Supplemental Digital Content is available in the text
Keywords: alcohol use, community-dwelling human immunodeficiency virus–positive patients, Rational Emotive Health Therapy
Abstract
Background:
Patients who have tested positive for the human immunodeficiency virus (HIV) and who also experience alcohol use disorder (AUD) symptoms have worse clinical outcomes when compared with those who do not have AUD symptoms. The objective of the present study was to determine the effect of rational emotive health therapy (REHT) on AUD among community-dwelling, HIV-positive patients in the Southeastern region of Nigeria.
Methods:
The research design included a pretest/post-test control group with a total of 124 community-dwelling, HIV-positive patients with AUD symptoms participating in the study. The measures employed for data collection included Alcohol-related Irrational Beliefs Scale (AIBS) and Alcohol Use Disorder Scale (AUDS). Repeated measures analysis of variance was used for statistical analysis.
Results:
The result obtained at the initial assessment indicated that AUD was severe. Furthermore, REHT intervention led to a significant reduction in AUD symptoms, as shown by a reduction in AUDS and AIBS scores with time in the treatment group compared to those in the waitlist control group after the intervention. Also, the effect of REHT was positively maintained in the treatment group participants at follow-up assessment.
Conclusion:
The presence of HIV symptoms alone does not cause HIV-positive patients to be dependent on alcohol; rather, irrational beliefs about the infection may contribute to unhealthy feelings and abuse of alcohol. Rational emotive health therapy is an effective approach that can be employed by therapists and health counselors in helping HIV-positive patients to think rationally about themselves and work to be able to overcome HIV-related, as well as alcohol-related, irrational beliefs.
1. Introduction
Alcohol is the most commonly used psychoactive substance and is associated with risks for sexually transmitted infections, including human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS).[1] As observed by Weinhardt and Carey,[2] alcohol use is related to sexual risks in several populations, especially among those with the highest rates of HIV infections. In recent time, HIV-positive patients have increased prevalence and frequency of medical, psychiatric, and substance-use disorders, which result in increased mortality.[3] Alcohol use, for instance, progressively facilitates HIV transmission by influencing people's behavior.[3] Several people at risk of or already infected with HIV depend on alcohol, which contributes to the difficulties in preventing and managing the spread of the infection, as well as treating infected patients.[4] Cook and Clark[5] noted that alcohol elevates sexual risks through multiple channels, including risk-taking personality characteristics, drinking environments, expectations regarding the effects of alcohol on risk-taking, and the psychogenic effects of alcohol on decision making. The association between drinking and HIV transmission has led to interventions, which address the connection between alcohol use and HIV risk behaviors.[6]
Alcohol use disorder is a pattern of alcohol use, which involves difficulty in controlling drinking, being preoccupied with alcohol, continuing to use alcohol even when it causes problems, drinking more to get the same effect, or experiencing withdrawal symptoms when rapidly decreasing drinking.[7,8] Alcohol use disorder symptoms can range from mild to moderate or severe. The severity is based on the number of symptoms an individual experiences. Alcohol use disorder represents one of the leading causes of preventable death, illness, and injury among HIV-positive patients in many societies around the world. This is because AUD is associated with a variety of unpleasant health and social consequences, including liver cirrhosis, mental illness, several types of cancer, pancreatitis, and damage to the fetus among pregnant women.[7,8] Alcohol use disorder symptoms are also strongly related to social consequences such as drinking and driving injuries and fatalities, aggressive behavior, family disruptions, and reduced industrial productivity.[7,8] The World Health Organization[8] noted that reviews of the international literature on disease and death related to alcohol have identified at least 61 different types of injury, illness, or death, which are potentially caused by AUD. Studies have also shown that testing positive for HIV[9] is independently associated with AUD.
In treating HIV-positive patients, it is commonly advocated that attempts to address alcohol use disorder should precede initiation of ART.[10] However, the advent of highly active antiretroviral therapy has resulted in improved virological, immunological, and clinical outcomes, including reduced mortality rates in individuals infected with HIV.[11] Studies have shown that HIV-positive patients who are suffering from AUD symptoms may delay testing for HIV, accessing appropriate medical care, and initiating ART, which may hasten disease progression to full-blown AIDS.[3,4,6] Studies have also shown that individuals who drink are significantly more likely to become HIV-positive[12]; people who drink more heavily and report being intoxicated in sexual situations also report less condom use and more concurrent sex partners, demonstrating higher risk for HIV[13,14]; and HIV-positive people undergoing treatment concurrent with AUD often render the treatment ineffective because they frequently fail to adhere to the strict treatment regimens necessary to achieve control of the infection.
