Abstract
Rationale:
Acute phlegmonous gastritis (PG) is a rare and often fatal condition mainly characterized by severe bacterial infection of the gastric wall. Case reports of PG over the past century average about 1 per year. Early diagnosis and immediate treatment are crucial to achieve positive outcomes.
Patient concerns:
A 47-year-old man was referred to our hospital because of abdominal pain, high fever, and vomiting for 4 days, with aggravation for 24 hours. Physical examination revealed epigastric abdominal pain, rebound pain, and abdominal wall tightness. Abdominal CT showed thickening of the stomach wall with edema and gas.
Diagnoses:
On the basis of symptoms and CT imaging findings, the patient was diagnosed with acute PG.
Interventions:
Antibiotic therapy and operation.
Outcomes:
The patient immediately underwent an operation after conservative treatment using antibiotics proved ineffective. The whole stomach was obviously swollen, and the anterior side and posterior wall of the stomach were nigrescent necrotic. Hence, total gastrectomy was performed followed by reconstruction (roux-en-y), and pus that accumulated in the stomach wall was cultured. At postoperative broad-spectrum antibiotic coverage, the patient finally recovered.
Lessons:
Acute PG is a rare infection of the gastric wall especially after antibiotic treatment. Given the fast progression of this disease, early recognition and immediate action are crucial to achieve positive outcomes.
Keywords: acute phlegmonous gastritis, clinical manifestation, pneumonia, prognosis, treatment
1. Introduction
Acute phlegmonous gastritis (PG) is a rare clinical disease mainly characterized by severe bacterial invasion of the gastric wall. Clinical manifestations of acute PG lack specificity, and patients often present with abdominal pain, nausea, vomiting, fever, and signs of infection. Early diagnosis is difficult, but this disease develops quickly and often with stomach wall necrosis and peritonitis. Acute PG has an extremely high mortality rate because diagnosis is often delayed or overlooked.[1,2] Before the advent of antibiotics, its mortality rate reached as high as 92%; with antibiotics, the mortality rate dropped to 48%.[3] However, immediate surgical intervention is needed to improve prognosis when antibiotic treatment is ineffective. In this paper, we report a case of acute PG in our hospital.
2. Case report
A 47-year-old male patient presented in our inpatient department with epigastric pain, high fever, and vomiting for 4 days, with aggravation for 24 hours. Four days prior, the patient complained of severe epigastric pain with high fever (highest temperature was 39.2 °C) and vomited. The patient also reported that he had a respiratory infection about 2 weeks ago, which improved after taking an oral anti-inflammatory drug, but he did not recover completely. The patient was sent to the local hospital and received the second-generation antibiotic cefuroxime, but the condition was not improved. Twenty-four hours ago, the condition progressed, and he was sent to our hospital. The patient had a history of 30 years of alcohol intake of 250 g/d and had a gastric ulcer for many years without regular treatment.
Upon admission, the temperature was 39.0 °C, P was 136 times/min, and blood pressure was 136/85 mmHg. Physical examination revealed difficult abdominal breathing, epigastric pain, rebound pain, abdominal wall tightness, and weak bowel movement (0–1 times/min). Blood biochemical tests showed that the white blood cell count was 6.41 G/L and the Neut% was 87.1%. Contrast-enhanced computed tomography (CT) indicated that the whole gastric wall was edematous and thickened, but no sign of perforation was observed (Fig. 1).
Figure 1.
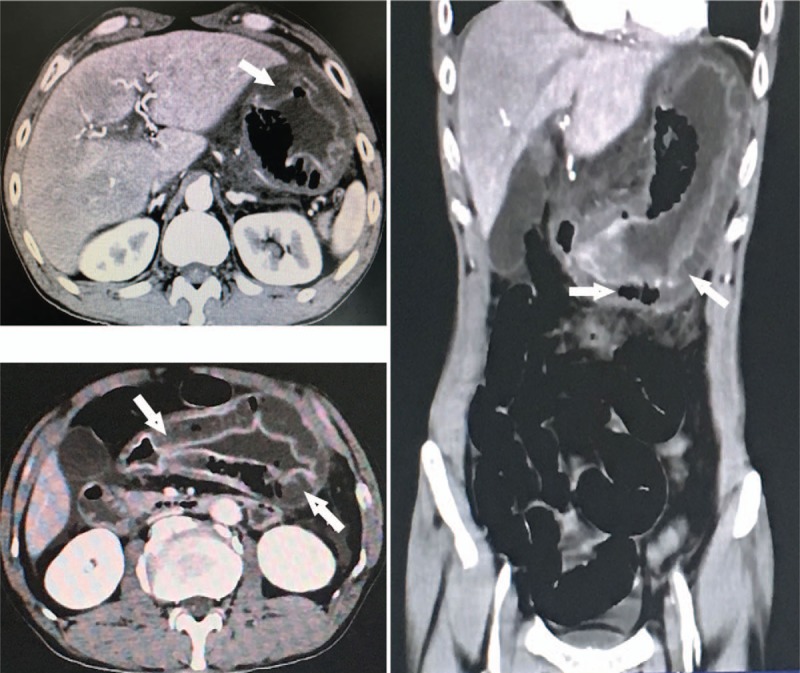
CT indicated extensive diffusely mural thickness in the region of the whole stomach with low-density fluid and gas within the wall. Ample exudate was found around the stomach. CT = computed tomography.
