Abstract
Rationale:
Simultaneous presentation of peripheral infiltrates, which can be easily misidentified as satellite lesions, is rarely observed in patients with acute infectious keratitis.
Patient concerns:
A 70-year-old woman was referred to our clinic due to acute mucopurulent keratitis following application of a therapeutic soft contact lens for the treatment of epithelial defects caused by entrance of soil foreign bodies into the eye. The patient was diagnosed with Pseudomonas keratitis, following which she was treated with alternating administration of fourth-generation fluoroquinolone (Vigamox) and 5% fortified ceftazidime eyedrops every 2 hours. Although infectious keratitis rapidly improved, discrete catarrhal infiltrates at the corneolimbal junction (10- to 2-o’clock and 7- to 8-o’clock positions) were rapidly aggravated, forming bead-like stromal pustules inversely proportional to the extent of Pseudomonas keratitis.
Diagnosis:
Acute exacerbation of staphylococcal catarrhal infiltration associated with treatment for Pseudomonas aeruginosa keratitis.
Interventions:
Addition of 1% prednisone acetate eyedrops (Pred Forte) four times per day.
Outcomes:
Dramatic improvement was observed at the sites of catarrhal infiltration without recurrence of infectious keratitis.
Lessons:
Clinicians should thus remain aware of the risk for co-occurring non-infectious, immune-related keratitis, as treatment for infectious keratitis may induce significant aggravation of non-infectious keratitis.
Keywords: catarrhal infiltration, keratitis, marginal, Pseudomonas aeruginosa, Staphylococcus
1. Introduction
Staphylococcus-related marginal keratitis is a noninfectious, immune-related peripheral corneal disorder that is relatively common and self-limiting. Although Staphylococcus aureus can be identified in lid cultures in 90% of healthy participants, deposition of immune complexes into the peripheral cornea is likely to induce an immune response or type III hypersensitivity reaction.[1,2] In immunocompetent patients, immune reactions involving marginal catarrhal infiltrates are usually caused by bacterial antigens, teichoic acid, or protein A of Staphylococcus aureus (not found in Staphylococcus epidermidis) fused to the Fc portion of antibodies at the corneal limbus.[2–4] However, non-S aureus catarrhal infiltrates have also been observed.[5]
Pseudomonas aeruginosa keratitis is a common corneal microbial infection often associated with the use of contact lenses.[6]P aeruginosa penetrates the corneal epithelium at the site of the defect, following which it induces rapid damage to the corneal stroma. During this process, several proteases such as alkaline protease, elastase A, elastase B, and P aeruginosa small protease (PASP) may induce considerable corneal damage.[7]
In the present paper, we discuss the case of a patient in whom P aeruginosa keratitis rapidly improved following treatment with fourth-generation fluoroquinolone and fortified third-generation cephalosporin eyedrops. However, such treatment resulted in rapid aggravation of catarrhal infiltrates at the corneal limbus.
2. Case presentation
A 70-year-old woman presented to our hospital with ocular pain and redness of the left eye that had persisted for 3 days. Her symptoms were initiated by the entrance of soil foreign bodies into the left eye, and had become more aggravated after applying a therapeutic contact lens at a local ophthalmic clinic the day before referral. She had no history of eye surgery or keratitis in either eye. During the initial examination, we evaluated unaided visual acuity in the patient's left eye, which was capable of distinguishing hand-motion only and did not respond to attempts at correction. Slit-lamp examination revealed a central, well-demarcated, mucopurulent epithelial defect (4.0 × 4.5 mm) with thick stromal infiltrations. Creamy white subepithelial infiltrates were observed at the corneolimbal junction (10- to 2-o’clock and 7- to 8-o’clock positions), although no epithelial defects were observed over either lesion. In addition, the patient exhibited 1+ blepharitis on both upper and lower eyelids. The anterior chamber exhibited 3+ cellular reaction with mild cyclitic membrane formation (Fig. 1A and B). Corneal scrapings and cultures were obtained using a No. 15 Bard-Parker blade (Aspen Surgical, Caledonia, MI) with cotton-tipped swabs. Initial corneal scrapings were positive for gram-negative bacilli. The patient was hospitalized and treated with 0.5% moxifloxacin (Vigamox, Alcon Laboratories, Fort Worth, TX), 5% (50 mg/mL) fortified ceftazidime (Tazime injection, Hanmi Pharma, Seoul, Korea), and 5% (50 mg/mL) vancomycin (Hanomycin injection, Samjin Pharm, Seoul, Korea) eyedrops. For the loading dose, eyedrops were instilled every 10 minutes for 1 hour, every 30 minutes for 2 hours, and hourly for 6 hours. Subsequently, antibiotic eyedrops were alternatively instilled bihourly.
