Abstract
Rationale:
Metastases of nonthyroid malignancies to the thyroid gland are rare, and only sporadic cases have been reported in literature. We present our experience in treating patients with metastases to the thyroid gland at Peking Union Medical College Hospital.
Patient concerns:
The clinical data of 32 patients who presented with secondary thyroid tumors were retrospectively analyzed.
Interventions:
Eleven patients (34.5%) had thyroidectomy.Two patients (6.25%) had tracheostomies to alleviate compression caused by enlarged thyroid tumors.
Outcomes:
The most common primary lesion was in the lungs (14/32), followed by the kidney (5/32) and gastrointestinal system (5/32). The interval from the diagnosis of the primary tumor to thyroid metastasis varied from 0 month to 16 years. Ten patients (31.3%) are still alive, and the longest follow-up survival time was 7 years.
Lessons:
Thyroid metastases are rare, and the lung was the most common primary site of origin. It seems that thyroidectomy has not been considered in cases with a high clinical stage of the neoplastic process such as lung cancer.
Keywords: therapy, thyroid cancer, thyroid metastases
1. Introduction
In spite of the high incidence of thyroid cancer,[1,2] metastases to the thyroid receive little attention. Metastases to the thyroid gland are uncommon, and only sporadic cases have been reported in literature during past decade.[3–5] Therefore, when present, the metastatic thyroid tumor could mimic the primary thyroid tumor, leading to diagnostic difficulties. On the other hand, controversies remain on the prevalence and management of this rare disease. This study aims to investigate the prevalence, management, and prognosis of metastases to the thyroid.
2. Patients and methods
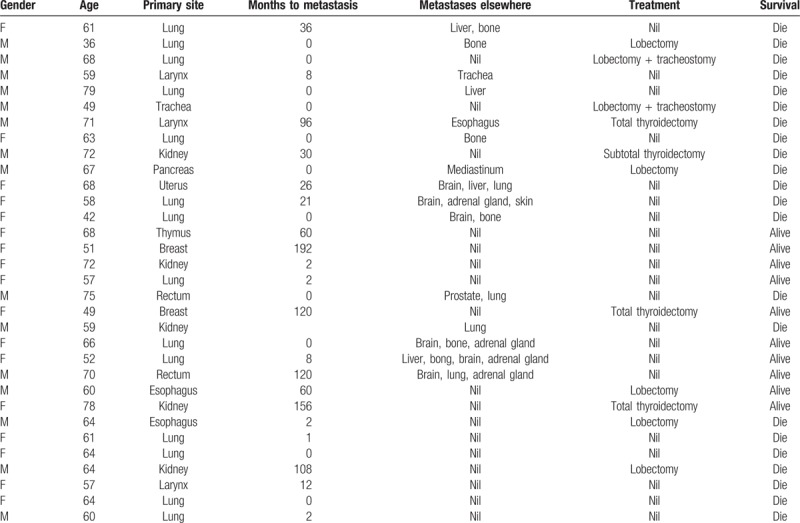
The database of patients with histologically proven metastases to the thyroid at Peking Union Medical College Hospital (PUMCH) from January 2003 to December 2015 was screened. Thirty-two patients who presented with metastatic tumors of the thyroid were included into this study. Among these patients, 17 patients were female and 15 patients were male. The female-to-male ratio of these patients was 1.13:1.00, and the age of these patients ranged within 36 to 79 years old, with a median age of 62 years old. These 32 patients accounted for 0.3% of all thyroid malignancies surgically treated in PUMCH. The records of these patients are presented in Table 1.
Table 1.
Clinical data of patients with thyroid metastases.
