Abstract
Background:
Preservation and enhancement of cognitive function are essential for the restoration of functional abilities and independence following stroke. While cognitive-motor dual-task training (CMDT) has been utilized in rehabilitation settings, many patients with stroke experience impairments in cognitive function that can interfere with dual-task performance. In the present study, we investigated the effects of CMDT combined with auditory motor synchronization training (AMST) utilizing rhythmic cues on cognitive function in patients with stroke.
Methods:
The present randomized controlled trial was conducted at a single rehabilitation hospital. Thirty patients with chronic stroke were randomly divided an experimental group (n = 15) and a control group (n = 15). The experimental group received 3 CMDT + AMST sessions per week for 6 weeks, whereas the control group received CMDT only 3 times per week for 6 weeks. Changes in cognitive function were evaluated using the trail making test (TMT), digit span test (DST), and stroop test (ST).
Results:
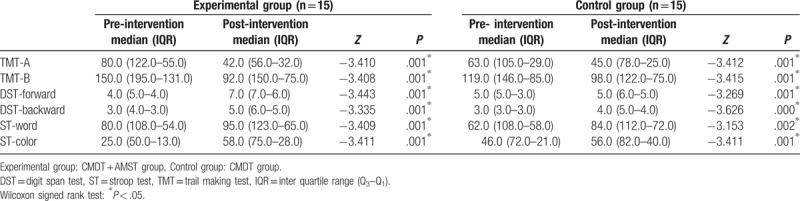
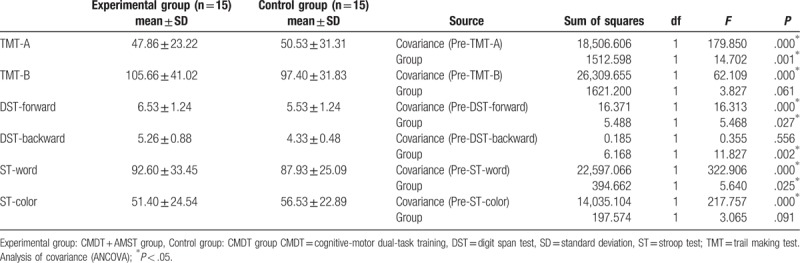
Significant differences in TMT-A and B (P = .001, P = .001), DST-forward (P = .001, P = .001), DST-backward (P = .000, P = .001), ST-word (P = .001, P = .001), and ST-color (P = .002, P = .001) scores were observed in both the control and experimental groups, respectively. Significant differences in TMT-A (P = .001), DST-forward (P = .027), DST-backward (P = .002), and ST-word (P = .025) scores were observed between the 2 groups. Performance speed on the TMT-A was faster in the CMDT + AMST group than in the CMDT group. Moreover, DST-forward and DST-backward scores were higher in the CMDT + AMST group than in the CDMT group. Although ST-color results were similar in the 2 groups, ST-word scores were higher in the CMDT + AMST group than in the CMDT group.
Conclusion:
This finding indicates that the combined therapy CMDT and AMST can be used to increase attention, memory, and executive function for people with stroke.
