Abstract
Treatment strategies for small side branch compromise related to main vessel stenting are not well investigated and not established.
This study is to compare the clinical prognosis of different strategies for bifurcations with or without percutaneous coronary intervention (PCI) of small side branch after it compromised.
A total of 119 consecutive bifurcation subjects from January 2013 to March 2015 were enrolled, all bifurcations were characterized by small side branch (1.5 mm ≤side branch diameter ≤2.5 mm). Subjects were assigned into side branch treatment (SBT) group and nonside branch treatment group (NSBT) according to whether advanced treatment of side branch was taken or not after it compromised. Major adverse cardiovascular event (MACE) was evaluated, so were the CCS angina and NYHA heart function classification.
SBT subjects were associated with longer procedure time (46.7 vs 19.6 min, P < .001) and more complications (18.9% vs 0.0%, P < .001). 12 MACEs were followed including 4 in SBT group and 8 in NSBT group (10.8% vs 9.8%, P = 1.00). There were no significant difference between 2 groups regarding the CCS and NYHA classification, neither were the calculated classification improvement rate, respectively. In subgroup analysis for true and nontrue bifurcations, no statistical difference was found in terms of the MACE rate, the CCS, and NYHA classification improvement rate.
Nontreatment of side branch will not increase the risk of MACE and will not worsen the CCS and NYHA classification when small side branch compromises during the bifurcation PCI.
Keywords: bifurcation intervention, percutaneous coronary intervention, side branch
1. Introduction
Bifurcation lesion is technically challenging and associated with bad prognosis due to high risk of acute occlusion of side branch (SB) or main vessel (MV) and in-stent restenosis,[1] it accounts for 15% to 20% among all the percutaneous coronary intervention (PCI) cases.[2] Large amount of clinical trials about bifurcation PCI strategies have been carried out but its effectiveness and safety still remain controversial. In the Nordic bifurcation study, MV stenting with optional SB treatment (provisional-T) showed similar major adverse cardiovascular event (MACE) rate with planned 2 vessels stenting strategy.[3] In the SMART-STRATEGY trial, aggressive treatment of compromised SB after MV stenting resulted in similar 1-year, but higher 3-year target vessel failure rate, compared with conservative strategy.[4,5] However, in the DKCRUSH-II study, planned 2 vessels stenting showed significant reduction of target vessel revascularization (TVR) and target lesion revascularization rate.[6] Although controversy persists, provisional-T strategy is now considered as the standard PCI technique for most bifurcations, because of its noninferiority along with less radiation time and less contrast agent consumption.[7] However, 2 main problems are noted in most bifurcation trials:in most trials, only large SB bifurcations [side branch diameter (SBD) >2.5 mm] were studied, but small SB (SBD ≤ 2.5 mm) were left uninvestigated. Although, Nordic (SBD > 2.0 mm) and CACTUS (2.25 < SBD < 2.5 mm) studies included part of bifurcations with an SBD ≤ 2.5 mm,[3,8] very few trials were designed particularly for small SB bifurcations. Some researcher doubted the importance of small SB, for instance, Chen et al[6] pointed out that small SB compromise would not cause poor prognosis. In addition, Kralev S found that small SB (SBD > 1.0 mm) closure did not increase the risk of MACE.[7] However, in fact, the Nordic study only took small SB (SBD ≤ 2.0 mm) as an exclusive criterion, but never provided proof that small SB was not important. In addition, Kralev S's study had very small sample size and significant imbalance between groups in terms of sample size (n = 10 vs n = 70), which might reveal biased findings. Actually, small SB closure was associated with elevated periprocedural and recurrent myocardial infarction (MI) risk in 30 days.[9,10] Therefore, small SB did not act as a dispensable role like other researchers concluded and PCI strategies for bifurcations with small SB worth further evaluation. Large amount of published bifurcation studies tended to focus on the MACE rate and angiographic outcomes, but ignored patients’ symptom improvement. In contrast, from patients’ perspective, the major purpose for receiving PCI was controlling symptoms and improving quality of life. In our clinical practice, if large SB (SBD > 2.5 mm) compromise after MV stenting, most operators will reopen SB with stent or balloon, but when it comes to small SB (SBD ≤ 2.5 mm), different operators use various strategies from letting alone to aggressive treatment. Therefore, we performed a trial to study the treatment strategies when small SB compromise after MV stenting, which paid particular attention to bifurcations with 1.5 mm ≤ SBD ≤ 2.5 mm. We took not only MACE, but also CCS angina classification and NYHA heart function classification, as outcomes of interest.
2. Materials and methods
2.1. Patients and study design
The present study was a retrospective, single-center study designed to compare side branch treatment group (SBT) and nonside branch treatment group (NSBT) when small SBs compromised during the coronary bifurcations PCI with drug-eluting stents (DES). A total of 119 consecutive bifurcation patients who underwent PCI in the Second Xiangya hospital from January 2013 to March 2015 were enrolled. Bifurcation patients who aged 18 to 85 years with a diagnosis of angina pectoris or acute MI (symptom onset to PCI > 24 h) and who confronted SB (1.5 ≤ SBD ≤ 2.5 mm) compromise after MV stenting were considered eligible for enrollment. Patients who did not tolerate aspirin, clopidogrel, or other antiplatelet drugs or whose data were incomplete were excluded from this study. Patients with chronic total occlusion in the target bifurcation vessels immediately after successful recanalization and with MV or SB TIMI < grade 2 before procedure were also excluded. Clinical, operational, and follow-up data including MACE were collected. Also collected patients’ NYHA heart function classification and CCS angina classification data before PCI and during follow-up. The study was approved by the institutional review board of the Second Xiangya Hospital. Informed consent was not required because all patients were discharged state before our analysis.