Figure 1.
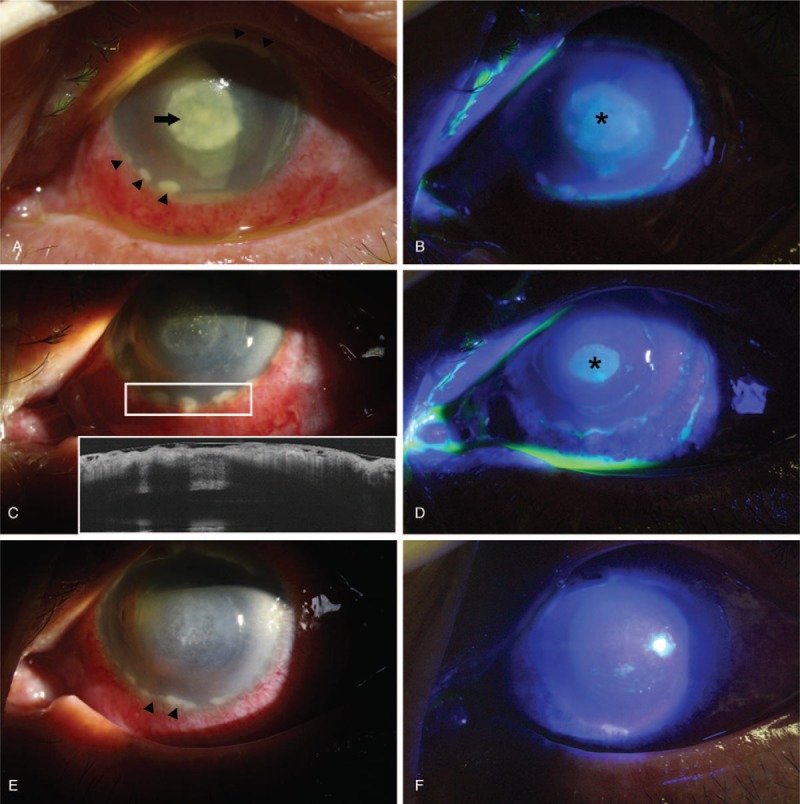
(A) Slit-lamp photograph of initial presentation. Central, well-demarcated mucopurulent keratitis was apparent (arrow). Well-demarcated round infiltrates were noted at the 6-to-8-o’clock position (arrow heads). (B) Fluorescein staining revealed an elliptical epithelial defect of 4.0 × 4.5 mm in size (asterisk). (C) Five days after admission, considerable improvement in the central mucopurulent lesion had occurred, although aggravation of the corneolimbal infiltrates was noted, along with additional infiltrates at the 6- and 5-o’clock positions (white inlet). Anterior segment optical coherence tomography revealed elevation of the round infiltrates. (D) Fluorescein staining revealed a decrease in the size of the epithelial defect (asterisk), although corneolimbal infiltrates overlying the epithelium remained intact. (E) On the day following initiation of treatment with 1% prednisone acetate eyedrops (arrow heads), considerable improvement in corneolimbal infiltrates was observed. (F) Fluorescein staining revealed complete healing of the epithelium at the site previously affected by P aeruginosa keratitis.
On the fifth day after hospitalization, the central epithelial defect had shrunk to 2.5 × 1.8 mm in size, and mucopurulent discharge had markedly decreased. Although the anterior chamber exhibited 2+ cells without visible cyclitic membranes, corneolimbal infiltrates were refractory to antimicrobial treatments. Marked aggravation of the infiltrates, which had formed a bead-like pattern elevated from the corneal surface, was observed (Fig. 1C and D).