Keywords: auditory motor synchronization, cognition, cognitive motor dual task, stroke
1. Introduction
Stroke occurs when blood flow to the brain is impeded due to blockage or rupture of vessels, often leading to long-term disability.[1] Approximately 25% of patients with stroke experience severe cognitive impairment (eg, dementia), while between 50% and 75% experience mild-to-moderate cognitive impairment.[2] Preservation and enhancement of cognitive function are essential for the restoration of functional abilities and independence following stroke.[3] Indeed, previous studies have indicated that both loss of motor function and cognitive are closely associated with functional recovery in activities of daily living such as walking, standing, etc.[4] Many previous studies have demonstrated that cognitive-motor dual-task training (CMDT) is effective in promoting the recovery of both cognitive and motor functions following stroke.[5,6]
The CMDT is the therapeutic method of promoting the recovery of both motor and cognitive functions from neurologic damage. CMDT is a training technique of performing a cognitive task during the execution of a motor task. It has usually been applied to the patients with stroke, brain damage, and Parkinson's disease to improve their balance and walking ability, and has actively been researched so far.[7]
However, patients with stroke or neurologic impairment exhibit dual-task interference due to difficulties in performing cognitive and motor tasks simultaneously,[8] which manifests as reduced performance on the primary motor task when a secondary cognitive task is introduced.[9] The ability to perform 2 tasks simultaneously is significantly associated with attentional capacity and the allocation of cognitive resources.[10,11] Previous research has indicated that patients with stroke exhibit decreased attentional capacity, concentration, memory function, and executive function relative to healthy controls, contributing to poor functioning in activities of daily living.[12,13] After brain damage has occurred, most patients recover the ability to concentrate on simple tasks, although more complex/multidimensional tasks require further improvement.[14] Some studies have suggested that attention improvement training involving various types of feedback (eg, auditory feedback) during task performance may improve functional outcomes following stroke.[15–17] For example, Rossignol and Jones reported that training based on rhythmic auditory stimulation contributed to the activation of neural networks involved in the sequential processing of external auditory signals.[18] During motor performance, auditory stimulation with a constant tempo is first transmitted to the temporal lobe, following which the movement is planned by the prefrontal cortex and accomplished via the cooperation of the premotor cortex, primary motor cortex, and supplementary motor area.[19] Timing training using repeated rhythms with a constant tempo helps the brain process information sequentially and improves cognitive functioning associated with motor planning and sequencing, as well as motor performance.[20] Rochester et al reported that such rhythmic external auditory cues are effective in reducing dual-task interference on functional performance in patients with Parkinson's disease.[17] Furthermore, in the Choi et al's study compared the effects of dual tasks using external auditory cue and simple task without auditory cue on balance in patient with stroke. The results suggested that the dual tasks accompanied by external auditory cues were more effective in increasing balance.[21] However, previous studies have failed to investigate cognitive changes during such tasks. Thus, it remains to be determined whether auditory cues presented at a rhythmic tempo exert these effects by enhancing motor as well as cognitive functions.
Based on the aforementioned evidence, we hypothesized that CMDT combined with auditory motor synchronization training (AMST) using rhythmic auditory cues would significantly improve cognitive function in patients with stroke. Therefore, we aimed to compare the effects of CMDT and CMDT with AMST on cognitive functioning in individuals with chronic stroke.
2. Material and methods
2.1. Study design
The present randomized control trial was approved by the institutional ethics committee of Soonchunhyang University (1040872-201605-BM-014). The study was performed at Glory Rehabilitation Hospital in Inchen, South Korea, from March to September 2016. About 42 eligible participants were firstly recruited. However, 8 participants did not meet inclusion criteria, and 4 participants refused to perform in the study. Finally a total of 30 participants were randomly divided an experimental group or control group at an equal ratio of 1:1.
2.2. Participants
Inclusion criteria were as follows: diagnosis of stroke with cerebral hemorrhage and cerebral infarction by a medical doctor specialized in rehabilitation medicine or neurology; stroke occurrence more than 6 months prior to enrollment; score ≥21 on the Korean version of the mini mental status examination (MMSE-K), adequate understanding of the purpose of the study, capability to respond to oral instructions; upper and lower extremity recovery of Brunnstrom stage 4 or greater to ensure ability to perform dual tasks. Exclusion criteria were as follows: secondary diagnoses such as dementia; history of seizure; history of high blood pressure or angina preventing long-term participation in activity; and visual or auditory impairments that would interfere with task performance.
2.3. Randomization and blinding
Participants were allocated by a study coordinator into 2 groups using a computerized randomization table: an experimental group (n = 15) and a control group (n = 15) (true random number generator, www.random.org). Initially, 1 was entered as the minimum number, 30 as the maximum number, and the patients corresponding to the calculated numbers were randomly assigned to the experimental group. Next, the maximum number was replaced by 29, and the patients corresponding to the calculated numbers were randomly assigned to the control group. This process was repeated step by step, decreasing the maximum number at each iteration. Allocation of groups was sequentially numbered and sealed with black envelopes. Outcome assessors were not informed whether a patient was assigned to the experimental or the control group. Also, the data analyst was blinded to the intervention allocation. The study protocol followed the recommendations outlined in the Consolidations Standards of Reporting Trials (CONSORT) (Fig. 1).
Figure 1.