3. Results
Merely 7 patients (21.9%) presented with clinical complaints such as enlarged thyroid gland, dysphagia, dysphonia, or hoarseness. Most of the secondary thyroid tumors were incidentally found through screening examinations such as ultrasound. The sonographic characteristics of secondary thyroid cancer were diverse, and multiple thyroid nodules were a common manifestation, with the tumor size ranging within 0.6 to 6.6 cm. Furthermore, large, multiple, and ill-defined solid lesions with rich blood flow could be helpful in identifying secondary thyroid cancer. Among these 32 patients, 28 patients (87.5%) were diagnosed histologically by surgery or cytologically by fine-needle aspiration biopsy (FNAB); while for the remaining 4 patients (12.5%), the diagnosis was performed based on seriousness of the clinical condition. The most common primary lesion was in the lungs (14), followed by kidney (5), and gastrointestinal system (5). Other primary locations also include the breast, uterus, larynx, and trachea. The interval from the diagnosis of the primary tumor to the metastases varied from 0 month to 16 years. The interval was particularly long in 1 patient with breast cancer (16 years). Eleven metastases (34.4%) were synchronously found with the primary site. In addition, 16 patients (50%) had metastases in other locations such as in the bone, brain, liver, adrenal gland, prostate, and esophagus at diagnosis. Eleven patients (34.5%) had thyroidectomy, including 3 patients with renal clear cell carcinoma, 2 patients with lung cancer, 2 patients with esophagus cancer, 1 patient with breast cancer, 1 patient with trachea cancer, 1 patient with larynx cancer, and 1 patient with pancreatic cancer. A total of 3 patients (27.3%) are still alive, including 1 patient with renal clear cell carcinoma, 1 patient with breast cancer, and 1 patient with esophagus cancer. Two patients (6.25%) had tracheostomies to alleviate compression caused by enlarged thyroid tumors. No preoperative morbidity or mortality was noted. Furthermore, among these 32 patients, 22 patients (68.8%) died from primary tumors, and 10 patients (31.2%) are still alive; and the longest survival time was 7 years after the diagnosis of metastatic thyroid cancer from breast cancer.
4. Discussion
The incidence of thyroid cancer has continuously increased over the last decade. However, it is unusual to see a patient with metastatic thyroid tumor in clinical practice. The incidence of secondary thyroid tumor has been reported to be as low as 2% to 3% of all malignant tumors of the thyroid.[6,7] In the present report, only 32 patients presented with thyroid metastases at PUMCH over a 13-year period, accounting for only 0.3% of all thyroid malignancies. On the contrary, autopsy studies revealed that the incidence of thyroid metastases in patients with a known malignancy can be as high as 24%, which meant that a certain number of thyroid metastases had been overlooked. Therefore, for a new thyroid mass in a patient with a previous history of malignancy, metastatic thyroid tumors should not be excluded in the differential diagnosis of thyroid tumors.
Metastatic thyroid disease is usually associated with cancer dissemination through blood from a distant focus or with a direct or lymphatic spread to the thyroid gland by a neoplastic process situated in the adjacent organs. Among the 32 patients in the present study, 27 patients (84.4%) had metastatic tumors that originated from remote organs such as the lungs, kidney, and digestive systems, while 5 patients (15.6%) had metastatic tumors that originated from adjacent organs such as the trachea, esophagus, and larynx. The most frequently reported nonthyroid malignancy is renal clear cell carcinoma, followed by colorectal and lung carcinoma.[8] In the present study, the most common site of primary tumor was the lungs (14/32), followed by the kidney (5/32) and gastrointestinal system (5/32). This may be explained by the fact that the incidence of lung cancer has risen sharply in recent years in China.
Metastatic thyroid tumors often occur in the elderly, who are at their 60s and 70s. In this series, the mean age of patients was 62 years old, which was consistent with the reported result in a literature.[9] A strong female predominance has been proven for primary thyroid cancer. Furthermore, Duggal and Horattas[10] also noted a 6:1 female-to-male ratio of metastases to the thyroid gland. However, a large review on the metastases of the thyroid merely revealed a modest high ratio of 1:4,[8] which is similar to the results of the present study (1:13).
Thyroid metastases may present with symptoms such as dyspnea, dysphagia, and hoarseness, have an asymptomatic mass, or even be clinically occult. We found that these symptoms were closely correlated with the location of the primary site. Tumors originating from adjacent organs such as the trachea, esophagus, or larynx often cause symptoms such as dyspnea, dysphagia, or hoarseness, which mimics primary thyroid cancer. In some critical cases, compression on the trachea can be fatal. In the present study, 7 patients were symptomatic. Among these patients, 5 patients had metastases from adjacent organs, and 2 patients had tracheostomies to alleviate airway compression caused by the invasion of adjacent tumors. Nevertheless, an incidentally found asymptomatic thyroid mass may be the initial evidence of recurrent disease.
The majority of metastases were found metachronously, which often occurred some years after the diagnosis of primary tumors. The longest interval between the initial diagnosis of primary tumors and metastasis to the gland has been reported to be 21 years.[11] Among the 23 patients, 21 patients were found metachronously. The mean interval between the discovery of the primary tumor and the thyroid metastasis was 3.3 years, with the longest interval being 16 years after the diagnosis of breast cancer. We note that the interval depended on the characteristic of the primary tumor. For tumors with an aggressive nature such as lung cancer, the interval ranged within 0 to 21 months, which was the shortest. On the contrary, the longest interval occurred in patients with tumors such as renal clear cell cancer and breast cancer.
