Abstract
We investigated the effects of tonsillectomy by low-temperature plasma on the growth development and psychological behavior in children with obstructive sleep apnea hypopnea syndrome (OSAHS).
This study included 72 moderate and severe OSAHS children with tonsils or adenoids hypertrophy, which were randomly assigned into either the study group (n = 36) or the control group (n = 36). Patients in study group underwent tonsillectomy by low-temperature plasma, while in the control group underwent tonsil-pecking, then the efficacy were compared.
The time of surgery, VAS scores on postoperative day 1, 3, and 7 were significantly lower in the study group than in the control group, and the efficiency was significantly higher in the study group than the control group (P = .018). In the study group, the BMI was lower, the score of C-WISC (VIQ, PIQ, and FIQ) was higher, the score of CBCL social competence was higher and the score of behavioral questions was lower than that in the control group; differences were statistically significant (P = .022). The serum levels of IgA, IgG, and IgM, as well as the percentage of T lymphocytes, between the study group and the control group were not significantly different (P = .132).
Tonsillectomy by low-temperature plasma was effective on the treatment of children with severe OSAHS, and could improve growth development and psychological behavior.
Keywords: child behavior checklist (CBCL), low-temperature plasma, obstructive sleep apnea hypopnea syndrome, tonsillectomy, Wechsler intelligence scale for children (C-WISC)
1. Introduction
The morbidity of obstructive sleep apnea hypopnea syndrome (OSAHS) in children is about 2% to 5%, and achieves a peak at 2 to 5 years old.[1] OSAHS is closely associated with obesity, which can worsen the symptoms of OSAHS.[2] Clinical manifestations of OSAHS include sleep disorder, inattention, memory decline, and subsequent impact on normal development and psychological behavior.[3] Surgery is recommended for moderate and severe OSAHS children with tonsils or adenoids hypertrophy. Surgical procedures include conventional tonsil removal and resection by either ultrasound knife, laser, microwave, and plasma.[4,5] Low-temperature plasma knife is based on the plasma triggered by an electromagnetic wave with a certain frequency; the plasma can perform cutting, ablation, and hemostasis in tissues. Low-temperature plasma knife is reported to cause less trauma and bleeding, rapid recovery, and mild postoperative pain, and thus has been increasingly applied.[6] This study is aimed at analyzing the effects of tonsillectomy by low-temperature plasma on the grow development and psychological behavior of OSAHS children.
2. Material and methods
2.1. General information
This study included 72 consecutive moderate and severe OSAHS children with tonsils or adenoids hypertrophy, that were diagnosed and treated in this hospital from January 2014 to June 2015. PSG (US) was used to monitor and record the nose and mouth breathing airflow, loudness of snoring, oxygen saturation (SO2), electrocardiogram (ECG), electroencephalogram (EEG), and electro-oculogram (EOG) for at least 7 hours. The number of sleep apnea and the number and duration of hypopnea episodes were calculated. These data were collected and analyzed by sleep software with artificial adjustment. The criteria of moderate and severe OSAHS were as follows: the time for Apnea Hypopnea Index (AHI) ≥5 times/h, SpO2≤85%, peak End Tidal CO2 (PET CO2 peak) > 60 mm Hg and End Tidal CO2 (PET CO2) > 50 mm Hg accounted for > 25% of total sleep time, and awakening events > 11 times/h.[7,8] Patients with acute infection, immune dysfunction, and nasal developmental abnormalities were excluded from this study. This study obtained the approval from the Ethics Committee and the informed consent was obtained from both the patients (children and their family). The children were randomly assigned into either the study group (n = 36) or the control group (n = 36). In the control group, there were 21 males and 15 females, with a mean age of 5.2 ± 1.3 years; there were 12 children with moderate OSAHS and 24 children with severe OSAHS. In the study group, there were 20 males and 16 females, with a mean age 5.3 ± 1.4 years. There were 13 children with moderate OSAHS and 23 children with severe OSAHS. The baseline data between the study group and the control group were comparable.