Although individuals have learned much about the nature of HIV—the course of the disease, routes of transmission, and strategies to suppress viral replication and disease progression—the epidemic continues alarmingly, particularly in developing countries like Nigeria.[2,15] The authors further observed that one of the factors contributing to the difficulties of preventing the spread of the infection and treating infected patients is the tendency for AUD symptoms among people who are at risk for infection and/or those who are already infected.[2,15] In addition, alcohol-HIV/AIDS literature[2] has shown the need to address AUD as medical condition for treating HIV infection. Different treatment measures, including social skills training, self-control training, and behavioral techniques such as covert sensitization, behavioral contracting, and in particular, cognitive therapy, are often been employed to assist those suffering from AUD symptoms.[17] However, cognitive-behavioral approaches to the reduction of AUD symptoms are known to be efficacious.[17] Meanwhile, studies[17–20] have shown that one form of therapy, which has been effective in the treatment of many types of psychological problems is rational emotive behavior therapy (REBT). Ellis and Griege[21] maintain that emotional disturbance is correlated with dysfunctional cognitions termed irrational beliefs. Ellis noted that such irrational beliefs may include catastrophizing a situation, judging oneself as worthless, or taking simple desires or preferences and turning them into demands. With regard to AUD symptoms, the irrational beliefs may be the following: I cannot stand avoiding a drink; I cannot function without a drink; I am not strong enough to resist alcohol; I cannot stand the deprivation of my desire for a drink; and I am a horribly deprived person if I cannot have a drink.[16] REBT helps to decrease emotional distress by promoting more realistic, logical, and flexible thinking.[21,22] Ellis postulated that if people experience negative behavioral and emotional consequences, more positive consequences will emerge once irrational beliefs are disputed and replaced by new effective beliefs. According to Ellis, this is true even in the case of AUD symptoms.[23]
The current study illustrates the development of rational emotive health therapy (REHT) from the principles of REBT. Rational emotive health therapy is a form of cognitive behavioral health therapy for the management of AUD symptoms. It is possible that REHT may help community-dwelling, HIV-positive patients who experience AUD symptoms to reduce their alcohol use. To that end, the purpose of the present study was to determine the effect of REHT on alcohol use among community-dwelling, HIV-positive patients. We therefore hypothesized that there will be an effect of REHT on measurable AUD symptoms among HIV-positive patients.
2. Methods
2.1. Ethical approval
The Department of Educational Foundations at the University of Nigeria, Nsukka, Nigeria provided the researchers with approval to conduct the study. The researchers conformed to the Declaration of Helsinki[24] and the APA ethical principles of psychological research with human participants.[25]
2.2. Study area
The study was conducted in Enugu State, Nigeria.
2.3. Design
A pretest/post-test control group design was used.
2.4. Participants
The participants included 124 individuals who were identified as community-dwelling, HIV-infected patients who experienced AUD symptoms and were residents of the Southeastern region of Nigeria (Fig. 1). The study sample size was based on statistical power (1-β err prob.) of 0.92 and was determined using G∗Power 3.1 software.[26,27]Figure 1 shows the results of the sample size determination. A total of 85 participants were men, whereas 39 participants were women. The mean age for the group was 33.76 years (sd = 2.16), ranging from 27 to 56 years. Furthermore, 79.9% of participants were single; 75.8% were not in paid employment; 65% were not involved in religious activities; and 58% were active members of social clubs in their communities. Participants were recruited by posting fliers in infectious disease clinics and hospitals at 10 community-affiliated medical/health centers and hospitals and through community agencies specializing in providing services to HIV-infected persons. Fifty-five percent of participants met the Centers for Disease Control and Prevention diagnostic criteria for AIDS.[15]
Figure 1.
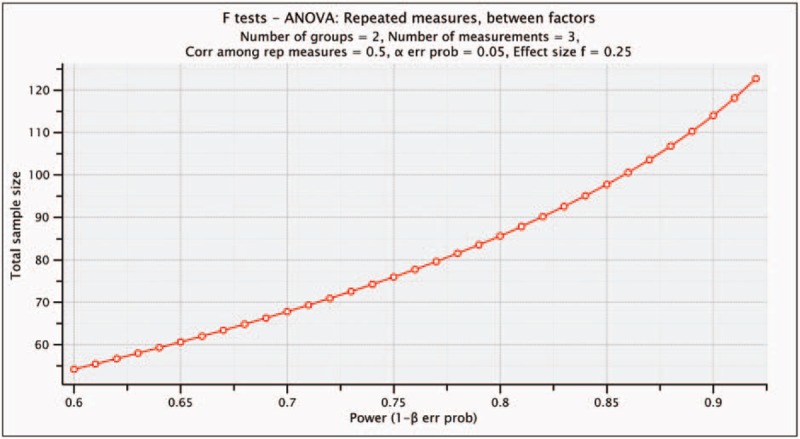
Sample size determination using G∗power software. The results of the sample size determination based on statistical power (1-β err prob.) of 0.92.