2.2. Study procedure
All PCIs were performed as follows: wiring MV and SB (or not); optional predilation of MV and/or SB; MV stenting with DES, making sure that the SB ostium was covered; advanced PCI of compromised SB was at the discretion of operators. They made the decision whether to implant another stent into SB or not if they decided to reopen the compromised SB. Postdilation or final kissing balloon inflation (FKBI) of bifurcation area was also at the discretion of individual operators. PCI for other diseased vessels if needed. All patients were pretreated with aspirin and clopidogrel; if not, 300 mg aspirin and 300 to 600 mg clopidogrel were administered as a loading dose before the procedure. Intravenous heparin was administrated to maintain an activated clotting time >300 seconds. After the procedure, clopidogrel (75 mg/day) was recommended to all patients for at least 12 months and aspirin (100 mg/day) was prescribed for life-long.
2.3. Follow-up
Clinical and operational data were obtained through reviewing the computerized medical record system and angiography system in the Second Xiangya hospital. The medicine taken information and MACE including all-caused death, cardiac death, recurrent MI (PCI related MI was not included), TVR, and definite stent thrombosis were obtained through outpatient or telephone follow-up. We evaluated patients’ NYHA heart function classification and CCS angina classification based on a dedicated questionnaire also through outpatient or telephone follow-up. All data were collected by a professional cardiologist who was blind to the assignment.
2.4. Quantitative coronary angiographic analysis
Coronary angiograms obtained before and after the stenting procedure were analyzed by an experienced operator who was blind to the patients’ assignment using a computerized quantitative coronary angiographic (QCA) analysis system (Crealife. version 3.0.3.4512). Vessel segments including bifurcation lesions consisted of the SB segment, the proximal and distal MV segments proximal or distal to the stent.