Abstract
Rationale:
Anatomical segmentectomy of the pancreatic head along the embryological fusion plane (EFP) has been used in the treatment of benign, borderline, and low-grade malignancy neoplasms. However, few studies have reported on the outcomes of this procedure. The aim of this study was to retrospectively assess the outcomes of anatomical segmentectomy of the pancreatic head along the EFP.
Patient concerns:
We experienced two patients who underwent anatomical segmentectomy of the pancreatic head along the EFP for the treatment of pancreatic cystadenoma. Case 1 was a 69-year-old man presented with upper abdominal pain that had lasted for 3 months. Case 2 was a 52-year-old man presented with upper abdominal pain that had lasted for 1 week.
Diagnosis:
Both patients were diagnosed of pancreatic cystadenoma.
Intervention:
Anatomical segmentectomy of the pancreatic head along the EFP was performed.
Outcomes:
Both patients successfully underwent anatomical segmentectomy of the pancreatic head along the EFP, including ventral segmentectomy and dorsal segmentectomy, and each patient recovered uneventfully. With the inclusion of these 2 cases, there are now a total of 15 cases that have been reported in the literature, including 9 cases of ventral segmentectomy and 6 cases of dorsal segmentectomy. Although pancreatic fistula occurred in 6 of these patients (40%), all of the patients recovered completely without severe complications.
Lessons:
These results suggest that anatomical segmentectomy of the pancreatic head along the EFP is a safe and feasible procedure for cases of benign pancreatic disease confined to the dorsal or ventral segment of the pancreas.
Keywords: embryological fusion plane, pancreas, segmentectomy
1. Introduction
In embryonic development, the head of the pancreas is composed of the dorsal and ventral anlagens. Consequently, the head of the pancreas can theoretically be divided into 2 embryological segments. The embryological fusion plane (EFP) contains few communicating vessels or ducts (except for the junction of the dorsal and ventral duct systems, which is present >90% of the time), thus making segmental pancreatic resection through this plane theoretically feasible.[1,2] Segmentectomy of the pancreatic head along the EFP, that is, dorsal or ventral pancreatectomy, has been reported previously.[3–5] The advantage of this procedure over pancreatoduodenectomy is that the duodenum, bile duct, and pancreatic parenchyma can be largely preserved. Anatomical segmentectomy of the head of the pancreas may thus result in a better quality of life for patients.[6] However, this procedure remains controversial because of the poor demarcation between the 2 segments and the complicated surgical technique that is required. In addition, studies of this technique and its potential outcomes have been limited. In this study, we sought to retrospectively assess the outcomes of anatomical segmentectomy of the pancreatic head along the EFP, and we review the literature on this procedure.
2. Methods
2.1. Patients
Two patients who underwent anatomical segmentectomy of the pancreatic head along the EFP for the treatment of pancreatic cystadenoma were included in this study. This study was approved by our institutional review board (The Affiliated Changzhou No. 2 People's Hospital with Nanjing Medical University). Patients have given fully informed consent.
2.2. Literature review
The PubMed database was searched for studies describing anatomical segmentectomy of the pancreatic head along the EFP, using the keywords “embryological fusion plane” or “dorsal pancreatectomy,” or “ventral pancreatectomy,” and “English language.” Potentially relevant articles were retrieved, and their reference lists were reviewed to identify any missed studies.
3. Results
3.1. Case 1
A 69-year-old man presented with upper abdominal pain that had lasted for 3 months. His past medical history was unremarkable. Evaluation with abdominal magnetic resonance imaging (MRI) (Fig. 1A, B) and contrast-enhanced computed tomography (CT) (Fig. 1C) revealed a well-circumscribed cystic lesion in the ventral pancreas measuring approximately 3.7 × 2.1 cm in diameter. Results of all laboratory tests were normal. On the basis of these imaging and laboratory results, the lesion was diagnosed as a benign cystadenoma. The case was discussed by the institute's tumor board, and ventral segmentectomy was suggested as the most appropriate management option.
Figure 1.
