Abstract
Most publications about breast cancer do not provide accurate and comprehensive information, giving few or no data about risk/benefit ratios. We conducted a comparative study among 10 European countries about health information on breast cancer screening, assessing the first 10 Web sites addressing the general public that appeared following an Internet search.
With the help of medical residents involved in the EuroNet MRPH Association, we analyzed the first 30 results of an Internet search in 10 European countries to determine the first 10 sites that offered screening mammography. We searched for the following information: source of information, general information on mammography and breast cancer screening, potential harms and risks (false positives, false positives after biopsy, false negatives, interval cancer, overdiagnosis, lead-time bias, and radiation exposure), and potential benefits (reduced mortality and increased survival).
The United Kingdom provided the most information: 39 of all 70 possible identified risks (56%) were reported on its sites. Five nations presented over 35% of the possible information (United Kingdom, Spain, France, Ireland, and Italy); the others were under 30% (Portugal, Poland, Slovenia, Netherlands, and Croatia). Regarding the benefits, sites offering the most complete information were those in France (95%) and Poland (90%).
Our results suggest that, despite consensus in the scientific community about providing better information to citizens, further efforts are needed to improve information about breast cancer screening. That conclusion also applies to countries showing better results. We believe that there should be greater coordination in this regard throughout Europe.
Keywords: breast cancer screening, informed choice, mammography, preventive medicine
1. Introduction
The debate over breast cancer screening is one of the most controversial and emotional within the scientific community.[1–6] Over the past 15 years, there has been a huge development in the discourse and recognition of the harms and benefits of breast cancer screening. Beyond the scientific issues, several factors have made this a complex matter: self-referral; slow recognition of the possible harms; diverging views about the preference between autonomy and paternalism; and the strong influence of public opinion in this area.[7–9]
The scientific and ethical debate concerns 2 core questions. It is questioned the precise contribute of screening in reducing the mortality rate for breast cancer.[10,11] Second, it is uncertain whether the trade-off between benefits and harms favors screening.[12–16] Regarding the second issue, according to current prevailing opinion, women should be informed about both the risks and benefits of screening to make decisions based on informed choices.[17–19]
Information about screening mammography can come from various sources (Web sites, journals, television, oncological centers, or other health organizations), be in varying formats (leaflets, booklets, brochures, pamphlets, technical reports), and be directed at different audiences (general public, administrators, health-care providers).
Previous studies have found that information on Web sites and in invitations were lacking and were more intended at making people get screened than ensuring informed choice; thus, a number of European investigations have shown that most documents about breast cancer published for the public did not provide accurate, comprehensive information: such documents were found to contain few or no data about the risk/benefit ratio, and they were biased in favor of benefits.[7,20–24]
Therefore, since this represents an important topic in public health context, we conducted the presented comparative study with the aim of pointing out deficiencies in informed decision-making policies of many European countries. We examined health information about breast cancer screening by exploring online Web sites that linked information to mammography among the first 10 results that appeared in an Internet search of sites directed at the general public.
2. Methods
2.1. Women's point of view
This study adopted the perspective of women seeking information about mammography and breast cancer screening. They were aiming to obtain details about mammography following an Internet search, and they read the first appropriate Web sites they found.
2.2. Country selection
To compare Web sites providing health information about mammography and breast cancer screening throughout Europe, we relied on the European Network of Medical Residents in Public Health (EuroNet MRPH; euronetmrph.org). We contacted and presented to the EuroNet MRPH Board the study protocol and obtain their approval. After approval, we selected one member of each EuroNet MRPH national commission from a list of associate delegates. Of the 11 countries belonging to EuroNet MRPH, 10 participated in this study (Malta did not).
2.3. Search and analysis strategies
In order to bypass location-related hurdles and translation-related inaccuracies, each involved professional from EuroNet MRPH conducted a Web search in the capital city of their country or in a populous city. The following cities were identified for each country: Zagreb (Croatia), Paris (France), Dublin (Ireland), Rome (Italy), Rotterdam (Netherlands), Warsaw (Poland), Lisbon (Portugal), Ljubljana (Slovenia), Valencia (Spain), and Liverpool (United Kingdom). We were thus able to cover 7 capitals and 3 populous cities.
