Abstract
Post-traumatic stress disorder (PTSD) and anxiety are both prevalent in trauma-related populations. However, comorbidity of these 2 psychiatric disorders has not been investigated in flood survivors. This study aimed to estimate the extent to which PTSD and anxiety co-occur in flood survivors, and identify shared risk factors for PTSD only and comorbidity of PTSD and anxiety.
Individuals who experienced Dongting Lake flood in 1998 were enrolled in this study using stratified and systematic random sampling method. Information on social support, personality traits, PTSD, and anxiety was collected using self-report questionnaires. The intensity of exposure to the flood was measured by some questions. Logistic regression analyses were used to identify factors associated with PTSD only and comorbidity of PTSD and anxiety.
In all, 325 participants were enrolled in this study. The prevalence of PTSD, anxiety, and comorbidity of PTSD and anxiety among survivors of the 1998 Dongting Lake flood at 17-year follow-up was 9.54%, 9.23%, and 6.15%, respectively. Furthermore, 64.52% of those with PTSD had anxiety and 66.67% of those with anxiety had PTSD. Loss of relative, injury of body, damage of house, and emotional instability were shared risk factors for PTSD only and comorbidity of PTSD and anxiety, in comparison with neither PTSD nor anxiety.
Post-traumatic stress disorder only and comorbidity of PTSD and anxiety are prevalent in flood survivors, and are both related to the intensity of exposure to the flood and personality traits, indicating that integrated intervention strategies of PTSD and anxiety for flood survivors are needed.
Keywords: anxiety, comorbidity, flood, post-traumatic stress disorder, risk factor
1. Introduction
Post-traumatic stress disorder (PTSD) is the most prevalent psychiatric disorder in trauma-related populations, followed by anxiety.[1,2] Furthermore, for the type of trauma which may cause long-term effects, such as wars and natural disasters, comorbidity of PTSD and anxiety is the rule rather than the exception. For example, nearly a fifth of the elderly survivors of the Wenchuan earthquake met the criteria for both PTSD and anxiety,[3] and in Northern Uganda, more than a third of the former abductees were identified with both PTSD and anxiety.[4] In addition, about 87% of the Iranian Chemical Warfare survivors who developed PTSD also suffered from anxiety,[5] and the prevalence of anxiety among female Bosnian refugees with PTSD was 97.1%.[6]
Comorbidity involving PTSD may lead to decreased health-related quality of life,[7] and the risk for committing suicide in those with comorbidity involving PTSD has been notably higher than in those who suffered from either of them.[8] Moreover, evidence has shown that when PTSD and other psychiatric disorder co-occur in trauma-related populations, a combined stress model with a shared vulnerability and similar risk factors might be formed.[9,10] In this regard, identifying shared risk factors for PTSD only and comorbidity involving PTSD is of great significance. Currently, studies exploring comorbidity involving PTSD have mostly focused on survivors of wars and earthquakes,[3,6] and this has not been investigated in flood survivors.
Floods are among the most destructive natural disasters globally,[11,12] and also frequently occur in China. For example, in Hunan Province of China, a flood that hit the Dongting Lake in 1998, affecting hundreds of thousands of people, was 1 of the most devastating floods throughout China's history.[13,14] Our previous studies have shown that the prevalence of PTSD among survivors of the 1998 Donting Lake flood at 2-year follow-up was 9.2%,[14] and 15.89% of the survivors who developed PTSD in 2000 continued to have PTSD in 2013 to 2014.[15] Comorbidity of PTSD and anxiety in this population, however, has not been identified. Therefore, this study aimed to explore the extent to which PTSD and anxiety co-occur in this population, and identify shared risk factors for PTSD only and comorbidity of PTSD and anxiety.
2. Methods
2.1. Ethics statement
This investigation was carried out in accordance with the latest version of the Declaration of Helsinki. The Ethics Committee of Xiangya School of Public Health, Central South University of China, approved this investigation, and written informed consent was obtained from the participants.
2.2. Study area and participants
This cross-sectional study was conducted in Huarong County in December 2015. Huarong County, a catchment area of Dongting Lake, was heavily hit by the 1998 Dongting Lake flood. No more flood struck this area since the Dongting Lake flood in 1998. Participants in this area were selected using stratified and systematic random sampling method. Firstly, 2 towns—Zhuzikou and Xingfu—were randomly selected from southeast Huarong, and then 4 villages were selected from each town using systematic random sampling method. Finally, due to the minimum sample size of 384 for cross-sectional studies,[16] 30% of households in these villages were randomly selected.
