Abstract
Previous studies investigate the relationship between peroxisome proliferator-activated receptor γ-2 (PPAR) gene Pro12Ala polymorphisms and risk of hypertension. However, the number of available studies was extremely limited. We updated this evidence and gave more significant results. We performed comprehensive computer-based searches in the PubMed, Web of Science, Embase, Google Scholar, the Cochrane library, Wanfang database, China National Knowledge Infrastructure, and China Biological Medicine Database. All studies that reported the association between the PPARγ2Pro12Ala polymorphisms and hypertension were identified. Twenty-one studies were finally included in the present study. In the domain model, the PPARγ1Pro12Ala polymorphism was not associated with hypertension (odds ratio (OR) = 0.85, 95% confidence interval (CI): 0.71–1.03, P=0.108). The significant relationship was found in the recessive model (OR = 0.67, 95% CI: 0.53–0.85), in the additive model (OR = 0.61, 95% CI: 0.48–0.77), and in the allele genetic model (OR = 0.81, 95% CI: 0.66–0.99). Subgroup analysis indicated that the PPARγ1Pro12Ala polymorphism from the all gene models was also not related to the risk of hypertension in Caucasians. In Asians, however, the results (P=0.002; I2 = 57.6%) suggested a significant relationship between PPARγ1Pro12Ala and hypertension in the domain model (OR = 0.80, 95% CI: 0.65–0.99), in the recessive model (OR = 0.57, 95% CI: 0.44–0.75), in the additive model (OR = 0.51, 95% CI: 0.39–0.66), and in the allele model (OR = 0.75, 95% CI: 0.60–0.94). The PPARγ1Pro12Ala polymorphism could affect the risk of primary hypertension amongst Asians. The A allele gene was a protective genotype for primary hypertension. The PPARγ1Pro12Ala polymorphism was not associated with hypertension amongst Caucasians.
Keywords: Hypertension, meta-analysis, polymorphism, peroxisome proliferator-activated receptor
Introduction
Cardiovascular disease is the leading cause of death for adults in developed or developing countries, including China [1]. Hypertension has been proved the primary and independent modifiable risk factor for stroke and coronary heart disease so that controlling hypertension is one of the most effective ways to prevent cardiovascular disease [2]. Hypertension amongst adults with no identifiable cause is essential hypertension. Essential hypertension as complex quantitative trait is affected by varying combinations of genetic and environmental factors. Probably, genetic factor influences the blood pressure through numerous minor-effect genes, and biological process of hypertension involves multiple physiological pathways with gene and environmental factors [3]. Recently, two-stage association study-based community population is a cost-effective approach for identifying complex disease genes in genetic studies and it has received much attention. Researchers have conducted lots of association studies and identified some potential candidate genes in hypertension.
Peroxisome proliferator-activated receptor-γ (PPARγ) belongs to member of the steroid hormone receptor superfamily. Human PPARγ gene is located in the chromosome of 3p25 with 479 amino acid resides [4]. The gene’s full length is 146485 bp. PPAR gene is the one of the PPARs subtypes that is by far the most widely studied. It is not only the target molecular of Thiazolane diketones but also an important regulatory factor of adipocyte differentiation and fat endocrine functions of the important regulatory factor [5]. Moreover, PPAR gene acted as a signal transfer regulator between gene expression of adipocytes and adipogenesis and insulin-producing cells. It was widely expressed in the heart, blood vessels, kidney, muscle and other tissues, and participates in regulating lipid and carbohydrate and smooth muscle proliferation, migration and apoptosis, inflammation, atherosclerosis, and other pathologic processes [6]. Recent studies reported that PPARγ can regulate the blood pressure through renin–angiotensin–aldosterone system. Several studies have assessed the relationship between PPARγ gene polymorphism and primary hypertension [7–10]. These reports were not consistent because of differences in study populations, sample sizes, and so on. Yang et al. [11] had conducted a meta-analysis to quantitatively evaluate the relationship between the PPARγ2Pro12Ala (rs19813) polymorphism and hypertension. However, several important studies were not included in the analyses [10,12–18]. In the present study, we updated this evidence and gave more significant results.
Materials and methods
This meta-analysis was in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Cochrane Handbook for Systematic Reviews.
Literature search
We performed comprehensive computer-based searches in the PubMed, Web of Science, Embase, Google Scholar, the Cochrane Library, Wanfang database, China National Knowledge Infrastructure, and China Biological Medicine Database from the inception to 28 December 2018. All studies that reported the association between the PPARγ2Pro12Ala polymorphisms and hypertension were identified. The following keywords were used for searching: peroxisome proliferator-activated receptor-γ, PPAR-γ, Pro12Ala, genotype, polymorphism, mutation, single nucleotide polymorphism (SNP,) variant, hypertension. The search language was restricted to Chinese and English. We also reviewed the references lists of reviews and relevant studies for the potential studies as possible as we can.
Criteria for inclusion and exclusion
The included studies have to meet the following criteria: (i) study is from a case–control or cohort study design about relationship between PPAR-γ2Pro12Ala polymorphism and the risk of hypertension; (ii) the diagnostic of hypertension is clear: systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg without antihypertension medications or antihypertension medications were used [7]; (iii) study provides enough genotypes data of case group and control group for analysis; and (iv) the score is not less than 5 points according to the Newcastle–Ottawa Scale. We excluded the following studies: reviews, comments, letters, studies without enough data, quality score < 5. The latest data were used for duplicate data.
