Abstract
The presence of interval nodes (IN) in melanoma is testified in several studies and sometimes these lymph nodes can contain metastatic disease. Currently there are no guidelines about the management of patients with tumor-positive INs.
We enrolled all patients affected by melanoma who underwent sentinel lymph node biopsy (SLNB) in a single institution. All patients with tumor-positive IN underwent the lymphadenectomy of the subsequent draining lymphatic field. Prognosis of IN+-patients was compared with subjects with positive SLNB in usual field through Kaplan-Meier and multivariate Cox regression analysis.
Overall 596 subjects underwent lymphoscintigraphy and one or more INs were identified in 94 (15.8%) patients. The mean number of sentinel lymph nodes (SNs) identified per patient was significantly higher in patients with INs. Macrometastasis were more common in patients with INs. Matched pair analysis testified a statistically significant better prognosis in patients with positive-INs when compared with patients with positive SNs in usual side with the same demographic and clinical characteristics. These findings were confirmed both in analysis of 10-year recurrence-free period, then in 10-years overall survival analysis.
Lymphadenectomy of the lymphatic draining field beyond positive-IN testify has proved to be a safe procedure that may improve prognosis in melanoma patients with tumor-positive INs. The better prognosis of patients with tumor-positive INs undergoing lymphadenectomy may be justified by the earlier treatment of lymphatic metastases. Further multicentric comparative studies are needed to evaluate possible impact of this procedure on prognosis of melanoma patients.
Keywords: interval lymph node, melanoma, metastasis, sentinel lymph node biopsy, tumor progression
KEY POINTS
The presence of interval nodes (IN) in melanoma is testified in several studies.
Lymphadenectomy of the lymphatic draining field beyond positive-IN has proved to be a safe procedure that may improve prognosis in melanoma patients with tumor-positive INs.
Lymphadenectomy should be recommended in melanoma patients with positive interval nodes.
1. Introduction
Lymphatic metastatic progression in melanoma is characterized by the development of a rich lymphovascular network.[1] Lymphoscintigraphy is indicated to identify the lymphatic draining pathways and to guide the sentinel lymph node biopsy (SLNB).[2,3] SNLB allows a better staging of disease and an early detection of melanoma lymphatic metastasis, identifying patients eligible to locoregional lymphadenectomy (LA).[4] The sentinel lymph node (SN) is the first lymph node receiving direct lymphatic drainage from a primary cancer site.[5] SNs is usually located in axillary, inguinal, and cervical basins, but SNs may be located outside from these conventional basins because of anatomical differences in lymphatic pathway. This is even more true in melanomas arising in specific surgical sites (such as the head and neck), because the presence of the high complexity and variability of lymphatic drainage.[6] Sentinel lymphs (SLs) arising outside of conventional basins were called in different ways (aberrant, in-transit, ectopic, or intercalated) during years,[7–10] but nowadays literature termed them as interval sentinel lymph nodes (INs).[11–13] INs lie in subcutaneous fat along the course of lymphatic collecting vessels between a primary tumor site and a draining node field.[14] INs can contain metastatic disease and the presence of tumor-positive IN (IN+) worsens the prognosis of patients affected by melanoma.[10] Nevertheless, currently there are no guidelines about the surgical management of these patients.[15–18]
2. Materials and methods
2.1. Population in study
All patients who underwent SLNB for primary cutaneous melanoma were retrospectively identified from a single-institution (Plastic and Reconstructive Department of Policlinico di Bari) electronic medical records, including data of patients treated from July 1994 to December 2016. Patients with stage IV melanoma or affected by other carcinomas were excluded.
Within the 90th day from excision of the primary lesion, patients with a primary melanoma ≥0.75 mm in thickness or with adverse prognostic features (high Clark level, regression, ulceration, high mitosis rate) underwent lymphoscintigraphy to identify SN draining fields. Complete lymph node dissection was proposed to all patients with positive SLNB.[19–22]
Histological reports were reviewed and standardized for all patients included in the study. Pathologists reviewed results of specimens of the SLNB and wide excision for each patient include in this study. All patients underwent a clinical and imaging follow-up—including chest x-ray, abdominal and lymphatic ultrasound, and single photon emission computerized tomography/computerized tomography for difficult areas—every 6 months for the first 5 years and yearly thereafter.
