Abstract
Introduction
Secukinumab is a fully human anti-interleukin 17A monoclonal antibody approved for the treatment of psoriatic arthritis (PsA) in the United States. Few studies have investigated prescribing patterns among rheumatologists who have initiated secukinumab for the treatment of patients with PsA in real-world settings. This US medical chart review describes clinical and treatment characteristics of patients with psoriatic arthritis (PsA) who were prescribed secukinumab and rheumatologist-reported reasons for prescribing secukinumab in clinical practice.
Methods
This US medical chart review included patients with physician-diagnosed PsA aged ≥ 18 years initiating secukinumab after January 15, 2016. Eligible rheumatologists used online forms to collect patient demographics, disease characteristics, comorbidity profiles, and treatment histories before or on the date of the first secukinumab prescription recorded in the medical chart. Information on reasons for secukinumab prescription and dosing was also collected.
Results
Medical charts from 153 patients with PsA who initiated secukinumab were reviewed by 46 rheumatologists between July 7, 2017, and August 11, 2017. Overall, 53.6% of patients were male, mean (standard deviation) age was 47.3 (11.5) years, and 24.8% were biologic naive. The most common reasons for secukinumab prescription among biologic-naive and biologic-experienced patients, respectively, were efficacy/effectiveness of secukinumab (84.2%) and failure of other prior biologics (80.9%). Nearly all patients (94.1%) received a loading regimen, including 150 mg every week (32.7%) and 300 mg every week (61.4%). Overall, 145 patients (94.8%) received ≥ 1 maintenance dose, of whom 49.7% received 150 mg every 4 weeks and 50.3% received 300 mg every 4 weeks.
Conclusions
At the time of the chart review, most patients with PsA who initiated secukinumab were biologic experienced, although one-quarter received secukinumab as first-line biologic therapy. Efficacy/effectiveness of secukinumab and failure of other biologics were the most common reasons for initiating secukinumab.
Funding
Novartis Pharmaceuticals Corporation, East Hanover, NJ.
Plain Language Summary
Plain language summary available for this article.
Keywords: Biologicals, Epidemiology, Psoriatic arthritis, Spondylarthropathies
Plain Language Summary
Psoriatic arthritis (PsA) is a chronic inflammatory condition that may involve the nails and skin, peripheral joints, enthesitis, dactylitis, and/or axial disease, either alone or in combination. The goals of therapy for all patients with PsA are to achieve the lowest possible level of disease activity in all domains of disease. Switching biologic therapies can be an effective strategy for many patients whose disease does not respond to their initial biologic; however, therapies with novel mechanisms of action provide patients and physicians with additional options for managing the disease. Secukinumab is a fully human anti-interleukin (IL)-17A monoclonal antibody, and in January 2016, it became the first IL-17A inhibitor approved for the treatment of PsA in the United States. A limited number of studies have investigated prescribing patterns and reasons for initiation among rheumatologists who have initiated secukinumab for the treatment of patients with PsA in real-world settings.
In this retrospective chart review of 153 patients who initiated secukinumab for the treatment of PsA in US clinical practice, nearly all patients (90.8%) had rheumatologist-assessed moderate or severe PsA; and approximately 80% of patients were biologic experienced. The most frequently cited reasons for secukinumab initiation among rheumatologists treating patients with PsA were its efficacy/effectiveness, failure of other biologics, and its status as a newly available agent with a new mechanism of action. These findings are among the first data to highlight characteristics of patients with PsA who initiate secukinumab in real-world clinical practice and may help inform treatment decisions for rheumatologists.
Introduction
Psoriatic arthritis (PsA) is a chronic inflammatory arthritis involving the skin and musculoskeletal system that affects approximately 6–41% of patients with psoriasis, with an estimated prevalence of 0.25% in the United States [1, 2]. PsA is a heterogenous condition associated with nail and skin changes, peripheral joint inflammation, enthesitis, dactylitis, and/or axial involvement, along with additional comorbidities that impact clinical burden and complicate disease management [3, 4].
The Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) and the European League Against Rheumatism (EULAR) have developed guidelines for the treatment and management of patients with PsA [5, 6]. The goals of therapy for all patients with PsA are to achieve the lowest possible level of disease activity in all domains of disease (peripheral arthritis, spondylitis/axial disease, enthesitis, dactylitis, skin disease, nail disease); to optimize functional status, improve quality of life and well-being, and prevent structural damage to the greatest extent possible; and to avoid or minimize complications, both from untreated active disease and from therapy [5]. For patients with moderate-to-severe PsA, or for patients whose disease remains active despite traditional therapies, conventional synthetic disease-modifying antirheumatic drugs (DMARDs), biologic therapies, or targeted synthetic DMARDs are recommended. Switching biologic therapies can be an effective strategy for many patients whose disease does not respond to their initial biologic; however, switching to therapies with different mechanisms of action may be associated with better outcomes than cycling between therapies within the same class [e.g., subsequent lines of tumor necrosis factor inhibitors (TNFis)], but more research is needed to compare these responses [7, 8]. Therapies with novel mechanisms of action provide patients and physicians with additional options for managing the disease. Indeed, the biologic landscape for the treatment of PsA has seen tremendous growth since early 2013, when only TNFis were available in the United States. Within the last 5 years, several non-TNFi biologics and targeted synthetic DMARDs have been approved by the US Food and Drug Administration for the treatment of PsA, including monoclonal antibodies targeting interleukin (IL) 12/23 [9, 10] and IL-17A [11–14], a selective T cell costimulation modulator [15, 16], an oral phosphodiesterase 4 inhibitor [17–19], and an oral Janus kinase inhibitor [20, 21].
Secukinumab is a fully human anti–IL-17A monoclonal antibody, and in January 2016, it became the first IL-17A inhibitor approved for the treatment of PsA in the United States. Studies examining physicians’ reasons for why or how a treatment is prescribed would make available valuable information to help navigate complex treatment algorithms or decision trees. However, a limited number of studies have investigated prescribing patterns among rheumatologists who have initiated secukinumab for the treatment of patients with PsA in real-world settings.
The objectives of this descriptive analysis were to characterize clinical and treatment profiles of patients with PsA who were prescribed secukinumab treatment in US clinical practice and to evaluate rheumatologist-reported reasons for prescribing secukinumab.
Methods
Data Source and Study Design
This was a retrospective medical chart review of patients in the United States diagnosed with PsA aged ≥ 18 years who initiated secukinumab after its approval date, January 15, 2016. Rheumatologists from an existing physician panel across various practice settings and regions in the United States were screened on the basis of the following eligibility criteria: (1) completed their residency and fellowship training, (2) treated ≥ 1 patient with PsA in the past 12 months prior to the chart review, and (3) had prescribed secukinumab for the treatment of PsA. Eligible rheumatologists were then invited to provide patient information using an online chart abstraction form.
This study was designed and implemented in accordance with the Guidelines for Good Pharmacoepidemiology Practices of the International Society for Pharmacoepidemiology, the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines, and the ethical principles laid down in the Declaration of Helsinki [22, 23]. An institutional review board exemption was obtained for the study prior to initiation of data collection.
Study Population
Eligible patients were required to meet the following criteria: (1) physician diagnosis of PsA; (2) prescription of secukinumab for the treatment of PsA by participating rheumatologists in a real-world setting (i.e., outside an interventional clinical trial) on or after January 15, 2016; (3) age ≥ 18 years at the time of secukinumab initiation; and (4) medical records containing information on PsA diagnosis, comorbidities, and treatment history prior to the secukinumab initiation that were accessible to the participating rheumatologists.
Measures and Outcomes
The chart abstraction form was used to collect patient-level information extracted by rheumatologists from eligible patients’ medical charts, such as demographics (age, sex, race, and insurance type), disease characteristics (disease duration, physician-assessed disease severity, PsA symptoms experienced, and comorbidities), treatment history (previous treatments and reasons for discontinuation of treatment immediately preceding secukinumab), and characteristics of secukinumab use [duration of treatment, dosing, current secukinumab treatment status, rheumatologist-reported reasons for secukinumab prescription, and reasons for secukinumab discontinuation (if applicable)].
Data Analysis
Descriptive analyses were conducted for all patient demographics, disease characteristics, treatment history, and characteristics of secukinumab use, as well as for physician-level characteristics. Rheumatologist-reported reasons for secukinumab prescription were also described for patients stratified by use of prior biologics. Categorical variables were summarized using frequency counts and percentages. Continuous variables were summarized by means and standard deviations (SDs) or medians and interquartile ranges. All data analyses were conducted using SAS, version 9.4 (SAS Institute).
Results
Rheumatologist Characteristics
Medical charts from 153 patients with PsA who initiated secukinumab were reviewed by 46 rheumatologists between July 7, 2017, and August 11, 2017. Participating rheumatologists contributed a mean (SD) of 3.3 (1.6) PsA patient medical charts to the analysis. Characteristics of the participating rheumatologists are presented in Table 1. Overall, the rheumatologists had been in practice for a mean (SD) of 14.2 (9.5) years; 73.9% were from a private practice setting, and 41.3% were from the Northeast region of the United States. Most rheumatologists (78.3%) referenced published international treatment guidelines to assist with PsA diagnosis (i.e., GRAPPA and/or EULAR).