Data extraction
Two authors [M.Z. and Q.W.] independently extracted the data. Disagreement was resolved by consensus. If these two authors could not reach a consensus, the result was reviewed by a third author [L.F.]. The extracted data consisted of the follow items: the first author’s name, publication year, country, methods of genotype, sample size of cases and controls, the gene frequency (PP, PA, AA) of case group and control group, Hardy–Weinberg equilibrium (HWE) test results, and scores of quality assessment.
Quality assessment
To determine the methodological quality of each study, we used the Newcastle–Ottawa Scale, which uses a ‘star’ rating system to judge the quality of observational studies [19]. The NOS ranges from zero (worst) up to nine stars (best). Studies with a score equal to or higher than seven were of high quality. Two investigators (J.Z. and L.L.) independently assessed the quality of included studies, and the result was reviewed by a third investigator (L.F.). Disagreement was resolved by discussion.
Statistical analysis
We assessed the association between PPAR gene Pro12Ala polymorphisms and risk of hypertension using the following gene model: dominant (AA/PA vs. PP), recessive (AA vs. PA/PP), additive (AA vs. PP), and allele gene model (A vs. P). The odds ratios (ORs) with 95% confidence intervals (CIs) were calculated to assess the relationship between gene models and risk of hypertension. Heterogeneity was assessed using the Chi-square test (significance level of P<0.1) and the I2 test (greater than 50% as an evidence of significant inconsistency). Pooled effect sizes were determined using a fixed-effects model (the Mantel–Haenszel method) when heterogeneity was negligible (I2 < 50%) or a random-effects model (the DerSimonian and Kacker method) when significant heterogeneity was present (I2 ≥ 50%) [20]. HWE was assessed by the χ2 test in the controls. Subgroup analysis was also performed amongst different populations (Caucasian vs. Asian). We performed the sensitivity analysis by omitting one study each time. To study the relevance of such publication bias, funnel plots were constructed by plotting the trial results against their precision. Begg’s and Egger’s tests were also used to assess the publication bias [21]. A P-value less than 0.05 was considered statistically significant throughout the analyses.
Ethical approval
This meta-analysis belonged to secondary analysis based on the studies published previously, the patients’ informed consent; and the ethical approval was not necessary.
Results
Study selection and general characteristics
The flow of study selection was presented in Figure 1. Our initial search yielded 241 citations. Of these, 125 duplicate records were removed. One hundred and sixteen records were further screened via reviewing title and abstract. Eighty-eight studies were excluded because of results of interest not reported or other reasons. The remaining 28 studies were full-text reviewed, and 7 studies were excluded due to unrelated topics, duplicates, cases and no data for extraction. Finally, 21 studies met the inclusion criteria and were included in the meta-analysis [7–10,12–18,22–31].
Figure 1. Flow chart of study selection.
The general characteristics of the studies included in the meta-analysis are shown in Table 1. Twenty-one studies consisted of 5503 cases and 7862 controls. These studies were published from 2003 to 2018. Fourteen studies were from China, two from Japan, and one each from Sweden, Spain, German, Poland, and Katar. The sample size of case ranged from 70 to 816, and control was from 112 to 1308. Most of studies used the PCR-restriction fragment length polymorphism (PCR-RFLP) to detect the genotype of PPARγ2Pro12Ala. The control selection of three studies did not conform to the HWE.
Table 1. General characteristics of studies included in the meta-analysis.