2.2. Lymphatic mapping, sentinel lymph node biopsy, and follow-up
Lymphoscintigraphy was performed using Technetium 99m nanocolloid human serum albumin with a dosage of 18 to 37 MBq (in relationship with procedure time) injected closely around primary lesion. Ultra-high-resolution collimators were used to image all the territories between the primary melanoma site and the recognized draining node fields, reducing artifacts. Dynamic and planar images were acquired using dual-headed digital gamma cameras both immediately after the radiolabeled colloid injection and then after every lymph node visualization. Further static images were acquired to ensure that all SNs were marked. A handheld gamma probe was used during surgery to guide SN detection.[23,24] Lymph nodes lying outside from usual or minor fields between a primary tumor site and an usual drainage field are considered INs.[23,24] For each SN, multiple sections of specimens were examined both by conventional hematoxylin and eosin and immunohistochemical stains using European Organization for Research and Treatment of Cancer protocol from 2009[25–27] and World Health Organization melanoma program protocol before 2009.[27] A clinically detectable nodal metastasis confirmed by therapeutic LA, or the histological presence of a metastasis exhibiting gross extracapsular extension, was considered as macrometastasis, otherwise it was defined as micrometastasis.[28] After obtaining informed consent, complete lymph node dissection was performed in all patients with lymphatic metastasis. All patients underwent a clinical and imaging follow-up every 6 months for the first 5 years and yearly thereafter.
2.3. Statistical analysis
Patients’ baseline characteristics were reported as the frequency (percentage) and mean ± standard deviation or median and interquartile ranges. Categorical variables were assessed by the χ2 test to compare the results for specific subgroups with those of the rest of the patient population, whereas continuous variables were compared among groups using Wilcoxon rank-sum test. Recurrence-free survival was defined as the time between complete removal of the primary melanoma and clinical or imaging detection of the first recurrence. Follow-up time was defined as the time between complete removal of the primary melanoma and the last contact with patient. A matched pair 1-to-1 analysis was used to allow an unbiased comparison between patients in which the IN was the only positive-SN (Group 1) and those with a positive-SN in usual field (control group).[29] A logistic regression model including age, sex, ulceration of primary lesion, Breslow thickness, and size of metastasis in SLNB as covariates was used to predict the probability (propensity score) to detect a positive-IN as the only SL. Adequacy of balance for the covariates in the matched sample was assessed via standardized mean difference between the 2 groups, considering differences <10% as good balance.[30]
Overall survival and disease-free period were evaluated through time-to-death analyses performed using survival curves and probabilities according to the Kaplan-Meier method. Multivariate analysis was performed using Cox proportional hazards regression models, with risks reported as hazard ratios along with their 95% confidence interval. The P value was considered significant if P < .05. All statistical analyses were performed using SAS Software Release 9.4 (SAS Institute, Cary, NC).
3. Results
3.1. Patients’ characteristics, frequency of interval nodes, and results of sentinel lymph node biopsy
Overall 596 subjects underwent lymphoscintigraphy and one or more INs were identified in 94 (15.8%) patients. The clinical-pathological features and the location of the primary cutaneous melanoma are reported in Table 1. INs were reported significantly more frequently in patients with melanomas on head and neck,[31,32] whereas the incidence of interval nodes was significantly lower in patients with primary lesion in the limbs (P < .001). No further major differences were found in age and sex or primary lesion characteristics between patients with and without INs. The mean number of SNs identified per patient was significantly higher in patients with INs (Table 2). This finding was due to the presence of at least another usual draining lymphatic field in 54 patients with INs, whereas in 40 cases the interval node was the only SN.
Table 1.
Clinical and pathological characteristics of population.