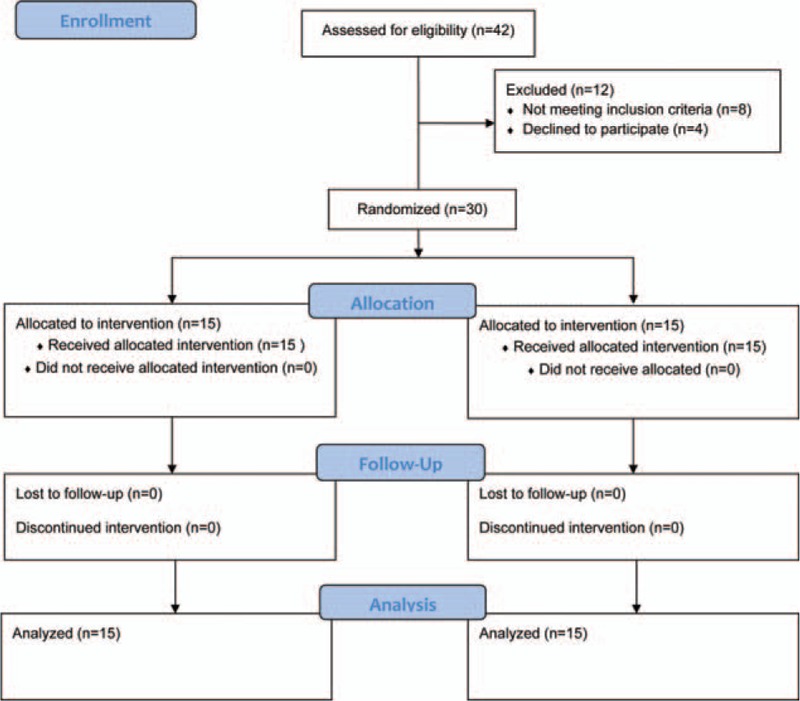
Flow diagram of the study process for the 2 groups.
2.4. Intervention methods
2.4.1. Control group
Participants of the control group received three 30-minute sessions of CMDT per week for 6 weeks. CMDT was comprised of motor tasks associated with balance and posture while sitting and standing, which were performed simultaneously with cognitive tasks associated with attention, memory, and executive function. For example, participants were required to count backwards from a specific number while sitting up, and to name the days of the week in reverse order from Monday to Sunday during trunk rotation (Table 1).
Table 1.
Comparison of CMDT and CMDT + AMST programs.
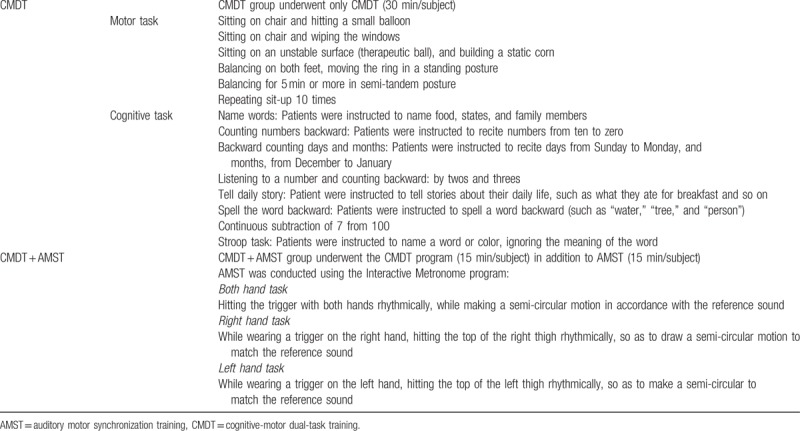
2.4.2. Experimental group
Participants of the experimental group received CMDT combined with AMST (CMDT + AMST). They enrolled intervention in the separated room from control group. The CMDT and AMST components of each session lasted 15 minutes each, for a total session time of 30 minutes. The CMDT portion of the combined training was conducted in the same manner as described for the control group. AMST consisted of tasks performed using an interactive metronome (IM pro 9.0, Interactive Metronome, Sunrise, Florida).[2] The intervention environment consisted of a computer equipped with the interactive metronome, additional hardware, software, a headset, a hand trigger, and a foot trigger. Participants performed 13 motor tasks while pressing the trigger at an appropriate interval from the reference sound, which was played through the headset. The following AMST tasks were selected based on their appropriateness for patients with stroke: 2-hand task, right-hand task, and left-hand task. The 2-hand task involved tapping both hands in time to the reference sound while performing a semi-circular movement, while each single-handed task involved pressing the right or left trigger in response to the reference sound (Table 1, Fig. 2).