For each country, the local health operator selected the top 30 sites that resulted from a Google search using the key word “mammography” (translated into the local language) from May 19 to 22, 2017. The URLS for those 30 sites were then sent, via the Web, to the referent center: the Department of Experimental Medicine of University of Campania in Naples.
There, the top consecutive 10 sites that fallen within the inclusion criteria (see below) were extracted and assessed by at least 2 investigators at the referent center. Where evaluation and selection of the sites proved more difficult, those were resolved by group discussion. For the sites in Dutch, Croatian, Slovenian, and Polish, we used an external language service to translate information on the sites. For translation of the remaining languages, we made use of internal resources in our department. We chose the key word “mammography,” rather than “breast cancer screening” or other terms, to restrict translation-related disparities and following a one-word search engine strategy, to select an extremely competitive head-term keyword, selected as crucial to the research itself, as suggested by Clarke's search engine optimization.[25]
We included in this study consecutive sites that we considered provided information about mammography to the general public. We excluded sites that were linked to previously assessed sites, technical documents specifically directed at health-care personnel, the sites of private medical diagnostic centers that indicated only prices of diagnostic examinations, and pages that required user registration to be accessed.
2.4. Assessment of health information
Where available, we entered the following information into our database: source of information–reference country, position of link in the results page, type of Web site (governmental, public health organizations, private health companies, other), author of text and whether that person was a health-care worker, and last update of content; general information on mammography–its nature, recommended age, execution modality, presence of breast implants, and further diagnostic examinations in case of abnormalities; general information about breast cancer screening–national cancer screening program, screening, recommended age-range for screening, and recommended frequency of screening; potential harms and risks–false positives, false positives after biopsy, false negatives, interval cancer, overdiagnosis, early diagnosis without improved prognosis (lead-time bias), and radiation exposure; potential benefits–reduced mortality reduction and increased survival. We also took into consideration whether risks were simply identified or whether they were also adequately detailed. In addition, we assessed existing quantitative data for risks and benefits.
For the purpose of this study, we constructed a data set using Stata version 14, statistical software (StataCorp., Stata Statistical Software: Release 14, College Station, TX).
2.5. Ethics
Ethics committee approval was not required because this study did not involve patients.
3. Results
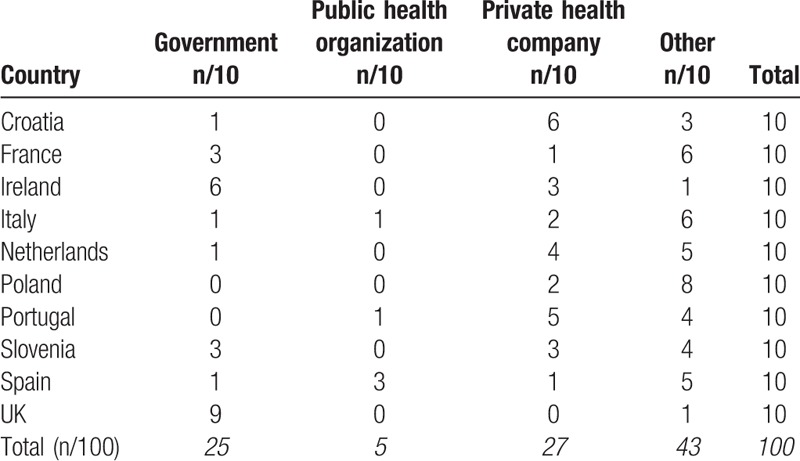
The 100 sites examined (10 for each selected country) were as follows: 27 sites of private health companies; 25 government sites; 5 of public health organizations; and 43 related to such entities as associations, magazines, blogs, and free encyclopedias (Table 1). The government sites we found were mainly in the United Kingdom (9/10) and Ireland (6/10); they were completely absent in Poland and Portugal. Conversely, private company sites were absent in the United Kingdom; they were more conspicuous in Croatia (6/10) and Portugal (5/10). Almost all the Polish sites belonged to the “other” category (8/10).
Table 1.
Web site types according to country.
