Abstract
Background
Microinvasive breast cancer is an uncommon pathological entity. Owing to the rarity of this condition, its surgical axillary management and overall prognosis remain controversial.
Methods
A database was analysed to identify patients with microinvasive ductal carcinoma in situ (DCIS) who had surgery for invasive breast cancer at the European Institute of Oncology, Milan, between 1998 and 2010. Women who had undergone axillary staging by sentinel lymph node biopsy were included in the study.
Results
Of 257 women with microinvasive breast cancer who underwent sentinel lymph node biopsy (SLNB), 226 (87·9 per cent) had negative sentinel lymph nodes (SLNs) and 31 had metastatic SLNs. Twelve patients had isolated tumour cells (ITCs), 14 had micrometastases and five had macrometastases in sentinel nodes. Axillary lymph node dissection was performed in 16 of the 31 patients with positive SLNs. After a median follow-up of 11 years, only one regional first event was observed in the 15 patients with positive SLNs who did not undergo axillary lymph node dissection. There were no regional first events in the 16 patients with positive SLNs who had axillary dissection.
Conclusion
Good disease-free and overall survival were found in women with positive SLNs and microinvasive DCIS. This study is in line with studies showing that SLNB in microinvasive DCIS may not be useful, and supports the evidence that less surgery can provide the same level of overall survival with better quality of life.
No added value
Introduction
Microinvasive breast cancer is an uncommon pathological entity, accounting for approximately 1 per cent of all breast cancers1,2. The definition of microinvasive breast cancer has varied over time3,4.
Recently, the definition of microinvasion, as given by the seventh edition of the AJCC staging manual5, of extension of cancer cells beyond the basement membrane into the adjacent tissue with no focus more than 1 mm in greatest dimension, has gained common acceptance. As a result, the term ‘T1mic’ has now been added to the TNM staging system5,6.
Owing to the rarity of this condition, questions remain regarding the surgical management of the axilla and the overall prognosis of this entity. In the literature, a large incidence spectrum of axillary metastasis is found. This can be attributable to differing definitions of microinvasive ductal carcinoma in situ (DCIS) over the years and to the varying techniques used to analyse the sentinel node. These differences are probably responsible for the different recommendations on how to manage the axilla in microinvasive DCIS7.
DCIS is a disease devoid of invasive behaviour and thus without potential for spread to the axillary lymph nodes. Current practice is to perform sentinel lymph node biopsy (SLNB) only in selected patients with DCIS when there is substantial risk of upgrade of the lesion at final pathology, such as a mass lesion highly suggestive of invasive cancer at imaging and physical examination, patients with a large area of DCIS at imaging (5 cm or greater), or when mastectomy is indicated8. However, evidence for this recommendation is inadequate because of the sparsity of data analysed in the literature, also characterized by a lack of long-term follow-up studies and still subject to controversial scientific analysis9.
If staging the axilla in DCIS is accepted globally in the above conditions, what remains controversial is the real value of staging the axilla with SLNB in microinvasive DCIS4,6–7,10–31, as reviewed in Table 14,6–7,10–24,27–31. The incidence of axillary metastasis in sentinel nodes varies in studies from approximately 2 to 20 per cent. This is probably due to the different pathological methods used to examine the sentinel node, as well as differences in the methodology used to section the breast tissue. Factors correlated with axillary nodal positivity in women with DCIS and microinvasive DCIS are younger age, size of DCIS lesion, histological grade, receptor status, human epidermal growth factor receptor (HER) 2 overexpression and lymphovascular invasion6,23,25.
Table 1.