Figure 2.

Auditory motor synchronization training of the experimental group. Auditory motor timing training used interactive metronome. Experimental group received cognitive motor dual task training with auditory motor synchronization training.
2.5. Outcome measures
The primary outcome was the attention changes in the 2 groups. The secondary outcome was the cognitive control and flexibility based on executive function. To evaluate primary and secondary outcomes, participants were assessed using sub-items included in the Seoul Neurocognitive Screening Battery developed by Kang et al, as follows: trail making test (TMT; A and B), stroop test (ST; word and color), and digit span test (DST; forward and backward).[22] The TMT is designed to assess psychomotor speed, divided attention, and cognitive flexibility based on visual-motor tracking ability. The ST is designed to measure frontal lobe functions such as inhibitory function, cognitive control, cognitive flexibility. The DST is designed to evaluate attention for auditory input and is not influenced greatly by age, education, or intelligence. All tests were administered both prior to and 6 weeks following the first day of the intervention to evaluate changes in cognitive function in both groups.
2.6. Statistical analysis
All statistical analyses were performed using Statistical Package for the Social Science (SPSS) software v.20.0 (IBM, North Castle, NY). The sample size was calculated by mean difference in the TMT score between groups, as reported in the study by Choi et al[21] The effect size was 1.1, calculated by G∗Power software version 3.1, with α = 0.05 and β = 0.8. Kolmogorov–Smirnov test analyzed data normality. The Mann–Whitney U test was used to analyze differences in continuous variables between the CMDT and CMDT + AMST groups, while χ2 test and Fisher's exact test were used to compare categorical variables. The Wilcoxon signed rank test was used to analyze changes within each group. Analysis of covariance was used to compare changes between pre- and post-intervention between the 2 groups. The level of statistical significance was set at P < .05 level. All P-values were 2-tailed.
3. Results
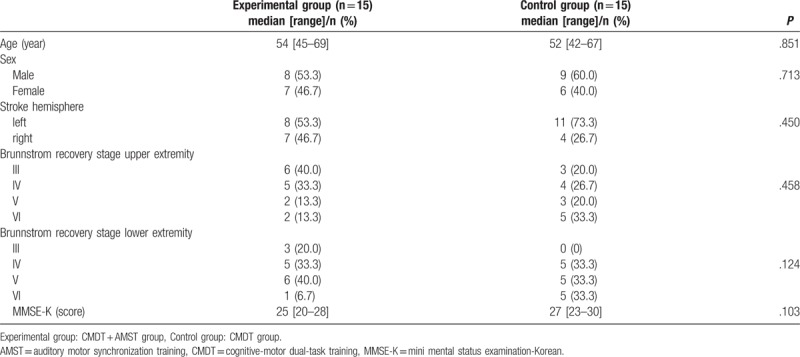
Between March and September 2016, a total of 42 participants with stroke were initially assessed for entry in the study (Fig. 1). Twelve participants, who did not meet the inclusion criteria of the study (n = 8) or disagreed to participate in the study (n = 4), were excluded. Finally, 30 participants were included in the study and randomly assigned to the experimental (n = 15) or control group (n = 15). All 30 participants completed the intervention (Fig. 1). The demographic characteristics of the participants in each group at base line are shown in Table 2. No significant differences in median age were observed between the CMDT + AMST group (54 years; range: 45–69 years) and CMDT group (52 years; range: 42–67 years) (P = .851). In addition, no significant differences in sex, stroke hemisphere, MMSE-K scores, or Brunnstrom recovery stage of the upper and lower extremities were observed (Table 2).
Table 2.
Demographic characteristics of the study groups.