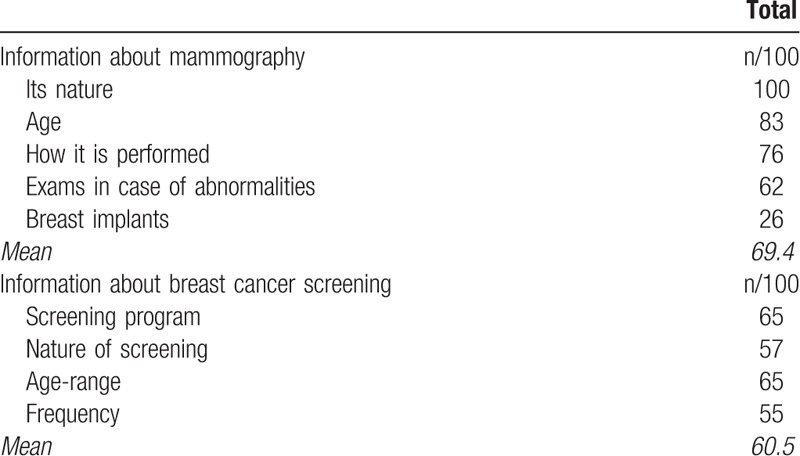
The general information we found about mammography and breast cancer screening appears in Table 2. All the sites provided an explanation of mammography; 83% indicated the recommended screening age; however, fewer sites provided information about mammography in the case of breast implants (26%). The mean proportion of sites that offered information about screening mammography (i.e., its nature, national programs, age-range, and frequency) was 60.5%.
Table 2.
General information about mammography and breast cancer screening.
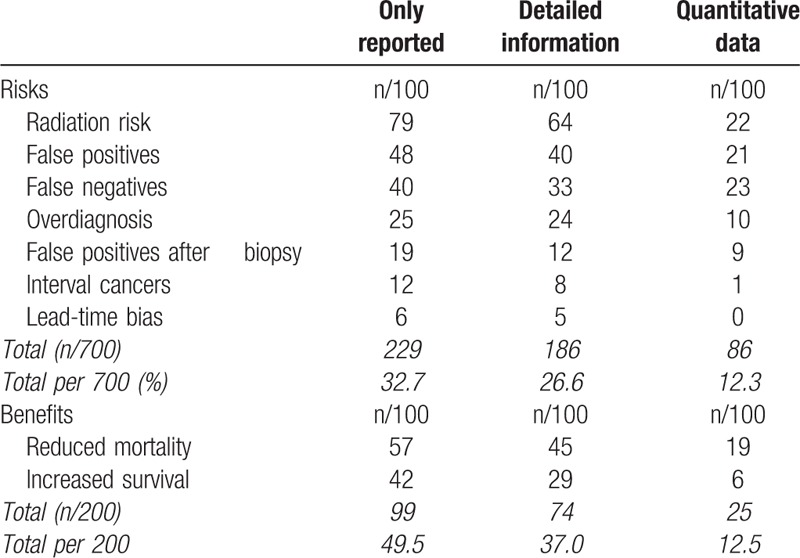
Data about the risks and benefits are shown in Table 3. The most reported information concerned radiation risks (79%). The remaining risks and benefits accounted for under 50%; interval cancer and lead-time bias were less reported: 12% and 6%, respectively. Table 3 also presents detailed information and quantitative data (i.e., percentages for occurrence) for each investigated item. We found 57 instances of reduced mortality times and 42 of increased survival.
Table 3.
Information about risks and benefits.
Information about risks and benefits according to country appears in Table 4. It is evident there that the United Kingdom provided the most information: its sites reported 39 of all 70 (56%) possible total risks. Overall, 5 nations disclosed over 35% of the possible information (United Kingdom, Spain, France, Ireland, and Italy); the others were under 30% (Portugal, Poland, Slovenia, Netherlands, and Croatia). Regarding benefits, the most complete sites were those in France (19/20) and Poland (18/20).
Table 4.
Information about risks and benefits, ranked from most to least informative country concerning risks.