Literature review of selected studies of microinvasive ductal carcinoma in situ in patients who had sentinel lymph node biopsy
| Reference | Year | Total no. of patients with axillary staging | Patients submitted to SLNB | Type of metastasis (AJCC criteria) | SLNB positivity (%) | ||
|---|---|---|---|---|---|---|---|
| ITCs | Micro | Macro | |||||
| Without defined SLNB status | |||||||
| Cox et al.11 | 2001 | 15 | 15 | n.s. | n.s. | n.s. | 3 (20) |
| Camp et al.10 | 2005 | 13 | 13 | n.s. | n.s. | n.s. | 2 (15) |
| Wilkie et al.29 | 2005 | 51 | 51 | 5 | n.s. | n.s. | 7 (14) |
| Tunon-de-Lara et al.28 | 2008 | 45 | 45 | 0 | n.s. | n.s. | 2 (4) |
| Fortunato et al.12 | 2008 | 77 | 77 | n.s. | n.s. | n.s. | 6 (8) |
| Vieira et al.6 | 2010 | 17 | 14 | n.s. | n.s. | n.s. | 1 (6) |
| Parikh et al24 | 2012 | 46 | 4 | n.s. | n.s. | n.s. | 1 (2) |
| With defined SLNB status | |||||||
| Zavotsky et al.31 | 1999 | 14 | 14 | 1 | 0 | 1 | 2 (14) |
| Klauber-DeMore et al.19 | 2000 | 31 | 31 | 0 | 2 | 1 | 3 (10) |
| Intra et al.16 | 2003 | 41 | 41 | 0 | 2 | 2 | 4 (10) |
| Katz et al.18 | 2006 | 21 | 21 | 0 | 1 | 1 | 2(10) |
| Leidenius et al.21 | 2006 | 11 | 11 | 1 | 0 | 0 | 1 (9) |
| Zavagno et al.30 | 2007 | 43 | 43 | 0 | 1 | 3 | 4 (9) |
| Gray et al.13 | 2007 | 79 | 77 | 2 | 2 | 2 | 6 (8) |
| Guth et al.14 | 2008 | 44 | 20 | 2 | 0 | 3 | 5 (11) |
| Sakr et al.27 | 2008 | 20 | 20 | 0 | 2 | 0 | 2 (10) |
| Lyons et al.7 | 2012 | 112 | 112 | 6 | 5 | 3 | 14 (12·5) |
| Ko et al.20 | 2012 | 293 | 180 | 6 | 12 | 4 | 22 (7·5) |
| Kapoor et al.17 | 2013 | 45 | 31 | 4 | 4 | 1 | 9 (20) |
| Margalit et al.22 | 2013 | 68 | 53 | 4 | 3 | 0 | 7 (10) |
| Matsen et al.23 | 2014 | 414 | 414 | 0 | 26 | 6 | 32 (7·7) |
| Hanna et al.15 | 2014 | 81 | 64 | 2 | 0 | 0 | 2 (2) |
| Orzalesi et al.4 | 2016 | 126 | 126 | 10 | 3 | 5 | 18 (14·3) |
Values in parentheses are percentages. SLNB, sentinel lymph node biopsy; ITC, isolated tumour cell; micro, micrometastases; macro, macrometastases; n.s., not stated.
To contribute to a better understanding of this surgical aspect, as well as to the prognostic implications of microinvasion, this retrospective observational study examined patients with microinvasive breast cancer who underwent axillary staging via SLNB.
Methods
After institutional review board approval, a database of patients who underwent surgery for invasive breast cancer at the European Institute of Oncology, Milan, Italy, between 1998 and 2010 was analysed, and patients with microinvasive DCIS were identified. Patients who did not undergo axillary surgery were excluded, and the remaining patients with microinvasive breast cancer who had undergone axillary staging by SLNB were included in the analysis.
Sentinel lymph node (SLN) identification was usually performed using a radiocolloid technique (99mTc-labelled colloidal particles of human albumin). Intraoperative lymph node analysis was conducted using haematoxylin and eosin-stained sections, aided by immunohistochemical staining when necessary, as has been reported previously32.
Based on AJCC classification criteria5, axillary lymph node metastases were defined as follows: macrometastases (larger than 2·0 mm), micrometastases (0·2–2·0 mm) or isolated tumour cells (ITCs) (smaller than 0·2 mm). Systemic adjuvant therapy was recommended according to the contemporary St Gallen treatment guidelines33–37.
The following parameters were used in the analysis: clinical (year of surgery, age, menopausal status), pathology (tumour histology, tumour grade, tumour subtype) and type of treatment (local or systemic). Long-term outcomes were studied via follow-up data recording the first recurrence events, classified as local (ipsilateral breast and chest), regional (ipsilateral axillary or supraclavicular lymph nodes), distant metastasis, contralateral breast cancer, other primary tumour and death as the first-reported event.
Statistical analysis
Demographic and clinical characteristics of the study sample were analysed using descriptive statistics. The association between SLN status, and demographic and clinical variables was evaluated using the χ2 test. Cumulative incidences of the first observed relapse (categorized as local recurrence, regional recurrence or distant metastasis) were assessed from the date of surgery to the date of event. In case of no event, the observation was censored at the last follow-up visit. Cumulative incidence functions were estimated according to the method described by Kalbfleisch and Prentice38, taking into account the competing causes of relapse. Gray's test39 was used to assess cumulative incidence differences between groups.
Overall survival (OS) was defined as the time from date of surgery to date of death from any cause; disease-free survival (DFS) was defined, according to standardized definitions for efficacy end points (STEEP) criteria40, as the time from surgery to events such as relapse (including ipsilateral breast tumour recurrence), appearance of a second primary cancer (including contralateral breast cancer) or death, whichever occurred first. OS and DFS curves were estimated using the Kaplan–Meier method, and the log rank test was used to assess differences between groups.