Table 1.
Characteristics of rheumatologists participating in the medical chart review of patients with PsA (N = 46)
| Characteristics | Rheumatologists (N = 46) |
|---|---|
| Age, mean (SD), years | 48.0 (11.2) |
| Male, n (%) | 33 (71.7) |
| Type of practice, n (%) | |
| Private practicea | 34 (73.9) |
| Academic institution | 11 (23.9) |
| Region of practice, n (%) | |
| Northeast | 19 (41.3) |
| Midwest | 8 (17.4) |
| South | 10 (21.7) |
| West | 9 (19.6) |
| Years in practice, mean (SD) | 14.2 (9.5) |
| Total patients with PsA seen in the past year, mean (SD)b | 208.1 (140.2) |
| No. of medical charts of patients with PsA contributed by physician, mean (SD) | 3.3 (1.6) |
| PsA treatment guidelines referenced, n (%)c | |
| GRAPPA | 25 (54.3) |
| EULAR | 21 (45.7) |
| GRAPPA and EULAR | 11 (23.9) |
| Otherd | 1 (2.2) |
| No guidelines | 10 (21.7) |
ACR American College of Rheumatology; CASPAR Classification Criteria for Psoriatic Arthritis; EULAR European League Against Rheumatism; GRAPPA Group for Research and Assessment of Psoriasis and Psoriatic Arthritis; PsA psoriatic arthritis; SD standard deviation
aThe proportions of solo, single-specialty group, multispecialty group, and hospital-owned practices were calculated among physicians in a private practice
bThe chart abstraction form collected the number of patients with PsA the responding physician has personally seen in the last 12 months prior to questionnaire completion. This question included a maximum range of 500 patients. After removing the outliers (i.e., trimming at 5%; the highest 5% of the data were excluded), the mean number of patients was 187.7 patients. Some physicians may have reported the number of visits rather than the number of patients or may have been subject to recall bias, leading to a higher number of patients than expected
cMultiple guidelines could have been selected by a single physician except when “no guidelines” was selected
dOther psoriatic arthritis treatment guidelines included “ACR”
Patient Demographic and Disease Characteristics at the Time of Secukinumab Initiation
Among the 153 patients with PsA whose charts were reviewed, 53.6% were male, and the mean (SD) age was 47.3 (11.5) years (Table 2). At the time of secukinumab initiation, 15.0% of patients had a disease duration of > 10 years, and 28.1% of patients had severe rheumatologist-assessed PsA disease severity. The most common symptoms at the time of secukinumab initiation were joint pain and swelling (90.8%), stiffness (87.6%), skin rashes (73.9%), and enthesitis (46.4%). Nearly three-quarters of patients (74.5%) experienced comorbidities (Table 3); the most common comorbidities were psoriasis (41.2%), hypertension (28.8%), and hyperlipidemia (19.6%).
Table 2.
Demographic and disease characteristics at the time of secukinumab initiation of patients with PsA (N = 153)
| Characteristic | Patients with PsA (N = 153) |
|---|---|
| Age, mean (SD), years | 47.3 (11.5) |
| Male, n (%) | 82 (53.6) |
| Race/ethnicity, n (%) | |
| White/non-Hispanic | 115 (75.2) |
| Hispanic | 19 (12.4) |
| Black/non-Hispanic | 10 (6.5) |
| Asian/Pacific Islander | 9 (5.9) |
| Insurance type, n (%) | |
| Commercial/private | 115 (75.2) |
| Medicare | 17 (11.1) |
| Medicaid | 17 (11.1) |
| Military | 5 (3.3) |
| Unknown/not sure | 3 (2.0) |
| Duration of PsA, n (%) | |
| < 1 year | 10 (6.5) |
| 1–2 years | 39 (25.5) |
| 3–5 years | 46 (30.1) |
| 6–10 years | 35 (22.9) |
| 11–15 years | 17 (11.1) |
| > 15 years | 6 (3.9) |
| Physician-assessed disease severity, n (%) | |
| Mild | 14 (9.2) |
| Moderate | 96 (62.7) |
| Severe | 43 (28.1) |
| PsA symptoms experienced, n (%)a | 150 (98.0) |
| Joint pain and swelling | 139 (90.8) |
| Stiffness | 134 (87.6) |
| Skin rashes | 113 (73.9) |
| Enthesitis | 71 (46.4) |
| Nail changes | 71 (46.4) |
| Fatigue | 70 (45.8) |
| Dactylitis | 57 (37.3) |
| Reduced range of motion | 56 (36.6) |
| Inflammatory eye disease | 6 (3.9) |
| Otherb | 3 (2.0) |
PsA psoriatic arthritis; SD standard deviation
aMultiple PsA symptoms could be selected for each patient except when “none of the above” was selected
bOther symptoms included “impaired activities of daily living and job performance (carpenter),” “could not hold eating utensils because of arthritis,” and “impaired activities of daily living (works as a chef).”