Thyroid metastases can be diagnosed by thyroidectomy specimen or by FNAB. Immunohistochemistry is usually helpful in differentiating between primary thyroid malignancy and secondary malignancy.
The prognosis of metastases to the thyroid depends on the stage of the primary tumor and the extent of disease dissemination rather than its spread to the thyroid gland.[12] There are no consistent guidelines on the surgical policy of metastatic thyroid tumors, although most literature reports recommended thyroidectomy for patients with secondary thyroid tumor. In our series, 11 patients (34.5%) had thyroidectomy, and only 3 of these patients are still alive, with the longest follow-up survival time of 6 years. Therefore, aggressive surgery may not be recommended for patients whose primary tumor had a comparatively poor prognosis.
5. Summary and conclusion
Lung cancer is the most common tumor that metastasized to the thyroid gland in PUMCH over the last decade. It accounted for almost half of patients with this condition in this study. Kidney and gastrointestinal system were also relatively common sources of metastatic tumor to the thyroid. For a patient with a secondary thyroid cancer from lung cancer, the symptom was often clinically occult, and the interval between the initial diagnosis of the primary tumor and metastasis to the gland was very short, which was often <2 years. Imaging studies and FNAB were important diagnostic tools. Thyroidectomy was not recommended for aggressive primary tumors such as lung cancer due to poor prognosis.
In conclusion, the diagnosis of suspicious metastatic thyroid tumors should be kept in mind for thyroid masses in patients with a previous history of malignancy, even if it occurred many years after surgery. For a primary tumor with a comparatively poor prognosis, excision of the secondary metastatic thyroid cancer may not be recommended.
Footnotes
Abbreviations: FNAB = fine-needle aspiration biopsy, PUMCH = Peking Union Medical College Hospital.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Mazzaferri EL, Sipos J. Should all patients with subcentimeter thyroid nodules undergo fine-needle aspiration biopsy and preoperative neck ultrasonography to define the extent of tumor invasion? Thyroid 2008;18:597–602. [DOI] [PubMed] [Google Scholar]
- [2].Uhry Z, Colonna M, Remontet L, et al. Estimating infra-national and national thyroid cancer incidence in France from cancer registries data and national hospital discharge database. Eur J Epidemiol 2007;22:607–14. [DOI] [PubMed] [Google Scholar]
- [3].McCabe DP, Farrar WB, Petkov TM, et al. Clinical and pathologic correlations in disease metastatic to the thyroid gland. Am J Surg 1985;150:519–23. [DOI] [PubMed] [Google Scholar]
- [4].Chen H, Nicol TL, Udelsman R. Clinically significant, isolated metastatic disease to the thyroid gland. World J Surg 1999;23:170–80. [DOI] [PubMed] [Google Scholar]
- [5].Czech JM, Lichtor TR, Carney JA, et al. Neoplasms metastatic to the thyroid gland. Surg Gynecol Obstet 1982;155:503–5. [PubMed] [Google Scholar]
- [6].Barczynski M, Jamski J, Cichon S, et al. Diagnosis, treatment and prognosis in cases of renal clear cell carcinoma metastases into the thyroid gland. Przegl Lek 2000;57:157–9. [PubMed] [Google Scholar]
- [7].Bayram F, Soyuer I, Atmaca H, et al. Prostatic adenocarcinoma metastasis in the thyroid gland. Endocr J 2004;5:445–50. [DOI] [PubMed] [Google Scholar]
- [8].Chung AY, Tran TB, Brumund KT, et al. Metastases to the thyroid: a review of the literature from the last decade. Thyroid 2012;22:258–68. [DOI] [PubMed] [Google Scholar]
- [9].Heffess CS, Wening BM, Thompson LD. Metastatic renal cell carcinoma to the thyroid gland: a clinicopathologic study of 36 cases. Cancer 2002;95:1869–78. [DOI] [PubMed] [Google Scholar]
- [10].Duggal NM, Horattas MC. Metastatic renal cell carcinoma to the thyroid gland. Endocr Prac 2008;14:1040–6. [DOI] [PubMed] [Google Scholar]
- [11].Mattavelli F, Collini P, Pizzi N, et al. Thyroid as a target of metastases. A case of foregut neuroendocrine carcinoma with multiple abdominal metastases and a thyroid localization after 21 years. Tumori 2008;94:110–3. [DOI] [PubMed] [Google Scholar]
- [12].Papi G, Fadda G, Corsello SM, et al. Metastases to the thyroid gland: prevalence, clinicopathological aspects and prognosis: a 10-year experience. Clin Endocrinol (Oxf) 2007;66:565–71. [DOI] [PubMed] [Google Scholar]