Median follow-up was calculated using the reverse Kaplan–Meier method41. All analyses were performed using SAS® software version 9.4 (SAS Institute, Cary, North Carolina, USA). All statistical tests were two-sided.
Results
Of 22 120 patients in the database, 310 with microinvasive DCIS were identified. Fifty-three were excluded as they did not undergo axillary surgery, and the remaining 257 patients (82·9 per cent) with microinvasive breast cancer who had axillary staging by SLNB were included in the analysis. Of these 257 women, 161 (62·6 per cent) had only one SLN, 57 (22·2 per cent) had two SLNs, 26 (10·1 per cent) had three SLNs and 13 patients (5·1 per cent) had more than three SLNs removed.
Sentinel node metastasis and tumour characteristics
Negative SLNs were found in 226 of the 257 women (87·9 per cent). In one of these 226 patients, axillary dissection was performed owing to micrometastasis in an additional level 1 lymph node removed at the time when this still was an institutional criterion for axillary dissection. A total of 31 women presented with metastatic SLNs: 12 with ITCs, 14 with micrometastases and five with macrometastases. Thus, the overall rate of metastasis in the SLN was 12·1 per cent (31 of 257), with macrometastasis in 1·9 per cent, micrometastasis in 5·4 per cent and ITCs in 4·7 per cent (Table S1, supporting information). All patients with metastatic SLNs had ductal histology of the breast cancer. A higher proportion with positive SLNs were found in luminal B (31 per cent) and triple-negative (21 per cent) subtypes compared with other subtypes (Table 2).
Table 2.
Patient characteristics according to sentinel lymph node status
| SLN status* | All patients (n = 257)† | |||
|---|---|---|---|---|
| Negative (n = 226) | Positive (n = 31) | P | ||
| Year of surgery | 0·915 | |||
| Before 2003 | 42 (89) | 5 (11) | 47 (18·3) | |
| 2003–2006 | 111 (88·1) | 15 (11·9) | 126 (49·0) | |
| 2007–2010 | 73 (87) | 11 (13) | 84 (32·7) | |
| Age (years) | 0·079 | |||
| < 50 | 91 (82·7) | 19 (17·3) | 110 (42·8) | |
| 50–59 | 69 (91) | 7 (9) | 76 (29·6) | |
| ≥ 60 | 66 (93) | 5 (7) | 71 (27·6) | |
| Menopausal status | 0·030 | |||
| Premenopausal | 99 (83·2) | 20 (16·8) | 119 (46·3) | |
| Postmenopausal | 127 (92·0) | 11 (8·0) | 138 (53·7) | |
| Histology | 0·177 | |||
| Ductal | 203 (86·8) | 31 (13·2) | 234 (91·1) | |
| Lobular | 8 (100) | 0 (0) | 8 (3·1) | |
| Other | 15 (100) | 0 (0) | 15 (5·8) | |
| Grade | 0·511 | |||
| G1 | 36 (88) | 5 (12) | 41 (16·0) | |
| G2 | 87 (90) | 10 (10) | 97 (37·7) | |
| G3 | 83 (85) | 15 (15) | 98 (38·1) | |
| Unknown | 20 (95) | 1 (5) | 21 (8·2) | |
| Subtype | 0·387 | |||
| Unknown | 23 (88) | 3 (12) | 26 (10·1) | |
| Luminal A | 70 (91) | 7 (9) | 77 (30·0) | |
| Luminal B (Ki67 ≥ 20%) | 22 (81) | 5 (19) | 27 (10·5) | |
| Luminal B (HER2-positive) | 22 (88) | 3 (12) | 25 (9·7) | |
| HER2-positive | 66 (90) | 7 (10) | 73 (28·4) | |
| Triple negative | 23 (79) | 6 (21) | 29 (11·3) | |
| Local treatment | 0·206 | |||
| Mastectomy without radiotherapy | 49 (82) | 11 (18) | 60 (23·3) | |
| Mastectomy with radiotherapy | 27 (87) | 4 (13) | 31 (12·1) | |
| Quadrantectomy with radiotherapy | 150 (90·4) | 16 (9·6) | 166 (64·6) | |
| Systemic treatment | < 0·001 | |||
| None | 109 (93·2) | 8 (6·8) | 117 (45·5) | |
| Endocrine therapy | 110 (89·4) | 13 (10·6) | 123 (47·9) | |
| Chemotherapy | 5 (36) | 9 (64) | 14 (5·4) | |
| Chemotherapy + endocrine therapy | 2 (67) | 1 (33) | 3 (1·2) | |
Values in parentheses are percentages of
row and.
column. SLN, sentinel lymph node; HER2, human epidermal growth factor receptor 2.