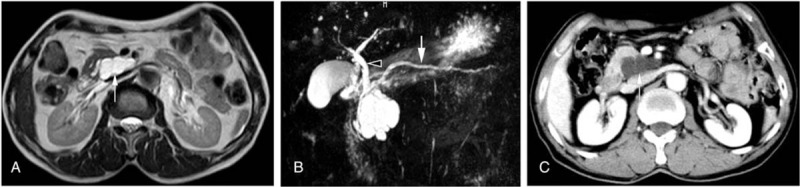
Initial imaging studies of the pancreas demonstrated a well-circumscribed cystic lesion in the ventral pancreas measuring approximately 3.7 × 2.1 cm in diameter. (A) T2-weighted MRI demonstrated a high-signal mass (arrow) in the ventral segment, with a clearly defined border. (B) MR cholangiopancreatography demonstrated a dilated distal pancreatic duct (arrow) and proximal common bile duct (arrowhead) due to local compression by the mass. (C) Contrast-enhanced CT (portal phase) showed a hypodense noninfiltrative lesion (arrow) in the ventral segment.
The patient underwent ventral segmentectomy along the EFP. An exploratory laparotomy via a middle incision was performed with the patient under general anesthesia. The gastrocolic and duodenocolic ligaments were first dissected to expose the pancreatic head, duodenum, and superior mesenteric vein. A limited Kocher maneuver was performed to facilitate slight mobilization of the duodenum and palpation of the intrapancreatic common bile duct (CBD). The posterior aspect of the mesoduodenum was identified and carefully preserved. Palpation and intraoperative ultrasound examination were performed to confirm the presence of a cystic mass in the ventral segment of the pancreas. The inferior pancreatic head was then exposed by careful dissection. A faint line of loose fibrous connective tissues was visible in the inferior pancreatic head (Fig. 2A). This line was identified as the EFP, situated at the interface between the posterior ventral segment and the anterior dorsal segment. This plane, which appeared as a fibrous septum running from the anterior-inferior aspect to the superior-posterior portion of the pancreatic head, was easily dissected without major bleeding, and the ventral and dorsal segments were separated (Fig. 2B). The main pancreatic duct was identified at the left side of the EFP (Fig. 2B), penetrating the fusion plane from the dorsal segment to the ventral segment. This duct was incised and a draining catheter was inserted into the distal duct. The intrapancreatic CBD between the duodenum and ventral pancreas was identified and carefully preserved (Fig. 2C). The proximal pancreatic duct was identified, with this duct running across the ventral segment and flowing into the bile duct (Fig. 2C). The duct was ligated and cut at a distance of 5 mm from the bile duct. Finally, the uncinate process of the pancreas was carefully separated and the entire ventral segment was resected (Fig. 2D). An intraoperative frozen section examination indicated pancreatic ductal mucinous cystadenoma with negative margins of resection. An end-to-side, duct-to-mucosa pancreaticojejunostomy was created using the Roux-en-Y method (Fig. 2E). Histological examination confirmed the presence of pancreatic ductal mucinous cystadenoma (Fig. 2F).
Figure 2.