On the sixth day after admission, aggravation of corneolimbal lesions had again increased, and band-like infiltration was observed along the limbus. Corneal scrapings and cultures were again obtained to evaluate infiltrates affecting the conjunctiva near the corneal limbus, following which corneal biopsy of infiltrates at the 11-o’clock position was performed for histological analysis. The surface of the eyelid and upper lid cilia were also swabbed to obtain cultures for the identification of staphylococcal colonization. Eight days after admission, corneal scrapings were negative for microbial organisms, although S epidermidis was identified in cultures. Corneal biopsy of the limbal lesions revealed numerous neutrophilic infiltrates around the peripheral lesion. We suspected that the patient's peripheral lesions were marginal staphylococcal infiltrates, following which she was treated with 1% prednisone acetate eyedrops (Pred Forte, Allergan, Irvine, CA) 4 times per day while maintaining the previous antibiotic eyedrop regimen (Vigamox, 5% fortified vancomycin and ceftazidime 4 times per day). One day after the treatment with steroid eyedrops, considerable improvements in pain and redness were observed. Complete healing of the epithelial defect was observed on day 11 (Fig. 1F). Two weeks after the initiation of steroid eyedrop treatment, corneolimbal lesions had completely resolved, without recurrence of bacterial keratitis. However, thinning of the central cornea was apparent.
3. Discussion and conclusion
In the present case, multiple corneolimbal infiltrates and severe mucopurulent keratitis due to non-staphylococcal, P aeruginosa infection were observed at the time of presentation. Fortunately, the patient stated that the acute exacerbation of ocular pain and redness occurred following application of the therapeutic contact lens, and—given the history of soil foreign body entrance in the eye—Pseudomonas infection was suspected. Therefore, both fortified third-generation cephalosporin (5% ceftazidime) and fourth-generation synthetic fluoroquinolone (moxifloxacin 0.5%) eyedrops were alternatively loaded prior to obtaining scraping report or culture findings. Signs and symptoms of Pseudomonas keratitis dramatically improved following initiation of these treatments.
Although multiple peripheral infiltrates were observed during the initial examination, these lesions were overlooked as satellite lesions of central keratitis or reactive changes induced by severe keratitis. Therefore, paradoxical rapid aggravation of corneolimbal catarrhal infiltrations despite dramatic improvement in central Pseudomonas keratitis appeared unusual. In addition, although improvements were observed in the central epithelial defects and surrounding areas of infiltration, rapid aggravation of conjunctival edema, hyperemia, and peripheral corneal infiltrates was observed for several days. Based on these findings, I suspected that the patient's symptoms may have been associated with other conditions such as scleritis or autoimmune-related peripheral ulcerative keratitis. However, thorough re-evaluation of initial slit-lamp images revealed that the initial peripheral lesions were separated from the limbus (lucid interval), while no epithelial defects were observed over any of the lesions. Furthermore, S epidermidis was isolated from the second corneoconjunctival culture, despite negative cultures for the eyelid and cilia swabs. As Staphylococcus aureus has also been previously identified in the conjunctiva and eyelid,[8] I strongly suspected the co-occurrence of marginal catarrhal infiltrates due to noninfectious, immune-related keratitis.
Moreover, although staphylococcal catarrhal infiltrates were strongly suspected, the decision to administer corticosteroids during culture-proven bacterial keratitis was complex due to the risk of acute exacerbation of keratitis and reactivation of remnant Pseudomonas. In addition, the use of steroid eyedrops during hospitalization and the treatment for bacterial keratitis remains controversial, as this may lead to progression of corneal thinning or damage.[9] Two weeks after the initiation of treatment with 1% prednisone acetate eyedrops in the present case, marked thinning of the area in which Pseudomonas keratitis had developed was confirmed using anterior segment optical coherence tomography, although the infiltrates at the corneolimbal junction had not yet completely resolved.