| Author | Year | Country | Methods of genotype | Sample size | Gene frequency (Case) | Gene frequency (Control) | HWE | Score of quality | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Control | PP | PA | AA | PP | PA | AA | ||||||
| Ostgren [22] | 2003 | Sweden | PCR-RFLP | 194 | 190 | 147 | 43 | 4 | 136 | 51 | 3 | 0.468 | 8 |
| Rodriguez-Esparragon [23] | 2003 | Spain | PCR | 229 | 212 | 206 | 22 | 1 | 174 | 36 | 2 | 0.928 | 7 |
| Horiki [7] | 2004 | Japan | PCR-RFLP | 205 | 300 | 193 | 12 | 0 | 276 | 24 | 0 | 0.471 | 7 |
| Shen [24] | 2004 | China | PCR-RFLP | 125 | 112 | 113 | 11 | 1 | 103 | 9 | 0 | 0.658 | 7 |
| Shen [12] | 2004 | China | PCR-RFLP | 70 | 220 | 66 | 3 | 1 | 206 | 13 | 1 | 0.128 | 6 |
| Zhang [25] | 2005 | China | PCR-RFLP | 132 | 157 | 128 | 4 | 0 | 148 | 9 | 0 | 0.712 | 7 |
| Gouni-Berthold [8] | 2005 | German | PCR-RFLP | 255 | 140 | 190 | 57 | 8 | 104 | 32 | 4 | 0.430 | 7 |
| Pan [26] | 2007 | China | PCR-RFLP | 177 | 119 | 154 | 23 | 0 | 101 | 18 | 0 | 0.372 | 7 |
| Hui [27] | 2007 | Jpan | TaqMan PCR | 261 | 271 | 215 | 16 | 0 | 261 | 10 | 0 | 0.757 | 7 |
| Lu [28] | 2008 | China | PCR-RFLP | 478 | 361 | 446 | 31 | 1 | 312 | 48 | 1 | 0.550 | 7 |
| Ruixing [13] | 2008 | China | PCR-RFLP | 446 | 1213 | 418 | 23 | 5 | 1247 | 64 | 12 | 0.000 | 7 |
| Gao [14] | 2010 | China | PCR-RFLP | 345 | 137 | 337 | 7 | 1 | 131 | 2 | 4 | 0.000 | 7 |
| Zhang [15] | 2011 | China | PCR-SSCP* | 280 | 410 | 264 | 16 | 0 | 392 | 18 | 0 | 0.650 | 7 |
| Dong [9] | 2012 | China | PCR-RFLP | 124 | 178 | 122 | 2 | 0 | 177 | 1 | 0 | 0.970 | 7 |
| Lian [16] | 2012 | China | TaqMan PCR | 272 | 548 | 166 | 90 | 16 | 293 | 205 | 50 | 0.108 | 7 |
| Bener [10] | 2013 | Katar | PCR | 220 | 1308 | 185 | 28 | 7 | 1175 | 122 | 11 | 0.000 | 8 |
| Gu [29] | 2013 | China | TaqMan PCR | 269 | 551 | 166 | 85 | 18 | 293 | 210 | 48 | 0.262 | 7 |
| Chen [30] | 2014 | China | MALDI-TOF-MS | 145 | 165 | 110 | 33 | 2 | 105 | 53 | 7 | 0.924 | 6 |
| Wang [31] | 2015 | China | PCR-RFLP | 816 | 824 | 536 | 244 | 36 | 426 | 318 | 80 | 0.071 | 7 |
| Grygiel-Gorniak [17] | 2015 | Poland | TaqMan PCR | 151 | 120 | 101 | 44 | 6 | 84 | 32 | 4 | 0.661 | 7 |
| Zhang [18] | 2018 | China | PCR-RFLP | 309 | 290 | 262 | 45 | 2 | 259 | 31 | 0 | 0.336 | 8 |
*PCR-SSCP, Polymerase chain reaction single-strand conformation polymorphism.
Assessment of quality
The score of each domain was presented in the Supplementary Material S1. The mean score of included studies was 7.04. The overall quality of studies was high. The main issues were that some studies selected a control population from a hospitalized one. Either cases and controls were not matched in the design and/or confounders were not adjusted for in the analysis. Besides, some studies did not report the non-response rate.
Pooling results
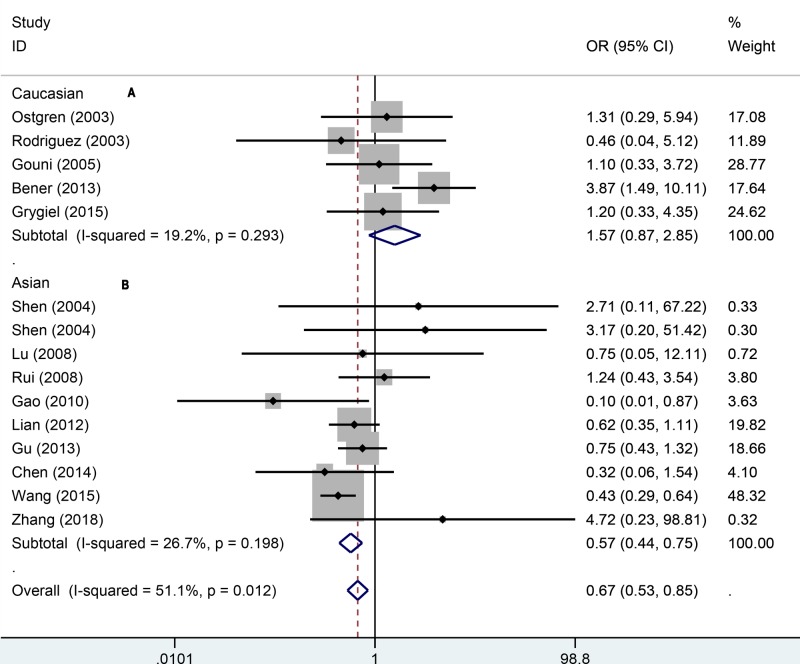
To quantitatively assess the association between PPAR-γ1Pro12Ala and hypertension, we first pooled 21 studies in the domain model (AA/AP vs. PP). The results indicated there was significant heterogeneity (P=0.000; I2 = 64.8%). We used the random-effect model to pool the data, which suggested that the PPARγ1Pro12Ala polymorphism was not associated with hypertension (OR = 0.85, 95% CI: 0.71–1.03, P=0.108). To explore the population differences, we performed the subgroup analyses amongst different populations (Figure 2). In Caucasians, we pooled the data using the fixed-effect model because of moderate heterogeneity (P=0.011; I2 = 69.2%). We found that the PPARγ1Pro12Ala polymorphism was also not related to the risk of hypertension. In Asians, however, the results from random-effect model (P=0.002; I2 = 57.6%) indicated significant relationship between PPAR-γ1Pro12Ala and hypertension (OR = 0.80, 95% CI: 0.65–0.99).