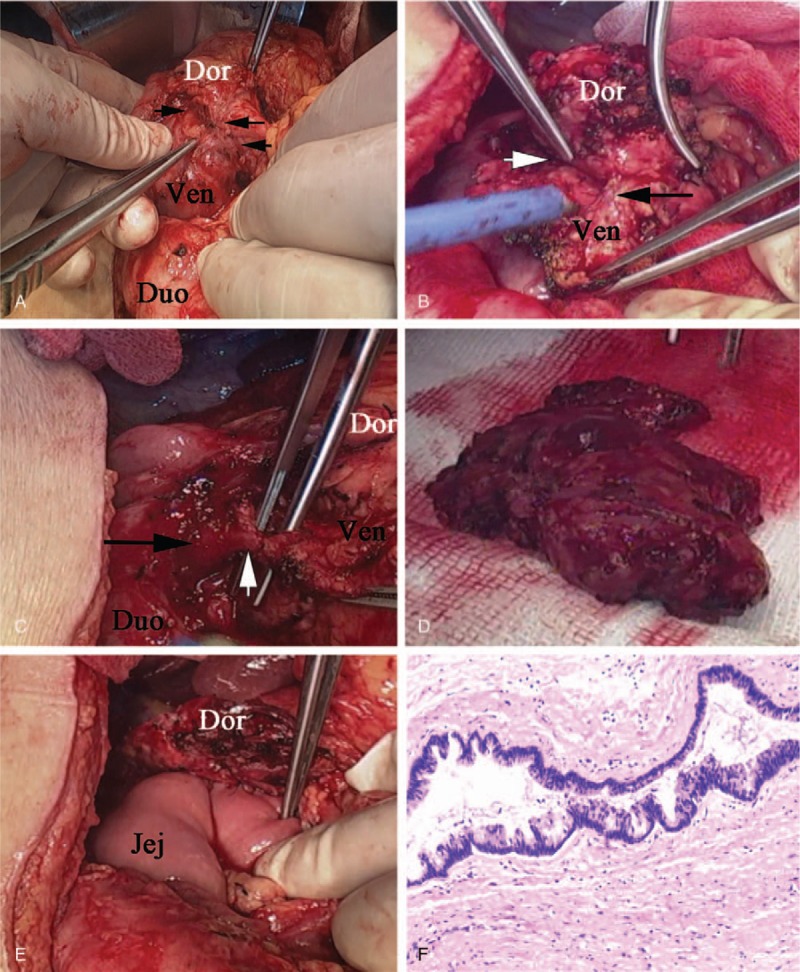
Surgical procedures and pathological examination. (A) The EFP (black arrows) was visible in the inferior pancreatic head between the dorsal and ventral segments. (B) The ventral and dorsal segments were divided along the EFP (white arrow). The main pancreatic duct (black arrow) ran across the EFP. (C) The intrapancreatic CBD (black arrow) ran between the duodenum and the ventral pancreas. The proximal pancreatic duct (white arrow) ran across the ventral segment and flowed into the bile duct. (D) Specimen of the ventral segment. (E) A pancreaticojejunostomy was created using the Roux-en-Y method. (F) Histological examination confirmed the presence of pancreatic ductal mucinous cystadenoma (hematoxylin and eosin, magnification ×100). Dor = dorsal pancreas; Duo = duodenum; Jej = jejunum; Ven = ventral pancreas.
The patient experienced a grade B pancreatic fistula, which healed 20 days after conservative treatment. After 33 months of follow-up, the patient had recovered uneventfully without recurrence of the tumor.
3.2. Case 2
A 52-year-old man presented with upper abdominal pain that had lasted for 1 week. MRI and CT suggested the presence of a gallbladder stone and a cystic tumor in the dorsal pancreas with a dilated pancreatic duct (Fig. 3). Results of laboratory tests were normal. Cholelithiasis and pancreatic head cystadenoma were diagnosed, and cholecystectomy and head dorsal pancreatectomy were suggested for treatment.
Figure 3.
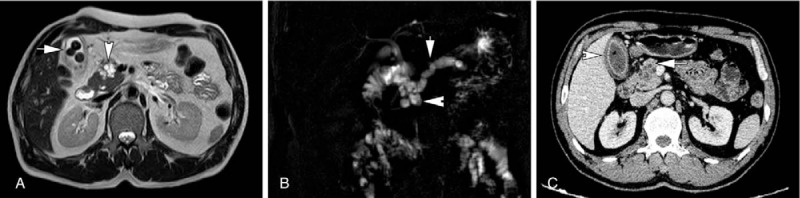
Preoperative imaging studies. (A) T2-weighted MRI demonstrated a high-signal mass (arrowhead) measuring approximately 2.8 × 1.8 cm in diameter in the dorsal segment. Gallbladder stones were also seen (arrow). (B) MR cholangiopancreatography demonstrated the lesion (arrowhead) and the dilated distal pancreatic duct (arrow). (C) Contrast-enhanced CT (portal phase) demonstrated a hypodense noninfiltrative lesion (arrow) in the dorsal segment and inflammatory gallbladder (arrowhead).