2.5. Measures
2.5.1. Alcohol use disorder scale
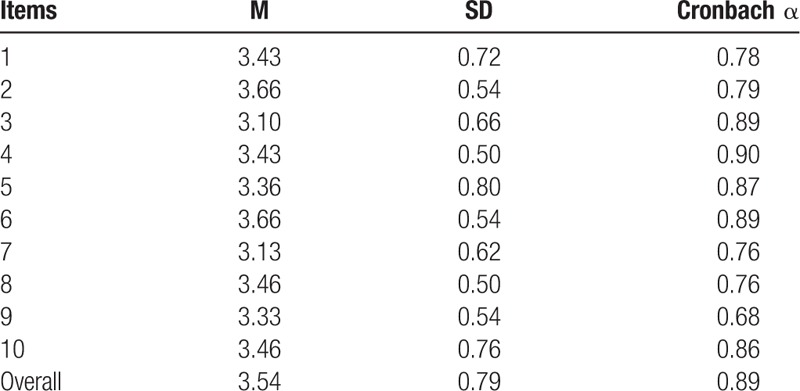
This scale is a 12-item instrument developed by the researchers to determine the extent to which individuals use alcohol and as well experience AUD symptoms (see Appendix A). The overall reliability of the Alcohol Use Disorder Scale (AUDS) was 0.89 (Table 1). The AUDS was validated by 4 experts in the fields of Measurement and Evaluation and Behavioral Health Counseling. High scores reflect a high level of AUD symptoms.
Table 1.
Reliability results of Alcohol Use Disorder Scale.
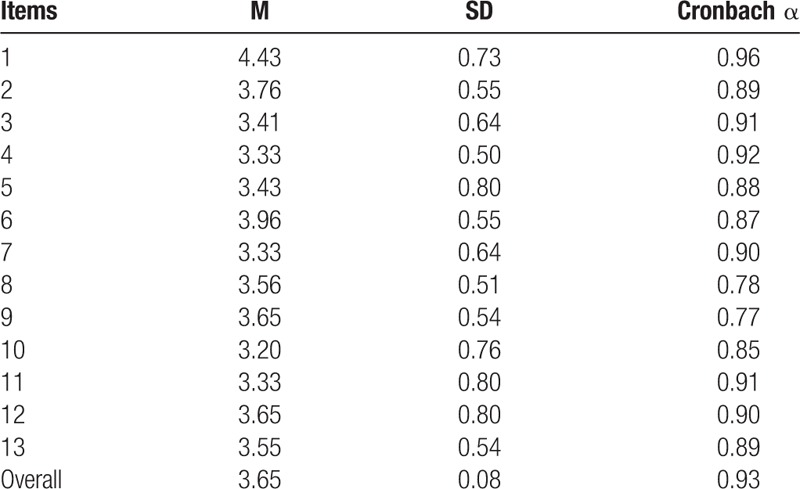
2.5.2. Alcohol irrational beliefs scale
Alcohol-related Irrational Beliefs Scale (AIBS) employs 13 items to measure the irrational beliefs regarding alcohol, which may cause people to experience AUD symptomatology. Each item was formulated based on irrational beliefs about alcohol as expressed by DiGiuseppe and Mclnerney[16] (see Appendix B). The overall reliability of the AIBS was 0.93 (Table 2). The AIBS was validated by 4 experts in the use of REBT and cognitive behavior therapy. High scores reflect a high level of alcohol-related irrational beliefs.
Table 2.
Reliability results of Alcohol Irrational Beliefs Scale.
2.6. Procedure
The researchers advertised the study within the study area between December 2015 and May 2016. Interested participants obtained enrollment and informed consent forms from designated centers, which they filled out and submitted to the researchers. The participants were given instructions for how to complete the forms and what to do with them after they had filled them out. The venues for the study were 2 community secondary schools. The researchers conducted screening for eligibility; HIV-positive patients who met the inclusion criteria were selected as participants after completing the informed consent form. The participants took a pretest before the intervention (Time 1). The first 124 persons presenting with a severe level of AUD and alcohol-related irrational beliefs were selected and randomly assigned to the treatment and control groups using randomization software.
The treatment process for managing AUD was based on the REHT Treatment Manual for Alcohol Use Disorder (RTMAUD) adapted from an REBT Treatment Manual for Addiction (RTMA).[28] Participants (n = 61) in the treatment group took part in REHT. Twenty sessions, lasting 50 minutes each, were held twice per week for 10 consecutive weeks. At the end of the intervention, a post-test was administered to both groups (time 2). Two weeks follow-up, which focused on terminating the therapy after a 6-month period, were conducted by the researchers a week after the intervention and a third assessment (time 3) was conducted at the end of the second follow-up meeting. Thus, the whole study comprised 12 weeks of controlled investigation. Participants (n = 63) in the waitlist control group received 20 twice-weekly 50-minute sessions of REHT immediately after the intervention in the treatment group to help them reduce alcohol use. To avoid selection and expectation bias, research assistants and data analysts were not exposed to group assignment sequences. The authors of the study who delivered the REHT have formal training as counselors and psychologists and also possess expertise in the principles and practice of REBT theory. Therefore, they were qualified to lead the treatment intervention. They were assigned by convenience sampling. The participants in both groups returned the AUDS and AIBS questionnaires directly to the researchers at end of each assessment.