Inclusion criteria for this study were: having experienced the Dongting Lake flood in 1998; aged at least 7 years in 1998; and willing to participate in this study. Excluded from this study were those who have been diagnosed with any psychiatric disorders before the Dongting Lake flood in 1998, or have received any psychiatric treatment since the Dongting Lake flood in 1998, or have suffered from mental retardation or dementia. Furthermore, those with a transformed total score of at least 60 on the subscale lie of the Eysenck Personality Questionnaire—Revised, Short Scale for Chinese (EPQ-RSC) were excluded. For the purposes of this study, participants were categorized into the PTSD-only group, anxiety-only group, comorbidity of PTSD and anxiety group, and neither PTSD nor anxiety group.
2.3. Data collection
Experienced investigators were recruited from Xiangya School of Public Health, Central South University, and Huarong Center for Disease Control and Prevention. Before data collection, a unified training was conducted for all investigators. After the training, they carried out face-to-face interviews with participants to collect data on sociodemographic characteristics, intensity of exposure to the flood, social support, and personality traits. The investigators were supervised by professional psychologists during data collection procedure. Full data for this study are available upon request to the corresponding author.
2.4. Measures
2.4.1. Intensity of exposure to the flood
In accordance with previous studies exploring psychiatric disorders in survivors of natural disasters,[3,17] the intensity of exposure to the Dongting Lake flood in 1998 was measured by the following questions:
-
1.
Have you lost at least 1 family member due to the Dongting Lake flood in 1998?
-
2.
Have you or your family members been physically injured due to the Dongting Lake flood in 1998?
-
3.
Have you or your family lost most of your property due to the Dongting Lake flood in 1998?
-
4.
Have you or your family lost your livelihood due to the Dongting Lake flood in 1998?
-
5.
Have your houses been destroyed due to the Dongting Lake flood in 1998?
The above 5 questions were treated as dichotomous variables with a response of either “Yes” or “No.”
2.4.2. Social support
The Chinese version of Social Support Rating Scale (SSRS), which consists of 10 items, was used to identify the social support level. This instrument is scored on a 4-point Likert scale (1 = none, 2 = slight, 3 = moderate, 4 = great), with a total score of 12 to 44, 45 to 54, and >54, indicating low, medium, and high social support level, respectively.[18] The Chinese version of SSRS has sound reliability and validity,[19] with Cronbach alpha coefficient ranging from 0.825 to 0.896.[20]
2.4.3. Personality traits
The EPQ-RSC, which consists of 48 items each with responses “Yes” or “No,” was used to assess personality traits. This instrument comprises 4 subscales: extraversion, psychoticism, neuroticism, and lie. The original total score of each subscale was transformed based on the Chinese norm. For the subscale extraversion, a transformed total score of <43.3, 43.3 to 56.7, and >56.7 indicates introversion, middle, and extraversion, respectively. For the subscale psychoticism, a transformed total score of <43.3, 43.3 to 56.7, and >56.7 indicates mild, middle, and obstinate, respectively. Besides, for the subscale neuroticism, a transformed total score of <43.3, 43.3 to 56.7, and >56.7 indicates emotional stability, middle, and emotional instability, respectively. Furthermore, those with a transformed total score of at least 60 on the subscale lie were considered as not providing credible information and were excluded from the study.[21] The EPQ-RSC has good reliability and validity, with Cronbach alpha coefficients more than 0.70 except for the subscale psychoticism.[22]
2.4.4. PTSD
The PTSD Checklist—Civilian version (PCL-C) was used to identify PTSD and the 1998 Dongting Lake flood was the specified trauma. This instrument is a self-report 17-item questionnaire based on the Diagnostic and Statistical Manual of Mental Disorders-forth edition (DSM-IV) and has been widely used, especially when the structured clinical interview is not feasible.[23] Each of the17 items has a 5-point Likert scale ranging from 1 (not at all) to 5 (extremely). Thus, the total score ranges from 17 to 85. Individuals with a total score of at least 38 are classified as having PTSD.[24,25] The PCL-C is highly internally consistent with Cronbach alpha coefficient equal to 0.94,[26] and the cut-off score of 38 has high levels of sensitivity (94%–97%) and specificity (86%–99%).[27]
2.4.5. Anxiety
The Zung Self-rating Anxiety Scale (SAS), which consists of 20 items, was used to identify anxiety. Each of the 20 items has a 4-point Likert scale ranging from 1 (never) to 4 (very often). Therefore, the total score ranges from 20 to 80. Individuals with a total score of at least 50 are classified as having anxiety.[28,29] This instrument has been widely used in China and has sound reliability and validity.[30]
2.5. Statistical analyses
Frequencies and percentages (%) were presented for categorical variables, whereas means and standard deviations (SDs) were presented for continuous variables. Logistic regression analyses were performed to identify shared risk factors for PTSD only, and comorbidity of PTSD and anxiety. Specifically, univariate logistic regression analyses were used to explore the relationship between each independent variable and PTSD only, and comorbdity of PTSD and anxiety, whereas multivariable logistic regression analyses were used to identify the independent role of each associated variable for PTSD only, and comorbdity of PTSD and anxiety. All statistically significant associated variables in the univariate logistic regression analyses were collectively entered into multivariable logistic regression analyses.[31–33] Participants in neither PTSD nor anxiety group were compared with those in PTSD-only group, and comorbidity of PTSD and anxiety group, respectively. Statistical analyses were conducted using SPSS Version 19.0 (IBM Corp, Armonk, NY). All statistical tests were 2-tailed, and a P value of less than .05 was considered statistically significant.