[3] We measured minimal lumen diameter, reference vessel diameter, maximal lumen diameter, lesion length, and luminal stenosis degree of target vessels. Then, the acute gain and the value of maximal stent diameter minus nominal stent diameter (MSD-NSD) were calculated according to the variables assessed by QCA. We defined the minimal and reference diameter as 0 mm and the stenosis degree as 100% when TIMI flow ≤grade 1.
2.5. Definitions
There were 2 definitions for SB compromise: If SB ostial stenosis <50° before MV stenting, then it was defined as SB stenosis increased to >50° or SB TIMI flow <grade 3 or SB ostial dissection ≥type B. If SB ostial stenosis ≥50° before MV stenting, then it was defined as stenosis increase or SB TIMI flow <grade 3 or SB ostial dissection ≥type B. All-cause death, cardiac death, definite stent thrombosis, recurrent MI, and TVR were defined in accordance with the Nordic study.[3] CCS angina and NYHA heart function classification improvement was defined as a postoperation grade lower than the grade before PCI.
2.6. Statistical analysis
Continuous variables were presented as mean ± SD and were compared using the Student t test. Categorical variables were summarized as counts and percentages and were compared by chi-square test or Fisher exact test. MACE-free survival was shown by Kaplan-Meier curve. A 2-tailed P value <.05 indicated statistical significance. All statistical analyses were performed using the R 3.2.3 program.
3. Results
3.1. Baseline characteristics
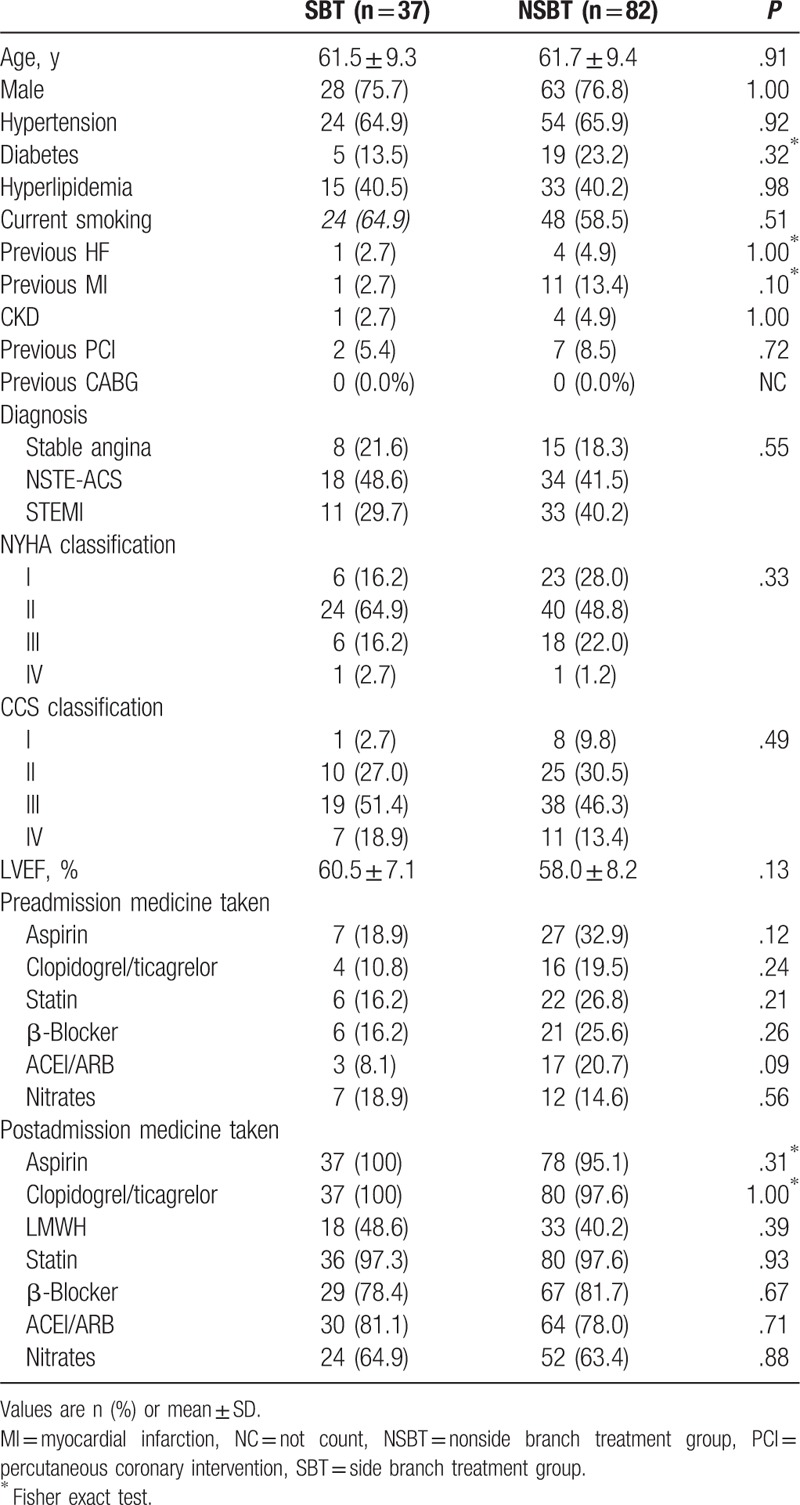
From January 2013 to March 2015, 1526 patients underwent PCI in our intervention center, among which 132 cases (8.7%) diagnosed as bifurcation lesions met with the inclusion criteria. A total of 119 cases (7.8%) were finally enrolled (SBT: n = 37; NSBT: n = 82), after excluding 13 cases (SBT: n = 4; NSBT: n = 9) with incomplete data. SBT patients were followed for 1 to 1136 days (median length of follow-up: 628 days), whereas the NSBT group was followed for 51 to 1201 days (median length of follow-up: 726.5 days). The study flow diagram is shown in Figure 1. The average age of SBT patients was 61.5 years, whereas in NSBT group it was 61.7 years. Approximately 75.7% of SBT patients were men, whereas 76.8% of NSBT patients. The 2 groups were well balanced in terms of clinical baseline characteristics (Table 1).