Table 3.
Comorbidity profile at the time of secukinumab initiation of patients with PsA (N = 153)
| Comorbidities, n (%)a | Patients with PsA (N = 153) |
|---|---|
| Psoriasis | 63 (41.2) |
| Hypertension | 44 (28.8) |
| Hyperlipidemia | 30 (19.6) |
| Digestive disorders | 28 (18.3) |
| Depression | 24 (15.7) |
| Anemia | 22 (14.4) |
| Anxiety | 20 (13.1) |
| Diabetes | 15 (9.8) |
| Inflammatory eye diseases (e.g., uveitis) | 6 (3.9) |
| Ulcerative colitis | 4 (2.6) |
| Crohn’s disease | 3 (2.0) |
| Malignancyb | 1 (0.7) |
PsA psoriatic arthritis
aIncludes comorbidities with prevalence > 10% and additional selected comorbidities. Multiple comorbidities could be selected for each patient except if “none of the above” was selected
bMalignancy included “multiple squamous cell skin cancer.”
PsA Treatment History
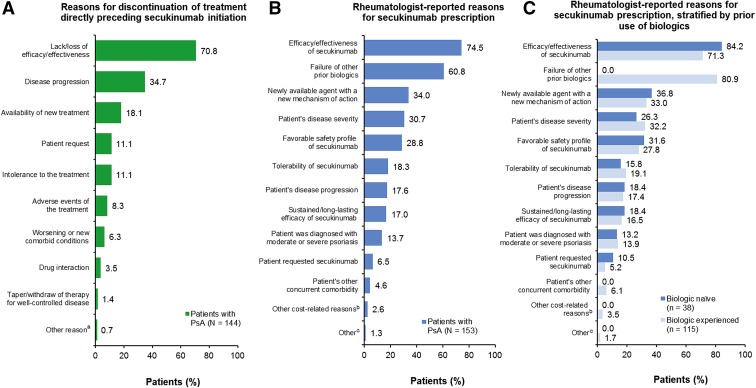
Of the 153 patients with PsA who initiated secukinumab, nearly all [144 (94.1%)] received prior PsA treatments, and nine patients (5.9%) received secukinumab as their first PsA treatment (Table 4). Of the 144 patients who received prior treatment, 115 (79.9%) received ≥ 1 biologic at any time prior to secukinumab initiation [mean (SD) number of prior biologics, 1.2 (1.0)], including 15 patients (10.4%) who received ≥ 3 prior biologics; adalimumab (47.2%), etanercept (42.4%), and infliximab (17.4%) were the most common biologics used at any time prior to secukinumab. A total of 38 patients (24.8% of 153) were biologic naive at secukinumab initiation. The most commonly used classes of treatments directly preceding secukinumab were any biologics (65.3%), conventional synthetic DMARDs (43.1%), and nonsteroidal anti-inflammatory drugs (NSAIDs) (33.3%). The most common reasons for discontinuation of treatment directly preceding secukinumab initiation were lack/loss of efficacy/effectiveness (70.8%), disease progression (34.7%), and availability of new treatment (18.1%) (Fig. 1a).
Table 4.
Treatment history of patients with PsA (N = 153)
| Characteristics | Patients with PsA (N = 153) |
|---|---|
| Received secukinumab as first treatment, n (%) | 9 (5.9) |
| Received treatment prior to secukinumab, n (%) | 144 (94.1) |
| Treatments received at any time prior to secukinumaba,b | |
| Mean (SD) | 2.7 (1.8) |
| 1, n (%) | 31 (21.5) |
| 2, n (%) | 42 (29.2) |
| ≥ 3, n (%) | 71 (49.3) |
| Any biologics, n (%) | 115 (79.9) |
| Mean (SD) | 1.2 (1.0) |
| 1, n (%) | 65 (45.1) |
| 2, n (%) | 35 (24.3) |
| ≥ 3, n (%) | 15 (10.4) |
| Conventional synthetic DMARDs, n (%) | 101 (70.1) |
| NSAIDs, n (%) | 66 (45.8) |
| Targeted synthetic DMARDs (apremilast), n (%) | 14 (9.7) |
| Treatments directly preceding secukinumab, n (%)a,b | |
| Any biologics | 94 (65.3) |
| Conventional synthetic DMARDs | 62 (43.1) |
| NSAIDs | 48 (33.3) |
| Targeted synthetic DMARDs (apremilast) | 7 (4.9) |
DMARD disease-modifying antirheumatic drug; NSAID nonsteroidal anti-inflammatory drug; PsA psoriatic arthritis; SD standard deviation
aAmong patients who had received ≥ 1 treatment prior to secukinumab (n = 144). The number of all previous distinct treatments was considered, regardless of treatment combinations
bMultiple treatments directly preceding secukinumab could be selected for each patient
Fig. 1.