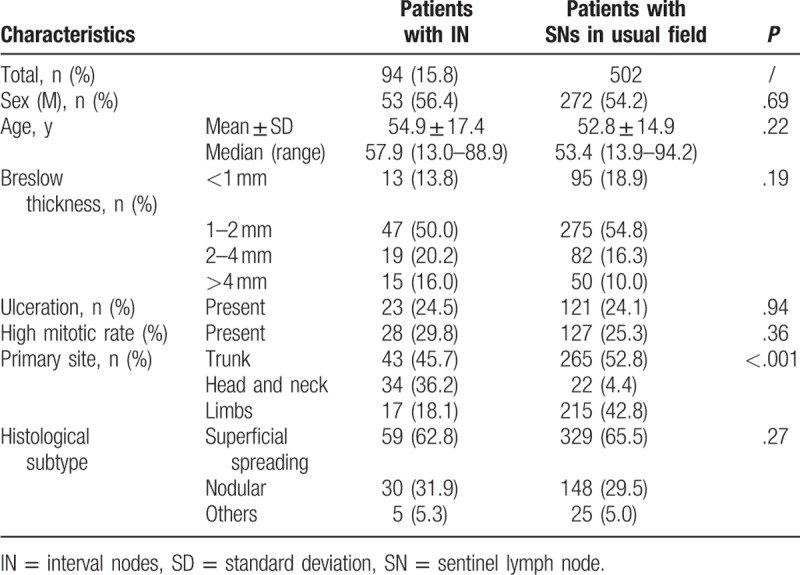
Table 2.
Results of sentinel lymph node biopsy and lymphadenectomy.
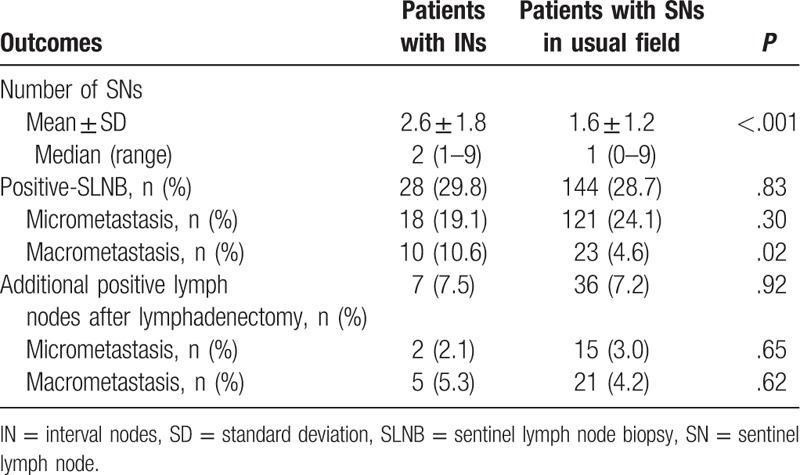
Overall, positive-SLNBs were recognized in 172 (28.9%) subjects: in 144 (28.7%) out of 502 patients with SNs in usual field and in 28 (29.8%) out of 94 subjects with INs. Macrometastasis were more common in patients with INs; in fact, macrometastasis were reported in 10 (10.6%) patients with INs versus 23 (4.6%) subjects with SNs in usual field (P < .02). After LA, additional lymph nodes were detected in 7 (7.5%) patients with positive-INs and in 36 (7.2%) patients with positive SLNBs in usual field, without significant differences between the 2 groups.
Among subjects with positive-INs, in 14 cases the IN was the only positive-SN (group 1), whereas in 14 there was another positive-SN in a usual field. Although in patients with both positive-INs and usual site SNs the complete dissection of the usual basin is recommended, there were no guidelines about the indication to LA in patients of group 1. According with the sequential diffusion of lymphatic metastases, radical dissection of the draining lymphatic field beyond the positive-IN (LFBI) was proposed also to patients of group 1.[16,19]
3.2. Frequency of lymphatic metastases, survival, and recurrence-free analysis
Follow-up information was available for 154 out 172 patients with tumor-positive SNs. The mean follow-up period in the population with positive-INs amounted to 67.9 ± 39.8 months, whereas the mean follow-up in the cohort with usual site positive-SNs (control group) was 80.7 ± 56.1 months. Additional positive lymph nodes were detected in 3 (21.4%) patients in group 1 and in 40 (28.6%) patients with positive-SNs in usual basin (control group). Among patients of control group, in 2 (1.4%) cases SNs identified in lymphoscintigraphy were not found during surgical resection.