After admission, we administered Cefperazone–Sulbactam and tinidazole anti-infection, PPI acid suppression therapy, and rehydration treatment. However, we decided to operate because abdominal pain intensified, vomiting occurred repeatedly, and the vomitus contained fester during the treatment. The operation revealed more abscess fluid surrounding the stomach wall. The anterior, side, and posterior wall of the stomach were nigrescent necrotic (Fig. 2). Hence, total gastrectomy was performed followed by reconstruction (roux-en-y). The specimen showed a considerable amount of pus accumulated in the stomach wall, and we sent the pus to culture (Fig. 3). The patient was sent to the intensive care unit, given Cefperazone–Sulbactam and tinidazole for anti-infection, nutrition support, and rehydration treatment. After 24 days of treatment, the patient was transferred back to the ordinary ward to continue treatment and at last recovered.
Figure 2.
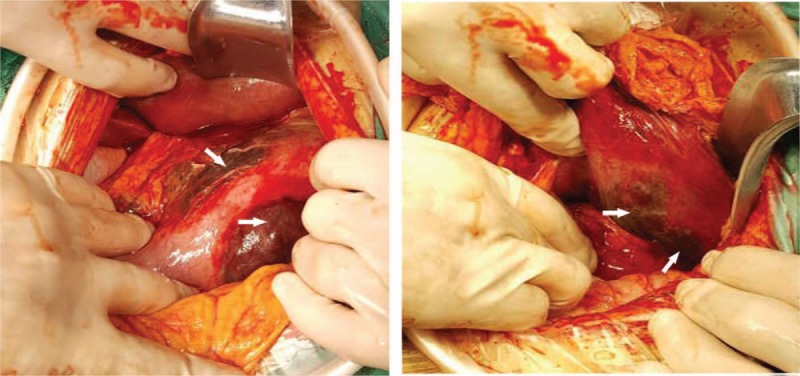
Entire stomach was clearly swollen. The anterior, side, and posterior wall of the stomach were nigrescent necrotic. Sanguinopurulent effusion fluid surrounded the stomach.
Figure 3.

Section of the specimen showing abundant purulent fluid accumulated in the wall.
Biopsy showed gastric mucosal necrosis, and necrosis was found on areas of the mucosal muscularis, muscularis, and serosa layer, where extensive neutrophil infiltration was present. Abscess formations were also found in the said areas, and the stomach and the greater omentum were phlegmonous (Fig. 4). Tissue culture specimens were positive for hemolytic streptococcus.
Figure 4.
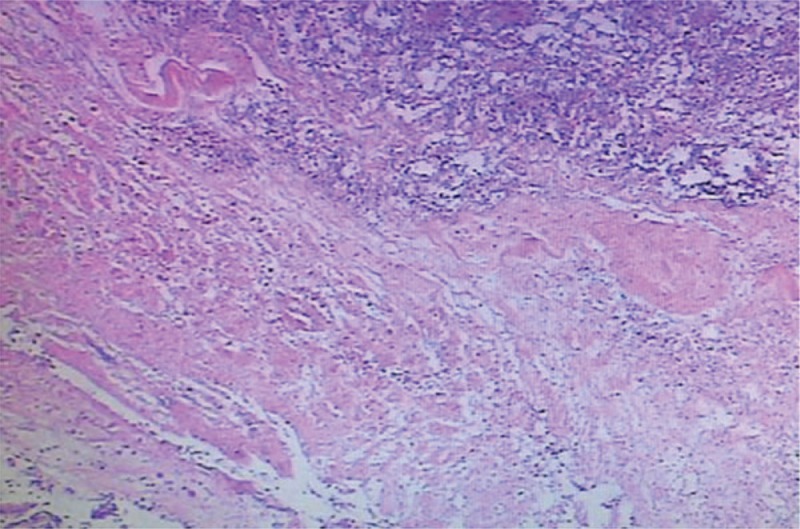
Gastric mucosal necrosis was found on areas of the mucosal muscularis, muscularis, and serosa layer, where extensive neutrophil infiltration was present. Abscess formations were also found in the said areas, and the stomach and the greater omentum were phlegmonous.