Figure 2. Forest plot for dominant effect model of association between PPAR gene Pro12Ala polymorphisms and risk of hypertension (A: Caucasian, B: Asian).
To explore how the PPARγ1Pro12Ala polymorphism affects the hypertension, we also used other genetic models to assess the relationship. In the recessive model (Figure 3), a significant relationship was found via random-effect model (OR = 0.67, 95% CI: 0.53–0.85). The same result of fixed-effect model was observed in Asians (OR = 0.57, 95% CI: 0.44–0.75). There was no significance for Caucasians (OR = 1.57, 95% CI: 0.87–2.85). In the additive (Figure 4), the overall pooling data indicated significant results (OR = 0.61, 95% CI: 0.48–0.77). The AA genotype was also associated with hypertension risk amongst Asians (OR = 0.51, 95% CI: 0.39–0.66) under the fixed-effect model. For the Caucasians, the additive model suggested no significant relationship between AA genotype and hypertension (OR = 1.58, 95% CI: 0.87–2.56). In the allele genetic model (Figure 5), the overall pooling results suggested significant relationship (OR = 0.81, 95% CI: 0.66–0.99) and so did Asians (OR = 0.75, 95% CI: 0.60–0.94). Just like previous results, there was still no significance between PPAR-γ1Pro12Ala polymorphism and hypertension (OR = 0.94, 95% CI: 0.64–1.73). More details of pooling results are presented in the Table 2.
Figure 3. Forest plot for recessive effect model of association between PPARγ-2 gene Pro12Ala polymorphisms and risk of hypertension (A: Caucasian, B: Asian).
Figure 4. Forest plot for additive effect model of association between PPARγ-2 gene Pro12Ala polymorphisms and risk of hypertension (A: Caucasian, B: Asian).
Figure 5. Forest plot for allele gene model of association between PPARγ-2 gene Pro12Ala polymorphisms and risk of hypertension (A: Caucasian, B: Asian).
Table 2. Summary of different comparative results.
| Category | Genetic model | OR (95% CI) | Z | P-value | I2 (%) | Pheterogeneity | Effect model | |
|---|---|---|---|---|---|---|---|---|
| Overall | Dominant | AA/PA vs. PP | 0.85 (0.71–1.03) | 1.61 | 0.108 | 64.8 | 0.000 | Random |
| Recessive | AA vs. PA/PP | 0.67 (0.53–0.85) | 0.65 | 0.518 | 51.1 | 0.012 | Random | |
| Additive | AA vs. PP | 0.61 (0.48–0.77) | 4.06 | 0.000 | 58.6 | 0.002 | Random | |
| Allele | A vs. P | 0.81 (0.66–0.99) | 2.08 | 0.038 | 76.5 | 0.000 | Random | |
| Asian | Dominant | AA/PA vs. PP | 0.80 (0.65–0.99) | 2.05 | 0.040 | 57.6 | 0.002 | Random |
| Recessive | AA vs. PA/PP | 0.57 (0.44–0.75) | 2.43 | 0.015 | 26.7 | 0.198 | Fixed | |
| Additive | AA vs. PP | 0.51 (0.39–0.66) | 5.00 | 0.000 | 36.4 | 0.117 | Fixed | |
| Allele | A vs. P | 0.75 (0.60–0.94) | 2.55 | 0.011 | 70.7 | 0.000 | Random | |
| Caucasian | Dominant | AA/PA vs. PP | 0.97 (0.66–1.43) | 0.14 | 0.887 | 69.2 | 0.011 | Random |
| Recessive | AA vs. PA/PP | 1.57 (0.87–2.85) | 1.49 | 0.136 | 17.4 | 0.304 | Fixed | |
| Additive | AA vs. PP | 1.58 (0.87–2.86) | 1.50 | 0.134 | 26.0 | 0.248 | Fixed | |
| Allele | A vs. P | 0.94 (0.64–1.37) | 0.33 | 0.743 | 75.1 | 0.003 | Random | |
Sensitivity analysis and publication bias
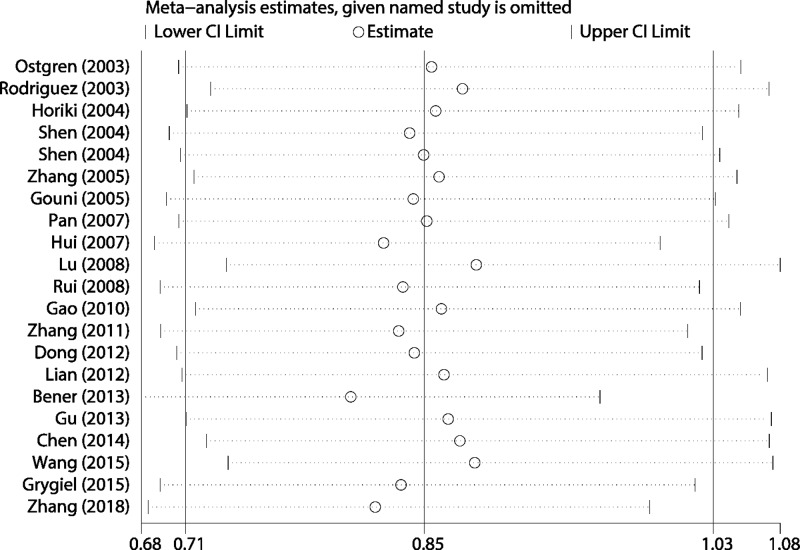
The sensitivity analysis result is presented in Figure 6. We performed the sensitivity analysis in the dominant because this model included all studies’ data. As we can see in the figure, the estimated results keep stable when given named study is omitted. The funnel plot indicated slight asymmetry, which means potential publication bias may exist (Figure 7). We also quantitatively assessed the publication bias using the Egger’s and Begg’s tests. The results suggested no potential publication bias (Z = 1.06, P=0.291; t = 1.98, P=0.062).