The procedures used to expose the pancreatic head were the same as those described in the previous case. Palpation and intraoperative ultrasound examination were performed to confirm the presence of a cystic mass in the dorsal segment of the pancreatic head. The EFP appeared as a faint line of loose fibrous connective tissue in the inferior pancreatic head (Fig. 4A). Dissection along the EFP was performed easily, with no major vessels to avoid, and the ventral and dorsal segments were divided (Fig. 4B). The main pancreatic duct was identified; this duct ran across the EFP from the dorsal segment to the ventral segment (Fig. 4B). The duct was ligated and cut off near the dorsal segment. Cholecystectomy was performed, and a catheter was inserted into the CBD via the cystic duct to help identify and preserve the intrapancreatic CBD. The CBD was located in the ventral segment, with its anterior surface constituting the right portion of the interface between the ventral segment and the dorsal segment. Dissection of the dorsal parenchyma was performed along the anterior surface of the intrapancreatic CBD.
Figure 4.
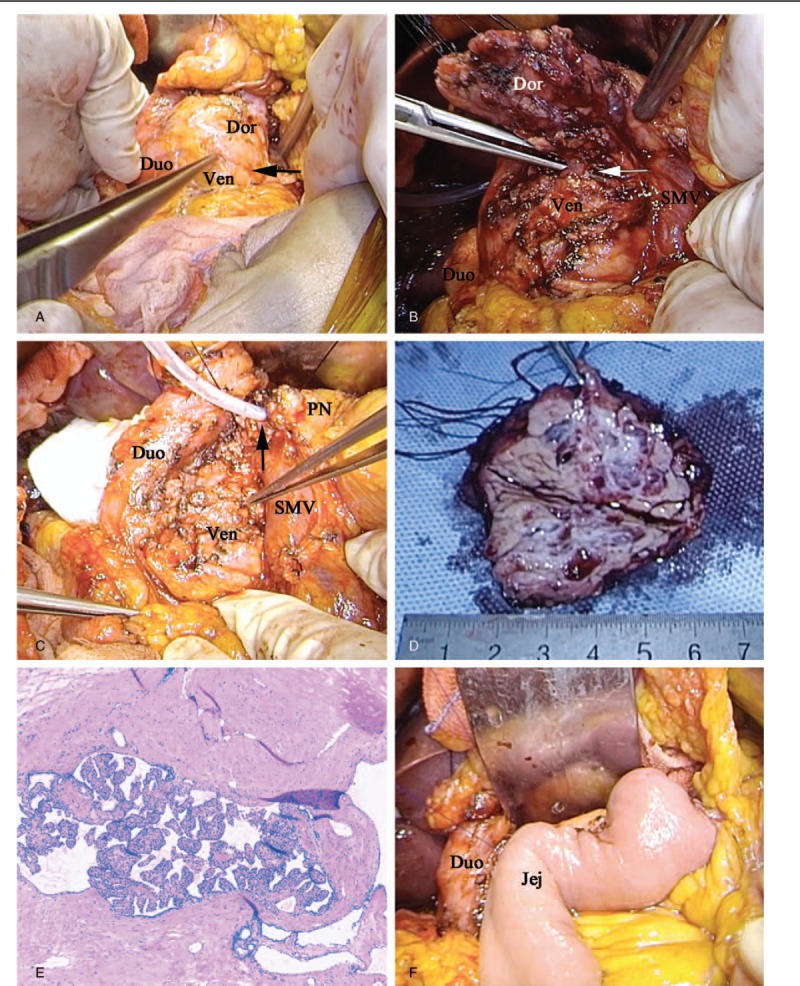
Surgical procedures and pathological examination of the specimen. (A) The EFP (black arrow) was identified in the inferior pancreatic head. (B) The ventral and dorsal segments were divided along the EFP. The main pancreatic duct (white arrow) was identified, ligated, and cut off near the dorsal segment. (C) The dorsal pancreatic head was resected and removed. The dilated distal main pancreatic duct was carefully isolated and intubated (black arrow). (D) Specimen of the head dorsal segment. (E) Pathological examination confirmed the diagnosis of serous papillary cystadenoma (hematoxylin and eosin, magnification ×100). (F) A pancreaticojejunostomy was created using the Roux-en-Y method. Dor = dorsal pancreas; Duo = duodenum; Jej = jejunum; PN = pancreas; SMV = superior mesenteric vein; Ven = ventral pancreas.