Overall, 74 (46.9%) of 154 patients with positive SNs developed a local, in-transit, regional, or distant recurrence: 3 (21.4%) out of 14 patients of group 1 after a median period of 33.2 ± 25.9 months and 71 (50.7%) out of 140 patients of control group after a mean period of 33.4 ± 36.6 months. Instead, 2 (14.3%) deaths were recorded in group 1 after a mean period of 40.6 ± 15.9 months and 57 (40.7%) in control group after a mean period of 41.1 ± 35.4 months (Table 3). Although frequencies of recurrences and deaths were significantly lower in patients in group 1, recurrence-free period (P = .13) and overall survival (P = .14) did not significantly differ between the 2 groups when compared in a Kaplan-Meier survival analysis.
Table 3.
Follow-up period and outcomes of patients of group 1 and control group.

3.3. Matched pair analysis
From the initial cohort of 14 subjects of group 1, 11 were selected using propensity score matching. Prematching characteristics widely differ between patients of group 1 and those of control group, but matched pair analysis let to a satisfactory balance for all the characteristics considered (Table 4). Postmatching cohort with positive-IN include patients with a mean age of 51.3 ± 18.4 years who showed a thick melanoma at diagnosis in 27.3% of cases; ulceration of primary lesion was present in 5 (45.5%) subjects and a macrometastatic-SN 3 (27.3%) cases. After LA, additional positive lymph nodes were detected in 3 (27.3%) patient in group 1 and in 4 (36.4%) patients of control group. Ten years recurrence-free period and survival rate were compared between the 2 postmatching cohorts. Kaplan-Meier analysis testified a statistically significant better prognosis in patients with positive-INs when compared with patients with positive SNs in usual side with the same demographic and clinical characteristics. These findings were confirmed both in analysis of 10-year recurrence-free period (P = .02) then in 10-years overall survival analysis (P = .03) (Fig. 1).
Table 4.
Clinical and pathological characteristics of patients of group 1 and control group before and after matching.
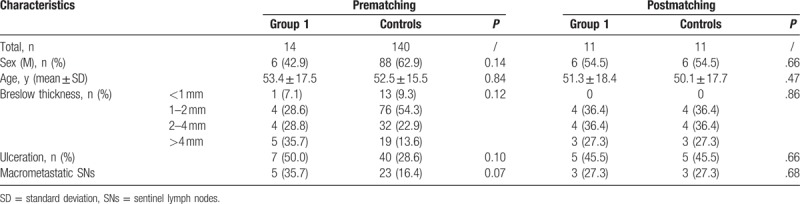
Figure 1.
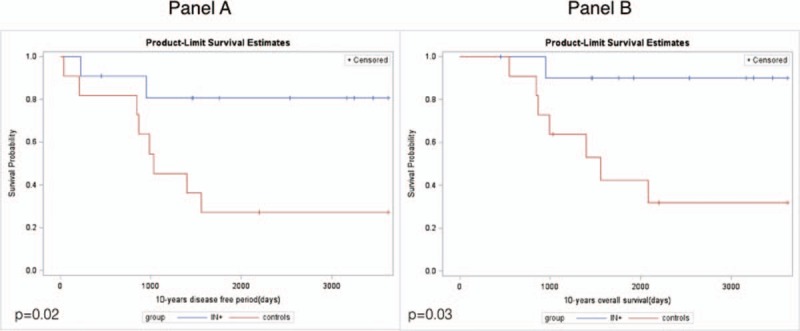
Kaplan-Meier curves. A, Overall survival. B, Recurrence-free period. Results of matched pair analysis.
4. Discussion
In our study, INs were reported in 15.8% of patients who underwent SLNB. This evidence was in accord with previous studies, in which the reported frequency of INs ranged among 3% and 22%.[7–18,26] The variability in frequency of INs could be explained by technical improvement in lymphascintigraphy. Nowadays, routine use of small particle radiocolloid combined with ultrahigh resolution collimators allow a better definition of lymphatic pathways, ensuring an accurate imaging of minor/unusual lymphatic fields.[33] The high accuracy of the lymphatic mapping in our study was testified by the low rate of SNs identified in lymphoscintigraphy but not found during surgical remotion. This high reliability could explain also the increasing rates of INs reported in more recent studies.