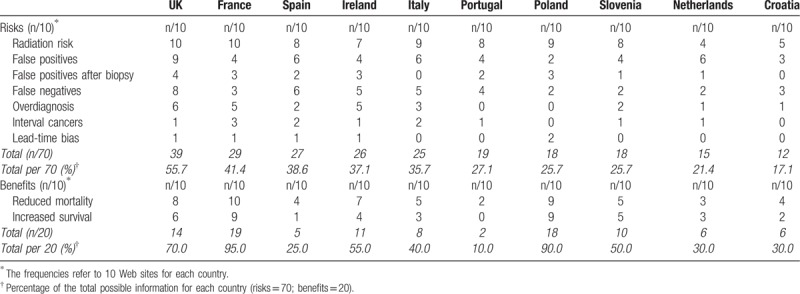
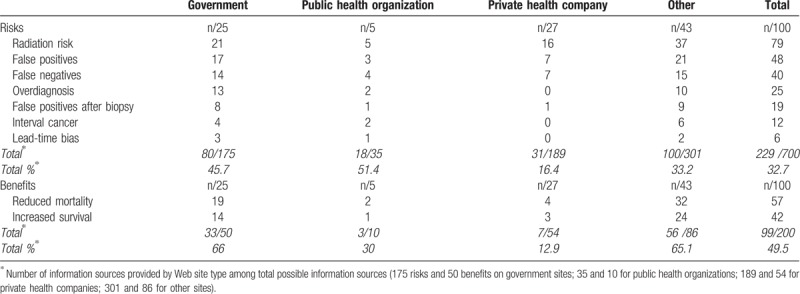
Table 5 displays the risks and benefits according to type of Web site. Regarding risks, the most complete sites were those of public health organization (51.4%); the most deficient were those of private companies (16.4%). Government sites appeared to be the most complete with respect to clarifying issues related to benefits (66%).
Table 5.
Information about risks and benefits according to Web site type.
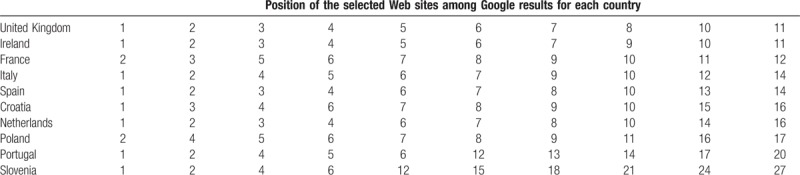
For each country, it is reported how many sites had to be opened to find the 10 most useful ones (Table 6). In the case of the United Kingdom and Ireland, the top 10 useful sites appeared among the first 11 results; therefore, only 1 site was excluded. For Portugal and Slovenia, it was necessary to open 20 and 26 sites, respectively.
Table 6.
Position of selected Web sites among Google results for each country.
4. Discussion
Due to the revolution brought by Internet, nowadays more and more patients consult the available online information and try to acquire notion regarding their health status through Web pages, with the aim of improving their wellness. However, beside the presence of many reliable health-related Web sites, patients may run into potentially misleading or inaccurate information when navigating the Internet. Indeed, much of the available information on the Internet does not pass through a review process and does not provide a source of authorship or origin.[26,27]
This study offers a general overview of Internet information on breast cancer screening available during the same period in 10 European countries. Starting from an ideal situation of complete information, whereby all 100 sites of the 10 countries would report all 7 risks (100% completeness), we found that 32.7% of the sites mentioned risks; only 26.6% explained the risks. Other studies have reported such lack of information–both with respect to the Internet[21,28,29] and in written documentation.[22–24,30–33] However, in a comparison of older and more recent studies, it is clear that there has been some improvement in the information level.[28,31] That trend is particularly evident in the case of overdiagnosis. That was scarcely reported until recently for 2 reasons: it was not properly recognized; the risk communication might dissuade women from participating in screening. In 2009, Gummersbach et al[22] analyzed information brochures about breast cancer screening in 4 European countries (Germany, Italy, Spain, and France); they found that no documents had any information about overdiagnosis. In the present study, we found that overdiagnosis was reported and explained in, respectively, 25% and 24% of the examined Web sites. One northern European study in 2004 found information about overdiagnosis in 7 of 27 (25.9%) Scandinavian and English-language Web sites.[29] In the present study, 11 of 20 (55.0%) sites in the United Kingdom and Ireland reported overdiagnosis.
Among the 10 countries, the United Kingdom provided the most complete information (56% of the risks reported). The issue of breast cancer screening is much debated in Britain. For example, the Independent Breast Screening Review, commissioned by the Department of Health of the United Kingdom, recommends that clear information about the benefits and risks should be given to women to empower them to make an informed choice.[34] Thus, since September 2013, British women invited to participate in mammography have received more detailed information about breast cancer screening than they previously did.[19]
Accessibility to information also depends on how many sites need to be opened to obtain useful information for decision-making. The United Kingdom and Ireland, produced 10 useful sites among the first 11 results. Generally, countries that offered more information produced more useful sites among the initial results. Thus, the 5 countries that offered the least information (under 30%) also produced the worst results: the top 10 useful sites did not appear until beyond the first 16 results (16–27).
