Abstract
Rationale:
In the past decade, epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) treatment had been an important therapy for treating advanced EGFR-mutated lung cancer patients. However, a large number of these patients with EGFR-TKIs treatment always acquired resistance to these drugs in one year. The histologic transformation is an important resistance mechanism.
Patient concerns:
Here we reported a 41-year-old man with EGFR-mutated lung adenocarcinoma and he showed histologic transformation to both small-cell lung cancer (SCLC) and squamous cell carcinoma (SCC) after treatment of gefitinib.
Diagnoses:
A case of EGFR-mutated lung cancer.
Interventions:
Medical thoracoscopy examination was performed and the patient was diagnosed as a EGFR-mutated lung adenocarcinoma. Then gefitinib was administered orally at a dose of 250 mg daily. The patient received treatment with chemotherapy (etoposide 0.1 g day 2-5 + cis-platinum 30 mg day 2-4) after acquiring resistance to gefitinib.
Outcomes:
The patient died in April 2017 that survived for 32 months from lung cancer was found for the first time.
Lessons:
To the best of our knowledge, it is the first case of EGFR-mutated lung adenocarcinoma transforming to both SCLC and SCC which was treated with and responded to gefitinib.
Keywords: adenocarcinoma, EGFR, histologic transformation, small-cell lung cancer, squamous cell carcinoma
1. Introduction
Cancers are the leading causes of death worldwide, over 20% of these dead people are related to lung cancer.[1] In the past decade, epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) treatment had been an important therapy for treating advanced lung cancer patients. However, a large number of these patients with EGFR-TKIs treatment always acquired resistance to these drugs in 1 year.[2–4] The histologic transformation is an important resistance mechanism.[5–7] Some cases have been reported that lung adenocarcinoma could transform into small cell lung cancer or squamous cell carcinoma after treatment of EGFR-TKIs.[6–9] As far as we know, there is no report mentioning that lung adenocarcinoma transforms into both small-cell lung cancer (SCLC) and squamous cell carcinoma (SCC) in a same patient.
Here we report a case of EGFR-mutated lung adenocarcinoma that showed histologic transformation to both SCLC and SCC after treatment of gefitinib.
2. Case report
In August 2014, a 41-year-old male smoker was admitted to our hospital because of right pleural effusion. After obtaining the patient's informed consent, medical thoracoscopy examination was performed and many parietal pleural nodules were found in right lung. Histopathologic examination showed low differentiated adenocarcinomas in parietal pleural nodules which considered to be metastases rather than the primary tumor (Fig. 1). Molecular testing using FISH was carried out on these parietal pleural nodules and found to be EGFR positive (exon 19 deletion). Considering the cancer was EGFR mutated, the patient began to receive treatment with 250 mg gefitinib daily since August 2014. The treatment was well tolerated and the chest computed tomography scan revealed a good response that the size of lesions in right upper lobe became smaller.
Figure 1.
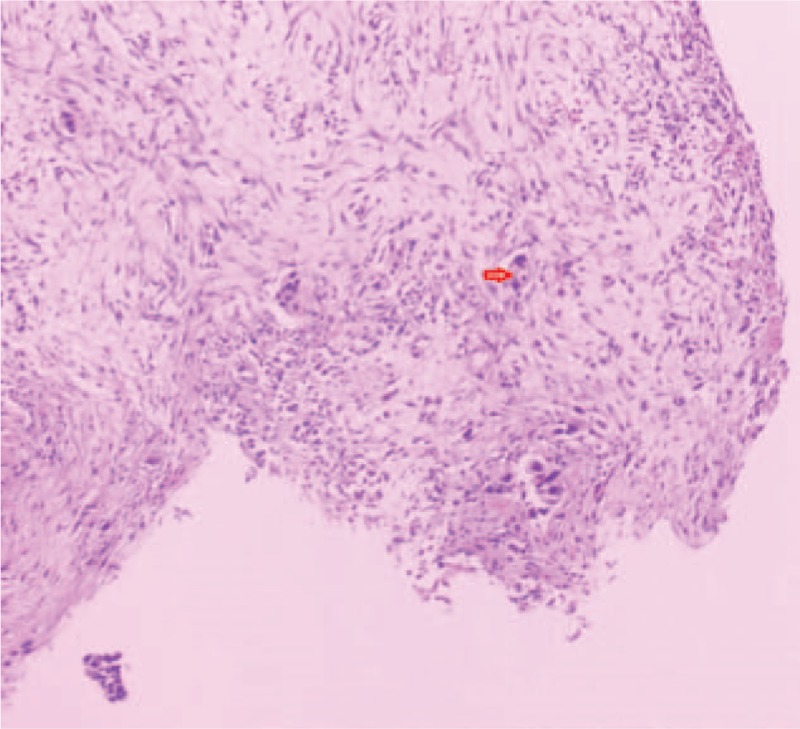
Histopathologic examination of parietal pleural nodules showed low differentiated adenocarcinoma.