Figure 1.
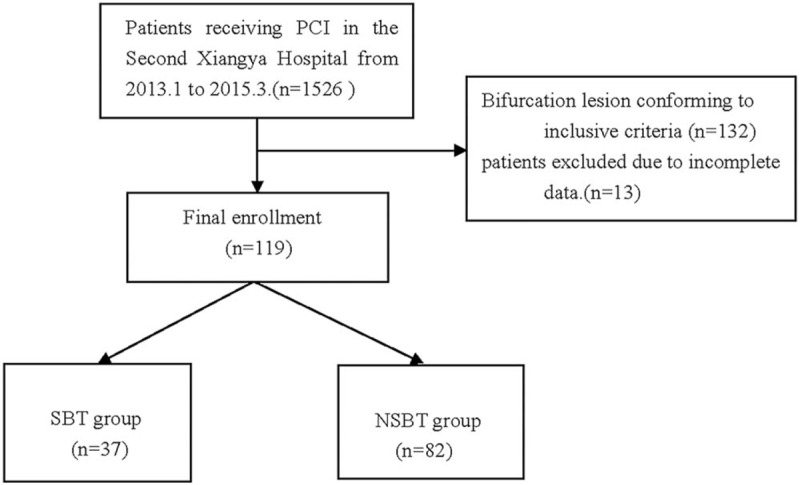
Study flow diagram. NSBT = nonside branch treatment, PCI = percutaneous coronary intervention, SBT = side branch treatment.
Table 1.
Clinical baseline characteristics.
3.2. Baseline lesion characteristics and procedural data
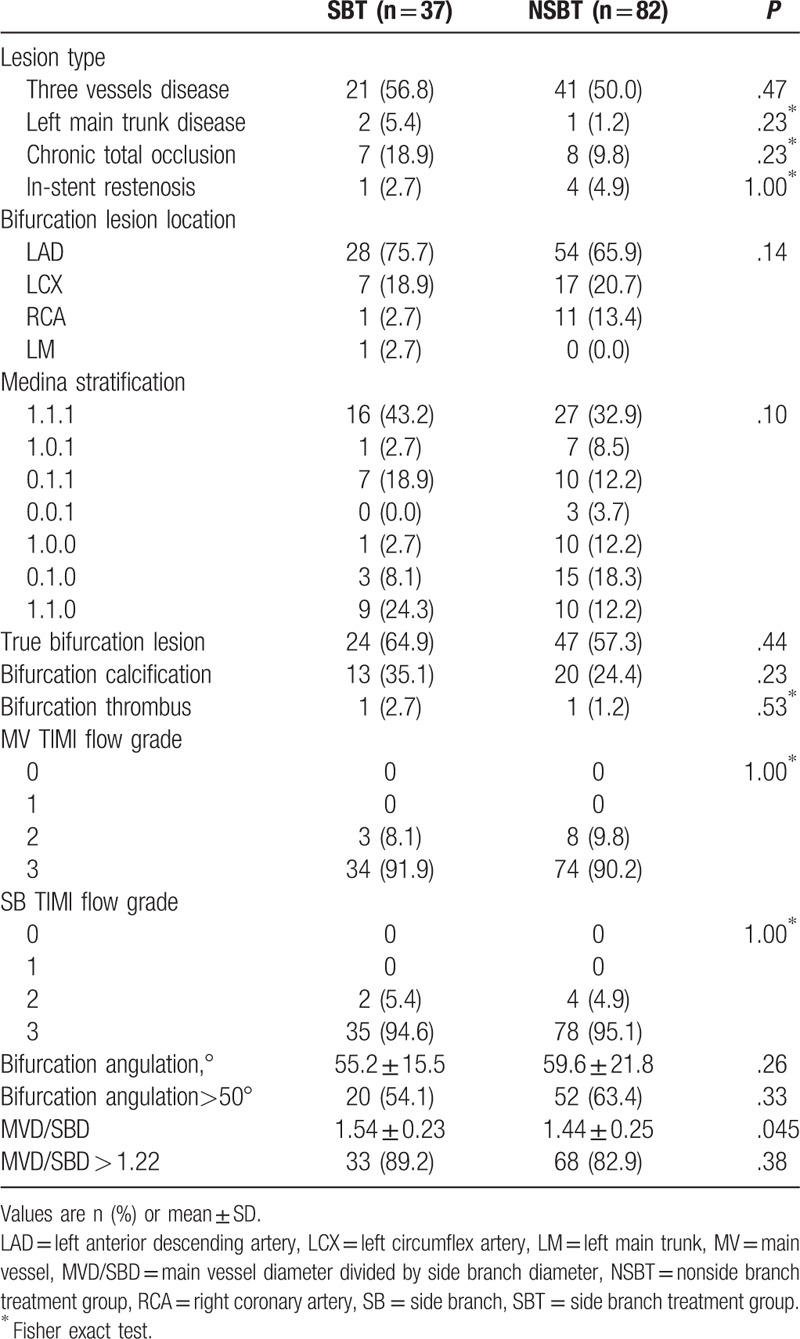
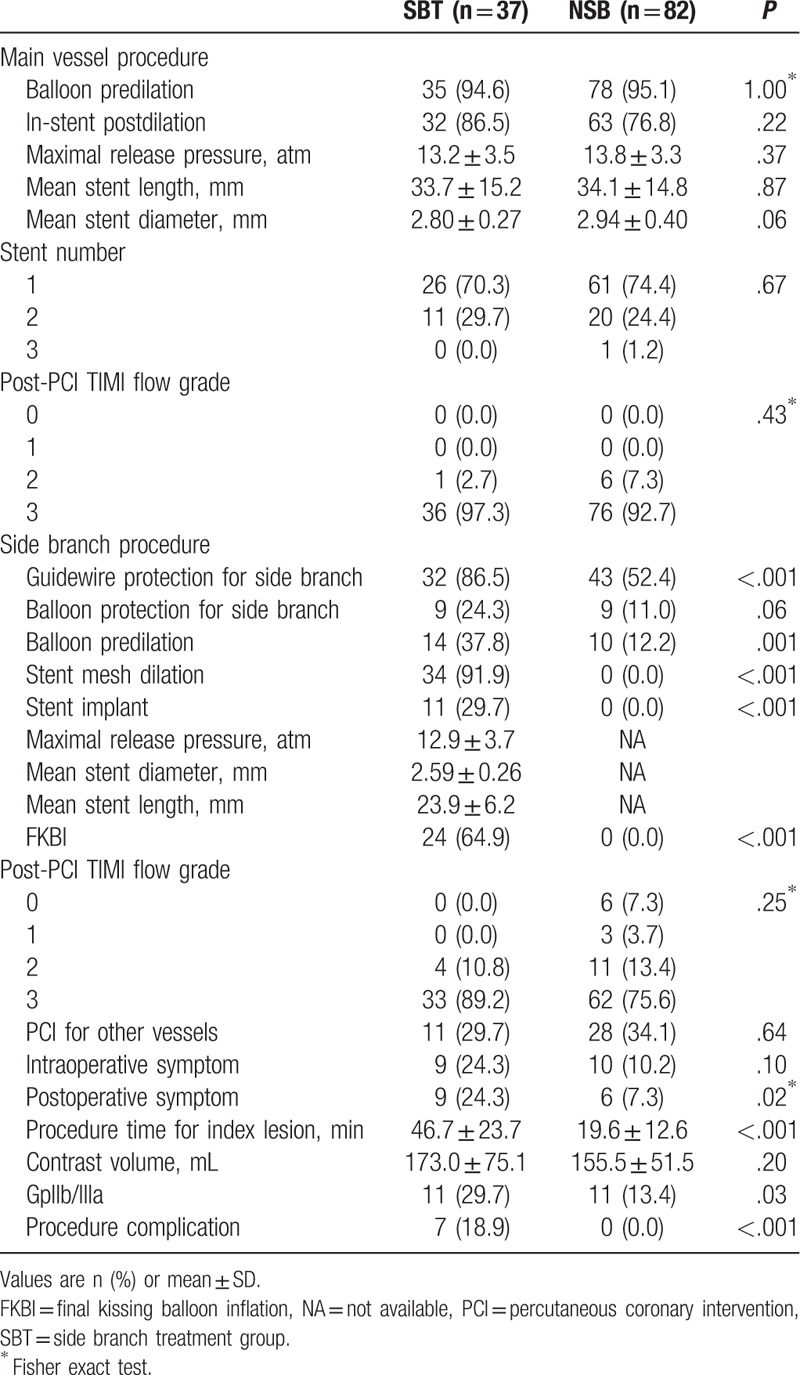
Baseline lesion characteristics are shown in Table 2. The left main bifurcations were detected in 1 patient (0.8%), 3 vessels disease in 62 patients (52.1%), and the true bifurcations were noted in 71 patients (59.7%). Most target bifurcations were located in the left anterior descending artery (68.9%). There were no significant difference between the 2 groups regarding the lesion types, lesion location, and distribution of true bifurcations based on Medina stratification (P > .05). Main vessel diameter (MVD)/SBD value in the SBT group was significantly higher than the NSBT group (1.54 vs 1.44, P = .045). However, no difference was found when comparing the MVD/SBD value of >1.22.[11,12] Procedural time of target bifurcation lesions was longer in SBT group (46.7 vs 19.6 min, P < .001), the volume of contrast used had no statistical difference, but SBT group tended to use more contrast. Stent number and total stent length implanted in MV were similar between 2 groups. SB guidewire protection technique was used more often in SBT group (86.5% vs 52.4%, P < .001), whereas balloon protection technique was used with similar frequency in 2 groups (P = .06). SB was predilated more often in SBT group (37.8% vs 12.2%, P = .001). SB dilation, SB stenting, and FKBI after SB compromise were performed in 91.9%, 29.7%, and 64.9% cases, respectively in SBT group, but none of the NSBT cases received above treatments. SB TIMI flow ≤grade 1 after MV stenting occurred in 17 patients, after target bifurcation PCI, SB TIMI flow ≤grade 1 was reduced to 9 cases, all belonged to the NSBT group.