Many sites reported only risks without providing any explanation; that practice could be considered supplying incorrect or incomplete information to women. Such terms as “false positive” and “overdiagnosis” may be unclear to many people. Accordingly, detailed information (column 2 in Table 2) signifies informative data. Also quantitative data were scarcely reported; that is probably the main reason for the great variability in the information presented on the same topic reported in literature.
In this study, we distinguished between institutional sites (those of governments and public health organizations) and non-institutional sites (those of private health companies and others). As we expected, the former were more informative than the latter–even if the former did not exceed the 50% threshold for given information. Moreover, non-institutional sites were prevalent in all countries; the exceptions were the United Kingdom, which has a well-established national health service, and–partially–Ireland. That could be an additional reason for our finding more information on English sites. By contrast, institutional sites were absent in Poland and mostly absent in the Netherlands, Croatia, and Portugal; those countries presented, on average, less informative Web sites.
Our results suggest that despite consensus in the scientific community for better information for citizens, further efforts are needed to improve information about breast cancer screening. That is necessary even among the countries we identified as having given better results.
Furthermore, regarding mammography, it's known that all women undergoing regular screening for breast cancer are at risk for false-positive results and unnecessary biopsies, as well as–particularly for younger patients–overdiagnosis, with subsequent treatment of non-invasive breast cancer that would otherwise not have become a threat to their health, or even apparent, during their lifetime.[35] Women should be completely aware of such information. Indeed, one of the most debated issues in clinical ethics is the contrast between patient's autonomy and the idea that medicine shall serve the interests of the patients, regardless of their complete self-determination.[36] All medical intervention, instead, are required to be approved by a well-informed patient, where information is an essential right of the person with disease. Screening procedures, for their part, must be subject to the same principle, even when they are designed for reducing consequences of life-threatening diseases and for saving lives.
Several instruments and guidelines have been proposed to assist patients and providers in evaluating the quality of medical and health information on the Internet.[37] Physicians may assist their patients by serving as guides to help them to find reliable material. Then, they may routinely inquire about their patients’ use of the Internet to obtain medical information. Moreover, health care providers should be prepared to offer to the patients suggestions for health resources and to assist them in evaluating the quality of health information available on the Internet.[38]
The main limitations of the study are as follows. The keyword “mammography” may not be equally appropriate among the 10 countries we investigated. Women may use other key words, such as “breast cancer,” “breast cancer screening,” and “breast cancer prevention.” As noted above, we chose “mammography” since it is a single word and therefore easier for searches and data management. The EuroNet MRPH does not include some important European countries, such as Germany and those of Scandinavia; accordingly, those places were not included in this study. We encountered some problems in the translation of Croatian, Slovenian, Dutch, and Polish with respect to both finding translators and agreeing on the most suitable translation for the purposes of our study. Those were the countries that had less informative sites, and so the 2 items (less information and difficulty in translation) could be related.
Yet, the found lack of information in certain countries can be explained by their health policies; nevertheless an adjustment of the results by the health care policies of each nation could not be performed because of the design study.
Finally, differences in the uses of the Internet and in the dissemination of health information (leaflets, booklets, brochures, pamphlets, technical reports) across the countries might have affected the results.
In conclusion, while information to the public about breast screening in many countries is still lacking, it is encouraging to see that a greater recognition of harms, such as overdiagnosis, in scientific circles is filtering through to the public as well, as shown in this study of information on Web sites in 10 European countries. Further efforts and studies are required to foster better informed decision-making policies in European countries.
Acknowledgments
The authors gratefully acknowledge the European Network of Medical Residents in Public Health and the participating residents. The members of the Collaborative Working Group are as follows: Miguel Cabral, Portugal; Damiano Cerasuolo, France, Damir Ivankovič, Croatia; Alberto Mateo-Urdiales, United Kingdom; Julio Muñoz-Miguel, Spain; Paulina Maria Nowicka, Poland; Naomi Petty-Saphon, Ireland; Pedro Prata-Andrade, Netherlands; Matej Vinko, Slovenia.