Figure 6. Sensitivity analysis for the overall pooled results based on dominant effect model.
Figure 7. Funnel plot for publication bias.
Discussion
In the present study, our results based on larger sample sizes and more study number indicated that (i) PPAR-γ1Pro12Ala gene polymorphism was associated with the risk of hypertension. The AA genotype and A allele could decrease the risk of hypertension in the overall population compared with PP genotype and P allele, respectively. (ii) The population difference was source of heterogeneity within studies. Furthermore, (iii) the subgroup analysis suggested that the PPARγ1Pro12Ala gene polymorphism affects the risk of hypertension amongst Asians. However, no significant relationships were found amongst Caucasians. Our results provided more strong evidence support for the confirmation of relationship between PPARγ1Pro12Ala polymorphism and the risk of primary hypertension. Previous studies also assessed the relationship between common polymorphism (rs1801282) in the PPAR-γ2 gene and hypertension susceptibility [32,33]. However, this study only consisted of eight studies, and one of these studies was not in accordance with HWE. Several studies also included controls with diabetes mellitus and other diseases. The sensitivity analysis was not performed for this issue, which made the pooled results unstable. After that, Yang et al. [11] performed another investigation about this topic. They also just added five studies based on previous studies. The present study consisted of 21 studies. Although Yang et al. [11] also conducted subgroup analyses, the subgroup analyses were performed between China and Japan. Of course, they drew no significant difference between two countries. The present study performed subgroup between two populations (Asian and Caucasian) because the genetic background has more profound effects on hypertension susceptibility [30]. The pooled results confirmed our assumption. The PPARγ1Pro12Ala gene polymorphism tend to be associated with hypertension in Asians not Caucasians.
Our results found that the A allele appears to have a protective effect against hypertension. This result is similar to previous several studies. Lu et al. [28] found that Pro12Ala polymorphism of the PPAR-γ2 gene is associated with hypertension and triglycerides levels in Chinese nonagenarians/centenarians. The A allele frequency was significantly lower in the hypertension than that in the control group (3.45 vs. 6.92%) [28]. Bener et al. [10] investigated the association of the Pro12Ala polymorphism of the human PPARγ 2 (PPAR-γ2) gene with hypertension in a highly consanguineous aboriginal Qatari population. This study also revealed an association between the PPAR-γ2Ala allele and hypertension in Qatar’s population [10]. Paralleled with Lu et al.’s [28] study, Wang et al. [31] conducted a case–control study on PPARγ polymorphism and essential hypertension in Chinese Han. They also found that the A allele of PPAR-γ was associated with lower risk of essential hypertension [31]. On the contrary, Li et al. [18] recently investigated the relationship between the polymorphism of peroxisome proliferators-activated receptor2 gene Pro12Ala and essential hypertension in Hui and Han nationality in Ningxia Province. This study reported that there was no correlation between Pro12Ala polymorphism of PPAR-γ 2 gene and essential hypertension Hui and Han population in Ningxia. Furthermore, this gene polymorphism had no racial difference between Hui and Han populations in Ningxia [18]. These results indicated the effect of Pro12Ala is also different even under the same genetic background. The underlying mechanism for the protective effect of the Ala allele remains speculative. The reasons could be explained by the following several mechanisms. First, PPAR-γ can inhibit the growth of vascular cells. Most cells from blood vessel can express PPAR-γ that induces apoptosis of vascular smooth muscle cells (VSMC) and improves the vascular structure. The infusion of Ang II can increase arterial blood vessels middle/space ratio, and this situation can be relieved through the usage of rosiglitazone and pioglitazone. PPAR-γ also can degrade AT1 receptor expression and inhibit DNA synthesis stimulated by Ang II by adjusting the cyclin-dependent kinase inhibitor. Rosiglitazone can induce VSMC apoptosis, which may be related to this effect [34]. Second, PPAR can affect the renin–angiotensin system (RASS) via the following several pathways: inhibiting the expression of angiotensinogen, inhibiting Ang II activity, and degrading the angiotensin receptor I expression in the VSMCs. In vitro, high-salt diet can make the SHR blood pressure significantly increased (185 + 6) mmHg vs. (128 ± 5) mmHg, and this process can be blocked by Rosiglitazone block (126 + 4 mmHg). Ang II synthetic process and glomerular mesangial cell proliferation was also inhibited, which indicated that the role in antihypertensive and protecting renal was associated with Ang II. Diep et al. [35] found that Rosiglitazone can reverse the elevation blood pressure effect caused by Ang II. Third, PPAR-γ can regulate the blood pressure by regulating vascular vasodilators and vasoconstrictors secretion. PPAR-γ can stimulate endothelial cells to secrete type-C natriuretic peptide (CNP). C peptide is one of diuresis sodium peptide family members, produced by endothelial cells, is a kind of new in the original diastolic peptide. Previous study found that CNP gene transfection mediated by adenovirus can significantly inhibit the proliferation of VSMCs [36]. During the process of coronary artery atherosclerosis formation, the CNP expressed by endothelial cell also gradually reduced. However, Triglidone and Pioglitazone can stimulate the secretion of CNP by endothelial cells. The present findings were from the effect of PPAR-γ agonist on blood pressure [37]. The direct function mechanism of PPAR in regulating blood pressure needs further research.