Axillary surgery
Axillary dissection was performed in 16 of the 31 women with positive SLNs: one patient with ITCs, ten with micrometastasis and five with macrometastasis. The five patients with macrometastasis had no more than three positive lymph nodes at final histological examination (pN1a). The remaining 15 women (11 with ITCs and 4 with micrometastasis of the SLN) were diagnosed in the later period (from 2004 onwards) and were thus not subjected to axillary dissection. Table 2 shows the clinical and pathological characteristics of the women in the study, according to lymph node status.
Breast surgery
Breast-conserving surgery (BCS) was performed in 166 of the 257 women (64·6 per cent); of these, 150 (90·4 per cent) had negative and 16 (9·6 per cent) had positive SLNs. A total of 91 women (35·4 per cent) had a mastectomy, with conservation of the nipple–areola complex and immediate reconstruction in most cases. Of these 91 women, 76 (84 per cent) had negative and 15 (16 per cent) had positive SLNs. Of the 31 women who had nipple-sparing mastectomy and received intraoperative radiotherapy of the nipple–areola complex, 27 had negative and four had positive SLNs.
Adjuvant treatment
Adjuvant endocrine treatment alone was given to 123 of the 257 women (47·9 per cent) who underwent SLNB; 14 (5·4 per cent) received chemotherapy alone and three women (1·2 per cent) had both chemotherapy and endocrine therapy (Table 2). The distribution of treatment by SLN status is shown in Table S1 (supporting information).
Of the 53 women who did not undergo SLNB, 21 received endocrine therapy alone; eight of these were classified as having the luminal A subtype. Four patients received chemotherapy alone: one had the luminal B subtype with Ki67 of 20 per cent or above, one patient had HER2+ cancer, one had the triple-negative subtype, and in one patient information to determine tumour subtype was missing. Five patients received endocrine therapy plus chemotherapy: two had the luminal A subtype, one had the luminal B subtype (HER2+), one had the triple-negative subtype, and one patient had insufficient information to ascertain the tumour subtype. The remaining 23 patients did not receive adjuvant treatment in accordance with pathological tumour stage.
Recurrence and survival
The median duration of follow-up was 11 years, with 2765 cumulative person-years. At median follow-up, 14 deaths and 69 first events were observed. Seventeen local recurrences, six regional recurrences and six distant metastases were observed among the 226 SLN-negative patients. In the SLN-positive group without further axillary dissection, two local events, one regional event and one case of distant metastasis were observed, whereas in the SLN-positive group that had subsequent axillary dissection, there were two local events and one case of distant metastasis. Fig. 1a shows the cumulative incidence of events over 15 years of follow-up. The estimated 10-year cumulative incidence of local, regional and distant recurrence was 7·0, 2·9 and 3·2 per cent respectively. DFS and OS are shown in Fig. 1b and 1c respectively. The estimated 10-year DFS rate was 77·5 per cent, and the estimated 10-year OS rate was 94·8 per cent. The cumulative incidence of regional and local recurrence in relation to SLN status and its associated surgical axillary treatment (SLN-negative or SLN-positive followed or not by axillary dissection) is shown in Fig. 2a,b.
Fig. 1.
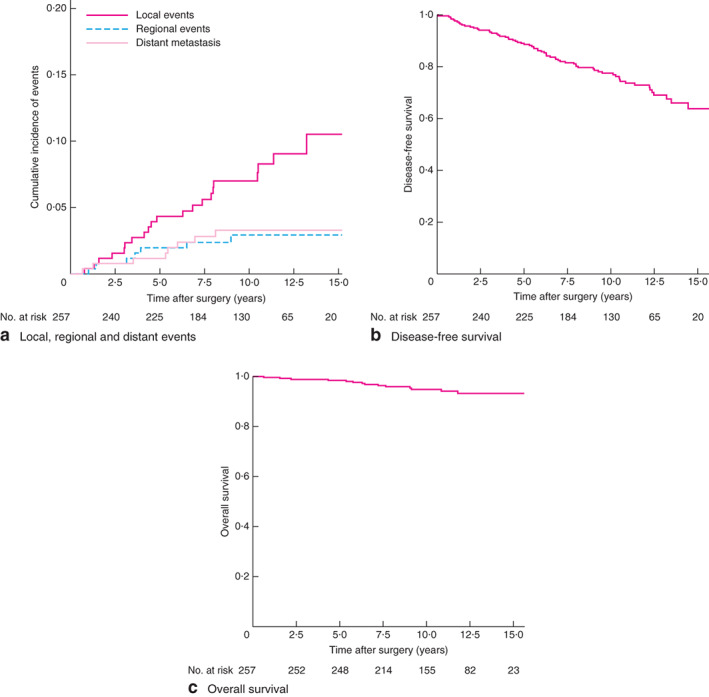
Cumulative incidence of local, regional and distant events, disease-free and overall survival. a Local, regional and distant events, b disease-free survival and c overall survival
Fig. 2.