2.7. Control of extraneous and confounding variables
The following steps were adopted by the researchers to prevent the interaction of extraneous variables with the intervention program in line with recent studies.[18,29] They include the following:
2.7.1. Nondifferential selection of participants
To avoid the effect of the treatment being confounded by differential selection, the researchers chose treatment and control group participants who were similar except for exposure to the treatment program.
2.7.2. Elimination of selection bias
All participants were asked to pick an envelope from a container to eliminate selection bias. Each of the envelopes contained 1 card labeled either “T” (for allocation to the treatment group) or “C” (for allocation to the control group). The labels were based on a computer-generated random list (Random Allocation Software version 1.0).[30] (see Fig. 2).
Figure 2.
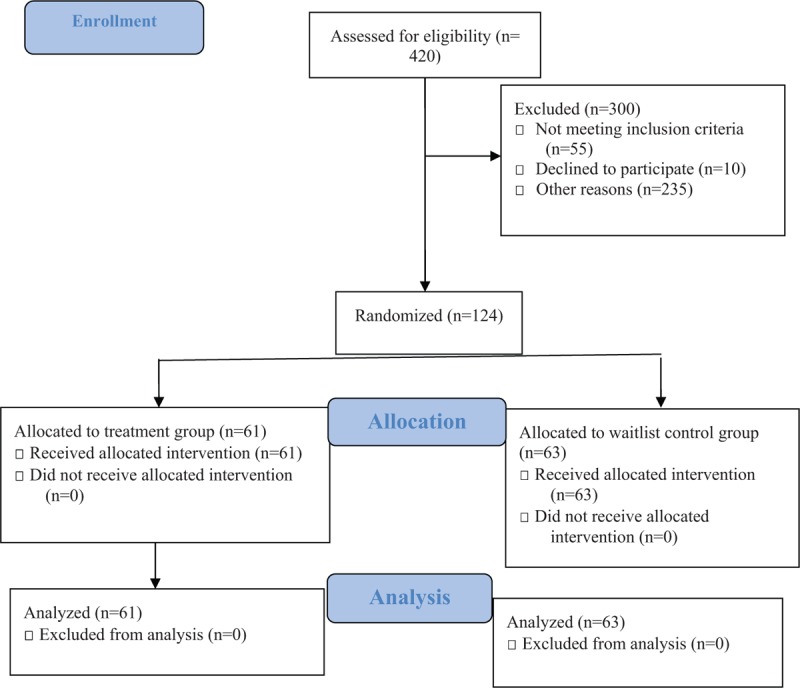
Flow diagram of study participants. The distribution of participants into the treatment and control groups.
2.7.3. Avoidance of interaction and contamination
In order to avoid any form of interaction between the groups and thus prevent contamination, participants from the 2 groups attended their program on different days and at different locations.
2.7.4. Consistency in assessment measures
The same instruments were used throughout all stages of the study to avoid observation of behavioral improvement between pretest and post-test assessments.
2.7.5. Ensuring full participation and elimination of experimental mortality
Only participants who signed the informed consent forms to indicate their readiness and willingness to participate in the study were selected and they were motivated to ensure full and committed participation and to avoid experimental mortality.
2.8. Intervention
2.8.1. Rational emotive health therapy treatment manual for alcohol use disorder symptoms
The intervention plan in this study was based on REHT Treatment Manual for AUD adapted from Hammels and Yalom's RTMA.[29] The RTMAUDS is used for the treatment of AUD among individuals with AUD. The RTMAUDS is based on the framework of rational emotive and cognitive behavior therapy. In using this manual, the authors ensured that they created rapport with the participants. They explained the rules of the therapy, the rationale of REHT for AUD symptoms reduction, and also discussed the goals for the study. RTMAUDS centers on problematic beliefs to mediate symptoms of AUD. Problematic beliefs include demandingness, self-downing, catastrophizing, and low frustration tolerance. Therefore, cognitive, behavioral, and emotive techniques were used to change the target problematic beliefs of the participants related to alcohol consumption. Behavioral techniques involved teaching the participants practical techniques to help them to cope with AUD symptoms, such as drinking more than you intended and having a strong urge to drink. Techniques included methods for planning and managing their daily schedule and for distracting themselves from unhealthy thoughts about drinking. Emotive techniques were used to help the study participants to change their negative thoughts on an emotional level; humorous methods, alcohol-related poems, and native satiric songs related to alcohol were used to generate feelings, which could help to challenge and change negative thoughts toward alcohol.
Following the principles of rational emotive behavioral therapy, the researchers disputed the alcohol-related irrational thoughts of the participants, such as “I cannot stand avoiding a drink”; “I cannot function without a drink”; “I am not strong enough to resist alcohol”; “I cannot stand the deprivation of my desire for a drink”; “I am a horribly deprived person if I cannot have a drink”; “drinking is a short-term solution to my problem”; and others. Participants were taught to overcome the discomfort and anxiety caused by irrational beliefs in several ways: they were taught to wait for the urges for the desired alcohol to pass by distracting themselves; they were taught to dispute the irrational beliefs that elicited the discomfort and anxiety and to tell themselves rational beliefs, such as “I can live with the discomfort of not giving in to the urge”; and “I can do without alcohol”). They were taught to quickly and immediately prevent the discomfort and anxiety by eliminating the activating event. Thus, the RTMAUDS served as an invaluable guide for the REHT intervention in the treatment group.