The present study has several strengths. Compared with previous studies, our study consisted of a larger sample size (5503 cases and 7862 controls), which improved the statistical power and provided more accurate results. We also conducted subgroup analysis that were not reported in previous study. Besides, the present study followed the PRISMA and Cochrane Handbook for Systematic Reviews. Several study limitations should be addressed. First, the present pooled results were from unadjusted data, and some potential confounding factors may affect the results. We confirm that the population difference was one of the potential confounding factors. Second, we can see publication bias may exist though the Egger’s and Begg’s tests gave no significant results. Maybe it was related to search language because we only performed search in English and Chinese. Third, the study number and sample size in Caucasians was very limited. Studies with larger sample sizes are needed. Finally, future study should take the gene–environment effects into consideration.
In conclusion, the PPAR-γ2 Pro12Ala polymorphism could affect the risk of primary hypertension amongst Asians. The A allele gene was a protective genotype in primary hypertension. The PPAR-γ1Pro12Ala polymorphism was not associated with hypertension amongst Caucasians. Study with more sample size is needed, especially for Caucasians. The future research should pay attention on the molecular mechanisms behind this.
Supporting information
Supplementary material 1. Methodological quality assessment (risk of bias) of included studies by Newcastle-Ottawa Scales.
Acknowledgments
We thank the help from Department of Clinical Medicine Tianjin University of Traditional Chinese.
Abbreviations
- Ang II
Angiotensin II
- AT I
Angiotensin type 1 receptor
- CI
Confidence interval
- CNP
Type-C natriuretic peptide
- HWE
Hardy–Weinberg equilibrium
- NOS
Nitric oxide synthase
- OR
Odds ratio
- PPAR
Peroxisome proliferator-activated receptor
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- SHR
Spontaneously hypertensive rat
- VSMC
Vascular smooth muscle cell
Funding
The authors declare that there are no sources of funding to be acknowledged.
Competing interests
The authors declare that there are no competing interests associated with the manuscript.
Author contribution
Z.M. conceived and designed the research; Z.J.P. and L.L.F. analyzed the data; W.Q. created and revised all tables and figures; Z.M. drafted the manuscript; F.L.M. made critical revision of the manuscript; all authors read and approved the final manuscript.
References
- 1.Bundy J.D. and He J. (2016) Hypertension and related cardiovascular disease burden in China. Ann. Glob. Health 82, 227–233 10.1016/j.aogh.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 2.Redon J., Tellez-Plaza M., Orozco-Beltran D., Gil-Guillen V., Pita F.S., Navarro-Perez J.. et al. (2016) Impact of hypertension on mortality and cardiovascular disease burden in patients with cardiovascular risk factors from a general practice setting: the ESCARVAL-risk study. J. Hypertens. 34, 1075–1083 10.1097/HJH.0000000000000930 [DOI] [PubMed] [Google Scholar]
- 3.Sharma V. and McNeill J.H. (2006) The etiology of hypertension in the metabolic syndrome part two: the gene-environment interaction. Curr. Vasc. Pharmacol. 4, 305–320 10.2174/157016106778521661 [DOI] [PubMed] [Google Scholar]
- 4.Tabassum A., Zaidi S., Yasmeen K. and Mahboob T. (2018) Potential role of peroxisome proliferator activated receptor γ activation on serum visfatin and trace elements in high fat diet induced type 2 diabetes mellitus. Life Sci. 205, 164–175 10.1016/j.lfs.2018.05.027 [DOI] [PubMed] [Google Scholar]
- 5.Sadeghabadi Z.A., Nourbakhsh M., Alaee M., Larijani B. and Razzaghy-Azar M. (2018) Peroxisome proliferator-activated receptor γ expression in peripheral blood mononuclear cells and angiopoietin-like protein 4 levels in obese children and adolescents. J. Endocrinol. Invest. 41, 241–247 10.1007/s40618-017-0730-y [DOI] [PubMed] [Google Scholar]