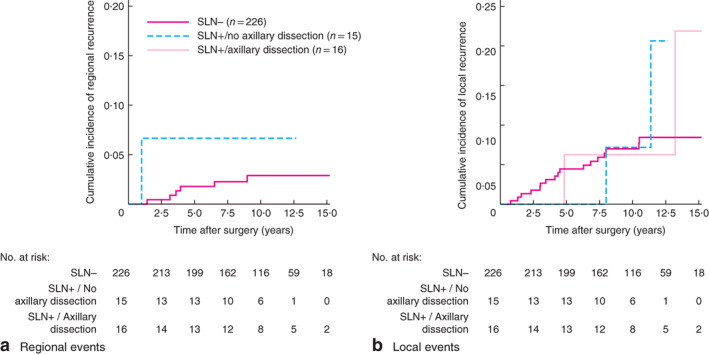
Cumulative incidence of regional and local events according to sentinel lymph node status and axillary dissection. a Regional events, b local events. SLN, sentinel lymph node. aP = 0·495, bP = 0·628 (Gray's test)
Discussion
In the present study, the incidence of SLNB metastasis was 12·1 per cent in patients with microinvasive breast cancer, which falls within the range described in the literature. The rate of macrometastasis was low (1·9 per cent). Moreover the long-term outcomes were favourable (median follow-up 11 years) with a very low rate of regional recurrence in patients with positive SLNs. There was only one regional recurrence among patients with positive SLNs who did not undergo axillary dissection, which was not significantly different from recurrence in the group of patients who had axillary dissection after a positive SLNB finding. No correlation was found between the incidence of SLN metastasis and type of breast surgery, conservation of the breast with or without radiotherapy, or mastectomy without radiotherapy. Most interesting is the discovery of a higher rate of regional recurrence in patients with microinvasive DCIS with negative SLNs, but with a specific molecular pattern.
The findings of this study indicate that SLNB may not be useful in microinvasive DCIS owing to the low risk of lymph node metastasis and good prognosis. The good prognosis may be explained by the theory15 that the major rate of positivity could correspond to an iatrogenic transit of tumour/epithelial cells to lymph nodes, without the significance of real metastasis. Level 1 evidence shows that, in patients with SLN-positive breast cancer, axillary dissection may be avoided when there is a low axillary metastatic burden (Z0011)42 and in patients undergoing BCS with radiotherapy; this also supports the conclusion that SLNB in microinvasive DCIS may not be useful. In particular, in the women in the present study who underwent BCS and axillary dissection for positive sentinel nodes, the total number of positive nodes, including sentinel nodes, was less than three, including those women who met the American College of Surgeons Oncology Group Z0011 criteria. An important consideration in staging the axilla in these patients is the possible implication for systemic therapy. In this study, however, adjuvant treatment was largely decided based on cancer biology.
Microinvasive breast cancer is a rare form of breast cancer defined by the presence of 1 mm of invasive cancer in a background of DCIS, and comprises 0·6–3·4 per cent of all breast cancer1,39,41. In the AJCC staging system, it is considered a subset of T1 disease (T1mi)39. A precise and more complete definition is the WHO classification of clearly separate microscopic foci of infiltration of tumour cells into the mammary stroma, each 1 mm or less in size. No further extension beyond the specialized intralobular stroma is required, the number of invasive foci and their proportion among all the carcinoma cells are irrelevant, and sizes of different foci are not to be added together43. Invasive cells are generally found in the context of DCIS in the background with microinvasive cancer found in 10–20 per cent of patients with DCIS2. This consideration could justify the fact that it is often defined as DCIS with microinvasion7,44. The sole presence of an invasive breast carcinoma of 1 mm or less, with no in situ background, is rare and should be regarded as an invasive carcinoma of that specific diameter1.
A number of relevant studies6,22,24,45–47 have investigated the histopathological characteristics and clinical outcomes of microinvasive DCIS; how patient survival and the biological behaviour of this rare form of breast carcinoma differ from DCIS remain controversial. Microinvasive DCIS is frequently found in a high nuclear grade comedo DCIS setting, and less frequently with other types of DCIS or lobular carcinoma in situ48.