Table 2.
Baseline lesion characteristics.
Intraprocedural symptoms were found in 19 cases, among which 1 case showed heart rate drop, 1 case showed heart rate and blood pressure drop, and 17 cases manifested chest distress or chest pain. There were 15 cases who still had symptoms after procedure, among which 9 cases had intraprocedural symptoms. Although more than half of the patients had 3-vessel disease in both groups, PCI of other coronary arteries besides target bifurcations was similar between SBT and NSBT group (29.7% vs 34.1%, P = .64). Procedural complications occurred in 7 patients, all in SBT group, including 5 cases of type A and B SB dissection all happened after SB dilation when treating compromised SB, 1 case of stent thrombosis and 1 case of type A MV dissection occurred during MV predilation. Four patients received GpIIb/IIIa receptor antagonist after occurrence of complication. Detailed procedural information is shown in Table 3.
Table 3.
Procedural characteristics.
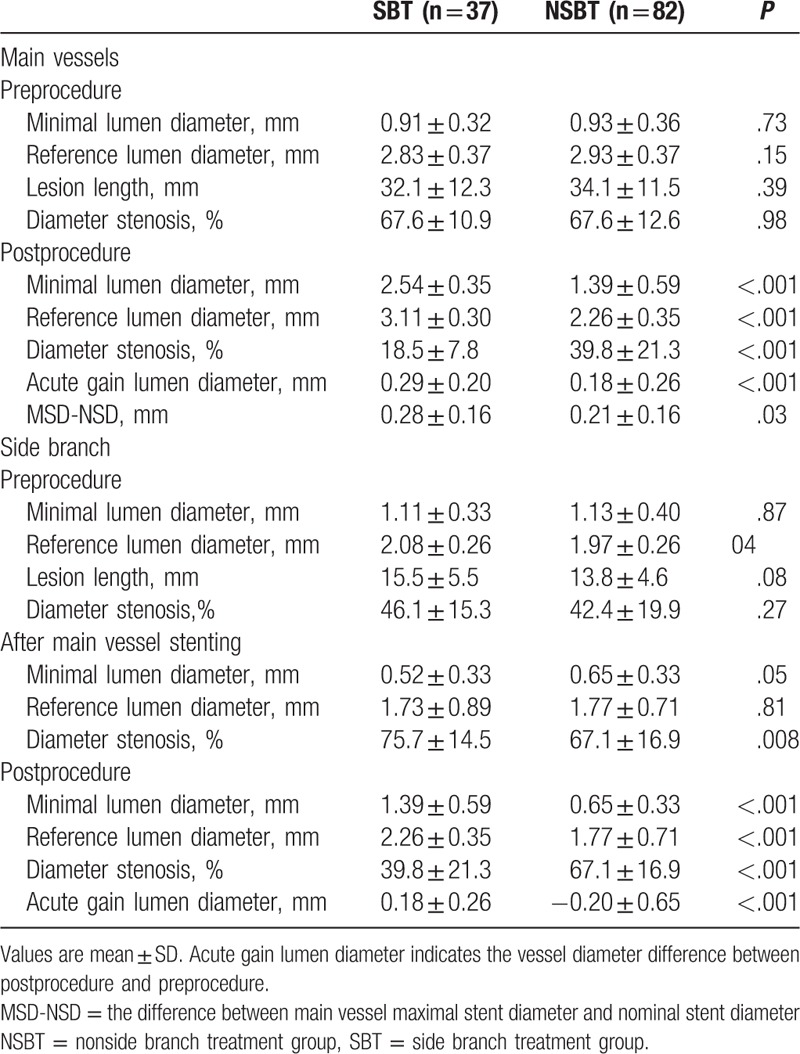
3.3. Quantitative coronary analysis
QCA analysis is shown in Table 4. There was no significant difference in terms of baseline characteristics between the 2 groups, with the exception of significantly larger SB reference diameter in SBT group (2.08 vs 1.97 mm, P = .04). SBT group was associated with higher post-MV stenting SB ostial stenosis (75.7% vs 67.1%, P = .008). After SB treatment, larger minimal lumen diameter, reference luminal diameter, and acute gain, along with lower residual lumen stenosis than in the NSBT group regarding the MV and SB, which proved that SB treatment had not only significantly decreased the luminal stenosis of SB, but also the MV. Moreover, the MSD-NSD was higher in SBT group (0.28 vs 0.21 mm, P = .03), which predicted better stent expansion in SBT group.
Table 4.
Quantitative coronary angiographic analysis for main vessels and side branches.