Unfortunately, the chest computed tomography in November 2015 revealed the lesions in right lung became larger and new lesions were found in the left lung. Without the doctor's advice, the patient tried Tarceva, Sorafenib, BIBW2992, AZD9291, XL184, and Crizotinib successively. However, there was no obvious curative effect and the tumor gained progress. In February 2017, the patient was admitted to our hospital again. Positron emission tomography-computed tomography revealed that a mass in the right hilus pulmonis and multiple nodules in the bilateral lungs with high glycometabolism, which were considered to be primary cancer or metastases. After obtaining the patient's informed consent, a lung puncture biopsy under computed tomography guidance of the right lung mass was performed. Histopathologic examination showed small cell lung cancer (Fig. 2) and the patient began to receive treatment with chemotherapy (etoposide 0.1 g day2–5 + cis-platinum 30 mg day2–4). Unfortunately, the chemotherapy treatment did not work and the right lung mass became larger. In order to get the latest pathology, a bronchoscopy was performed after obtaining the patient's informed consent. Interestingly, histopathologic examination showed squamous cell carcinoma (Fig. 3). The patient died in April 2017 that survived for 32 months from lung cancer was found for the first time.
Figure 2.
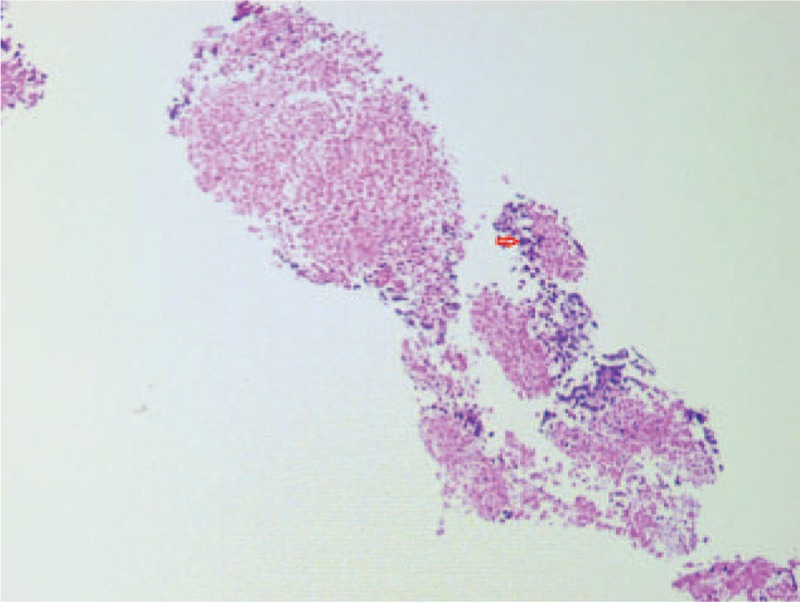
Histopathologic examination of right lung puncture biopsy specimens showed small cell lung cancer.
Figure 3.
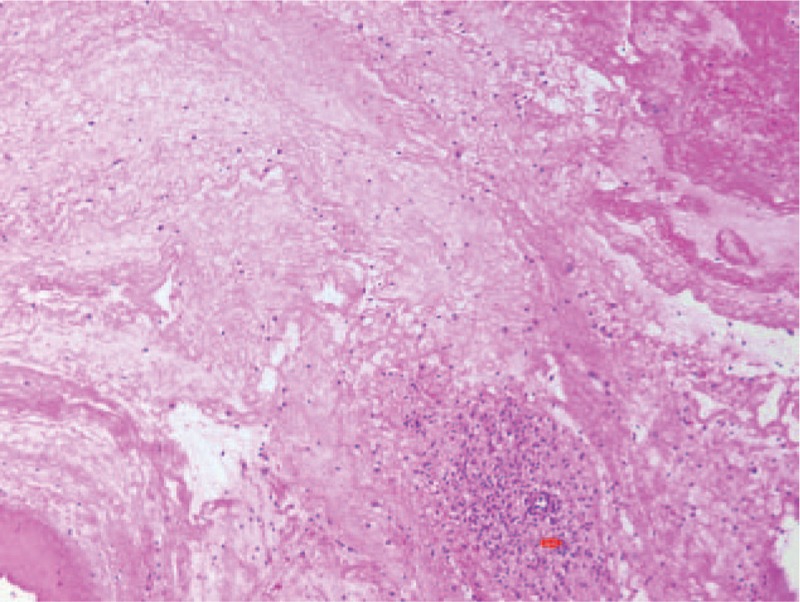
Histopathologic examination of the right main bronchus showed squamous cell carcinoma.