The present findings, of low positive SLN rates in women with good DFS and OS, and the lack of influence on selection of adjuvant treatment, are in line with other studies4,7,15,20,23 showing that SLNB in microinvasive DCIS may not be useful. This study supports the evidence that less surgery, combined with adequate presurgical clinical/histological information allowing the planning of a correct, personalized, clinical pathway for each patient, may provide the same level of OS with better patient quality of life.
Supplementary Material
Table S1 Distribution according to sentinel lymph node status
Acknowledgements
Preparation of this study was funded in part by National Institutes of Health/National Cancer Institute Cancer Center Support Grant P30 CA008748 to Memorial Sloan Kettering Cancer Center.
Informed consent was obtained from all individual participants included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki Declaration and its later amendments, or comparable ethical standards.
Disclosure: The authors declare no conflict of interest.
References
- 1. Bianchi S, Vezzosi V. Microinvasive carcinoma of the breast. Pathol Oncol Res 2008; 14: 105–111. [DOI] [PubMed] [Google Scholar]
- 2. Fang Y, Wu J, Wang W, Fei X, Zong Y, Chen Xet al. Biologic behavior and long-term outcomes of breast ductal carcinoma in situ with microinvasion. Oncotarget 2016; 7: 64 182–64 190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lagios MD, Westdahl PR, Margolin FR, Rose MR. Duct carcinoma in situ. Relationship of extent of noninvasive disease to the frequency of occult invasion, multicentricity, lymph node metastases, and short-term treatment failures. Cancer 1982; 50: 1309–1314. [DOI] [PubMed] [Google Scholar]
- 4. Orzalesi L, Casella D, Criscenti V, Gjondedaj U, Bianchi S, Vezzosi Vet al. Microinvasive breast cancer: pathological parameters, cancer subtypes distribution, and correlation with axillary lymph nodes invasion. Results of a large single-institution series. Breast Cancer 2016; 23: 640–648. [DOI] [PubMed] [Google Scholar]
- 5. Edge S, Byrd DR, Compton CC, Fritz GA, Greene FL, Trotti A. AJCC Cancer Staging Manual (7th edn). Springer: New York, 2009. [Google Scholar]
- 6. Vieira CC, Mercado CL, Cangiarella JF, Moy L, Toth HK, Guth AA. Microinvasive ductal carcinoma in situ: clinical presentation, imaging features, pathologic findings, and outcome. Eur J Radiol 2010; 73: 102–107. [DOI] [PubMed] [Google Scholar]
- 7. Lyons JM, Stempel M, Van Zee KJ, Cody HS. Axillary node staging for microinvasive breast cancer: is it justified? Ann Surg Oncol 2012; 19: 3416–3421. [DOI] [PubMed] [Google Scholar]
- 8. Lyman GH, Temin S, Edge SB, Newman LA, Turner RR, Weaver DLet al.; American Society of Clinical Oncology Clinical Practice. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 2014; 32: 1365–1383. [DOI] [PubMed] [Google Scholar]
- 9. Gojon H, Fawunmi D, Valachis A. Sentinel lymph node biopsy in patients with microinvasive breast cancer: a systematic review and meta-analysis. Eur J Surg Oncol 2014; 40: 5–11. [DOI] [PubMed] [Google Scholar]
- 10. Camp R, Feezor R, Kasraeian A, Cendan J, Schell S, Wilkinson Eet al. Sentinel lymph node biopsy for ductal carcinoma in situ: an evolving approach at the University of Florida. Breast J 2005; 11: 394–397. [DOI] [PubMed] [Google Scholar]
- 11. Cox CE, Nguyen K, Gray RJ, Salud C, Ku NN, Dupont Eet al. Importance of lymphatic mapping in ductal carcinoma in situ (DCIS): why map DCIS? Am Surg 2001; 67: 513–519. [PubMed] [Google Scholar]
- 12. Fortunato L, Santoni M, Drago S, Gucciardo G, Farina M, Cesarini Cet al.; Rome Breast Cancer Study Group. Sentinel lymph node biopsy in women with pT1a or ‘microinvasive’ breast cancer. Breast 2008; 17: 395–400. [DOI] [PubMed] [Google Scholar]
- 13. Gray RJ, Mulheron B, Pockaj BA, Degnim A, Smith SL. The optimal management of the axillae of patients with microinvasive breast cancer in the sentinel lymph node era. Am J Surg 2007; 194: 845–848. [DOI] [PubMed] [Google Scholar]