3. Methods
These surgeries were performed by the same surgical and nursing team. The control group used tonsil pecking method: the patient was supine under general anesthesia. The tonsil was exposed by a Davis Boyle Mouth Gag, the palatoglossal arch was dissected, the upper pole and lower pole of the tonsillar capsule was separated, and then the tonsil was removed by ecrasement and pecking. The tonsillar fossa was pressed by a gauze for 2 to 3 minutes for hemostasis, and a suture was performed if necessary. A tonsillectomy by low-temperature plasma was applied in the study group and a plasma surgery system (US) was used. The mucous membrane at the palatine arch was dissected with a Evac70 blade, and the upper pole of the tonsil was exposed. The tonsil was resected to the lower pole completely within the capsule and the surrounding gap. The tonsillar fossa was checked and electrocoagulation was performed.
3.1. Observational measurements
The time of surgery and the pain degree on postoperative day 1, 3, and 7 were compared. A visual analog scale (VAS) on pain severity of operative site after surgery was used with a grade range of 0 to 10 points; a higher grade indicated more severe pain. The efficacy was compared to a standard of efficacy measurement.
The number of low ventilation or pause by PSG monitoring ≥40%, the decrease of PetCO2 ≥20% and the reduction in number of awakening events ≥50% were considered to be significant efficacy. The number of low ventilation or pause by PSG monitoring ≥20%, the decrease of PetCO2 ≥10%, and the reduction in number of awakening events ≥30% was considered as efficacious; other results were considered as having no efficacy. The duration of the follow up was 12.0 months, at which height and weight were measured, and the body mass index (BMI) was caculated. The Chinese version of Wechsler Intelligence Scale for Children (C-WISC) and Achenbach Child Behavior Checklist (CBCL) were used to evaluate the intelligence development and psychological behavior. C-WISC included speech-language subscale (Information, Similarities, Arithmetic, Vocabulary and Comprehension) and performance subscale (Symbol Search, Cancellation, Block Design, Matrix Reasoning, Coding). Scores out of a total of 10 items were then transformed into verbal IQ (VIQ), performance IQ (PIQ) and full scale IQ (FSIQ) scores. The higher the score, the better the cognitive development. CBCL consisted of social competence (7 items, a score < 30 was considered abnormal) and behavior problems (113 items, a score > 60 was considered abnormal). The levels of IgA, IgG, and IgM, as well as the percentage of T lymphocytes, were compared. The levels of Ig were measured using immunoturbidimetry, and the reagents were purchased from Jiangsu Biyuntian Technology Co., Ltd. The percentage of CD4 + T cells and CD8 + T cells were measured using flow cytometry. The FACS Caliber flow cytometer was purchased from BD (New Jersey).
3.2. Statistical analysis
The SPSS 20.0 software was used for statistical analysis and the measurement data were represented by mean ± SD. Intergroup comparison was performed by an independent sample t-test, and intragroup comparison was performed by a paired t-test, if groups do not show normal distribution characteristics non parametric test consisting of Mann Whitney U and Wilcoxon Matched Pair tests should be used. Enumeration data were represented by an n or %, and intergroup comparison was performed by a chi-square test. P < .05 was considered to be significantly different.
4. Results
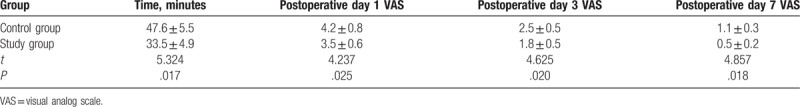
4.1. The time of surgery and pain scores
As shown in Table 1, the time of surgery, VAS scores on postoperative day 1, 3, and 7 were significantly lower in the study group than in the control group (groups have normal distribution, so a paired t-test was applied; P = .018).
Table 1.
The time of surgery and pain scores.
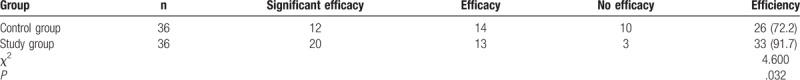
4.2. Clinical efficacy
As shown in Table 2, the efficacy was significantly higher in the study group than in the control group (P = .014).
Table 2.
Clinical efficacy [n (%)].