3. Results
3.1. Sample description
A representative sample consisting of 412 subjects from 204 households of 8 villages in 2 towns of Huarong County were initially yielded for this study. Among the 412 subjects, 364 were interviewed, and 5 of them were excluded for suffering from schizophrenia or mental retardation. Furthermore, since a subgroup of 34 participants were identified as not providing credible information by the subscale lie, a total of 325 respondents were finally enrolled in this study.
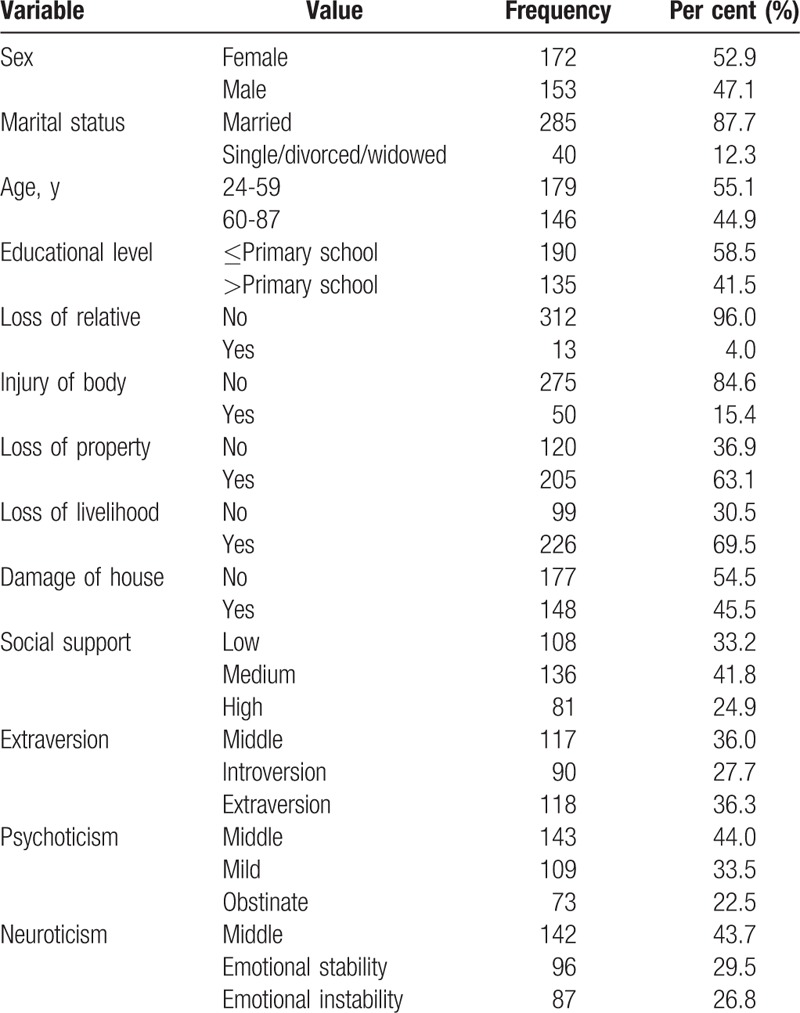
All participants were of Han ethnicity and none of them reported having a family history of psychiatric disorders. Among all participants, 172 (52.9%) were female and the mean (SD) age for the participants was 57.79 (12.26) years. Furthermore, 13 (4.0%) experienced loss of relative, 50 (15.4%) experienced injury of body, 205 (63.1%) experienced loss of property, 226 (69.5%) experienced loss of livelihood, and 148 (45.5%) had their houses damaged due to the 1998 Dongting Lake flood (Table 1).
Table 1.
Characteristics of study sample.