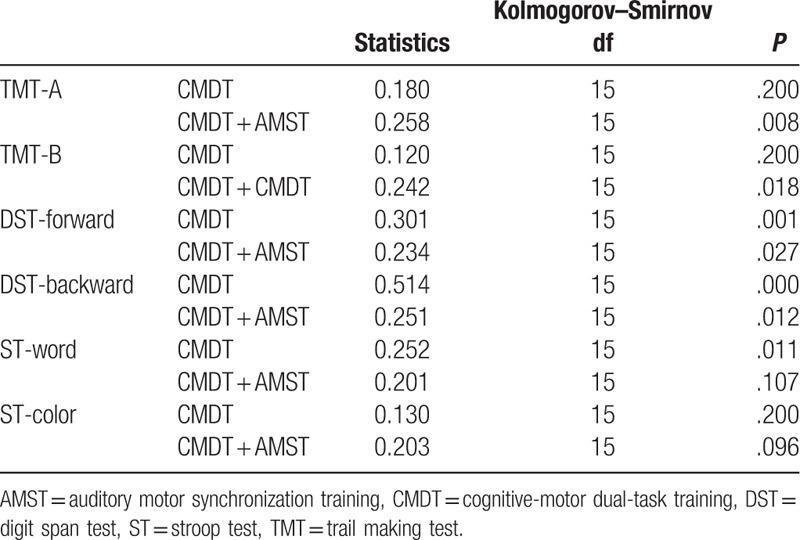
The normality of the primary data for each group at baseline is shown in Table 3. The data showed normality only for TMT-A (P = .200), TMT-B (P = .200), and ST-color (P = .200) in the CMDT group. While in the CMDT + AMST group, it showed normality only for ST-word (P = .107) and ST-color (P = .096). Since normality was not observed for both groups on the same data set, non-parametric methods analyzed results (Table 3).
Table 3.
Normality of the primary data on the groups.
The cognitive changes within each group are shown Table 4. In the CMDT group, there were significant changes in TMT-A and B (P = .001), DST-forward (P = .001), DST-backward (P = .000), ST-word (P = .001), and ST-color (P = .002) scores following the intervention (Table 2). In the CMDT + AMST group, there were also significant changes in TMT-A and B (P = .001), DST-forward, DST-backward (P = .001 each), ST-word, and ST-color (P = .001) scores following the intervention (Table 4).
Table 4.
Changes in cognitive functions within each groups.
The cognitive changes between 2 groups are shown Table 5. Significant differences in TMT-A (P = .001), DST-forward (P = .027), DST-backward (P = .002), and ST-word (P = .025) scores were observed between the groups (Table 5). No significant difference were found between 2 groups in TMT-B, ST-color after intervention (P > .05, Table 5).
Table 5.
Comparison of changes in cognitive functions between the 2 groups.
4. Discussion
Complex environments and multitasking may interfere with an individual's ability to focus attention following stroke, limiting the use of attentional strategies in specific situations.[17] Therefore, external cues, such as rhythmic auditory stimulation at a constant tempo, may require less effort and attention, and their use during more complex activities may facilitate dual-task performance.[23,24] In the present study, we examined the effect of CMDT + AMST involving the use of such cues on dual-task performance and cognitive functions such as attention, processing speed, and executive functioning.
Our findings indicated that the combined CMDT and AMST intervention was more effective in improving cognitive function than CMDT alone. Combined CMDT and AMST intervention resulted in significant improvement of DST-forward and DST-backward scores. These results indicated that the combined CMDT and AMST intervention, using rhythmic tempo, was effective in improving the concentration and auditory attention span. Although the TMT-B and ST-color scores was not significantly different after intervention, the TMT-A and ST-word scores was significant improved in the CMDT + AMST group. Also, it was more effective in improving attention capacity and attention. However, these results had limitation due to the small number of participants. Choi et al reported that the application of auditory feedback during dual-task training enhances cognitive attention and executive function in patients with stroke.[21] Similarly, our findings revealed that combined CMDT and AMST using rhythmic auditory cues exerted a positive effect on attention, memory, and executive function.
According a study by Moucha and Kilgard, the use of rhythmic cues with a constant tempo allows the listener to experience a pattern between sensory input and motor output that facilitates the production of neurotransmitters, increases cerebral cortical plasticity, and enhances cognitive processing.[25] Moreover, Rochester et al reported that motor dual-task training based on a rhythmic cue had positive effects on attentional capacity and motor performance in patients with Parkinson's disease.[26] Baker et al further reported that cues combining attentional strategy with a rhythmic beat improved executive functioning in patients with Parkinson's disease engaged in dual-task training.[24] Our findings are in accordance with the results of these previous studies, which collectively indicate that combined CMDT and AMST may be more effective than CMDT alone in improving attention, cognitive flexibility, and executive function following stroke.