- 14. Guth AA, Mercado C, Roses DF, Darvishian F, Singh B, Cangiarella JF. Microinvasive breast cancer and the role of sentinel node biopsy: an institutional experience and review of the literature. Breast J 2008; 14: 335–339. [DOI] [PubMed] [Google Scholar]
- 15. Hanna MG, Jaffer S, Bleiweiss IJ, Nayak A. Re-evaluating the role of sentinel lymph node biopsy in microinvasive breast carcinoma. Mod Pathol 2014; 27: 1489–1498. [DOI] [PubMed] [Google Scholar]
- 16. Intra M, Zurrida S, Maffini F, Sonzogni A, Trifirò G, Gennari Ret al. Sentinel lymph node metastasis in microinvasive breast cancer. Ann Surg Oncol 2003; 10: 1160–1165. [DOI] [PubMed] [Google Scholar]
- 17. Kapoor NS, Shamonki J, Sim MS, Chung CT, Giuliano AE. Impact of multifocality and lymph node metastasis on the prognosis and management of microinvasive breast cancer. Ann Surg Oncol 2013; 20: 2576–2581. [DOI] [PubMed] [Google Scholar]
- 18. Katz A, Gage I, Evans S, Shaffer M, Fleury T, Smith FPet al. Sentinel lymph node positivity of patients with ductal carcinoma in situ or microinvasive breast cancer. Am J Surg 2006; 191: 761–766. [DOI] [PubMed] [Google Scholar]
- 19. Klauber-DeMore N, Tan LK, Liberman L, Kaptain S, Fey J, Borgen Pet al. Sentinel lymph node biopsy: is it indicated in patients with high-risk ductal carcinoma-in-situ and ductal carcinoma-in-situ with microinvasion? Ann Surg Oncol 2000; 7: 636–642. [DOI] [PubMed] [Google Scholar]
- 20. Ko BS, Lim WS, Kim HJ, Yu JH, Lee JW, Kwan SBet al. Risk factor for axillary lymph node metastases in microinvasive breast cancer. Ann Surg Oncol 2012; 19: 212–216. [DOI] [PubMed] [Google Scholar]
- 21. Leidenius M, Salmenkivi K, von Smitten K, Heikkilä P. Tumour-positive sentinel node findings in patients with ductal carcinoma in situ. J Surg Oncol 2006; 94: 380–384. [DOI] [PubMed] [Google Scholar]
- 22. Margalit DN, Sreedhara M, Chen YH, Catalano PJ, Nguyen PL, Golshan Met al. Microinvasive breast cancer: ER, PR, and HER-2/neu status and clinical outcomes after breast-conserving therapy or mastectomy. Ann Surg Oncol 2013; 20: 811–818. [DOI] [PubMed] [Google Scholar]
- 23. Matsen CB, Hirsch A, Eaton A, Stempel M, Heerdt A, Van Zee KJet al. Extent of microinvasion in ductal carcinoma in situ is not associated with sentinel lymph node metastases. Ann Surg Oncol 2014; 21: 3330–3335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Parikh RR, Haffty BG, Lannin D, Moran MS. Ductal carcinoma in situ with microinvasion: prognostic implications, long-term outcomes, and role of axillary evaluation. Int J Radiat Oncol Biol Phys 2012; 82: 7–13. [DOI] [PubMed] [Google Scholar]
- 25. Pimiento JM, Lee MC, Esposito NN, Kiluk JV, Khakpour N, Carter WBet al. Role of axillary staging in women diagnosed with ductal carcinoma in situ with microinvasion. J Oncol Pract 2011; 7: 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ross DS, Hoda SA. Microinvasive (T1mic) lobular carcinoma of the breast: clinicopathologic profile of 16 cases. Am J Surg Pathol 2011; 35: 750–756. [DOI] [PubMed] [Google Scholar]
- 27. Sakr R, Bezu C, Raoust I, Antoine M, Ettore F, Darcourt Jet al. The sentinel lymph node procedure for patients with preoperative diagnosis of ductal carcinoma in situ: risk factors for unsuspected invasive disease and for metastatic sentinel lymph nodes. Int J Clin Pract 2008; 62: 1730–1735. [DOI] [PubMed] [Google Scholar]
- 28. Tunon-de-Lara C, Giard S, Buttarelli M, Blanchot J, Classe JM, Baron Met al. Sentinel node procedure is warranted in ductal carcinoma in situ with high risk of occult invasive carcinoma and microinvasive carcinoma treated by mastectomy. Breast J 2008; 14: 135–140. [DOI] [PubMed] [Google Scholar]
- 29. Wilkie C, White L, Dupont E, Cantor A, Cox CE. An update of sentinel lymph node mapping in patients with ductal carcinoma in situ. Am J Surg 2005; 190: 563–566. [DOI] [PubMed] [Google Scholar]
- 30. Zavagno G, Belardinelli V, Marconato R, Carcoforo P, Franchini Z, Scalco Get al. Sentinel lymph node metastasis from mammary ductal carcinoma in situ with microinvasion. Breast 2007; 16: 146–151. [DOI] [PubMed] [Google Scholar]