3. Discussion
Acute PG was originally described by Cruveilhier in the early 18th century, and an average of 1 case report per year has appeared over the last 60 years.[4–6] The disease affects all age groups and is highly common in adults in their 50s to 70s, and the male-to-female ratio is 2:1.[7] Acute PG is rare clinically, especially since the use of antibiotics, but becomes urgent and develops quickly once it occurs. With the high mortality of this disease, early recognition and immediate action are crucial. With <500 cases reported in the literature, it requires the attention of medical staff.
At present, acute PG's cause is not entirely clear presumably due to fester bacterium invading the stomach. Hemolytic streptococcus is reportedly found in approximately 70% of cases, followed by Staphylococcus aureus, Pneumococcus, and Enterococcus.[8] Bacterial invasion of the gastric wall can be caused by gastric ulcer, chronic gastritis, and the like, with the pathogenic bacteria of the pharynx directly infringing into the damaged mucosa; respiratory tract infection or other infection, with the pathogenic bacteria entering the gastric wall through blood flow; the pathogenic bacteria entering the gastric wall through the lymphatic system in the case of cholecystitis and peritonitis. Furthermore, drinking, malnutrition, and being elderly are often cited as causes of the disease.[9] Considering this case, the patient had the predisposing factor long-term alcohol consumption and gastritis, and he has not fully recovered from his recent respiratory tract infection (one of main pathogenic bacteria was hemolytic streptococcus). Considering that hemolytic streptococcus was cultivated from the percolate, we presumed that the acute PG was caused by pulmonary pathogen invasion into the stomach in this patient.
The pathophysiological process is chiefly caused by the bacteria's invasion of the submucosa, propagating and diffusing into the mucosa and serous membrane, and is classified into diffuse and localized types according to the lesion range.[10,11] The diffuse type is more common clinically than the localized type, and it is characterized by dark red stomach wall and diffuse thickening; when the stomach wall is squeezed, pus outflow occurs from the gastric wall. This type can also cause gastric cavity expansion and gastric wall perforation under severe circumstances. The localized type features gastric mucosal hyperemia and erosion, ulceration, necrosis, or bleeding. The localized type is associated with a lower mortality rate than the diffuse type (10% vs 54%, respectively).[12] In our patient, the stomach wall was obviously swollen, and necrosis was found in parts of the stomach. The postoperative section of the abscess accumulated in the stomach wall. Hence, this case belonged to the diffuse type.
An early diagnosis of PG is difficult due to the nonspecific nature of its clinical manifestations, including acute abdominal disease, sudden onset of abdominal pain, high fever, chills, nausea, and vomiting. Thus, differentiating PG from an acute abdomen (e.g., perforation peritonitis, acute cholecystitis, and acute pancreatitis) is necessary. With the development of the disease, body temperature can increase, peritoneal irritation signs become obvious, such as abdominal tenderness, rebound pain, and the vomitus can change to abscess fluid.[5,9,13] Abdominal CT typically reveals the following characteristic findings of PG: thickening of the gastric wall, low-intensity areas within the gastric wall (indicative of an abscess), and gas accumulation.[7] The patient's clinical manifestation included abdominal pain, epigastric peritonitis, and the feature of CT.[11] Considering that the purulent patient vomited, we made a diagnosis of acute PG, having distinguished it from other acute abdominal diseases.
Acute PG has an extremely high mortality rate, and the key to successful treatment is early diagnosis and treatment. Before the advent of antibiotics, the fatality rate was as high as 83% to 92%, and the mortality rate reduced to 48% even after antibiotics became available.[3] In addition, nutritional support and rehydration are very important to the success of the treatment.[14–16] However, if conservative treatment effect is ineffective, surgery should be performed immediately to avoid aggravation of the state of the illness. The condition of the patient in our center aggravated after conservative treatment. Hence, emergency operation was performed, and postoperative support treatment was provided. Finally, the patient recovered.