- 6.Szkup M., Owczarek A.J., Schneider-Matyka D., Brodowski J., Loj B. and Grochans E. (2018) Associations between the components of metabolic syndrome and the polymorphisms in the peroxisome proliferator-activated receptor γ (PPAR-γ), the fat mass and obesity-associated (FTO), and the melanocortin-4 receptor (MC4R) genes. Aging (Albany N.Y.) 10, 72–82 10.18632/aging.101360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horiki M., Ikegami H., Fujisawa T., Kawabata Y., Ono M., Nishino M.. et al. (2004) Association of Pro12Ala polymorphism of PPARγ gene with insulin resistance and related diseases. Diabetes Res. Clin. Pract. 66, S63–S67 10.1016/j.diabres.2003.09.023 [DOI] [PubMed] [Google Scholar]
- 8.Gouni-Berthold I., Giannakidou E., Muller-Wieland D., Faust M., Kotzka J., Berthold H.K.. et al. (2005) Peroxisome proliferator-activated receptor-γ2 Pro12Ala and endothelial nitric oxide synthase-4a/b gene polymorphisms are not associated with hypertension in diabetes mellitus type 2. J. Hypertens. 23, 301–308 10.1097/00004872-200502000-00012 [DOI] [PubMed] [Google Scholar]
- 9.Dong H.R., Han F.Q. and Su X.L. (2012) The relationship between peroxisome proliferator-activated receptor γ and its coactivated 1α and mongolian hypertension. Int. J. Lab. Med. 33, 2698–2700 [Google Scholar]
- 10.Bener A., Darwish S., Al-Hamaq A.O., Mohammad R.M. and Yousafzai M.T. (2013) Association of PPARγ2 gene variant Pro12Ala polymorphism with hypertension and obesity in the aboriginal Qatari population known for being consanguineous. Appl. Clin. Genet. 6, 103–111 10.2147/TACG.S49875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang W., Wang J., Ye W. and Li X. (2018) Quantitative evaluation of PPAR-γ2 Pro12Ala polymorphism with hypertension. Herz 43, 719–727 10.1007/s00059-017-4618-6 [DOI] [PubMed] [Google Scholar]
- 12.Shen D. and Ha D.W. (2005) Relationship between PPARγ2 gene Pro12Ala polymorphism and hypertension complicated with cerebral infarction in the elderly. Chin. J. Gerontol. 25, 235–237 [Google Scholar]
- 13.Ruixing Y., Jinzhen W., Shangling P., Weixiong L., Dezhai Y. and Yuming C. (2008) Sex differences in environmental and genetic factors for hypertension. Am. J. Med. 121, 811–819 10.1016/j.amjmed.2008.04.026 [DOI] [PubMed] [Google Scholar]
- 14.Gao L., Wang L., Yun H., Su L. and Su X. (2010) Association of the PPARγ2 gene Pro12Ala variant with primary hypertension and metabolic lipid disorders in Han Chinese of Inner Mongolia. Genet. Mol. Res. 9, 1312–1320 10.4238/vol9-3gmr833 [DOI] [PubMed] [Google Scholar]
- 15.Zhang Z.B. (2011) Genetic characteristics of essential hypertension and its association with LDLR, APM-1 and PPAR-γ2 genes in Yanbian Korean and Han Chinese. Graduation Thesis, Yanbian University, Yanbian, China [Google Scholar]
- 16.Lian Y., Gu S.J., Wu M., Chen Q., Zhou Z.Y., Yu H.. et al. (2012) Relationship between peroxisome proliferator-activated receptor single nucleotide polymorphisms and essential hypertension. Chin. J. Hypertens. 22, 1000 [Google Scholar]
- 17.Grygiel-Gorniak B., Kaczmarek E., Mosor M., Przyslawski J. and Nowak J. (2015) Association of PPAR-γ2 and beta3-AR polymorphisms with postmenopausal hypertension. J. Clin. Hypertens. (Greenwich) 17, 549–556 10.1111/jch.12537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang X.F., Li X.R., Xue X.H. and Xu Q.B. (2018) Relationship between the polymorphism of peroxisome proliferators-activated receptor2 gene Pro12Ala and essential hypertension in Hui and Han nationality in Ningxia Province. J. Clin. Cardio. (China) 34, 47–51 [Google Scholar]
- 19.Wen J., Lv Z., Ding H., Fang X. and Sun M. (2018) Association between PXR polymorphisms and cancer risk: a systematic review and meta-analysis. Biosci. Rep. 38, pii: BSR20171614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang M., Shi M. and Zhao Y. (2018) Association between serum copper levels and cervical cancer risk: a meta-analysis. Biosci. Rep. 38, pii: BSR20180161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dong Y., Zhou J., Zhu Y., Luo L., He T., Hu H.. et al. (2017) Abdominal obesity and colorectal cancer risk: systematic review and meta-analysis of prospective studies. Biosci. Rep. 37, pii: BSR20170945, 10.1042/BSR20170945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ostgren C.J., Lindblad U., Melander O., Melander A., Groop L. and Rastam L. (2003) Peroxisome proliferator-activated receptor-γPro12Ala polymorphism and the association with blood pressure in type 2 diabetes: skaraborg hypertension and diabetes project. J. Hypertens. 21, 1657–1662 10.1097/00004872-200309000-00014 [DOI] [PubMed] [Google Scholar]