3.4. Clinical outcomes
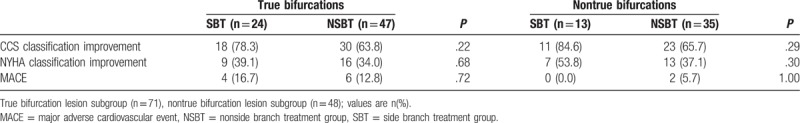
The MACE rate was similar between SBT and NSBT groups (10.8% vs 9.8%, P = 1.00∗), Kaplan-Meier curve for MACE-free survival is shown in Figure 2, and no significant difference was found by survival analysis. There were 3 cases of all-cause death, including 1 definite cardiac death occurred on the same day after PCI, 1 case of sudden death happened 157 days later after procedure and was estimated cardiac death according to his medical history of repeated chest pain before death. Both of the 2 cardiac death patients were from SBT group. Another death case came from NSBT group. The patient was diagnosed of type 2 diabetic mellitus and died of septicemia 51 days after operation puncture site infection. Seven cases of TVR, 4 cases of recurrent MI, and 2 cases of definite stent thrombosis were collected. MACE was followed in 6 patients (31.6%) among the 19 patients who had intraoperative symptom, along with 4 MACE (44.4%) among the 9 patients who have both intraoperative and postoperative symptom. Detailed clinical outcomes are shown in Table 5. In patients with true bifurcation lesions (71 cases, 59.7%), SBT (24 cases) tended to improve the CCS and NYHA classification, although no significant difference was found between SBT and NSBT groups (78.3% vs 63.8%, P = .22; and 39.1% vs 34.0%, P = .68). Similarly, in the nontrue bifurcation subgroup (48 patients, 40.3%), SBT (13 cases) tended to acquire higher CCS and NYHA classification improvement rate (84.6% vs 65.7%, P = .29; and 53.8% vs 37.1%, P = .30). No significant difference was found regarding MACE rate in both subgroups. Detailed subgroup analysis is shown in Table 6.
Figure 2.
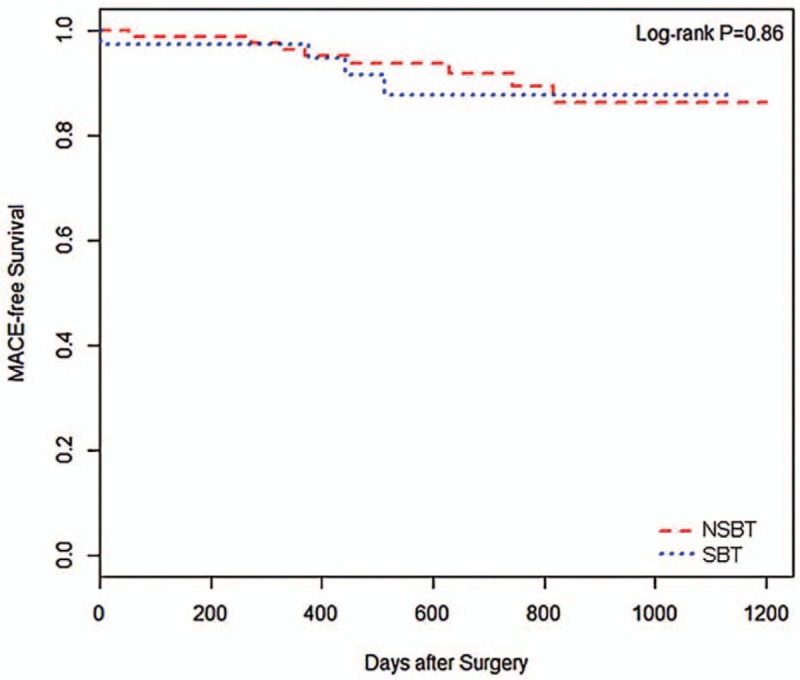
Kaplan-Meier curve. The Major Adverse Cardiac Events (MACE), defined as all-cause death, cardiac death, recurrent myocardial infarction [percutaneous coronary intervention (PCI)-related-myocardial infarction (MI) not included], target vessel revascularization (TVR) and definite stent thrombosis. NSBT = nonside branch treatment, SBT = side branch treatment.
Table 5.
Clinical outcome.
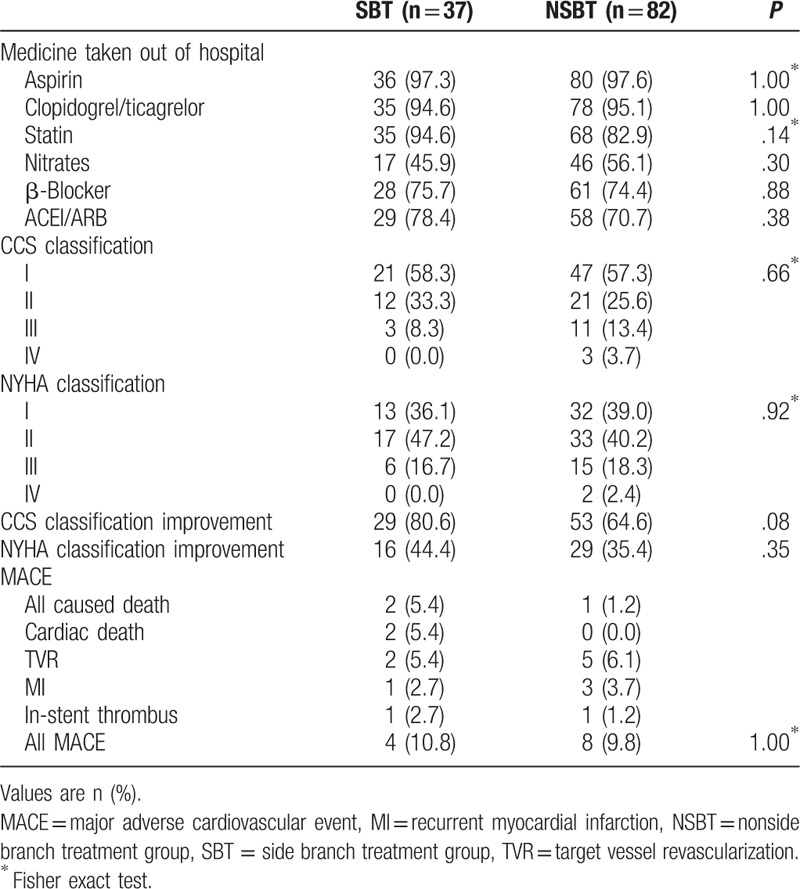
Table 6.