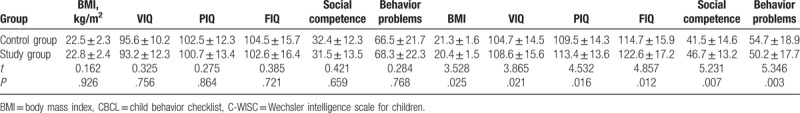
4.3. BMI, C-WISC scores, and CBCL scores
As shown in Table 3, the BMI was significantly lower in the study group than in the control group. The C-WISC score and the score of social competence was significantly higher in the study group than in the control group, while the score of behavioral problems was significantly lower in the study group than in the control group (groups have normal distribution, so a paired t-test was applied; P = .022).
Table 3.
BMI, C-WISC scores, and CBCL scores.
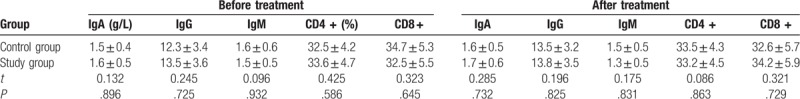
4.4. The serum levels of IgA, IgG, and IgM as well as the percentage of T lymphocytes
As shown in Table 4, the serum levels of IgA, IgG, and IgM, as well as the percentage of T lymphocytes, were not significantly different between the study group and the control group (groups have normal distribution, so a paired t-test was applied; P = .132).
Table 4.
The serum levels of IgA, IgG, and IgM as well as the percentage of T lymphocytes.
5. Discussion
OSAHS causes hypoxemia and sleep hypercapnia, affecting the normal development, intelligence, and psychological behavior of children. Nieminen et al[9] reported that OSAHS-induced growth hormone deficiency was associated with sleep cycles and sleep quality. The rapid eye movement (REM) sleep and slow wave sleep (SWS) of OSAHS children were decreased. Hypoxia could inhibit the regulation of endocrine hormone by the hypothalamic-pituitary axis, which may lead to developmental delay. Bédard et al[10] reported that the results of intelligence tests conducted in children were closely associated with the degree of hypoxia during night sleep. REM is important for the maturation of the neurological system in children. During REM, the synthesis of proteins is accelerated, the development of cerebral cortex contact fibers and myelogenesis constructs synaptic connections and promotes studying and memory activities.[11] Beebe and Gozal[12] reported that OSAHS induced injury in the prefrontal cortex and changed both metabolism and neurotransmitters, leading to decreased abilities of recognition, differentiation and memory.
Gozal and Pope[13] reported that young and preschool children with OSAHS were at an increased risk of poor academic achievement, and only partial cognitive impairment could be reversed even if the symptoms were relieved. Goldstein et al[14] reported that 30% of children may have abnormal behavior with respect to full performance, body disease, social functions and memory difficulties. OSAHS children tended to have introversional depression, extroversional misconduct, aggression and hyperactivity; the severity was increased with the severity of OSAHS.[15] Schechter[16] reported that the abnormal behavior of OSAHS children was related to hypoxia during sleep and sleep disorders. Animal models showed that intermittent hypoxia could impact brain function, cause minimal brain dysfunction, and REM sleep deprivation, which could increase the aggressiveness.[17]
This study found that at the time of surgery, VAS scores on postoperative day 1, 3, and 7 were significantly lower in the study group than in the control group, and the efficiency was significantly higher in the study group than in the control group. In the study group, the BMI was lower, the score of C-WISC (VIQ, PIQ, and FIQ) was higher, the score of CBCL social competence was higher and the score of behavioral questions was lower than the control group; differences were significant. The serum levels of IgA, IgG, and IgM, as well as the percentage of T lymphocytes, between the study group and the control group were not significantly different. Weight loss, pharyngeal and abdominal visceral fat reduction, and pharyngeal airway diameter increases after bariatric surgery were shown to improve OSAHS symptoms.[18] The physical parameter BMI was significantly lower in the study group than in the control group. Thus, the weight-loss surgery could exert therapeutic effects on OSAHS by resulting in decreases in body parameters (BMI), improvements in lipid metabolism indicators, and changing body fat distribution. All in all, the results indicated that tonsillectomy by low-temperature plasma was effective in the treatment of children with severe OSAHS, and could improve the growth development and psychological behavior, while had a lower impact on the immune system.