They also thank the Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Author contributions
Authorship: FA concepted and designed the study, contributed to data interpretation. LS, MN, PF, and VDP contributed to data collection, performed data entry, and contributed to data interpretation. All authors were involved in drafting, revising and finalizing the manuscript, and approved the final version which was submitted for publication.
Conceptualization: Francesco Attena.
Data curation: Laura Spagnoli, Monica Navaro, Pietro Ferrara, Viola Del Prete.
Investigation: Laura Spagnoli, Monica Navaro, Pietro Ferrara, Viola Del Prete.
Methodology: Francesco Attena.
Supervision: Francesco Attena.
Writing – original draft: Laura Spagnoli, Monica Navaro, Pietro Ferrara, Viola Del Prete.
Writing – review & editing: Francesco Attena.
Footnotes
Abbreviations: EuroNet MRPH = European Network of Medical Residents in Public Health, MRPHs = Medical Residents in Public Health.
Viola Del Prete is an Italian delegate for European Network of Medical Residents in Public Health.
Funding: None declared.
Authors declare no competing interests.
Contributor Information
Collaborators: and the Collaborative Working Group
References
- [1].Lannin DR, Wang S. Are small breast cancers good because they are small or small because they are good? N Engl J Med 2017;376:2286–91. [DOI] [PubMed] [Google Scholar]
- [2].Schmidt H. The ethics of incentivizing mammography screening. JAMA 2015;314:995–6. [DOI] [PubMed] [Google Scholar]
- [3].Kopans DB. An open letter to panels that are deciding guidelines for breast cancer screening. Breast Cancer Res Treat 2015;151:19–25. [DOI] [PubMed] [Google Scholar]
- [4].Printz C. Mammogram debate flares up: latest breast cancer screening study fuels controversy. Cancer 2014;120:1755–6. [DOI] [PubMed] [Google Scholar]
- [5].Fitzgerald SP. Breast-cancer screening. N Engl J Med 2012;366:191–2. [DOI] [PubMed] [Google Scholar]
- [6].Duffy SW, Smith RA. More on screening mammography. N Engl J Med 2011;364:281–6. [DOI] [PubMed] [Google Scholar]
- [7].Jørgensen KJ. Mammography screening. Benefits, harms, and informed choice. Dan Med J 2013;60:B4614. [PubMed] [Google Scholar]
- [8].Ploug T, Holm S, Brodersen J. To nudge or not to nudge: cancer screening programmes and the limits of libertarian paternalism. Epidemiol Community Health 2012;66:1193–6. [DOI] [PubMed] [Google Scholar]
- [9].Quanstrum KH, Hayward RAN. Lessons from the mammography wars. N Engl J Med 2010;363:1076–9. [DOI] [PubMed] [Google Scholar]
- [10].Miller AB, Wall C, Baines CJ, et al. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ 2014;348:g366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Mukhtar TK, Yeates DR, Goldacre MJ. Breast cancer mortality trends in England and the assessment of the effectiveness of mammography screening: population-based study. J R Soc Med 2013;106:234–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Beau AB, Lynge E, Njor SH, et al. Benefit-to-harm ratio of the Danish breast cancer screening programme. Int J Cancer 2017;141:512–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Raichand S, Dunn AG, Ong MS, et al. Conclusions in systematic reviews of mammography for breast cancer screening and associations with review design and author characteristics. Syst Rev 2017;6:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].van den Ende C, Oordt-Speets AM, Vroling H, et al. Benefits and harms of breast cancer screening with mammography in women aged 40-49 years: a systematic review. Int J Cancer 2017;141:1295–306. [DOI] [PubMed] [Google Scholar]
- [15].Broeders M, Paci E. The balance sheet of benefits and harms of breast cancer population-based screening in Europe: outcome research, practice and future challenges. Womens Health (Lond) 2015;11:883–90. [DOI] [PubMed] [Google Scholar]
- [16].Løberg M, Lousdal ML, Bretthauer M, et al. Benefits and harms of mammography screening. Breast Cancer Res 2015;17:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Hersch J, Barratt A, Jansen J, et al. The importance of enabling informed decision making for women considering breast cancer screening. J Med Screen 2016;23:55. [DOI] [PubMed] [Google Scholar]