A Reasons for discontinuation of treatment directly preceding secukinumab initiation among patients with PsA who received treatment prior to secukinumab (N = 144); rheumatologist-reported reasons for secukinumab prescription in B all patients with PsA (N = 153) and C stratified by use of prior biologics (N = 153).
PsA psoriatic arthritis.
aOther reason included “patient did not absorb methotrexate tabs”.
bOther cost-related reasons included “availability of samples and Novartis assistance,” “availability of samples,” “Novartis support and samples availability,” and “samples availability”.
cOther reasons included “job as a chef threatened by arthritis” and “patient and family preferred an injectable”
Rheumatologist-Reported Reasons for Prescription of Secukinumab and Characteristics of Secukinumab Use
The most common rheumatologist-reported reasons for secukinumab prescription included efficacy/effectiveness of secukinumab (74.5%), failure of other prior biologics (60.8%), and newly available agent with a new mechanism of action (34.0%) (Fig. 1b). When patients were stratified by use of prior biologics, efficacy/effectiveness of secukinumab (84.2%) remained the most common reason for secukinumab prescription among biologic-naive patients, followed by newly available agent with a new mechanism of action (36.8%), and favorable safety profile of secukinumab (31.6%). Failure of other prior biologics (80.9%) and efficacy/effectiveness of secukinumab (71.3%) were the most common reasons for secukinumab prescription among biologic-experienced patients (Fig. 1c).
At the time of chart abstraction, patients had received secukinumab for a mean (SD) duration of 5.9 (4.6) months (Table 5). Nearly one-third of patients with PsA (32.7%) received a loading regimen using a dose of 150 mg every week, while 61.4% received a loading regimen using a dose of 300 mg every week, and 5.9% did not receive a loading regimen. Of the 145 patients who received an initial maintenance dose, approximately one-half (49.7%) received an initial maintenance dose of 150 mg every 4 weeks, while the remaining 50.3% received an initial maintenance dose of 300 mg every 4 weeks. The majority of patients (90.2%) were still receiving secukinumab at the time of chart abstraction, while nine patients (5.9%) had discontinued treatment, and six patients (3.9%) had an unknown treatment status. Of the nine patients who discontinued treatment, reasons for discontinuation included lack/loss of efficacy/effectiveness (n = 5), intolerance to the treatment (n = 2), adverse events from the treatment (n = 2), and worsening or new comorbid condition (n = 1).
Table 5.
Characteristics of secukinumab use among patients with PsA (N = 153)
| Characteristic | Patients with PsA (N = 153) |
|---|---|
| Duration of treatment with secukinumab, mean (SD), monthsa | 5.9 (4.6) |
| Dose | |
| Received loading regimen, n (%) | 144 (94.1) |
| 150 mg every weekb | 50 (32.7) |
| 300 mg every weekc | 94 (61.4) |
| No loading regimen | 9 (5.9) |
| Received maintenance dose, n (%) | 145 (94.8) |
| Initial maintenance dosed | |
| 150 mg every 4 weeks | 72 (49.7) |
| 300 mg every 4 weeks | 73 (50.3) |
| Current secukinumab use, n (%) | |
| Still receiving secukinumab | 138 (90.2) |
| Discontinued secukinumab | 9 (5.9) |
| Reason for secukinumab discontinuation, n (%)e | |
| Lack/loss of efficacy/effectiveness | 5 (55.6) |
| Intolerance to the treatment | 2 (22.2) |
| Adverse events from the treatment | 2 (22.2) |
| Worsening or new comorbid condition | 1 (11.1) |
| Unknown secukinumab treatment status | 6 (3.9) |
PsA psoriatic arthritis; SD standard deviation
aDuration of treatment with secukinumab was calculated among all patients; the calculated duration may underestimate the true duration because most patients were still receiving secukinumab at the time of chart abstraction
bAmong the 50 patients who initiated secukinumab at 150 mg every week, 43 received an initial maintenance dose of 150 mg every 4 weeks, 6 received 300 mg every 4 weeks, and 1 did not receive maintenance treatment
cAmong the 94 patients who initiated secukinumab at 300 mg every week, 25 received an initial maintenance dose of 150 mg every 4 weeks, 63 received 300 mg every 4 weeks, 2 did not receive maintenance treatment, and 4 did not remain on the therapy long enough to receive maintenance treatment
dThe proportions of initial maintenance doses were calculated among patients who received a maintenance dose
eThe proportions of reasons for discontinuation were calculated among patients who discontinued secukinumab. Multiple reasons could be selected for each patient