The anterior superior pancreaticoduodenal artery was identified near the upper edge of the pancreatic head, and the collateral branches to the pancreas were carefully ligated. To insure the maintenance of blood supply to the duodenum and the remaining ventral pancreas, the posterior superior pancreaticoduodenal artery was preserved. The pancreatic neck was dissected and transected, and the dilated distal main pancreatic duct was carefully isolated and intubated (Fig. 4C). The head dorsal segment was totally divided and removed (Fig. 4D). An intraoperative pathological examination confirmed the diagnosis of serous papillary cystadenoma with negative margins (Fig. 4E). An end-to-side, duct-to-mucosa pancreaticojejunostomy was created using the Roux-en-Y method (Fig. 4F).
The patient experienced a grade B pancreatic fistula, which healed 25 days after conservative treatment. After 24 months of follow-up, there was no evidence of tumor recurrence.
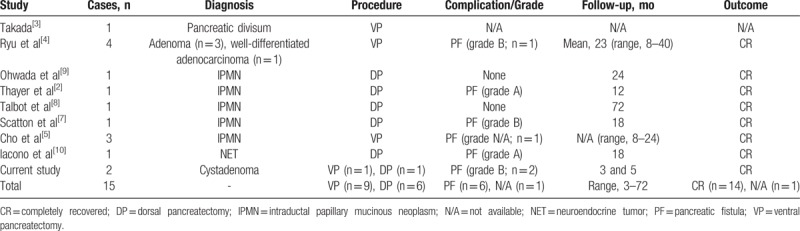
Only 15 cases of anatomical segmentectomy of the pancreatic head along the EFP have previously been reported in the literature (Table 1).[2–5,7–10]
Table 1.
Summary of patients who have undergone anatomical segmentectomy of the head of the pancreas.
4. Discussion
The pancreas is composed of 2 segments: the dorsal pancreas, which includes the pancreatic neck, body, and tail, as well as the anterior segment of the head, and the ventral pancreas, which includes most of the uncinate process and the posterior segment of the head. Research has suggested that segmental pancreatic resection along the EFP, which persists in the adult pancreas, may preserve functioning pancreatic tissue; this technique may prevent diabetes and obviate the potential risks of biliary and gastrointestinal reconstruction.[1,7,8,11]
In the 2 cases reported here, we successfully performed dorsal and ventral pancreatectomies in patients with cystadenoma. In these cases, noncommunication of the dorsal and ventral duct elements made it easier and oncologically rational to eliminate the entire neoplasm via a novel strategy that preserved the ventral or dorsal segment. This anatomical segmentectomy of the pancreatic head along the EFP is an anatomical resection that is reserved for benign, borderline, and low-grade malignant pancreatic tumors and represents an alternative to pancreaticoduodenectomy. In selected cases, this technique enables the complete removal of the pancreatic mass while avoiding biliary and gastroduodenal resection and reconstruction with the preservation of endocrine and exocrine functions.[2,7–9]
Only 15 cases of anatomical segmentectomy of the pancreatic head along the EFP have previously been reported in the literature (Table 1).[2–5,7–10] Dorsal pancreatectomy was performed for the first time in 2001 by Ohwada et al,[9] with other researchers subsequently reporting similar procedures.[2,8,10,12] Ventral pancreatectomy was performed for the first time in 1993 by Takada.[3] These studies demonstrated that anatomical segmentectomy of the pancreatic head along the EFP is technically and clinically feasible, with the advantage of preserving the duodenum, the CBD, and the papilla of Vater.[1]
Despite anatomic evidence that the dorsal and ventral duct systems apparently have few communications, fistula of pancreatic secretions from the dissected surface of the residual parenchyma can occur. In the cases reported here, postoperative pancreatic fistulas did occur, but each was of low volume and healed within a short period. Of the cases summarized in Table 1, 40% had pancreatic fistulas; however, all of the fistulas were classified as grade A or B, and all patients completely recovered without severe complications.