3. Discussion
Lung cancers harboring EGFR mutations respond to EGFR-TKIs. But patients with EGFR-TKIs treatment always acquired drug assistance in 1 year. To date, a variety of acquired resistance mechanisms have been reported, including secondary EGFR resistance mutations (T790M), MET amplification, histologic transformation to SCLC and so on.[3] In some reports, histologic transformation from adenocarcinoma to SCC also had been described as a mechanism of resistance to the EGFR-TKIs, but the mechanism of such histological transformation remains unclear.[3,6–9]
In our case, the patient was found with adenocarcinoma harboring EGFR mutation at first and responded to gefitinib well. However, the patient acquired drug resistance to gefitinib after 11 months of treatment. At last, the histopathologic examination showed the patient had both SCLC and SCC, while adenocarcinoma cell was not found. It was hard to distinguish the changed histopathology was made by the histologic transformation or it existed from the start, though the immunohistochemistry was performed. It is unclear why the histological changed from adenocarcinoma to both SCLC and SCC. It was possible that the tumor was initially a mixed histological type such as adenosquamous carcinoma with SCLC, all types of cells coexisted in the original tumor mass, but only SCC and SCLC remained after the treatment. The second possibility was that the tumor was initially an adenosquamous carcinoma that the adenocarcinoma transformed to SCLC under the pressure of gefitinib treatment. The third possibility was that the tumor was initially a mixed histological type of adenocarcinoma and SCLC that the adenocarcinoma transformed to SCC. Even it was possible that the tumor was initially only adenocarcinoma and transformed to both SCLC and SCC after the treatment.
Disappointingly, the first histopathologic examination specimens were parietal pleural nodules which were considered to be metastases rather than the primary tumor, which means it was hard to confirm which of the above conjectures was right. We also acknowledge that it is hard to rule out the possibility that whether the post-gefitinib treatment patient tried without the doctor's advice made a difference in histologic transformation or pathological selection.
4. Conclusion
To the best of our knowledge, it is the first case of EGFR-mutated lung adenocarcinoma transforming to both SCLC and SCC which was treated with and responded to gefitinib. The patient did not receive effective treatment after gefitinib resistance occurred. To help establish the best treatment for these patients, further studies are in need.
Author contributions
Writing – original draft: Yufeng Yao, Zhouyu Zhu, Yimin Wu.
Writing – review & editing: Zhouyu Zhu, Ying Chai.
Footnotes
Abbreviations: EGFR = epidermal growth factor receptor, SCC = squamous cell carcinoma, SCLC = small-cell lung cancer, TKI = tyrosine kinase inhibitors.
YY and ZZ contributed equally to this work.
Ethics approval and consent to participate: The Review Board of the Second Affiliated Hospital of Zhejiang University School of Medicine approved this retrospective study and waived written informed consent. And written informed consent was obtained from the patient to participate to this case report and any accompanying images.
The authors have no conflicts of interest to disclose.
References
- [1].Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67:30. [DOI] [PubMed] [Google Scholar]
- [2].Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 2010;362:2380–8. [DOI] [PubMed] [Google Scholar]
- [3].Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med 2011;3: 75ra26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sequist LV, Yang JC-H, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327–34. [DOI] [PubMed] [Google Scholar]
- [5].Mok TS, Wu Y-L, Ahn M-J, et al. Osimertinib or platinumepemetrexed in EGFR T790Mepositive lung cancer. N Engl J Med 2017;376:629–40.27959700 [Google Scholar]
- [6].Hsieh MS, Jhuang JY, Hua SF, et al. Histologic evolution from adenocarcinoma to squamous cell carcinoma after gefitinib treatment. Ann Thorac Surg 2015;99:316–9. [DOI] [PubMed] [Google Scholar]
- [7].Kuiper JL, Ronden MI, Becker A, et al. Transformation to a squamous cell carcinoma phenotype of an EGFR-mutated NSCLC patient after treatment with an EGFR tyrosine kinase inhibitor. J Clin Pathol 2015;68:320–1. [DOI] [PubMed] [Google Scholar]
- [8].Haratani K, Hayashi H, Watanabe S, et al. Two cases of EGFR mutation-positive lung adenocarcinoma that transformed into squamous cell carcinoma: successful treatment of one case with rociletinib. Ann Oncol 2016;27:200–2. [DOI] [PubMed] [Google Scholar]
- [9].Hiroki Izumi, Akira Yamasaki, Yasuto Ueda, et al. Squamous Cell Carcinoma Transformation from EGFR-mutated Lung Adenocarcinoma: A Case Report and Literature Review. Clin Lung Cancer 2018;19:e63–6. [DOI] [PubMed] [Google Scholar]