Discussion
In this medical chart review of patients with PsA who initiated secukinumab in clinical practice, nearly all patients had moderate or severe rheumatologist-reported PsA disease severity, and psoriasis was the most common comorbid condition noted at the time of secukinumab initiation, reported in approximately 40% of patients. Additionally, nearly two-thirds of patients received secukinumab as their first or second biologic, including approximately 25% of patients for whom secukinumab was their first biologic, which suggests that rheumatologists may be considering secukinumab early in the biologic treatment algorithm for PsA. Patients in this study were mostly similar in terms of age, sex, race, PsA disease duration, and presence of psoriasis compared with those enrolled in phase III clinical trials of secukinumab [13, 14, 24]. Patients enrolled in clinical trials met the Classification Criteria for Psoriatic Arthritis (CASPAR) and had active disease, defined as having ≥ 3 tender joints and ≥ 3 swollen joints, despite previous treatment with NSAIDs, DMARDs, or TNFis [13, 14]. Although there were no such tender or swollen joint requirements for inclusion in the current study, > 90% of patients included in the chart review reported joint pain and swelling, which may be a surrogate for increased tender and swollen joint counts.
In the phase III randomized controlled trials, approximately 65–70% of patients were TNFi-naive, which differed from our chart review, in which one-quarter of patients were biologic naive at the time of secukinumab initiation [13, 14, 24]. Additionally, the rates of enthesitis and dactylitis in our study (46.4 and 37.3%, respectively) were on the lower end of what was reported in randomized controlled trials (range 46.0–64.1% and 36.9–56.0%, respectively), possibly due to the lack of evaluation by rheumatologists or the lack of a washout period in real-world studies that is typically carried out in clinical trial settings. Despite similarities in patient characteristics between populations in clinical trials and in real-world clinical practice, comparison of disease severity across both treatment settings may be challenging due to data availability and differences in inclusion criteria. Patients enrolled in clinical trials are rigorously monitored and often have regular clinical visits in accordance with study protocols, whereas patients treated in real-world clinical practice settings may have fewer visits or visits at irregular intervals. In addition, clinical trial populations often do not represent real-world heterogeneity with regard to features such as ethnicity, age, differences in disease severity, and comorbidities. Accordingly, data obtained from real-world studies may provide insight into characteristics of more diverse patient populations.
Our study also provides information on characteristics of the rheumatologists who prescribed secukinumab to patients with PsA in clinical practice based on a short screening section of the chart abstraction form. There are limited data describing rheumatologists who treat patients with PsA in the United States, let alone data focusing only on rheumatologists who have experience with secukinumab [25, 26]. The rheumatologists participating in this chart review were primarily from private practice, with approximately 15 years of experience treating PsA.
The most common prescriber reasons for initiating secukinumab among patients with PsA in this study were its efficacy/effectiveness, failure of other biologics, and its status as a newly available agent with a new mechanism of action. Because PsA is a heterogenous disease that can affect one or more domains of disease (i.e., peripheral arthritis, spondylitis/axial disease, enthesitis, dactylitis, skin disease, and nail disease), it is important to consider the efficacy/effectiveness of the treatment agents in the disease domains affecting the patient. Rheumatologists in our study may have considered prescribing secukinumab because there are high proportions of patients in this study with symptoms reflecting impairment in different disease domains, and secukinumab has shown efficacy across all PsA disease domains [13, 14, 24, 27]. For instance, a diagnosis of moderate or severe psoriasis was reported as a prescriber reason for initiating secukinumab in approximately 14% of patients in this study. Additionally, more than 90% of patients included in the medical chart review had rheumatologist-assessed moderate or severe PsA disease severity, which may have contributed to the use of secukinumab earlier in treatment for some patients.