In conclusion, anatomical segmentectomy of the pancreatic head along the EFP is a feasible option for patients with pancreatic disease. In cases of benign disease confined to the dorsal or ventral segment of the pancreas, this technique should be considered.
Acknowledgment
We thank Megan Griffiths, Scientific Writer, Cleveland, OH, for her help with revising the manuscript.
Author contributions
Xihu Qin: Concept and design of study, data collection, data interpretation and analysis, drafting, revision, approval of final manuscript.
Chunfu Zhu and Zhongzhi Jia: data collection and revision.
Xudong Zhang and Qiang Yu: data collection.
Writing – original draft: Chunfu Zhu, Zhongzhi Jia, Qiang Yu, Xihu Qin.
Data curation: Xudong Zhang.
Conceptualization: Xihu Qin.
Footnotes
Abbreviations: CBD = common bile duct, CT = computed tomography, EFP = embryological fusion plane, MRI = magnetic resonance imaging.
Both CZ and ZJ contributed equally to this study.
Funding/support: This study was supported by the Social Development Foundation of Science and Technology of Jiangsu (BE2016658), and the Changzhou Sci&Tech Program (No. CE20165020). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no financial, consultative, institutional, and other relationships that might lead to bias or conflict of interest.
References
- [1].Sakamoto Y, Nagai M, Tanaka N, et al. Anatomical segmentectomy of the head of the pancreas along the embryological fusion plane: a feasible procedure? Surgery 2000;128:822–31. [DOI] [PubMed] [Google Scholar]
- [2].Thayer SP, Fernández-del Castillo C, Balcom JH, et al. Complete dorsal pancreatectomy with preservation of the ventral pancreas: a new surgical technique. Surgery 2002;131:577–80. [DOI] [PubMed] [Google Scholar]
- [3].Takada T. Ventral pancreatectomy: resection of the ventral segment of the pancreas. J Hep Bil Pancr Surg 1993;1:36–40. [Google Scholar]
- [4].Ryu M, Takayama W, Watanabe K, et al. Ventral pancreatic resection for adenoma and low-grade malignancies of the head of the pancreas. Surg Today 1996;26:476–81. [DOI] [PubMed] [Google Scholar]
- [5].Cho A, Arita S, Koike N, et al. Ventral pancreatectomy associated with segmental duodenectomy including the major papilla. Hepatogastroenterology 2007;54:2392–4. [PubMed] [Google Scholar]
- [6].Warshaw AL, Rattner DW, Fernández-del Castillo C, et al. Middle segment pancreatectomy: a novel technique for conserving pancreatic tissue. Arch Surg 1998;133:327–31. [DOI] [PubMed] [Google Scholar]
- [7].Scatton O, Sauvanet A, Cazals-Hatem D, et al. Dorsal pancreatectomy: an embryology-based resection. J Gastrointest Surg 2006;10:434–8. [DOI] [PubMed] [Google Scholar]
- [8].Talbot ML, Foulis AK, Imrie CW. Total dorsal pancreatectomy for intraductal papillary mucinous neoplasm in a patient with pancreas divisum. Pancreatology 2005;5:285–8. [DOI] [PubMed] [Google Scholar]
- [9].Ohwada S, Ogawa T, Kasahara M, et al. Ventral pancreas-preserving pancreatic head and body resection. Hepatogastroenterology 2001;48:1622–4. [PubMed] [Google Scholar]
- [10].Iacono C, Ruzzenente A, Conci S, et al. Head dorsal pancreatectomy: an alternative to the pancreaticoduodenectomy for not enucleable benign or low-grade malignant lesions. Pancreatology 2014;14:419–24. [DOI] [PubMed] [Google Scholar]
- [11].Uchida T, Takada T, Ammori BJ, et al. Three-dimensional reconstruction of the ventral and dorsal pancreas: a new insight into anatomy and embryonic development. J Hepatobiliary Pancreat Surg 1999;6:176–80. [DOI] [PubMed] [Google Scholar]
- [12].Sakamoto Y, Tanaka N, Nagai M, et al. Anterior segmentectomy of the pancreatic head for islet cell tumors. Pancreas 2002;24:317–9. [DOI] [PubMed] [Google Scholar]