Since tonsillectomy surgery is feasible and doable and is usually used by otolaryngology surgeons to treat the patients suffering from OSAHS.[19] Further studies that are done by several researchers have shown different results which caused some doubts in the efficacy of this procedure. This difference can largely be due to different criteria for assessing the success rate of surgery, which are used by different researchers. The momentum of plasma was low and the working temperature was low at 40 to 70°C. Low-temperature resection could decrease the strong traction of the surrounding capsule, make the plat wound, reduce postoperative mucosal edema, allow immediate formation of protein pseudomembrane, and occlude the capillaries in the wound to stop bleeding.[20] The coverage of surgical wound by a pseudomembrane could reduce postoperative pain significantly.
The main strength of the trial described here is its 2 center randomized design, which substantially reduces the risk of unwanted influences and selection biases. All polysomnograms were evaluated by hand by investigators blinded to the trial procedures, according to international standards. The main limitation of the trial is its patients’ number follow-up, which is not many enough to evaluate data efficacy. However, for ethical reasons more follow-up for the control group did not seem justifiable. Nevertheless, all patients should be recruited into a follow-up study in order to uncover potential adverse long-term effects.
6. Conclusions
In summary, tonsillectomy by low-temperature plasma has been shown to be safe and effective in patients who have obstructive sleep apnea and oropharyngeal obstruction. It should therefore be more strongly emphasized in future guidelines.
Author contributions
YC, JL, and QY were involved in the conception and design of the study, in the collection, assembly, analysis and interpretation of the data and in drafting of the article; they also provided statistical expertise, YC, XW, and WX contributed to final approval of the article, provision of study materials, technical and logistical support as well as critical revision of the article for important intellectual content.
Conceptualization: Ying-Chun Cao, Xiang-Yun Wang, Wei-Wei Xu.
Data curation: Ying-Chun Cao, Xiang-Yun Wang, Wei-Wei Xu, Qiu-Hong Yu.
Formal analysis: Ying-Chun Cao.
Funding acquisition: Ying-Chun Cao, Xiang-Yun Wang.
Investigation: Ying-Chun Cao, Wei-Wei Xu, Jian-Dong Li, Qiu-Hong Yu.
Methodology: Ying-Chun Cao, Jian-Dong Li.
Project administration: Ying-Chun Cao, Jian-Dong Li, Qiu-Hong Yu.
Resources: Ying-Chun Cao.
Supervision: Xiang-Yun Wang, Qiu-Hong Yu.
Validation: Ying-Chun Cao.
Visualization: Ying-Chun Cao.
Writing – original draft: Ying-Chun Cao.
Writing – review & editing: Ying-Chun Cao.
Footnotes
Abbreviations: BMI = body mass index, CBCL = child behavior Checklist, C-WISC = Wechsler intelligence scale for children, ECG = electrocardiogram, EEG = electroencephalogram, EOG = electro-oculogram, OSAHS = obstructive sleep apnea hypopnea syndrome, REM = rapid eye movement, SO2 = oxygen saturation, SWS = sleep and slow wave sleep, VAS = visual analog scale.
Competing interests: The authors declare there is no conflict of interests.
Funding: This study did not receive any funding from agencies in the public, commercial, or not-for-profit sector.
Ethics approval and consent to participate: This study was approved by The Ethics Committee of The People's Hospital of Dongying, Participants have provided their written informed consent to participate in this study.
Availability of data and materials: The datasets generated and analyzed during the current study are not publicly available due to statutory provisions regarding data- and privacy protection, the dataset supporting the conclusions of this article is available upon reasonable request directed to the corresponding author.
The authors have no conflicts of interest to disclose.