As with any retrospective chart review study, there are limitations of the study that should be considered when interpreting the results. The sample size was relatively small, which may preclude generalizability of the findings to larger patient populations in the United States; however, all regions of the United States were well represented by participating rheumatologists. Because of the small sample size, characteristics or events with a low prevalence may also not be estimated reliably. At the time of chart abstraction, approximately 90% of patients who initiated secukinumab had remained on therapy, but further longitudinal investigation is needed to document patient experiences and treatment outcomes. This study might have been affected by nonrandom missing data from the medical charts; for example, although information about comorbidities was collected by the chart review, the level of detail in the documentation may not have been consistent across medical charts. In addition, validated instruments that assess quantifiable measures of disease severity [e.g., the Composite Psoriatic Disease Activity Index (CPDAI), the Disease Activity Index for Psoriatic Arthritis (DAPSA), or achievement of minimal disease activity (MDA)] [28–30] or severity of patient-reported outcomes (e.g., the Psoriatic Arthritis Quality of Life (PsAQoL) questionnaire and the Psoriatic Arthritis Impact of Disease (PsAID) questionnaire] [31, 32], which are more relevant for clinical trials, are not often captured in clinical practice and are not reported in medical charts. Instead, assessments of disease severity and treatment effectiveness in real-world settings may be based on heterogeneous criteria from clinical opinion. Although our study captured the proportion of patients who experienced symptoms associated with PsA disease domains, additional studies with larger sample sizes that provide clarity on the number, type, and severity of disease domains affected in patients with PsA would help rheumatologists better understand which aspects of disease are most common among those patients treated with secukinumab. Finally, the choice of biologic and the decision of when to use secukinumab might have differed on the basis of the formulary of each payer/employer group. Despite these limitations, this study offers timely clinical data on patients with PsA who initiated secukinumab. Due to potential differences in patient characteristics between clinical trial settings and this real-world study, investigations into clinical outcomes and patient-reported experiences with duration of secukinumab use will provide additional insight into the real-world effectiveness of secukinumab.
Conclusions
Findings from this retrospective medical chart review provide information on the characteristics of patients with PsA who initiated secukinumab in US clinical practice. Most patients with PsA who initiated secukinumab were biologic experienced and had moderate-to-severe rheumatologist-reported PsA; efficacy/effectiveness of secukinumab, failure of other biologics, and desire to initiate a newly available agent with a new mechanism of action were the most common reasons for initiating secukinumab. These findings are among the first data to highlight characteristics of patients with PsA who initiate secukinumab in real-world clinical practice and may help inform treatment decisions for rheumatologists.
Acknowledgements
The authors thank all participants of this study.
Funding
This study was sponsored by Novartis Pharmaceuticals Corporation, East Hanover, NJ. Article processing charges were funded by Novartis Pharmaceuticals Corporation, East Hanover, NJ. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Medical Writing and Editorial Assistance
Support for third-party writing assistance, furnished by Eric Deutsch, PhD, CMPP, of Health Interactions, Inc, was provided by Novartis Pharmaceuticals Corporation, East Hanover, NJ.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, had full access to all of the data in this study, take complete responsibility for the integrity of the data and accuracy of the data analysis, and have given their approval for this version to be published.
Disclosures
Prashanth Sunkureddi has received speakers bureau fees from Novartis and is an investigator of a clinical trial sponsored by Novartis Pharmaceuticals Corporation. Dominick Latremouille-Viau is an employee of Analysis Group, Inc. Mark K. Meiselbach is an employee of Analysis Group, Inc. Jipan Xie is an employee of Analysis Group, Inc. Peter Hur is an employee of Novartis Pharmaceuticals Corporation. Reeti Joshi has received consulting fees from Novartis Pharmaceuticals Corporation.
Compliance with Ethics Guidelines
This study was designed and implemented in accordance with the Guidelines for Good Pharmacoepidemiology Practices of the International Society for Pharmacoepidemiology, the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines, and the ethical principles laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards [22, 23]. An institutional review board exemption was obtained for the study prior to initiation of data collection.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced digital features
To view enhanced digital features for this article go to 10.6084/m9.figshare.7473257.