- 31. Zavotsky J, Hansen N, Brennan MB, Turner RR, Giuliano AE. Lymph node metastasis from ductal carcinoma in situ with microinvasion. Cancer 1999; 85: 2439–2443. [DOI] [PubMed] [Google Scholar]
- 32. Veronesi U, Zurrida S, Mazzarol G, Viale G. Extensive frozen section examination of axillary sentinel nodes to determine selective axillary dissection. World J Surg 2001; 25: 806–808. [DOI] [PubMed] [Google Scholar]
- 33. Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart Met al.; Panel Members. Tailoring therapies – improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol 2015; 26: 1533–1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Goldhirsch A, Glick JH, Gelber RD, Coates AS, Senn HJ. Meeting highlights: International Consensus Panel on the Treatment of Primary Breast Cancer. Seventh International Conference on Adjuvant Therapy of Primary Breast Cancer. J Clin Oncol 2001; 19: 3817–3827. [DOI] [PubMed] [Google Scholar]
- 35. Goldhirsch A, Glick JH, Gelber RD, Senn HJ. Meeting highlights: International Consensus Panel on the Treatment of Primary Breast Cancer. J Natl Cancer Inst 1998; 90: 1601–1608. [DOI] [PubMed] [Google Scholar]
- 36. Goldhirsch A, Ingle JN, Gelber RD, Coates AS, Thürlimann B, Senn HJ; Panel members . Thresholds for therapies: highlights of the St Gallen International Expert Consensus on the primary therapy of early breast cancer 2009. Ann Oncol 2009; 20: 1319–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ; Panel Members . Strategies for subtypes – dealing with the diversity of breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol 2011; 22: 1736–1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kalbfleisch JD, Prentice RL. The Statistical Analysis of Failure Time Data. Wiley: Hoboken, 1980. [Google Scholar]
- 39. Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 1988; 16: 1141–1154. [Google Scholar]
- 40. Hudis CA, Barlow WE, Costantino JP, Gray RJ, Pritchard KI, Chapman JAet al. Proposal for standardized definitions for efficacy end points in adjuvant breast cancer trials: the STEEP system. J Clin Oncol 2007; 25: 2127–2132. [DOI] [PubMed] [Google Scholar]
- 41. Altman DG, De Stavola BL, Love SB, Stepniewska KA. Review of survival analyses published in cancer journals. Br J Cancer 1995; 72: 511–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Giuliano AE, McCall L, Beitsch P, Whitworth PW, Blumencranz P, Leitch AMet al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg 2010; 252: 426–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pinder SE, Ellis IO, Schnitt SJ, Tan PH, Rutgers E, Morrow M. Microinvasive carcinoma. In WHO Classification of Tumours of the Breast, Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, Van de vijvair MJ (eds). IARC Press: Lyons, 2012; 96–97. [Google Scholar]
- 44. Yang M, Moriya T, Oguma M, De La Cruz C, Endoh M, Ishida Tet al. Microinvasive ductal carcinoma (T1mic) of the breast. The clinicopathological profile and immunohistochemical features of 28 cases. Pathol Int 2003; 53: 422–428. [DOI] [PubMed] [Google Scholar]
- 45. Cavaliere A, Scheibel M, Bellezza G, Colella R, Vitali R, Gori Set al. Ductal carcinoma in situ with microinvasion: clinicopathologic study and biopathologic profile. Pathol Res Pract 2006; 202: 131–135. [DOI] [PubMed] [Google Scholar]
- 46. de Mascarel I, MacGrogan G, Mathoulin-Pélissier S, Soubeyran I, Picot V, Coindre JM. Breast ductal carcinoma in situ with microinvasion: a definition supported by a long-term study of 1248 serially sectioned ductal carcinomas. Cancer 2002; 94: 2134–2142. [DOI] [PubMed] [Google Scholar]
- 47. Wang W, Zhu W, Du F, Luo Y, Xu B. The demographic features, clinicopathological characteristics and cancer-specific outcomes for patients with microinvasive breast cancer: a SEER database analysis. Sci Rep 2017; 7: 42045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Nemoto T, Castillo N, Tsukada Y, Koul A, Eckhert KH, Bauer RL. Lobular carcinoma in situ with microinvasion. J Surg Oncol 1998; 67: 41–46. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Distribution according to sentinel lymph node status