We found a similar frequency of positive-SLNBs in INs and usual site SNs. Currently, there are no guidelines about the management of patients with positive-IN and in literature several approaches are described:
-
1.
some authors recommended only clinical and imaging follow-up of the lymphatic fields[9];
-
2.
others proposed the LA of the usual LFBI in all patients with positive-IN[13,16];
-
3.
more recently Verwer et al[18] recommended LA of the LFBI in patients with both positive-INs and positive-SNs in the LFBI, defining useless any further treatment in patients in which the positive-IN was the only positive SN.
Our and previous studies findings have testified the presence of additional lymph nodes after LA of the lymphatic pathways beyond a positive-IN.[13,16] Moreover, some authors reported a higher risk of recurrence and death from melanoma in patients with positive-INs during a period of 10 years of follow-up.[25] For these reasons a conservative approach with a clinical and imaging follow-up seems inadequate. Furthermore, a significant difference between positive and negative INs in the percentage of Ki67 positive nuclei and mean vessel number was already established, suggesting an increased cellular proliferation and angiogenesis in positive INs.[26] The presence of a high angiogenesis in melanomas and its correlation with poor prognosis and increased rates of relapse is well know.[33] This increased angiogenesis could be responsible of developing of pathways of drainage between the IN site and the LFBI, justifying the presence of lymphatic metastasis beyond the site of positive-IN also in patients in which the interval is the only metastatic-SN. Therefore, the LA appears recommendable not only in patients with metastasis in INs and in LFBI—as suggested by Verwer[18]—but also in patients in which the IN is the only metastatic lymph node.
For these reasons—in accordance with the pathophysiological mechanism of sequential diffusion of lymphatic metastases—we propose the radical dissection of the LFBI in all patients with a positive-IN. This surgical approach was already proposed by Sumner et al,[16] without meaningful conclusions on prognosis due to the limited number of patients and events. The greater numerical sample of this study and the use of a matched pair analysis has allowed to evaluate the possible impact of the proposed procedure on overall survival and disease-free period. In fact—although we cannot directly compare the prognosis of patients with IN+ undergoing or not undergoing LA of the LFBI—we were able to compare prognosis of patients in whom the IN was the only positive_SN with a control group with positive-SNs in usual field. Ten-year free recurrence and survival were significantly better in patients of group 1 than in subjects of control group with same clinic-demographic characteristics. This result suggests that the immediate dissection of the LFBI could allow to treat patients in earlier stages of disease, before the dissemination of the lymph nodes in the usual basins.
5. Conclusion
The increased cellular proliferation and angiogenesis and the detection of additional tumor-positive lymph node beyond positive-INs suggest the possible dissemination across the lymphatic pathways, even in case of detection of metastasis after SLNB of INs. The good prognosis of patients who underwent complete dissection of the lymphatic field beyond the metastatic IN can be explained by an early treatment of the lymphatic metastatic spread.
Author contributions
Conceptualization: Michelangelo Vestita, Fabio Robusto, Giuseppe Giudice.
Data curation: Fabio Robusto, Michele Maruccia, Paolo Annoscia, Giuseppe Giudice.
Formal analysis: Michelangelo Vestita, Fabio Robusto, Paolo Annoscia.
Funding acquisition: Giuseppe Giudice.
Investigation: Michelangelo Vestita, Fabio Robusto, Paolo Annoscia, Giuseppe Giudice.
Methodology: Fabio Robusto, Michele Maruccia, Paolo Annoscia.
Project administration: Michele Maruccia, Giuseppe Giudice.
Software: Fabio Robusto, Paolo Annoscia.
Supervision: Michelangelo Vestita, Fabio Robusto, Michele Maruccia, Giuseppe Giudice.
Validation: Eleonora Nacchiero, Michelangelo Vestita, Michele Maruccia, Giuseppe Giudice.
Visualization: Eleonora Nacchiero, Paolo Annoscia, Giuseppe Giudice.
Writing — original draft: Eleonora Nacchiero, Fabio Robusto.