2.9. Data analysis
The researchers used SPSS 22 (IBM Corp, Armonk, NY) to carry out statistical analysis, including screening for missing values and violation of assumptions. A repeated measures analysis of variance—with time as the within-subjects factor and group as the between-subjects factor—was conducted at time 1 (before intervention); at time 2 (end of the intervention); and at time 3 (follow-up meetings) to measure the participants’ level of AUD and alcohol-related irrational beliefs, which may make them depend on alcohol, as well as improvements over time across the treatment and control group participants. Partial eta squared was reported for this design to reveal the effect size of the intervention.
3. Results
Table 3 presents the results of assessments among the participants. It was observed that there was no baseline difference in level of alcohol use measured by AUDS between participants in the treatment and control conditions: F (1,123) = 0.162; P = .689,  = 0.003. The assessment after the intervention program showed a significant difference in level of alcohol use measured by AUDS between participants in the treatment and control groups: F (1,123) = 267.60; P = .000,
= 0.003. The assessment after the intervention program showed a significant difference in level of alcohol use measured by AUDS between participants in the treatment and control groups: F (1,123) = 267.60; P = .000,  = 0.904. Also, the follow-up assessment (time 3) indicated that there was a further significant difference in level of alcohol use measured by AUDS between participants in the treatment and control conditions: F (1,123) = 271, P = .000;
= 0.904. Also, the follow-up assessment (time 3) indicated that there was a further significant difference in level of alcohol use measured by AUDS between participants in the treatment and control conditions: F (1,123) = 271, P = .000;  = 0.905. This meant that rational emotive health therapy was efficacious in reducing the level of alcohol use among community-dwelling, HIV-positive patients.
= 0.905. This meant that rational emotive health therapy was efficacious in reducing the level of alcohol use among community-dwelling, HIV-positive patients.
Table 3.
Mean, standard deviation, analysis of variance, and effect size of Alcohol Use Disorder Scale and Alcohol Irrational Beliefs Scale among the participants in both treatment and control group.
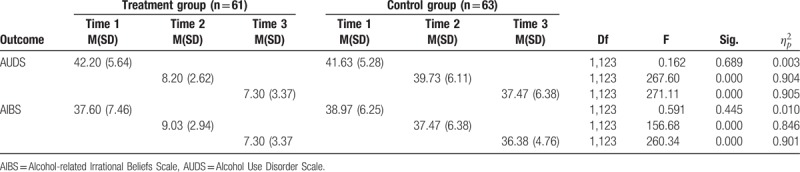
Similarly, Table 3 also reveals that there was no baseline difference in level of alcohol-related irrational beliefs measured by AIBS between participants in the treatment and control conditions: F (1, 123) = 0.591; P = .445,  = 0.010. The assessment after the intervention program showed a significant difference in the level of alcohol-related irrational beliefs measured by AIBS between participants in the treatment and control conditions: F (1, 123) = 156.68; P = .000,
= 0.010. The assessment after the intervention program showed a significant difference in the level of alcohol-related irrational beliefs measured by AIBS between participants in the treatment and control conditions: F (1, 123) = 156.68; P = .000,  = 0.846. Also, the follow-up assessment (time 3) indicated that there was a further significant difference in alcohol-related irrational beliefs measured by AIBS between participants in the treatment and control conditions: F (1, 123) = 260.34; P = .000,
= 0.846. Also, the follow-up assessment (time 3) indicated that there was a further significant difference in alcohol-related irrational beliefs measured by AIBS between participants in the treatment and control conditions: F (1, 123) = 260.34; P = .000,  = 0.901. This meant that rational emotive health therapy was efficacious in reducing the level of alcohol-related irrational beliefs among community-dwelling, HIV-positive patients.
= 0.901. This meant that rational emotive health therapy was efficacious in reducing the level of alcohol-related irrational beliefs among community-dwelling, HIV-positive patients.
4. Discussion
The objective of the present study was to determine the effect of REHT on alcohol use among community-dwelling, HIV-positive patients. The result obtained at the initial assessment indicated that alcohol use was severe, which supported Altice et al,[3] who observed that alcoholic HIV-positive patients have increased prevalence and frequency of substance-use disorder symptoms. Bryant et al[4] noted that exposure to alcohol use was widespread in societies in Africa, and this has resulted in high susceptibility to addiction. Furthermore, REHT significantly decreased alcohol use, which was shown by a reduction in AUDS and AIBS scores with time in the treatment group and lower scores in the treatment group than in the waitlist control group after the intervention. In addition, the effect of REHT was maintained in the participants at 2 follow-up assessments conducted after the end of the intervention. These results were consistent with previous studies, which found significant reductions in the frequency and amount of psychological or behavioral issues in clients exposed to an REBT intervention program.[17,18] The findings lend further credence to Hutchinson et al,[23] who maintained that alcohol dependence can be treated using REBT.