3.2. Prevalence of comorbidity
According to the total scores of PCL-C and SAS, there were 11 participants in PTSD-only group, 10 participants in anxiety-only group, 20 participants in comorbidity of PTSD and anxiety group, and 284 participants in neither PTSD nor anxiety group, indicating that the prevalence of PTSD, anxiety, and comorbidity of PTSD and anxiety was 9.54% (31/325), 9.23% (30/325), and 6.15% (20/325), respectively. Furthermore, 64.52% (20/31) of those with PTSD had anxiety and 66.67% (20/30) of those with anxiety had PTSD.
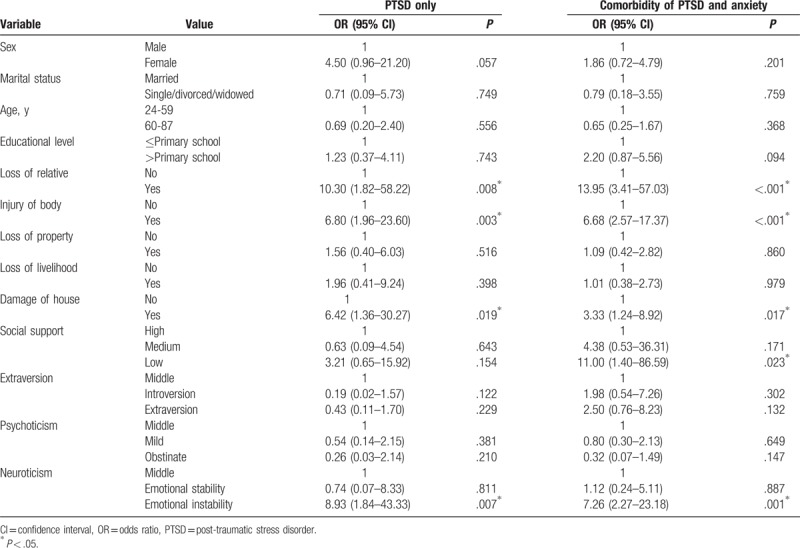
3.3. Univariate analyses
In comparison with neither PTSD nor anxiety group, univariate logistic regression analyses indicated that those with loss of relative (odds ratio [OR] 10.30, 95% confidence interval [CI] 1.82–58.22), injury of body (OR 6.80, 95% CI 1.96–23.60), damage of house (OR 6.42, 95% CI 1.36–30.27), and emotional instability (OR 8.93, 95% CI 1.84–43.33) were more likely to develop PTSD only. Additionally, those with loss of relatives (OR 13.95, 95% CI 3.41–57.03), injury of body (OR 6.68, 95% CI 2.57–17.37), damage of house (OR 3.33, 95% CI 1.24–8.92), low social support (OR 11.00, 95% CI 1.40–86.59), and emotional instability (OR 7.26, 95% CI 2.27–23.18) were more likely to develop comorbidity of PTSD and anxiety (Table 2).
Table 2.
Univariate logistic regression analyses of the effects of possible associated factors on the odds of post-traumatic stress disorder only and comorbidity of post-traumatic stress disorder and anxiety, in comparison with neither post-traumatic stress disorder nor anxiety.
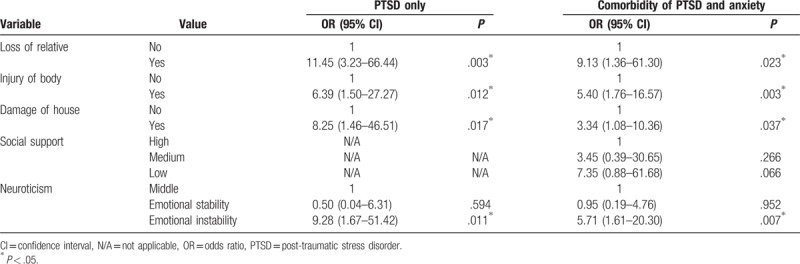
3.4. Multivariable analyses
Multivariable logistic regression analyses indicated that loss of relative (OR 11.45, 95% CI 3.23–66.44 for PTSD only; OR 9.13, 95% CI 1.36–61.30 for comorbidity), injury of body (OR 6.39, 95% CI 1.50–27.27 for PTSD only; OR 5.40, 95% CI 1.76–16.57 for comorbidity), damage of house (OR 8.25, 95% CI 1.46–46.51 for PTSD only; OR 3.34, 95% CI 1.08–10.36 for comorbidity), and emotional instability (OR 9.28, 95% CI 1.67–51.42 for PTSD only; OR 5.71, 95% CI 1.61–20.30 for comorbidity) were shared risk factors for PTSD only, and comorbidity of PTSD and anxiety (Table 3).
Table 3.
Multivariable logistic regression analyses of factors significantly associated with post-traumatic stress disorder only and comorbidity of post-traumatic stress disorder and anxiety in the univariate analyses.