- 23.Rodriguez-Esparragon F.J., Rodriguez-Perez J.C., Macias-Reyes A. and Alamo-Santana F. (2003) Peroxisome proliferator-activated receptor-γ2-Pro12Ala and endothelial nitric oxide synthase-4a/bgene polymorphisms are associated with essential hypertension. J. Hypertens. 21, 1649–1655 10.1097/00004872-200309000-00013 [DOI] [PubMed] [Google Scholar]
- 24.Shen D. and Ha D.W. (2004) Relationship between PPAR γ2 gene Pro12Ala polymorphism hypertension and blood lipids. Chin. J. Hypertens. 12, 41–44 [Google Scholar]
- 25.Zhang A.P., Zhang M.X., Zhang J.H., Xie H.J. and Yu Y.K. (2005) The influence of the Pro12Ala mutation of PPARγ2 receptor gene clinical character in metabolic syndrome. J. Clin. Intern. Med. 22, 50–52 [Google Scholar]
- 26.Pan H.J., Guo Y.Y., Wang K., Zhao L. and He B.X. (2007) Additive effects of the variants in the β 3 -AR and PPAR - γ2 genes on essential hypertension in Xinjiang kazakh population. Chin. J. Birth Heal Heredity 15, 19–21 [Google Scholar]
- 27.Hui P., Nakayama T., Morita A., Sato N., Hishiki M., Saito K.. et al. (2007) Common single nucleotide polymorphisms in Japanese patients with essential hypertension: aldehyde dehydrogenase 2 gene as a risk factor independent of alcohol consumption. Hypertens. Res. 30, 585–592 10.1291/hypres.30.585 [DOI] [PubMed] [Google Scholar]
- 28.Lu Z., Dong B., Mo X., Chen T., Wu H., Zhang Y.. et al. (2008) Pro12Ala polymorphism in PPAR γ 2 associated with essential hypertension in Chinese nonagenarians/centenarians. Exp. Gerontol. 43, 1108–1113 10.1016/j.exger.2008.08.046 [DOI] [PubMed] [Google Scholar]
- 29.Gu S.J., Guo Z.R., Wu M., Ding Y. and Luo W.S. (2013) Association of peroxisome proliferator-activated receptor γ polymorphisms and haplotypes with essential hypertension. Genet. Test Mol. Biomarkers 17, 418–423 10.1089/gtmb.2012.0425 [DOI] [PubMed] [Google Scholar]
- 30.Chen J., Zhang M., Liu J.M., Ma R.L., Guo H., Niu Q.. et al. (2014) Association of PPARγ gene polymorphism with hypertension in Xinjiang Uygur. J. Prac. Med. 30, 2922–2925 [Google Scholar]
- 31.Wang G., Xu P., Feng W., Jiang X., Zhang T. and Li J. (2015) Case-control study on peroxisome proliferator-activated receptor γ polymorphism and interaction with HDL on essential hypertension in Chinese Han. Iran J. Basic Med. Sci. 18, 1228–1232 [PMC free article] [PubMed] [Google Scholar]
- 32.Wang Y. and Liu C. (2012) Quantitative evaluation of common polymorphism (rs1801282) in the PPARγ2 gene and hypertension susceptibility. Gene 502, 159–162 10.1016/j.gene.2012.04.035 [DOI] [PubMed] [Google Scholar]
- 33.Shen W., Zhang T., Li S., Zhang H., Xi B., Shen H.. et al. (2017) Race and sex differences of long-term blood pressure profiles from childhood and adult hypertension: the Bogalusa Heart Study. Hypertension 70, 66–74 10.1161/HYPERTENSIONAHA.117.09537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao S.M., Shen L.H., Li H.W., Wang L., Chen H., Wang Y.L.. et al. (2008) Down-regulation of the expression of angiotensin II type 1 receptor in neonatal rat cardiac fibroblast by activation of PPARγ signal pathway. Chin. J. Physiol. 51, 357–362 [PubMed] [Google Scholar]
- 35.Diep Q.N., El M.M., Cohn J.S., Endemann D., Amiri F., Virdis A.. et al. (2002) Structure, endothelial function, cell growth, and inflammation in blood vessels of angiotensin II-infused rats: role of peroxisome proliferator-activated receptor-γ. Circulation 105, 2296–2302 10.1161/01.CIR.0000016049.86468.23 [DOI] [PubMed] [Google Scholar]
- 36.Jain A. and Anand-Srivastava M.B. (2018) Natriuretic peptide receptor-C-mediated attenuation of vascular smooth muscle cell hypertrophy involves Gqalpha/PLCbeta1 proteins and ROS-associated signaling. Pharmacol. Res. Perspect. 6, e00375 10.1002/prp2.375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Park B.C., Thapa D., Lee J.S., Park S.Y. and Kim J.A. (2009) Troglitazone inhibits vascular endothelial growth factor-induced angiogenic signaling via suppression of reactive oxygen species production and extracellular signal-regulated kinase phosphorylation in endothelial cells. J. Pharmacol. Sci. 111, 1–12 10.1254/jphs.08305FP [DOI] [PubMed] [Google Scholar]