The present study shows that REHT can be an effective treatment for AUD symptoms among community-dwelling, HIV-positive persons in Nigeria. Further studies around the world are essential to appraise the efficacy of REHT-based interventions in the treatment of AUD symptoms among HIV-positive patients. According to Kalichman et al,[1] alcohol is the most commonly used psychoactive substance, which is associated with HIV/AIDS. Weinhardt and Carey[2] observed that AUD symptoms are related to sexual risks in several populations, especially among those with the highest rates of HIV infections. Cook and Clark[5] noted that alcohol elevates sexual risks, which may result in HIV/AIDS infections. It is therefore imperative for cognitive behavioral therapists to assist HIV-positive patients to overcome alcohol use problems.
The background of the authors of the present study in the practice of REBT, coupled with the present findings provoked the argument that the presence of HIV symptoms alone does not cause HIV-positive patients to use alcohol. Rather, their irrational beliefs about the infection contribute to unhealthy feelings and self-defeating cognition that result in AUD symptomatology. Therefore, REBT is an effective approach for therapist and health counselors to teach HIV-positive patients to identify, evaluate, dispute, and act against their self-defeating beliefs, and help them to get better, despite their situation. This fact is in support of Lucas et al's [10] opinion that in treating HIV-positive patients, treatment for AUD symptoms should precede initiation of ART. The application of REBT will enable the patients to think rationally about themselves and thus be able to respond to ART process.
5. Limitations and suggestions for further studies
The first limitation observed in the study was that participants were all outpatients. The authors acknowledge that implementing the REHT intervention as a treatment for HIV-positive inpatients might give rise to considerable differences in effect. The reason is that HIV-positive inpatients may not have consistent access to alcoholic beverages. Thus, further studies should compare inpatient and outpatient treatment by implementing at least 25 weeks of REHT in inpatients and outpatients programs.
Another limitation of the study is the lack of data analysis for the demographic variables of the participants, such as location, educational status, and financial status. Future studies should include the demographic variables in the analysis to find out if there will be an interaction effect between demographic variables and REHT intervention for HIV-positive patients who indulge in alcohol drinking. Previous studies[18,31–33] have indicated that REBT programs are not usually disrupted by small sample sizes. This information notwithstanding, upcoming researchers should endeavor to use larger sample sizes to study the effectiveness of REHT on HIV-positive persons in the Nigerian communities.
Also, the delivery of the treatment modality does have variability between behavioral health providers. All experts are not the same. For instance, studies indicate that therapists’ sex could account for variability in treatment outcome.[31–33] There also are other variables between patients and therapists that could affect therapeutic alliance, outcomes, and engagement. For instance, active, engaging, and extraverted therapists may generate faster symptom reduction in short-term therapy, whereas nonintrusive therapists may produce better outcome in long-term therapy.[34] Another main factor for variability in treatment outcome could be due to the lack of therapeutic attunement and inflexibility on part of the therapist.[34] Also, technical adherence and directivity of the therapist could account for variability in treatment outcome.[35] To ameliorate these issues, therapists should improve their facilitative interpersonal skills, possess the ability for strong therapeutic alliance, effectively handle patient avoidance, possess a flexible interpersonal style,[34–36] and develop better rational emotive health therapy skills. One consideration for further research is to consider polysubstance abuse as a factor. Such research may have to indicate the drug test results in this regard and whether the study affects other substance abuse use. It is possible that other psychological interventions could be used to reduce AUD symptoms as well as other SUD symptoms.[35–40]
6. Conclusion
Alcohol use deters the ability of community-dwelling, HIV-positive patients to cope with the challenges of their situation and to manage the disease reasonably. REHT can, however, help these patients overcome their alcohol-related thoughts and feelings. On this note, Nigerian community health therapists and counselors are urged to deepen their efforts toward conducting REHT interventions that would significantly improve the psychosocial health of patients living with HIV/AIDS illnesses. In addition, REBT counselors, social workers, and other mental health professionals in Nigeria and other countries in the world should be assisting HIV-positive patients with various psychological health needs. Also, REBT practitioners are urged to conduct follow-up studies to examine the effectiveness of REHT for different HIV-positive patient populations who are depending on alcohol substances.
Acknowledgments
The authors acknowledge all the participants, research assistants, technical advisers, and consultants who, in one way or another, contributed to the success of the study. Special thanks go to Otusum Consult, Nigeria, for providing financial aid and expert advice to the researchers.
Author contributions
Conceptualization: Mkpoikanke Sunday Otu, Anthonia Olunwa Aneke, Victoria Ogwa Adikwu, Eberechukwu Francisca Chigbu, Liziana N. Onuigbo, Inwang Etim Udom, Nchedo Aye, Immaculata Nwakaego Akaneme, Doris Chika Egeonu, Ngozi Mary Eze.