4. Discussion
The present study, conducted 17 years after the Dongting Lake flood in 1998, explored comorbidity of PTSD and anxiety in flood survivors. To the best of our knowledge, this is the first study to explore comorbidity of PTSD and anxiety in flood survivors.
The prevalence of PTSD and anxiety among survivors of the 1998 Dongting Lake flood at 17-year follow-up was 9.54% and 9.23%, respectively. The PTSD prevalence identified in this study is lower than that found among earthquake survivors and war veterans. For example, previous studies indicated that 5 decades after the Korean War, 32.1% of the veterans developed PTSD,[34] and 1 year after the Wenchuan earthquake in China, 26.3% of the survivors developed PTSD.[3] Additionally, the anxiety prevalence identified in this study is lower than that found among former abductees in Northern Uganda.[4] Differences in the prevalence of PTSD and anxiety may be attributed to the differences in the intensity of exposure to the trauma, and also differences in the follow-up time since the trauma emerged.[35,36] For example, Wang et al[37] found that the prevalence of PTSD and anxiety measured 6 weeks after the traffic accidents decreased significantly, compared with that measured 1 week after the traffic accidents.
This study also found that the prevalence of comorbidity of PTSD and anxiety was 6.15%, with 64.52% of those with PTSD having anxiety and 66.67% of those with anxiety having PTSD. Comorbdity of PTSD and anxiety is prevalent in trauma-related populations.[38–40] For example, according to the National Comorbidity Survey in USA, 79% of women and 88% of men with PTSD had at least 1 other psychiatric disorder.[41] These findings indicate that integrated interventions of PTSD and anxiety for trauma-related populations are warranted.
Some studies found that females were at higher risk than males for developing psychiatric disorders including PTSD and anxiety,[9,42] whereas some found contradictory results.[43] Besides, associations between education level and age with psychiatric disorders were controversial.[42,44,45] This study found no association between sociodemographic variables of interest, and comorbidity of PTSD and anxiety. Therefore, more studies with large sample size are warranted to clarify these associations.
Multivariable logistic regression analyses indicated that loss of relative, injury of body, and damage of house were shared risk factors for PTSD only and comorbidity of PTSD and anxiety in flood survivors. This finding is consistent with many previous studies.[3,46] The intensity of exposure to the trauma is among the most robust predictive factors for psychiatric disorders. For example, in comparison with Iranian Chemical Warfare survivors who were only exposed to low-intensity warfare, those who were exposed to both chemical weapons and high-intensity warfare were significantly more likely to suffer from both PTSD and anxiety.[5]
Additionally, emotional instability was a shared risk factor for PTSD only and comorbidity of PTSD and anxiety in flood survivors. Previous studies indicated that neuroticism were associated with many psychiatric disorders, including PTSD and anxiety.[47–49] For example, Spinhoven et al[9] found that neuroticism was a risk factor for comorbidity of PTSD in anxiety and depressive disorders. Besides, though this study did not detect an independent contribution of social support to comorbidity of PTSD and anxiety in flood survivors, social support plays an important role in the incidence and maintenance of psychiatric disorders in trauma-related populations. Social support of this study was measured by SSRS, which only reflects the support from family, friends, or neighbors. Social support from society and community was not measured, which may lead to the insignificant relationship between social support and comorbidity of PTSD and anxiety observed in this study.
When interpreting the findings of this study, it is worth noting here that PTSD identified in this study was related to the 1998 Dongting Lake flood, which was the specified trauma in PCL-C. Though no more floods struck the study area since the Dongting Lake flood in 1998, participants could experience other potential traumas during this period, such as road traffic accidents. Therefore, there might be very low probability that participants may exhibit PTSD symptoms associated with other traumas, which were not measured in this study, and also in many previous studies exploring PTSD related to specified traumas.[50,51] Additionally, participants enrolled in this study were all of Han ethnicity without a family history of psychiatric disorders. Whether findings of this study could be generalized to other populations with different characteristics remains unknown.
This study has several limitations. Firstly, this study was retrospective. Therefore, recall bias might exist when collecting some information, such as the intensity of exposure to the 1998 Dongting Lake flood. However, the finding that the intensity of exposure to the flood was associated with both PTSD only and comorbidity of PTSD and anxiety was consistent with many studies. Secondly, the diagnoses of PTSD and anxiety were made based on self-report questionnaires rather than structured clinical interviews, which could contribute to a higher estimation of the prevalence of comorbidity of PTSD and anxiety. Finally, sparse data bias might exist when identifying the associations of some variables with PTSD only, and comorbidity of PTSD and anxiety, given that their corresponding 95% CIs were wide.