True and nontrue bifurcation subgroup analysis.
4. Discussion
To the best of our knowledge, this study is the first one to study PCI strategy for specific bifurcation lesions which have small SB with 1.5 mm ≤ SBD ≤ 2.5 mm. Main findings are as follows: SBT significantly increased the complication incidence and procedural time for index bifurcation lesions, when relatively small SB compromised after MV stenting. Clinical outcomes as assessed by MACE rate, CCS, and NYHA classification, CCS and NYHA classification improvement rate were similar between the 2 groups. However, CCS and NYHA classification improvement rate tended to be higher in SBT group. MACE rate, CCS, and NYHA classification improvement rate were similar between SBT and NSBT groups whether for true bifurcations or nontrue bifurcations. The SBT group also tended to obtain better CCS and NYHA classification improvement rate within both subgroups. SBT was associated with similar MACE rate to NSBT, which conformed to the previous Nordic bifurcation and DKCRUSH-II study,[3,6] while different from another single-center retrospective study which demonstrated that nontreatment of SB after it compromise was associated with lower MACE rate (23.8% vs 47.1%, P = .02).[13] However, the inclusive criteria for SBD in previous retrospective study was >1.5 mm and the largest SBD finally included even reached 3.3 mm which obviously exceeded the upper limitation 2.5 mm in our study; in other words, the previous retrospective study investigated different bifurcations with our present study. Furthermore, to be different with most previous study, CCS and NYHA classification were also compared as assessment for clinical outcomes. Interestingly, although there was no significant difference regarding CCS and NYHA classification between 2 groups, SBT patients tended to acquire higher CCS and NYHA improvement rate. Following findings may contribute to the trend to higher CCS and NYHA classification improvement rate in SBT group: SBT patients obtained lower lumen diameter stenosis, larger minimal and reference lumen diameter of SB than NSBT patients after target bifurcations PCI (39.8% vs 67.1%, P < .001; 1.39 vs 0.65 mm, P < .001; 2.26 vs 1.77 mm, P < .001). Similarly for MV after target bifurcations PCI (18.5% vs 39.8%, P < .001; 2.54 vs 1.39 mm, P < .001; 3.11 vs 2.26 mm, P < .001). This difference may attributed to more frequent FKBI among SBT patients (64.9% vs 0.0%, P < .001). SBT patients were associated with larger MV acute gain and MSD-NSD, which demonstrated better stent apposition and expansion, respectively. This may be responsible for the trend of higher CCS and NYHA classification improvement rate in SBT group, since previous study had concluded that stent malapposition and underexpansion will result in poor outcomes.[14] There were 9 patients of SB TIMI flow grade ≤1 in NSBT group after target bifurcation PCI, whereas all patients were TIMI flow grade ≥2 in SBT group, which may also contributed to the trend of higher CCS and NYHA classification improvement rate among SBT patients. It is noteworthy that CCS and NYHA classification may be influenced by PCI of nontarget vessels since 3 vessels disease was common in our enrolled patients (52.1%). Therefore, we compared the rate for treating nontarget vessels in SBT and NSBT group and no difference was found (29.7% vs 34.1%, P = .64). Given this, influence of nontarget vessels PCI on CCS and NYHA classification could be excluded. Although CCS and NYHA classification improvement rate of SBT patients tended to be higher, no statistical difference was found, which may correlate with the small sample size (n = 119) in our study. From the perspective of statistics, significant difference may emerge if more research subjects were enrolled. SBT was associated with longer target bifurcation PCI time, together with all 7 cases of procedural complications. SBT had definitely increased complication events as illustrated in our study, but even so, SBT group did not bring extra MACE risk compared with NSBT group. This could be interpreted well because most complications were type A or B dissection which had low risk of occlusion.[15] Moreover, frequent usage of FKBI may have offset part of adverse effects that intraoperative complications produced. Furthermore, we investigated patients with intraoperative and postoperative symptom, 6 MACE were followed among all 19 intraoperative symptom patients (31.6%), whereas the rate was 6.0% among other 100 nonoperative symptom patients. Four MACE (44.4%) were collected among all 9 patients who had both intraoperative and postoperative symptoms, whereas the rate was as low as 7.3% among other 110 patients. Although we did not perform statistical analysis because of great sample size deviation, we could also speculate that intraoperative symptoms may be associated with poor prognosis especially for the patients who have both intraoperative and postoperative symptoms.
4.1. Study limitations
We recognize several limitations to this study. First, the data come from a single center, this may detract from the ability to generalize to other centers overall. Second, this was a retrospective study with small number of cases, small enrolled cases and inevitable uncontrolled bias made it difficult to reach definite conclusion. A large patient sample and a perspective study were needed to gain a definite conclusion. Finally, some confounders were not measured in present study, such as antiplatelet dosage, patients who received SBT may be prescribed higher dosage of antiplatelets which may bring potential bias to our study.