This study applied the traditional CMDT method in addition to computer-based rhythmic tempo training. The study by De Luca et al provided evidence, although insufficient, to show that computerized cognitive rehabilitation is effective in improving the functioning of patients with severe acquired brain injury.[27] However, a recent study has shown that standard cognitive training combined with semi-immersive virtual reality improved the functioning of patients with neglect.[28] Therefore, it is necessary to verify whether applying the traditional CMDT method as a virtual reality-based cognitive training can positively affect the cognitive functions. The present study possesses some limitations of note. First, the sample size was relatively small because few patients at our institution were able to participate in the experimental condition. Second, this study did not examine long-term cognitive changes during a follow-up period. Therefore, further research in the form of long-term, multicenter studies is required to more fully elucidate the cognitive benefits of combined CMDT and AMST in patients with stroke. Third, this study examined the change of cognitive function using only the general assessment applied in the rehabilitation hospital setting. Therefore, further research will be necessary specific examination using f-MRI to know neural changes.
5. Conclusion
In summary, the combined intervention CMDT with AMST was shown to be an effective method for increasing cognitive functions of patients with stroke rather than only CDMT. Therefore, this method can be considered as a new approach to improve cognitive functions when try to CMDT training.
Author contributions
Conceptualization: Myoung-Ok Park, Sang-Heon Lee.
Data curation: Myoung-Ok Park.
Formal analysis: Myoung-Ok Park, Sang-Heon Lee.
Funding acquisition and investigation: Sang-Heon Lee
Investigation: Myoung-Ok Park, Sang-Heon Lee.
Methodology: Myoung-Ok Park.
Project administration: Myoung-Ok Park, Sang-Heon Lee.
Resources: Myoung-Ok Park, Sang-Heon Lee.
Software: Myoung-Ok Park, Sang-Heon Lee.
Supervision: Sang-Heon Lee.
Validation: Myoung-Ok Park, Sang-Heon Lee.
Visualization: Myoung-Ok Park, Sang-Heon Lee.
Writing – original draft: Myoung-Ok Park.
Writing – review & editing: Myoung-Ok Park, Sang-Heon Lee.
Footnotes
Abbreviations: AMST = auditory motor synchronization training, CMDT = cognitive-motor dual-task training, DST = digit span test, MMSE-K = mini mental status examination-Korean, ST = stroop test, TMT = trail making test.
This work was supported by the Soonchunhyang University Research Fund.
The authors have no conflicts of interest to disclose.
References
- [1].Bonita R. Epidemiology of stroke. Lancet 1992;339:342–4. [DOI] [PubMed] [Google Scholar]
- [2].Desmond DW, Moroney JT, Paik MC, et al. Frequency and clinical determinants of dementia after ischemic stroke. Neurology 2000;54:1124–31. [DOI] [PubMed] [Google Scholar]
- [3].Zorowitz RD, Gross E, Polinski DM. The stroke survivor. Disabil Rehabil 2002;24:666–79. [DOI] [PubMed] [Google Scholar]
- [4].Mercier L, Audet T, Hebert R, et al. Impact of motor, cognitive and perceptual disorders on ability to perform activities of daily living after stroke. Stroke 2001;32:2602–8. [DOI] [PubMed] [Google Scholar]
- [5].McDowell S, Whyte J, D’Esposito M. Working memory impairments in traumatic brain injury: evidence from a dual-task paradigm. Neuropsychologia 1997;35:1341–53. [DOI] [PubMed] [Google Scholar]
- [6].Li KZ, Roudaia E, Lussier M, et al. Benefits of cognitive dual-task training on balance performance in healthy older adults. J Gerontol A Biol Sci Med Sci 2010;65:1344–52. [DOI] [PubMed] [Google Scholar]
- [7].Kelly VE, Eusterbrock AJ, Shumway-Cook A. A review of dual-task walking deficits in people with Parkinson's disease: motor and cognitive contributions, mechanisms, and clinical implications. Parkinsons Dis 2012. 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Karatekin C, Couperus JW, Marcus DJ. Attention allocation in the dual task paradigm as measured through behavioral and psychophysiological responses. Psychophysiology 2004;41:175–85. [DOI] [PubMed] [Google Scholar]