Despite the preceding limitations, this study has quite a few strengths and implications. Firstly, to the best of our knowledge, this is the first study to explore comorbidity of PTSD and anxiety in flood survivors. Therefore, its findings could provide fundamental knowledge for proper interventions in flood survivors. Secondly, the high prevalence of PTSD and anxiety, and also the high prevalence of comorbidity of PTSD and anxiety found in this study, significantly underscores the importance of the implementation of timely and effective interventions for flood survivors. Thirdly, possible associated factors assessed in this study included not only sociodemographic characteristics and the intensity of exposure to the flood, but also personality traits and social support, which may help reduce the effects caused by potential confounding when interpreting the findings. Finally, the finding of this study that the intensity of exposure to the flood and personality traits were shared risk factors for PTSD only and comorbidity of PTSD and anxiety strongly supports the hypothesis that when PTSD and other psychiatric disorders co-occur after the trauma, a combined stress model with a shared vulnerability and similar risk factors might be formed,[52] which may also provide a basis for exploring underlying dimensions of comorbidity involving PTSD.
5. Conclusions
Comorbidity of PTSD and anxiety is prevalent in flood survivors, with its prevalence being 6.15% at 17-year follow-up since the Dongting Lake flood in 1998. Furthermore, the intensity of exposure to the flood (loss of relative, injury of body, damage of house) and emotional instability are shared risk factors for PTSD only and comorbidity of PTSD and anxiety. Integrated intervention strategies of PTSD and anxiety for flood survivors are warranted.
Acknowledgments
The authors are grateful to all participants, investigators, and officials of the local government.
Footnotes
Abbreviations: CI = confidence interval, DSM = Diagnostic and Statistical Manual of Mental Disorders, EPQ-RSC = Eysenck Personality Questionnaire—Revised, Short Scale for Chinese, N/A = not applicable, OR = odds ratio, PCL-C = PTSD Checklist—Civilian Version, PTSD = post-traumatic stress disorder, SAS = Zung Self-rating Anxiety Scale, SD = standard deviation, SSRS = Social Support Rating Scale.
Funding: This study was funded by the Natural Science Foundation of Hunan Province, China (2016JJ2153), the Specialized Research Fund for the Doctoral Program of Higher Education (20130162110054), and the Fundamental Research Funds for the postgraduates of Central South University (2015zzts282).
The authors report no conflicts of interest.
References
- [1].Groome D, Soureti A. Post-traumatic stress disorder and anxiety symptoms in children exposed to the 1999 Greek earthquake. Br J Psychol 2004;95(Pt 3):387–97. [DOI] [PubMed] [Google Scholar]
- [2].Karakaya I, Agaoglu B, Coskun A, et al. The symptoms of PTSD, depression and anxiety in adolescent students three and a half years after the Marmara earthquake. Turk Psikiyatri Derg 2004;15:257–63. [PubMed] [Google Scholar]
- [3].Zhang Z, Shi Z, Wang L, et al. Post-traumatic stress disorder, anxiety and depression among the elderly: a survey of the hard-hit areas a year after the Wenchuan earthquake. Stress Health 2012;28:61–8. [DOI] [PubMed] [Google Scholar]
- [4].Pfeiffer A, Elbert T. PTSD, depression and anxiety among former abductees in Northern Uganda. Conflict Health 2011;5:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Hashemian F, Khoshnood K, Desai MM, et al. Anxiety, depression, and posttraumatic stress in Iranian survivors of chemical warfare. JAMA 2006;296:560–6. [DOI] [PubMed] [Google Scholar]
- [6].Sundquist K, Johansson LM, DeMarinis V, et al. Posttraumatic stress disorder and psychiatric co-morbidity: symptoms in a random sample of female Bosnian refugees. Eur Psychiatry 2005;20:158–64. [DOI] [PubMed] [Google Scholar]
- [7].Mehnert A, Lehmann C, Graefen M, et al. Depression, anxiety, post-traumatic stress disorder and health-related quality of life and its association with social support in ambulatory prostate cancer patients. Eur J Cancer Care 2010;19:736–45. [DOI] [PubMed] [Google Scholar]
- [8].Kimbrel NA, Calhoun PS, Elbogen EB, et al. The factor structure of psychiatric comorbidity among Iraq/Afghanistan-era veterans and its relationship to violence, incarceration, suicide attempts, and suicidality. Psychiatry Res 2014;220:397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Spinhoven P, Penninx BW, van Hemert AM, et al. Comorbidity of PTSD in anxiety and depressive disorders: prevalence and shared risk factors. Child Abuse Neglect 2014;38:1320–30. [DOI] [PubMed] [Google Scholar]