5. Conclusion
Nontreatment of SB will not increase the risk of MACE and will not worsen the CCS and NYHA classification when small SB compromises during the bifurcation PCI.
Author contributions
Data curation: Xiao-fan Peng, Jia-bing Huang, Zheng-hua Xing, Zhao-wei Zhu, Bo Dong, Xiang-yu Meng, Zhen-fei Fang, Xin-qun Hu.
Formal analysis: Jia-bing Huang, Zheng-hua Xing, Xiang-yu Meng, Zhen-fei Fang, Xin-qun Hu.
Funding acquisition: Shenghua Zhou.
Investigation: Bo Dong.
Methodology: Xiao-fan Peng, Jia-bing Huang, Zhao-wei Zhu, Xiang-yu Meng, Zhen-fei Fang, Xin-qun Hu, Shenghua Zhou.
Project administration: Xiao-fan Peng.
Software: Xiang-yu Meng.
Supervision: Xin-qun Hu.
Writing – original draft: Xiao-fan Peng.
Writing – review and editing: Shenghua Zhou.
Footnotes
Abbreviations: DES = drug-eluting stent, FKBI = final kissing balloon inflation, MACE = major adverse cardiovascular event, MSD = maximal stent diameter, MV = main vessel, MVD = main vessel diameter, NSBT = nonside branch treatment group, NSD = nominal stent diameter, PCI = percutaneous coronary intervention, QCA = quantitative coronary angiographic, SB = side branch, SBD = side branch diameter, SBT = side branch treatment group, TVR = target vessel revascularization.
The authors report no conflicts of interest.
References
- [1].Pinkerton CA, Slack JD, Van Tassel JW, et al. Angioplasty for dilatation of complex coronary artery bifurcation stenoses. Am J Cardiol 1985;55(13 pt 1):1626–8. [DOI] [PubMed] [Google Scholar]
- [2].Latib A, Colombo A. Bifurcation disease: what do we know, what should we do? JACC Cardiovasc Interv 2008;1:218–26. [DOI] [PubMed] [Google Scholar]
- [3].Steigen TK, Maeng M, Wiseth R, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation 2006;114:1955–61. [DOI] [PubMed] [Google Scholar]
- [4].Song YB, Hahn JY, Song PS, et al. Randomized comparison of conservative versus aggressive strategy for provisional side branch intervention in coronary bifurcation lesions: results from the SMART-STRATEGY (Smart Angioplasty Research Team-Optimal Strategy for Side Branch Intervention in Coronary Bifurcation Lesions) randomized trial. JACC Cardiovasc Interv 2012;5:1133–40. [DOI] [PubMed] [Google Scholar]
- [5].Song YB, Park TK, Hahn JY, et al. Optimal strategy for provisional side branch intervention in coronary bifurcation lesions: 3-year outcomes of the SMART-STRATEGY randomized trial. JACC Cardiovasc Interv 2016;9:517–26. [DOI] [PubMed] [Google Scholar]
- [6].Chen SL, Santoso T, Zhang JJ, et al. A randomized clinical study comparing double kissing crush with provisional stenting for treatment of coronary bifurcation lesions: results from the DKCRUSH-II (Double Kissing Crush versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions) trial. J Am Coll Cardiol 2011;57:914–20. [DOI] [PubMed] [Google Scholar]
- [7].Stankovic G, Lefevre T, Chieffo A, et al. Consensus from the 7th European Bifurcation Club meeting. EuroIntervention 2013;9:36–45. [DOI] [PubMed] [Google Scholar]
- [8].Colombo A, Bramucci E, Sacca S, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) study. Circulation 2009;119:71–8. [DOI] [PubMed] [Google Scholar]
- [9].Zhang D, Xu B, Yin D, et al. Predictors and periprocedural myocardial injury rate of small side branches occlusion in coronary bifurcation intervention. Medicine (Baltimore) 2015;94:e992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Muramatsu T, Onuma Y, Garcia-Garcia HM, et al. Incidence and short-term clinical outcomes of small side branch occlusion after implantation of an everolimus-eluting bioresorbable vascular scaffold: an interim report of 435 patients in the ABSORB-EXTEND single-arm trial in comparison with an everolimus-eluting metallic stent in the SPIRIT first and II trials. JACC Cardiovasc Interv 2013;6:247–57. [DOI] [PubMed] [Google Scholar]
- [11].Gil RJ, Vassilev D, Formuszewicz R, et al. The carina angle-new geometrical parameter associated with periprocedural side branch compromise and the long-term results in coronary bifurcation lesions with main vessel stenting only. J Interv Cardiol 2009;22:E1–0. [DOI] [PubMed] [Google Scholar]
- [12].Dou K, Zhang D, Xu B, et al. An angiographic tool for risk prediction of side branch occlusion in coronary bifurcation intervention: the RESOLVE score system (Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion). JACC Cardiovasc Interv 2015;8(1 pt A):39–46. [DOI] [PubMed] [Google Scholar]
- [13].Von Korn H, Stefan V, Van Ewijk R, et al. Treatment of coronary bifurcation lesions: stent-covering of the side branch with and without PCI of the side branch: a retrospective analysis of all consecutive patients. BMC Cardiovasc Disord 2013;13:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Yoon HJ, Hur SH. Optimization of stent deployment by intravascular ultrasound. Korean J Intern Med 2012;27:30–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Huber MS, Mooney JF, Madison J, et al. Use of a morphologic classification to predict clinical outcome after dissection from coronary angioplasty. Am J Cardiol 1991;68:467–71. [DOI] [PubMed] [Google Scholar]