Writing — review and editing: Eleonora Nacchiero, Michelangelo Vestita, Giuseppe Giudice.
Footnotes
Abbreviations: IN = interval nodes, LA = lymphadenectomy, LFBI = lymphatic field beyond the positive-IN, SLNB = sentinel lymph node biopsy, SNs = sentinel lymph nodes, SPECT/CT = single photon emission computerized tomography/computerized tomography.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Ribatti D, Annese T, Longo V. Angiogenesis and melanoma. Cancers (Basel) 2010;2:114–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Rossi CR, De Salvo GL, Trifiro G, et al. The impact of lymphoscintigraphy technique on the outcome of sentinel node biopsy in 1313 patients with cutaneous melanoma: an Italian Multicentric Study (SOLISM-IMI). J Nucl Med 2006;47:234–41. [PubMed] [Google Scholar]
- [3].Macbeth F, Newton-Bishop J, O’Connell S, et al. Guideline development group. Melanoma: summary of NICE guide. BMJ 2015;351:h3708. [DOI] [PubMed] [Google Scholar]
- [4].Doubrovsky A, De Wilt JH, Scolyer RA, et al. Sentinel node biopsy provides more accurate staging than elective lymph node dissection in patients with cutaneous melanoma. Ann Surg Oncol 2004;11:829–36. [DOI] [PubMed] [Google Scholar]
- [5].Uren RF, Howman-Giles R, Thompson JF, et al. Lymphoscintigraphy to identify sentinel nodes in patients with melanoma. Melanoma Res 1994;4:395–9. [DOI] [PubMed] [Google Scholar]
- [6].Giudice G, Leuzzi S, Robusto F, et al. Sentinel lymph node biopsy in head and neck melanoma. G Chir 2014;35:149–55. [PMC free article] [PubMed] [Google Scholar]
- [7].O’Toole GA, Hettiaratchy S, Allan R, et al. Aberrant sentinel nodes in malignant melanoma. Br J Plast Surg 2000;53:415–7. [DOI] [PubMed] [Google Scholar]
- [8].Vidal-Sicart S, Pons F, Vilalta A, et al. Is the identification of in-transit sentinel nodes in malignant melanoma patients really necessary? Eur J Nucl Med Mol Imaging 2004;31:945–9. [DOI] [PubMed] [Google Scholar]
- [9].Lieber KA, Stanford SB, Kuvshinoff BW, et al. Surgical management of aberrant sentinel lymph node drainage in cutaneous melanoma. Surgery 1998;124:757–61. [DOI] [PubMed] [Google Scholar]
- [10].Chakera AH, Hansen LB, Lock-Andersen J, et al. In-transit sentinel nodes must be found: implication from a 10-year follow-up study in melanoma. Melanoma Res 2008;18:359–64. [DOI] [PubMed] [Google Scholar]
- [11].McMasters KM, Chao C, Wong SL, et al. Sunbelt Melanoma Trial Group. Interval sentinel lymph nodes in melanoma. Arch Surg 2002;137:543–7. [DOI] [PubMed] [Google Scholar]
- [12].Carling T, Pan D, Ariyan S, et al. Diagnosis and treatment of interval sentinel lymph nodes in patients with cutaneous melanoma. Plast Reconstr Surg 2007;119:907–13. [DOI] [PubMed] [Google Scholar]
- [13].Giudice G, Nacchiero E, Robusto F, et al. Optimizing the staging of melanoma patients for their best surgical management. Lymphology 2015;48:163–74. [PubMed] [Google Scholar]
- [14].Morton DL, Wen DR, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 1992;127:392–9. [DOI] [PubMed] [Google Scholar]
- [15].Uren RF, Howman-Giles R, Thompson JF, et al. Interval nodes: the forgotten sentinel nodes in patients with melanoma. Arch Surg 2000;135:1168–72. [DOI] [PubMed] [Google Scholar]
- [16].Sumner WE, Ross MI, Mansfield PF, et al. Implication of lymphatic drainage to unusual sentinel lymph node sites in patients with primary cutaneous melanoma. Cancer 2002;95:354–60. [DOI] [PubMed] [Google Scholar]