4. Conclusion
Acute PG lacks specific clinical performance, and abdominal CT is helpful for both early diagnosis and detecting complications. Once acute PG is detected, antibiotic treatment is important, but if this treatment fails, surgery should be performed immediately to improve the prognosis. At present, given the use of antibiotics, the incidence rate is extremely low. However, once the disease occurs, it rapidly progresses and has an extremely high fatality rate. Thus, it requires serious attention by clinicians.
Acknowledgments
This study was approved by the ethics committee at the Affiliated Hospital of Guizhou Medical University in China. The patient provided informed consent.
Author contributions
Conceptualization: Qian Wang, Haibin Wang, Zhiqiang Yan,Hongxin Yang, Haitao Xie.
Data curation: Hongxin Yang, Jiaju Chen.
Investigation: Hongxin Yang.
Writing – original draft: Hongxin Yang.
Writing – review and editing: Hongxin Yang, Qian Wang, Haibin Wang, Zhiqiang Yan.
Footnotes
Abbreviations: CT = computed tomography, PG = phlegmonous gastritis.
The authors have no conflicts of interest to disclose.
References
- [1].Min SY, Kim YH, Park WS. Acute phlegmonous gastritis complicated by delayed perforation. World J Gastroenterol 2014;20:3383–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kim KH, Kim CG, Kim YW, et al. Phlegmonous gastritis with early gastric cancer. J Gastric Cancer 2016;16:195–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Fan JQ, Liu DR, Li C. Phlegmonous gastritis after esophagectomy: a case report. World J Gastroenterol 2013;19:1330–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Liu YJ, Siracuse JJ, Gage T, et al. Phlegmonous gastritis presenting as portal venous pneumatosis. Surg Infect (Larchmt) 2013;14:221–4. [DOI] [PubMed] [Google Scholar]
- [5].Paik DC, Larson JD, Johnson SA, et al. Phlegmonous gastritis and group a streptococcal toxic shock syndrome in a patient following functional endoscopic sinus surgery. Surg Infect (Larchmt) 2010;11:545–9. [DOI] [PubMed] [Google Scholar]
- [6].Cortes-Barenque F, Salceda-Otero JC, Angulo-Molina D. Acute phlegmonous gastritis. Rev Gastroenterol Mex 2014;79:299–301. [DOI] [PubMed] [Google Scholar]
- [7].Nomura K, Iizuka T, Yamashita S. Phlegmonous gastritis secondary to superior mesenteric artery syndrome. SAGE Open Med Case Rep 2015;1:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Seidel RH, Burdick JS. Gastric leiomyosarcoma presenting as a gastric wall abscess. Am J Gastroenterol 1998;93:2241–4. [DOI] [PubMed] [Google Scholar]
- [9].Kato K, Tominaga K, Sugimori S, et al. Successful treatment of early-diagnosed primary phlegmonous gastritis. Intern Med 2015;54:2863–6. [DOI] [PubMed] [Google Scholar]
- [10].Aviles JF, Fernandez SJ, Barcena R, et al. Localized phlegmonous gastritis: endoscopic view. Endoscopy 1988;20:38–9. [DOI] [PubMed] [Google Scholar]
- [11].Sood BP, Kalra N, Suri S. CT features of acute phlegmonous gastritis. Clin Imaging 2000;24:287–8. [DOI] [PubMed] [Google Scholar]
- [12].Kim GY, Ward J, Henessey B, et al. Phlegmonous gastritis: case report and review. Gastrointest Endosc 2005;61:168–74. [DOI] [PubMed] [Google Scholar]
- [13].Kim HS, Hwang JH, Hong SS, et al. Acute diffuse phlegmonous esophagogastritis: a case report. J Korean Med Sci 2010;25:1532–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Alonso JV, Gutiérrez Solis MA, Vara Morate FJ, et al. Gastric wall abscess presenting as thoracic pain: rare presentation of an old disease. Ann Gastroenterol 2013;26:360–2. [PMC free article] [PubMed] [Google Scholar]
- [15].Odai T, Hibino T. The abdominal ultrasonographic appearance of acute phlegmonous gastritis. Kansenshogaku Zasshi 2016;90:113–9. [DOI] [PubMed] [Google Scholar]
- [16].Kelly SG, Vanagunas AD, Dinh MH, et al. Phlegmonous gastritis: a previously unknown complication of listeria monocytogenes infection. Infect Dis Clin Pract 2016;24:17–9. [Google Scholar]


