.
Investigation: Jing Huang, Yunxia Yao, Cuiying Li.
Methodology: Jing Huang, Yunxia Yao, Cuiying Li.
Project administration: Jiuhui Jiang.
Resources: Jing Huang, Yunxia Yao, Cuiying Li.
Software: Jing Huang, Yunxia Yao, Cuiying Li.
Supervision: Cuiying Li, Jiuhui Jiang.
Validation: Jing Huang, Yunxia Yao, Cuiying Li.
Visualization: Jing Huang, Yunxia Yao, Cuiying Li.
Writing – original draft: Yunxia Yao.
Writing – review and editing: Yunxia Yao, Jiuhui Jiang.
Supplementary Material
Footnotes
Abbreviations: CCT = clinical controlled trial, CI = confidence interval, GI = gingival index, MD = mean difference, OHI = Oral hygiene instruction, PI = plaque index, PRISMA = preferred reporting items for systematic reviews and meta-analyses, RCT = random controlled trials.
JH and YY have contributed equally to this work.
Funding: There was no funding for the study.
Availability of data and materials: The dataset analyzed during the current study is included in the manuscript.
Consent for publication: Not applicable.
Ethics approval and consent to participate: Not applicable.
The authors declare that they have no competing interests.
Supplemental Digital Content is available for this article.
References
- [1].Balenseifen JW, Madonia J. Study of dental plaque in orthodontic patients. J Dent Res 1970;49:320–4. [DOI] [PubMed] [Google Scholar]
- [2].Gwinnett AJ, Ceen RF. Plaque distribution on bonded brackets: a scanning microscope study. Am J Orthod 1979;75:667–77. [DOI] [PubMed] [Google Scholar]
- [3].Mitchell L. Decalcification during orthodontic treatment with fixed appliances—an overview. Br J Orthod 1992;19:199–205. [DOI] [PubMed] [Google Scholar]
- [4].Zachrisson BU. Cause and prevention of injuries to teeth and supporting structures during orthodontic treatment. Am J Orthod 1976;69:285–300. [DOI] [PubMed] [Google Scholar]
- [5].Palomares NB, Celeste RK, de Oliveira BH, et al. How does orthodontic treatment affect young adults’ oral health-related quality of life? Am J Orthod Dentofac 2012;141:751–8. [DOI] [PubMed] [Google Scholar]
- [6].Skidmore KJ, Brook KJ, Thomson WM, et al. Factors influencing treatment time in orthodontic patients. Am J Orthod Dentofac 2006;129:230–8. [DOI] [PubMed] [Google Scholar]
- [7].Beckwith FR, Ackerman RJ, Cobb CM, et al. An evaluation of factors affecting duration of orthodontic treatment. Am J Orthod Dentofac 1999;115:439–47. [DOI] [PubMed] [Google Scholar]
- [8].Page RC, Schroeder HE. Pathogenesis of inflammatory periodontal disease. A summary of current work. Lab Invest 1976;34:235–49. [PubMed] [Google Scholar]
- [9].Mehra T, Nanda R, Sinha P. Orthodontists’ assessment and management of patient compliance. Angle Orthod 1998;68:115–22. [DOI] [PubMed] [Google Scholar]
- [10].Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from http://handbook.cochrane.org. [Google Scholar]
- [11].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Acharya S, Goyal A, Utreja AK, et al. Effect of three different motivational techniques on oral hygiene and gingival health of patients undergoing multibracketed orthodontics. Angle Orthod 2011;81:884–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ay ZY, Sayin M, Özat Y, et al. Appropriate oral hygiene motivation method for patients with fixed appliances. Angle Orthod 2007;77:1085–9. [DOI] [PubMed] [Google Scholar]
- [14].Lalic M, Aleksic E, Gajic M, et al. Does oral health counseling effectively improve oral hygiene of orthodontic patients? Eur J Paediatr Dent 2012;13:181–6. [PubMed] [Google Scholar]
- [15].Lees A, Rock W. A comparison between written, verbal, and videotape oral hygiene instruction for patients with fixed appliances. J Orthod 2000;27:323–8. [DOI] [PubMed] [Google Scholar]
- [16].Marini I, Bortolotti F, Parenti SI, et al. Combined effects of repeated oral hygiene motivation and type of toothbrush on orthodontic patients: a blind randomized clinical trial. Angle Orthod 2014;84:896–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Peng Y, Wu R, Qu W, et al. Effect of visual method vs plaque disclosure in enhancing oral hygiene in adolescents and young adults: a single-blind randomized controlled trial. Am J Orthod Dentofac 2014;145:280–6. [DOI] [PubMed] [Google Scholar]
- [18].Wang SY, Yang J, Chang HP. The effect of an oral hygiene instruction intervention on plaque control by orthodontic patients. J Dent Sci 2007;2:45–51. [Google Scholar]
- [19].Wright NS, Fleming PS, Sharma PK, et al. Influence of supplemental written information on adolescent anxiety, motivation and compliance in early orthodontic treatment. Angle Orthod 2010;80:329–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Li X, Xu ZR, Tang N, et al. Effect of intervention using a messaging app on compliance and duration of treatment in orthodontic patients. Clin Oral Investig 2016;20:1849–59. [DOI] [PubMed] [Google Scholar]
- [21].Zotti F, Dalessandri D, Salgarello S, et al. Usefulness of an app in improving oral hygiene compliance in adolescent orthodontic patients. Angle Orthod 2016;86:101–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Brent Bowen T, Rinchuse DJ, Zullo T, et al. The influence of text messaging on oral hygiene effectiveness. Angle Orthod 2014;85:543–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Eppright M, Shroff B, Best AM, et al. Influence of active reminders on oral hygiene compliance in orthodontic patients. Angle Orthod 2014;84:208–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Cozzani M, Ragazzini G, Delucchi A, et al. Oral hygiene compliance in orthodontic patients: A randomized controlled study on the effects of a post-treatment communication. Prog Orthod 2016;17:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].McGlynn FD, LeCompte EJ, Thomas RG, et al. Effects of behavioral self-management on oral hygiene adherence among orthodontic patients. Am J Orthod Dentofacial Orthop 1987;91:15–21. [DOI] [PubMed] [Google Scholar]
- [26].Aljabaa A, McDonald F, Newton JT. A systematic review of randomized controlled trials of interventions to improve adherence among orthodontic patients aged 12 to 18. Angle Orthod 2015;85:305–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Feil PH, Grauer JS, Gadbury-Amyot CC, et al. Intentional use of the hawthorne effect to improve oral hygiene compliance in orthodontic patients. J Dent Educ 2002;66:1129–35. [PubMed] [Google Scholar]
- [28].Yeung S, Howell S, Fahey P. Oral hygiene program for orthodontic patients. Am J Orthod Dentofacial Orthop 1989;96:208–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