Data curation: Inwang Etim Udom, Mkpoikanke Sunday Otu, Immaculata Nwakaego Akaneme
Formal analysis: Mkpoikanke Sunday Otu, Chiedu Eseadi.
Funding acquisition: Joachim Chinweike Omeje, Gabriel Ochaka Okpanachi
Investigation: Mkpoikanke Sunday Otu, Immaculata Nwakaego Akaneme.
Methodology: Mkpoikanke Sunday Otu, Victoria Ogwa Adikwu, Okechukwu O. Nwauabani, Liziana N. Onuigbo, Gabriel Ochaka Okpanachi.
Resources: Mkpoikanke Sunday Otu, Okechukwu O. Nwauabani, Doris Chika Egeonu.
Supervision: Mkpoikanke Sunday Otu, Victor Sunday Ezema.
Validation: Eberechukwu Francisca Chigbu, Liziana N. Onuigbo, Abah George Ohabuenyi, Chiedu Eseadi.
Writing – original draft: Joachim Chinweike Omeje, Mkpoikanke Sunday Otu, Victoria Og
Writing – review and editing: Joachim Chinweike Omeje, Mkpoikanke Sunday Otu, Eberechukwu Francisca Chigbu, Nchedo Aye, Victor Sunday Ezema, Abah George Ohabuenyi, Chiedu Eseadi.
Supplementary Material
Footnotes
Abbreviations: AIBS = Alcohol Irrational Beliefs Scale, AUDS = Alcohol Use Disorder Scale, HIV = human immunodeficiency virus, AIDS = acquired immunodeficiency syndrome, REHT = rational emotive health therapy, RTMA = REBT Treatment Manual for Addiction.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Kalichman SC, Simbayi LC, Kaufman M, et al. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci 2007;8:141–51. [DOI] [PubMed] [Google Scholar]
- [2].Weinhardt L, Carey MP. Does alcohol lead to sexual risk behavior? Annu Rev Sex Res 2001;12:125–57. [PMC free article] [PubMed] [Google Scholar]
- [3].Altice FL, Kamarulzaman A, Soriano VV, et al. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet 2010;376:367–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bryant KJ, Nelson S, Braithwaite RS, et al. Integrating HIV/AIDS and alcohol research. Alcohol Health Res World 2010;33:167–78. [PMC free article] [PubMed] [Google Scholar]
- [5].Cook RL, Clark D. Is there an association between alcohol consumption and sexually transmitted diseases? A systematic review. Sex Transm Dis 2005;32:156–64. [DOI] [PubMed] [Google Scholar]
- [6].Palepu A, Raj A, Horton N, et al. Substance abuse treatment and risk behaviors among HIV infected persons with alcohol problems. J Subst Abuse Treat 2005;28:3–9. [DOI] [PubMed] [Google Scholar]
- [7].White K. An Introduction to the Sociology of Health and Illness. 2nd rev edThousand Oaks, CA: Sage; 2009. [Google Scholar]
- [8].World Health Organization. Department of Mental Health and Substance Dependence. Noncommunicable Diseases and Mental Health: Investing in Mental Health. Geneva: World Health Organization; 2003. [Google Scholar]
- [9].Ayisi JG, Eijk AM, Kuile FO, et al. Risk factors for HIV infection among asymptomatic pregnant women attending an antenatal clinic in western Kenya. Int J STD AIDS 2000;11:393–401. [DOI] [PubMed] [Google Scholar]
- [10].Lucas GM, Gebo KA, Chaisson RE, et al. Longitudinal assessment of the effects of drug and alcohol abuse on HIV-1 treatment outcomes in an urban clinic. AIDS 2002;16:767–74. [DOI] [PubMed] [Google Scholar]
- [11].Hinkin CH, Hardy DJ, Mason KI, et al. Medication adherence in HIV-infected adults: effect of patient age, cognitive status, and substance abuse. AIDS 2004;18:S19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Morojele NK, Kachieng MA, Nkoko MA, et al. Perceived effects of alcohol use on sexual encounters among adults in South Africa. Afr J Drug Alcohol Stud 2004;3:1–20. [Google Scholar]
- [13].Dunkle KL, Jewkes RK, Brown HC, et al. Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Soc Sci Med 2004;59:1581–92. [DOI] [PubMed] [Google Scholar]
- [14].Zachariah R, Spielmann MP, Harries AD, et al. Sexually transmitted infections and sexual behaviour among commercial sex workers in a rural district in Malawi. Int J STD AIDS 2003;14:185–8. [DOI] [PubMed] [Google Scholar]
- [15].Centers for Disease Control, Prevention. Revised Guidelines for, HIV, Counseling, Testing, Referral Technical Expert Panel Review of CDC HIV Counseling, Testing, and Referral Guidelines. Atlanta, GA: CDC; 1999. [Google Scholar]
- [16].DiGiuseppe R, Mclnerney J. Patterns of addiction: a rational-emotive perspective. J Cogn Psychother 1990;4:121–34. [Google Scholar]
- [17].Terjesen MD, DiGiuseppe R, Gruner P. A review of REBT research in alcohol abuse treatment. J Ration Emot Cogn Behav Ther 2000;18:165–79. [Google Scholar]
- [18].Eseadi C, Onwuka GT, Otu MS, et al. Effects of rational emotive cognitive behavioral coaching on depression among type 2 diabetic inpatients. J Ration Emot Cogn Behav Ther 2017;35:363–82. [Google Scholar]