- [18].Kuppermann M, Sawaya GF. Shared decision-making: easy to evoke, challenging to implement. JAMA Intern Med 2015;175:167–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Forbes LJ. Ramirez AJ, the expert group on information about breast screening. Offering informed choice about breast screening. J Med Screen 2014;21:194–200. [DOI] [PubMed] [Google Scholar]
- [20].Attena F, Cancellieri M, Pelullo CP. Scarce information about breast cancer screening: an Italian websites analysis. Medicine (Baltimore) 2016;95:e5615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ferreira D, Carreira H, Silva S, et al. Assessment of the contents related to screening on Portuguese language websites providing information on breast and prostate cancer. Cad Saúde Pública 2013;29:2163–76. [DOI] [PubMed] [Google Scholar]
- [22].Gummersbach E, Piccoliori G, Zerbe CO, et al. Are women getting relevant information about mammography screening for an informed consent: a critical appraisal of information brochures used for screening invitation in Germany, Italy, Spain and France. Eur J Public Health 2010;20:409–14. [DOI] [PubMed] [Google Scholar]
- [23].Giordano L, Rowinski M, Gaudenzi G, et al. What information do breast cancer screening programmes provide to Italian women? Eur J Public Health 2005;15:66–9. [DOI] [PubMed] [Google Scholar]
- [24].Slaytor EK, Ward JE. How risks of breast cancer and benefits of screening are communicated to women: analysis of 58 pamphlets. BMJ 1998;317:263–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Clarke A. SEO 2016: Learn SEO with Smart Internet Marketing Strategies. CreateSpace. USA, 3rd ed. 2015. [Google Scholar]
- [26].Eysenbach G, Powell J, Kuss O, et al. Empirical studies assessing the quality of health information for consumers on the world wide web: a systematic review. JAMA 2002;287:2691–700. [DOI] [PubMed] [Google Scholar]
- [27].Bernstam EV, Walji MF, Sagaram S, et al. Commonly cited website quality criteria are not effective at identifying inaccurate online information about breast cancer. Cancer 2008;112:1206–13. [DOI] [PubMed] [Google Scholar]
- [28].Ghanouni A, Meisel SF, Hersch J, et al. Information on ’Overdiagnosis’ in breast cancer screening on prominent United Kingdom- and Australia-Oriented Health Websites. PLoS One 2016;11:e0152279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Jørgensen KJ, Gøtzsche PC. Presentation on websites of possible benefits and harms from screening for breast cancer: cross sectional study. BMJ 2004;328:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Sadigh G, Singh K, Gilbert K, et al. Mammography patient information at hospital websites: most neither comprehensible nor guideline supported. AJR Am J Roentgenol 2016;207:947–51. [DOI] [PubMed] [Google Scholar]
- [31].Castagno R, Canuti D, Petrella M, et al. Information provided by Italian breast cancer screening programmes: a comparison between 2001 and 2014. Epidemiol Prev 2015;39(3 suppl 1):48–51. [PubMed] [Google Scholar]
- [32].Gøtzsche PC, Jørgensen KJ. The breast screening programme and misinforming the public. J R Soc Med 2011;104:361–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Kurzenhäuser S. What kind of information do German health information pamphlets provide on mammography screening? Z Arztl Fortbild Qualitatssich 2003;97:53–7. [PubMed] [Google Scholar]
- [34].Marmot M, Altman DG, Cameron DA, et al. The benefits and harms of breast cancer screening: an independent review. Lancet 2012;380:1778–86. [DOI] [PubMed] [Google Scholar]
- [35].Houssami N. Overdiagnosis of breast cancer in population screening: does it make breast screening worthless? Cancer Biol Med 2017;14:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Entwistle VA, Carter SM, Cribb A, et al. Supporting patient autonomy: the importance of clinician-patient relationships. J Gen Intern Med 2010;25:741–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Winker MA, Flanagin A, Chi-Lum B, et al. Guidelines for medical and health information sites on the internet: principles governing AMA web sites. American Medical Association. JAMA 2000;283:1600–6. [DOI] [PubMed] [Google Scholar]
- [38].Diaz JA, Griffith RA, Ng JJ, et al. Patients’ use of the Internet for medical information. J Gen Intern Med 2002;17:180–5. [DOI] [PMC free article] [PubMed] [Google Scholar]