- [10].Vinck P, Pham PN, Stover E, et al. Exposure to war crimes and implications for peace building in northern Uganda. JAMA 2007;298:543–54. [DOI] [PubMed] [Google Scholar]
- [11].Dai W, Kaminga AC, Wu X, et al. Brain-derived neurotropic factor Val66Met polymorphism and posttraumatic stress disorder among survivors of the 1998 Dongting Lake flood in China. BioMed Res Int 2017;2017:4569698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Dai W, Wang J, Kaminga AC, et al. Predictors of recovery from post-traumatic stress disorder after the Dongting Lake flood in China: a 13-14 year follow-up study. BMC Psychiatry 2016;16:382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Dai W, Kaminga AC, Tan H, et al. Long-term psychological outcomes of flood survivors of hard-hit areas of the 1998 Dongting Lake flood in China: prevalence and risk factors. PloS One 2017;12:e0171557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Huang P, Tan H, Liu A, et al. Prediction of posttraumatic stress disorder among adults in flood district. BMC Public Health 2010;10:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Dai W, Chen L, Tan H, et al. Association between social support and recovery from post-traumatic stress disorder after flood: a 13-14 year follow-up study in Hunan, China. BMC Public Health 2016;16:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Wu Z, Xu J, Sui Y. Posttraumatic stress disorder and posttraumatic growth coexistence and the risk factors in Wenchuan earthquake survivors. Psychiatry Res 2016;237:49–54. [DOI] [PubMed] [Google Scholar]
- [17].Wang L, Zhang Y, Wang W, et al. Symptoms of posttraumatic stress disorder among adult survivors three months after the Sichuan earthquake in China. J Trauma Stress 2009;22:444–50. [DOI] [PubMed] [Google Scholar]
- [18].Feng S, Tan H, Benjamin A, et al. Social support and posttraumatic stress disorder among flood victims in Hunan, China. Ann Epidemiol 2007;17:827–33. [DOI] [PubMed] [Google Scholar]
- [19].Xu J, Ou L. Resilience and quality of life among Wenchuan earthquake survivors: the mediating role of social support. Public Health 2014;128:430–7. [DOI] [PubMed] [Google Scholar]
- [20].Liu J, Li F, Lian Y. Investigation of reliability and validity of the social support scale. J Xinjiang Med Univ 2008;31:3. [Google Scholar]
- [21].Cui Y, Tian SS, Qiao N, et al. Associations of individual-related and job-related risk factors with nonfatal occupational injury in the coal workers of Shanxi Province: a cross-sectional study. PloS One 2015;10:e0134367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Qian M, Wu G, Zhu R, et al. Revision for the Eysenck Personality Questionnaire-Revised, Short Scale for Chinese (EPQ-RSC). Acta Psychol Sin 2000;32:323. [Google Scholar]
- [23].Terhakopian A, Sinaii N, Engel CC, et al. Estimating population prevalence of posttraumatic stress disorder: an example using the PTSD checklist. J Trauma Stress 2008;21:290–300. [DOI] [PubMed] [Google Scholar]
- [24].Lang AJ, Laffaye C, Satz LE, et al. Sensitivity and specificity of the PTSD checklist in detecting PTSD in female veterans in primary care. J Trauma Stress 2003;16:257–64. [DOI] [PubMed] [Google Scholar]
- [25].Wen J, Shi YK, Li YP, et al. Quality of life, physical diseases, and psychological impairment among survivors 3 years after Wenchuan earthquake: a population based survey. PloS One 2012;7:e43081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Ruggiero KJ, Del Ben K, Scotti JR, et al. Psychometric properties of the PTSD Checklist-Civilian Version. J Trauma Stress 2003;16:495–502. [DOI] [PubMed] [Google Scholar]
- [27].Blanchard EB, Jones-Alexander J, Buckley TC, et al. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther 1996;34:669–73. [DOI] [PubMed] [Google Scholar]
- [28].Yin W, Pang L, Cao X, et al. Factors associated with depression and anxiety among patients attending community-based methadone maintenance treatment in China. Addiction 2015;110suppl 1:51–60. [DOI] [PubMed] [Google Scholar]
- [29].Hou Y, Li X, Yang L, et al. Factors associated with depression and anxiety in patients with end-stage renal disease receiving maintenance hemodialysis. Int Urol Nephrol 2014;46:1645–9. [DOI] [PubMed] [Google Scholar]
- [30].Zhang Z, Su H, Peng Q, et al. Exam anxiety induces significant blood pressure and heart rate increase in college students. Clin Exp hypertens 2011;33:281–6. [DOI] [PubMed] [Google Scholar]