- [19].Onyechi KC, Eseadi C, Umoke PC, et al. Effects of a group-focused cognitive behavioral health education program on cigarette smoking in a sample of Nigerian prisoners. Medicine (Baltimore) 2017;96:e5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Walen SR, DiGiuseppe R, Dryden W. A Practitioner's Guide to Rational Emotive Therapy. 2nd edNew York: Oxford University Press; 1992. [Google Scholar]
- [21].Ellis A, Griege R. Handbook of Rational-Emotive Therapy. New York: Springer; 1977. [Google Scholar]
- [22].Eseadi C, Anyanwu JI, Ogbuabor SE, et al. Effects of cognitive restructuring intervention program of rational-emotive behavior therapy on adverse childhood stress in Nigeria. J Ration Emot Cogn Behav Ther 2005;34:51–72. [Google Scholar]
- [23].Hutchinson GT, Patock-Peckham JA, Cheong J, et al. Irrational beliefs and behavioral misregulation in the role of alcohol abuse among college students. J Ration Emot Cogn Behav Ther 1998;16:61–74. [Google Scholar]
- [24].World Medical Association. WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. 1964. Available at: http://www.wma.net/en/30publications/10policies/b3/. Accessed March 20, 2015. [Google Scholar]
- [25].American Psychological Association. Ethical Principles of Psychologists and Code of Conduct. Washington, DC: American Psychological Association; 2010. [Google Scholar]
- [26].Faul F, Erdfelder E, Lang AG, et al. G∗Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175–91. [DOI] [PubMed] [Google Scholar]
- [27].Faul F, Erdfelder E, Buchner A, et al. Statistical power analyses using G∗Power 3.1: tests for correlation and regression analyses. Behav Res Methods 2009;41:1149–60. [DOI] [PubMed] [Google Scholar]
- [28].Hammels D, Yalom V. Instructor's Manual for Rational Emotive Behavior Therapy for Addictions With Albert Ellis. Mill Valley, CA: Psychotherapy.net, 2009. [Google Scholar]
- [29].Esere MO. Effect of sex education programme on at-risk sexual behaviour of school-going adolescents in Ilorin, Nigeria. Afri Health Sci 2008;8:120–5. [PMC free article] [PubMed] [Google Scholar]
- [30].Saghaei M. Random location software, 2004. Available at: http://mahmoodsaghaei.tripod.com/Softwares/randalloc.html. Accessed March 15, 2015. [Google Scholar]
- [31].Owuamanam TO, Ajidahun BO, Owuamanam DO. The influence of gender and family background on the effectiveness of client centered and rational emotive behaviour counselling therapies in enhancing the self-concept of adolescents. LICEJ 2012;3:584–90. [Google Scholar]
- [32].Onyechi KCN, Eseadi C, Okere AU, et al. Effects of rational-emotive health education program on HIV risk perceptions among in-school adolescents in Nigeria. Medicine 2016;95:e3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Ogbuanya TC, Eseadi C, Orji CT, et al. Effects of rational emotive behavior coaching on occupational stress and work ability among electronics workshop instructors in Nigeria. Medicine 2017;96:e6891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Tobias S. Characteristics of highly effective therapists. Master's Thesis, Faculty of Psychology and Educational Sciences, Universiteit Gent. [Google Scholar]
- [35].Greeson JKP, Guo S, Barth RP, et al. Contributions of therapist characteristics and stability to intensive in-home therapy youth outcomes. Res Soc Work Pract 2009;19:239–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Heinonen E, Lindfors O, Laaksonen MA, et al. Therapists’ professional and personal characteristics as predictors of outcome in short- and long-term psychotherapy. J Affect Disord 2012;138:301–12. [DOI] [PubMed] [Google Scholar]
- [37].Watson JC. Treatment failure in humanistic and experiential psychotherapy. J Clin Psychol 2011;67:1117–28. [DOI] [PubMed] [Google Scholar]
- [38].Henry WP, Schacht TE, Strupp HH, et al. Effects of training in time-limited dynamic psychotherapy: mediators of therapists’ responses to training. J Consult Clin Psychol 1993;61:441–7. [DOI] [PubMed] [Google Scholar]
- [39].Bein TH, Miller WR, Boroughs JM. Motivational interviewing with alcohol outpatients. Behav Cogn Psychother 1993;21:347–56. [Google Scholar]
- [40].Stade BC, Bailey C, Dzendoletas D, et al. Psychological and/or educational interventions for reducing alcohol consumption in pregnant women and women planning pregnancy. Cochrane Database Syst Rev 2009. CD004228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