- [9].Kizony R, Levin MF, Hughey L, et al. Cognitive load and dual-task performance during locomotion poststroke: a feasibility study using a functional virtual environment. Phys Ther 2010;90:252–60. [DOI] [PubMed] [Google Scholar]
- [10].Plummer-D’Amato P, Altmann LJ, Saracino D, et al. Interactions between cognitive tasks and gait after stroke: a dual task study. Gait Posture 2008;27:683–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Plummer P, Eskes G. Measuring treatment effects on dual-task performance: a framework for research and clinical practice. Front in Hum Neurosci 2015;28:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Zinn S, Bosworth HB, Hoenig HM, et al. Executive function deficits in acute stroke. Arch Phys Med Rehabil 2007;88:173–80. [DOI] [PubMed] [Google Scholar]
- [13].Pendlebury ST, Rothwell PM. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol 2009;8:1006–18. [DOI] [PubMed] [Google Scholar]
- [14].Vogels RL, Scheltens P, Schroeder Tanka JM, et al. Cognitive impairment in heart failure: a systematic review of the literature. Eur J Heart Fail 2007;9:440–9. [DOI] [PubMed] [Google Scholar]
- [15].Hanslmayr S, Sauseng P, Doppelmayr M, et al. Increasing individual upper alpha power by neurofeedback improves cognitive performance in human subjects. Appl Psychophysiol Biofeedback 2005;30:1–0. [DOI] [PubMed] [Google Scholar]
- [16].Koomar J, Burpee JD, DeJean V, et al. Theoretical and clinical perspectives on the interactive metronome: a view from occupational therapy practice. Am J Occup Ther 2001;55:163–6. [DOI] [PubMed] [Google Scholar]
- [17].Rochester L, Nieuwboer A, Baker K, et al. The attentional cost of external rhythmical cues and their impact on gait in Parkinson's disease: effect of cue modality and task complexity. J Neural Transm 2007;114:1243. [DOI] [PubMed] [Google Scholar]
- [18].Rossignol S, Jones GM. Audio-spinal influence in man studied by the H-reflex and its possible role on rhythmic movements synchronized to sound. Electroencephalogr Clin Neurophysiol 1976;41:83–92. [DOI] [PubMed] [Google Scholar]
- [19].Sergent C, Baillet S, Dehaene S. Timing of the brain events underlying access to consciousness during the attentional blink. Nat Neurosci 2005;8:1391–400. [DOI] [PubMed] [Google Scholar]
- [20].Greenspan SI, Benderly BL. The Growth of the Mind: And the Endangered Origins of Intelligence. Boston, MA: Da Capo Press; 1997. [Google Scholar]
- [21].Choi W, Lee G, Lee S. Effect of the cognitive-motor dual-task using auditory cue on balance of survivors with chronic stroke: a pilot study. Clin Rehabil 2015;29:763–70. [DOI] [PubMed] [Google Scholar]
- [22].Kang YW, Jang SM, Na DR. Seoul Neuropsychological Screening Battery Second Edition (SNSB-d). Incheon, South Korea: Hub R&C; 2012. [Google Scholar]
- [23].Ashoori A, Eagleman DM, Jankovic J. Effects of auditory rhythm and music on gait disturbances in Parkinson's disease. Front Neurol 2015;11:234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Baker K, Rochester L, Nieuwboer A. The immediate effect of attentional, auditory, and a combined cue strategy on gait during single and dual tasks in Parkinson's disease. Arch Phys Med Rehabil 2007;88:1593–600. [DOI] [PubMed] [Google Scholar]
- [25].Moucha R, Kilgard MP. Cortical plasticity and rehabilitation. Prog Brain Res 2006;157:111–389. [DOI] [PubMed] [Google Scholar]
- [26].Rochester L, Hetherington V, Jones D, et al. The effect of external rhythmic cues (auditory and visual) on walking during a functional task in homes of people with Parkinson's disease. Arch Phys Med Rehabil 2005;86:999–1006. [DOI] [PubMed] [Google Scholar]
- [27].De Luca R, Calabrò RS, Bramanti P. Cognitive rehabilitation after severe acquired brain injury: current evidence and future directions. Neuropsychol Rehabil 2006;25:1–20. [DOI] [PubMed] [Google Scholar]
- [28].De Luca R, Lo Buono V, Leo A, et al. Use of virtual reality in improving poststroke neglect: promising neuropsychological and neurophysiological findings from a case study. Appl Neuropsyhol Adult 2017. 1–5. [DOI] [PubMed] [Google Scholar]