- [31].Zhang Z, Wang W, Shi Z, et al. Mental health problems among the survivors in the hard-hit areas of the Yushu earthquake. PloS One 2012;7:e46449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Chen G, Shen H, Chen G. A cross-sectional study on posttraumatic stress disorder among elderly Qiang citizens 3 years after the Wenchuan earthquake in China. Can J Psychiatry 2012;57:547–53. [DOI] [PubMed] [Google Scholar]
- [33].Guo L, Deng J, He Y, et al. Alcohol use and alcohol-related problems among adolescents in China: a large-scale cross-sectional study. Medicine 2016;95:e4533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ikin JF, Creamer MC, Sim MR, et al. Comorbidity of PTSD and depression in Korean War veterans: prevalence, predictors, and impairment. J Affect Disord 2010;125:279–86. [DOI] [PubMed] [Google Scholar]
- [35].Ginzburg K, Ein-Dor T, Solomon Z. Comorbidity of posttraumatic stress disorder, anxiety and depression: a 20-year longitudinal study of war veterans. J Affect Disord 2010;123:249–57. [DOI] [PubMed] [Google Scholar]
- [36].Dai W, Chen L, Lai Z, et al. The incidence of post-traumatic stress disorder among survivors after earthquakes: a systematic review and meta-analysis. BMC Psychiatry 2016;16:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Wang CH, Tsay SL, Bond AE. Post-traumatic stress disorder, depression, anxiety and quality of life in patients with traffic-related injuries. J Adv Nurs 2005;52:22–30. [DOI] [PubMed] [Google Scholar]
- [38].Saxe G, Geary M, Bedard K, et al. Separation anxiety as a mediator between acute morphine administration and PTSD symptoms in injured children. Ann N Y Acad Sci 2006;1071:41–5. [DOI] [PubMed] [Google Scholar]
- [39].Hofmann SG, Litz BT, Weathers FW. Social anxiety, depression, and PTSD in Vietnam veterans. J Anxiety Disord 2003;17:573–82. [DOI] [PubMed] [Google Scholar]
- [40].Ikin JF, Sim MR, McKenzie DP, et al. Anxiety, post-traumatic stress disorder and depression in Korean War veterans 50 years after the war. Br J Psychiatry 2007;190:475–83. [DOI] [PubMed] [Google Scholar]
- [41].Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048–60. [DOI] [PubMed] [Google Scholar]
- [42].Zaffina S, Camisa V, Monducci E, et al. PTSD prevalence and associated risk factors after a fire disaster that broke out in a paediatric hospital: a cross-sectional study. Med Lav 2014;105:163–73. [PubMed] [Google Scholar]
- [43].Fu Y, Chen Y, Wang J, et al. Analysis of prevalence of PTSD and its influencing factors among college students after the Wenchuan earthquake. Child Adolesc Psychiatry Ment Health 2013;7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Kolltveit S, Lange N, Thabet II, al, et al. Risk factors for PTSD, anxiety, and depression among adolescents in Gaza. J Trauma Stress 2012;25:164–70. [DOI] [PubMed] [Google Scholar]
- [45].Mak IW, Chu CM, Pan PC, et al. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen Hosp Psychiatry 2010;32:590–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Kashdan TB, Morina N, Priebe S. Post-traumatic stress disorder, social anxiety disorder, and depression in survivors of the Kosovo War: experiential avoidance as a contributor to distress and quality of life. J Anxiety Disord 2009;23:185–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Chen L, Tan H, Cofie R, et al. Prevalence and determinants of chronic post-traumatic stress disorder after floods. Disaster Med Public Health Prep 2015;9:504–8. [DOI] [PubMed] [Google Scholar]
- [48].Jaksic N, Brajkovic L, Ivezic E, et al. The role of personality traits in posttraumatic stress disorder (PTSD). Psychiatr Danub 2012;24:256–66. [PubMed] [Google Scholar]
- [49].Kootker JA, van Mierlo ML, Hendriks JC, et al. Risk factors for symptoms of depression and anxiety one year poststroke: a longitudinal study. Arch Phys Med Rehabil 2016;97:919–28. [DOI] [PubMed] [Google Scholar]
- [50].Cheng Y, Wang F, Wen J, et al. Risk factors of post-traumatic stress disorder (PTSD) after Wenchuan earthquake: a case control study. PloS One 2014;9:e96644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Bowler RM, Kornblith ES, Li J, et al. Police officers who responded to 9/11: comorbidity of PTSD, depression, and anxiety 10-11 years later. Am J Ind Med 2016;59:425–36. [DOI] [PubMed] [Google Scholar]
- [52].Hasanovic M, Pajevic I. Religious moral beliefs as mental health protective factor of war veterans suffering from PTSD, depressiveness, anxiety, tobacco and alcohol abuse in comorbidity. Psychiatr Danub 2010;22:203–10. [PubMed] [Google Scholar]