References
- [1].Liu JF, Tsai CM, Su MC, et al. Application of desaturation index in post-surgery follow-up in children with obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 2016;17:156–7. [DOI] [PubMed] [Google Scholar]
- [2].Parola M, Vajro P. Nocturnal hypoxia in obese-related obstructive sleep apnea as a putative trigger of oxidative stress in pediatric NAFLD progression. J Hepatol 2016;65:470–2. [DOI] [PubMed] [Google Scholar]
- [3].Davies CR, Harrington JJ. Impact of obstructive sleep apnea on neurocognitive function and impact of continuous positive air pressure. Sleep Med Clin 2016;11:287–98. [DOI] [PubMed] [Google Scholar]
- [4].Prosser JD, Shott SR, Rodriguez O, et al. Polysomnographic outcomes following lingual tonsillectomy for persistent obstructive sleep apnea in down syndrome. Laryngoscope 2016;12:123–4. [DOI] [PubMed] [Google Scholar]
- [5].Shao J, Yu Q, Zhang S, et al. Effect of plasma radio frequency ablation on obstructive sleep apnea hypopnea syndrome. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2008;22:558–9. [PubMed] [Google Scholar]
- [6].Wei M, Li L, Qin H. The effect of uvulopalatopharyngoplasty by radio frequency plasma. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2010;24:116–8. [PubMed] [Google Scholar]
- [7].Peña-Zarza JA, De la Peña M, Yañez A, et al. Glycated hemoglobin and sleep apnea syndrome in children: beyond the apnea-hypopnea index. Sleep Breath 2018;22:205–10. [DOI] [PubMed] [Google Scholar]
- [8].Kaditis AG, Alonso Alvarez ML, Boudewyns A, et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J 2016;47:69–94. [DOI] [PubMed] [Google Scholar]
- [9].Nieminen P, Löppönen T, Tolonen U, et al. Growth and biochemical markers of growth in children with snoring and obstructive sleep apnea. Pediatrics 2002;109:e55. [DOI] [PubMed] [Google Scholar]
- [10].Bédard MA, Montplaisir J, Richer F, et al. Obstructive sleep apnea syndrome: pathogenesis of neuropsychological deficite. J Clin Exp Neuropsychol 1991;13:950–64. [DOI] [PubMed] [Google Scholar]
- [11].Koo DL, Nam H. Clinical considerations of obstructive sleep apnea with little REM sleep. J Clin Neurol 2016;12:426–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Beebe DW, Gozal D. Obstructive sleep apnea and the prefrontal cortex: towards a comprehensive model linking nocturnal upper airway obstructive to daytime cognitive and behavioral deficits. J Sleep Res 2002;11:1–6. [DOI] [PubMed] [Google Scholar]
- [13].Gozal D, Pope DW., Jr Snoring during early childhood and academic performance at ages thirteen and fourteen years. Pediatrics 2001;107:1394–9. [DOI] [PubMed] [Google Scholar]
- [14].Goldstein NA, Post JC, Rosenfeld RM, et al. Impact of tonsillectomy and a denidectomy on child behavior. Arch Otolaryngol Head Neck Surg 2000;126:494–8. [DOI] [PubMed] [Google Scholar]
- [15].Yosunkaya S, Kutlu R, Cihan FG. Evaluation of depression and quality of life in patients with obstructive sleep apnea syndrome. Niger J Clin Pract 2016;19:573–9. [DOI] [PubMed] [Google Scholar]
- [16].Schechter MS. Section on pediatric pulmonology, subcommittee on obstructive sleep apnea syndrome. Technical report: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2002;109:e691. [DOI] [PubMed] [Google Scholar]
- [17].Miano S, Esposito M, Foderaro G, et al. Sleep-related disorders in children with attention-deficit hyperactivity disorder: preliminary results of a full sleep assessment study. CNS Neurosci Ther 2016;3:556–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Sutherland K, Lee RW, Phillips CL, et al. Effect of weight loss on upper airway size and facial fat in men with obstructive sleep apnoea. Thorax 2011;66:797–803. [DOI] [PubMed] [Google Scholar]
- [19].Holty J-EC, Guilleminault C Maxillomandibular advancement for the treatment of obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev 2010;14:287–97. [DOI] [PubMed] [Google Scholar]
- [20].Tvinnereim M, Mitic S, Hansen RK. Plasma radio frequency preceded by pressure recording enhances success for treating sleep-related breathing disorders. Laryngoscope 2007;117:731–6. [DOI] [PubMed] [Google Scholar]