The mechanism underlying the findings observed in the present case remains to be determined, as no similar cases can be found in the literature. However, a previous study indicated that treatment with the LasA protease of P aeruginosa (a staphylolytic endopeptidase) significantly improved clinical scores in a rabbit model of Staphylococcal keratitis.[10] Although Staphylococcus colonization was not observed on the eyelid in the present study (culture-negative result at eyelid swab and cilia), secreted protease from Pseudomonas organisms in the corneal stroma may have suppressed Staphylococcus colonization on the eyelid or conjunctiva. While successful treatment eliminated Pseudomonas aeruginosa, the titer of staphylolytic protease may have abruptly decreased. In addition, broad-spectrum coverage of antimicrobial agents may have disturbed the normal flora of the ocular surface or eyelid, enabling the selective and explosive growth of a resistant strain of Staphylococcus and potentiating exposure of the cornea to Staphylococcus antigens.
In conclusion, simultaneous presentation of peripheral infiltrates, which can be easily misidentified as satellite lesions, is rarely observed in patients with acute infectious keratitis. Clinicians should thus remain aware of the risk for co-occurring noninfectious, immune-related keratitis, as treatment for infectious keratitis may induce significant aggravation of noninfectious keratitis.
Author contributions
Conceptualization: Jong Hwa Jun.
Data curation: Jong Hwa Jun.
Formal analysis: Seung Pil Bang.
Investigation: Seung Pil Bang, Jong Hwa Jun.
Resources: Jong Hwa Jun.
Supervision: Jong Hwa Jun.
Validation: Jong Hwa Jun.
Writing – original draft: Seung Pil Bang.
Writing – review & editing: Seung Pil Bang.
Footnotes
Abbreviation: PASP = Pseudomonas aeruginosa small protease.
Ethics approval and consent to participate: This report was approved by the Institutional Review Board (IRB) of Keimyung University Dongsan Medical Center (IRB no. 2018-02-028) and was performed in accordance with the tenets of the Declaration of Helsinki. Furthermore, the patient signed a written informed consent form.
This research was supported by the Keimyung University Research Grant of 2018. The authors have no conflicts of interest to disclose.
References
- [1].Ficker L, Ramakrishnan M, Seal D, et al. Role of cell-mediated immunity to staphylococci in blepharitis. Am J Ophthalmol 1991;111:473–9. [DOI] [PubMed] [Google Scholar]
- [2].Ficker L, Seal D, Wright P. Staphylococcal infection and the limbus: study of the cell-mediated immune response. Eye (Lond) 1989;3(pt 2):190–3. [DOI] [PubMed] [Google Scholar]
- [3].Boto-de-los-Bueis A, del Hierro Zarzuelo A, Garcia Perea A, et al. Staphylococcus aureus blepharitis associated with multiple corneal stromal microabscess, stromal edema, and uveitis. Ocul Immunol Inflamm 2015;23:180–3. [DOI] [PubMed] [Google Scholar]
- [4].Mondino BJ, Laheji AK, Adamu SA. Ocular immunity to Staphylococcus aureus. Invest Ophthalmol Vis Sci 1987;28:560–4. [PubMed] [Google Scholar]
- [5].Mannis MJ, Holland EJ. Cornea. Philadelphia: Elsevier Saunders; 2016. Bacterial Keratitis; pp. 875-901. [Google Scholar]
- [6].Poggio EC, Glynn RJ, Schein OD, et al. The incidence of ulcerative keratitis among users of daily-wear and extended-wear soft contact lenses. N Engl J Med 1989;321:779–83. [DOI] [PubMed] [Google Scholar]
- [7].Matsumoto K, Shams NB, Hanninen LA, et al. Cleavage and activation of corneal matrix metalloproteases by Pseudomonas aeruginosa proteases. Invest Ophthalmol Vis Sci 1993;34:1945–53. [PubMed] [Google Scholar]
- [8].Ueta M, Sotozono C, Takahashi J, et al. Examination of Staphylococcus aureus on the ocular surface of patients with catarrhal ulcers. Cornea 2009;28:780–2. [DOI] [PubMed] [Google Scholar]
- [9].Ni N, Srinivasan M, McLeod SD, et al. Use of adjunctive topical corticosteroids in bacterial keratitis. Curr Opin Ophthalmol 2016;27:353–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Barequet I, Safrin M, Bourla N, et al. Pseudomonas aeruginosa LasA protease as a therapeutic agent in staphylococcal keratitis. Invest Ophthalmol Vis Sci 2004;45:4947–14947. [Google Scholar]