- [17].Roozendaal GK, De Vries JD, Van Poll D, et al. Sentinel nodes outside lymph node basins in patients with melanoma. Br J Surg 2001;88:305–8. [DOI] [PubMed] [Google Scholar]
- [18].Verwer N, Scolyer RA, Uren RF, et al. Treatment and prognostic significance of positive interval sentinel nodes in patients with primary cutaneous melanoma. Ann Surg Oncol 2011;18:3292–9. [DOI] [PubMed] [Google Scholar]
- [19].Guida M, Cramarossa A, Fistola E, et al. High activity of sequential low dose chemo-modulating Temozolomide in combination with Fotemustine in metastatic melanoma. A feasibility study. J Transl Med 2010;8:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Giudice G, Robusto F, Nacchiero E. The surgical treatment of a melanoma patient with macroscopic metastasis in peri and retrocaval lymph nodes and with a positive sentinel lymph node in the groin. Ann Ital Chir 2016;87:pii: S2239253X16024762. [PubMed] [Google Scholar]
- [21].Rossi CR, Mozzillo N, Maurichi A, et al. Number of excised lymph nodes as a quality assurance measure for lymphadenectomy in melanoma. JAMA Surg 2014;149:700–6. [DOI] [PubMed] [Google Scholar]
- [22].Rossi CR, Mozzillo N, Maurichi A, et al. The number of excised lymph nodes is associated with survival of melanoma patients with lymph node metastasis. Ann Oncol 2014;25:240–6. [DOI] [PubMed] [Google Scholar]
- [23].Thompson JF, Uren RF, Shaw HM, et al. Location of sentinel lymph nodes in patients with cutaneous melanoma: new insights into lymphatic anatomy. J Am Coll Surg 1999;189:195–204. [DOI] [PubMed] [Google Scholar]
- [24].Caracò C, Marone U, Di Monta G, et al. Surgical management of sentinel lymph node biopsy outside major nodal basin in patients with cutaneous melanoma. Ann Surg Oncol 2014;21:300–5. [DOI] [PubMed] [Google Scholar]
- [25].Chakera AH, Hesse B, Burak Z, et al. EANM-EORTC general recommendations for sentinel node diagnostics in melanoma. Eur J Nucl Med Mol Imaging 2009;36:1713–42. [DOI] [PubMed] [Google Scholar]
- [26].Marinaccio C, Giudice G, Nacchiero E, et al. Interval sentinel lymph nodes in melanoma: a digital pathology analysis of Ki67 expression and microvascular density. Clin Exp Med 2016;16:383–9. [DOI] [PubMed] [Google Scholar]
- [27].Clemente C, Cochran AJ, Elder DE, et al. Histopathologic diagnosis of dysplastic nevi: concordance among pathologists convened by the World Health Organization Melanoma Programme. Hum Pathol 1991;22:313–9. [DOI] [PubMed] [Google Scholar]
- [28].Spanknebel K, Coit DG, Bieligk SC, et al. Characterization of micrometastatic disease in melanoma sentinel lymph nodes by enhanced pathology: recommendations for standardizing pathologic analysis. Am J Surg Pathol 2005;29:305–17. [DOI] [PubMed] [Google Scholar]
- [29].Yanovitzky I, Zannuto E, Hornik R. Estimating casual effects of public health education campaigns using propensity score methodology. Eval Program Plans 2005;28:209–20. [Google Scholar]
- [30].Austin PC, Grootendorst P, Anderson GM. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med 2007;26:734–53. [DOI] [PubMed] [Google Scholar]
- [31].Balch CM, Soong SJ, Atkins MB. An evidence-based staging system for cutaneous melanoma. CA Cancer J Clin 2004;54:131–49. [DOI] [PubMed] [Google Scholar]
- [32].Gandini S, Montella M, Ayala F, et al. Sun exposure and melanoma prognostic factors. Oncol Lett 2016;11:2706–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Straume O, Salveson HB, Aksel LA. Angiogenesis is prognostically important in vertical growth phase of melanoma. Int J Oncol 1999;15:595–9. [DOI] [PubMed] [Google Scholar]