References
- 1.Gelfand JM, Gladman DD, Mease PJ, Smith N, Margolis DJ, Nijsten T, et al. Epidemiology of psoriatic arthritis in the population of the United States. J Am Acad Dermatol. 2005;53:573. doi: 10.1016/j.jaad.2005.03.046. [DOI] [PubMed] [Google Scholar]
- 2.Ogdie A, Weiss P. The epidemiology of psoriatic arthritis. Rheum Dis Clin N Am. 2015;41:545–568. doi: 10.1016/j.rdc.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gladman DD. Clinical features and diagnostic considerations in psoriatic arthritis. Rheum Dis Clin N Am. 2015;41:569–579. doi: 10.1016/j.rdc.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 4.Lee S, Mendelsohn A, Sarnes E. The burden of psoriatic arthritis: a literature review from a global health systems perspective. Pharm Ther. 2010;35:680–689. [PMC free article] [PubMed] [Google Scholar]
- 5.Coates LC, Kavanaugh A, Mease PJ, Soriano ER, Laura Acosta-Felquer M, Armstrong AW, et al. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis 2015 treatment recommendations for psoriatic arthritis. Arthritis Rheumatol. 2016;68:1060–1071. doi: 10.1002/art.39573. [DOI] [PubMed] [Google Scholar]
- 6.Gossec L, Smolen JS, Ramiro S, de Wit M, Cutolo M, Dougados M, et al. European League Against Rheumatism (EULAR) recommendations for the management of psoriatic arthritis with pharmacological therapies: 2015 update. Ann Rheum Dis. 2016;75:499–510. doi: 10.1136/annrheumdis-2015-208337. [DOI] [PubMed] [Google Scholar]
- 7.Reddy SM, Crean S, Martin AL, Burns MD, Palmer JB. Real-world effectiveness of anti-TNF switching in psoriatic arthritis: a systematic review of the literature. Clin Rheumatol. 2016;35:2955–2966. doi: 10.1007/s10067-016-3425-4. [DOI] [PubMed] [Google Scholar]
- 8.Merola JF, Lockshin B, Mody EA. Switching biologics in the treatment of psoriatic arthritis. Semin Arthritis Rheum. 2017;47:29–37. doi: 10.1016/j.semarthrit.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 9.McInnes IB, Kavanaugh A, Gottlieb AB, Puig L, Rahman P, Ritchlin C, et al. Efficacy and safety of ustekinumab in patients with active psoriatic arthritis: 1 year results of the phase 3, multicentre, double-blind, placebo-controlled PSUMMIT 1 trial. Lancet. 2013;382:780–789. doi: 10.1016/S0140-6736(13)60594-2. [DOI] [PubMed] [Google Scholar]
- 10.Ritchlin C, Rahman P, Kavanaugh A, McInnes IB, Puig L, Li S, et al. Efficacy and safety of the anti-IL-12/23 p40 monoclonal antibody, ustekinumab, in patients with active psoriatic arthritis despite conventional non-biological and biological anti-tumour necrosis factor therapy: 6-month and 1-year results of the phase 3, multicentre, double-blind, placebo-controlled, randomised PSUMMIT 2 trial. Ann Rheum Dis. 2014;73:990–999. doi: 10.1136/annrheumdis-2013-204655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mease PJ, van der Heijde D, Ritchlin CT, Okada M, Cuchacovich RS, Shuler CL, et al. Ixekizumab, an interleukin-17A specific monoclonal antibody, for the treatment of biologic-naive patients with active psoriatic arthritis: results from the 24-week randomised, double-blind, placebo-controlled and active (adalimumab)-controlled period of the phase III trial SPIRIT-P1. Ann Rheum Dis. 2017;76:79–87. doi: 10.1136/annrheumdis-2016-209709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nash P, Kirkham B, Okada M, Rahman P, Combe B, Burmester GR, et al. Ixekizumab for the treatment of patients with active psoriatic arthritis and an inadequate response to tumour necrosis factor inhibitors: results from the 24-week randomised, double-blind, placebo-controlled period of the SPIRIT-P2 phase 3 trial. Lancet. 2017;389:2317–2327. doi: 10.1016/S0140-6736(17)31429-0. [DOI] [PubMed] [Google Scholar]
- 13.Mease PJ, McInnes IB, Kirkham B, Kavanaugh A, Rahman P, van der Heijde D, et al. Secukinumab inhibition of interleukin-17A in patients with psoriatic arthritis. N Engl J Med. 2015;373:1329–1339. doi: 10.1056/NEJMoa1412679. [DOI] [PubMed] [Google Scholar]
- 14.McInnes IB, Mease PJ, Kirkham B, Kavanaugh A, Ritchlin CT, Rahman P, et al. Secukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURE 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2015;386:1137–1146. doi: 10.1016/S0140-6736(15)61134-5. [DOI] [PubMed] [Google Scholar]
- 15.Mease P, Genovese MC, Gladstein G, Kivitz AJ, Ritchlin C, Tak PP, et al. Abatacept in the treatment of patients with psoriatic arthritis: results of a six-month, multicenter, randomized, double-blind, placebo-controlled, phase II trial. Arthritis Rheum. 2011;63:939–948. doi: 10.1002/art.30176. [DOI] [PubMed] [Google Scholar]
- 16.Mease PJ, Gottlieb AB, van der Heijde D, FitzGerald O, Johnsen A, Nys M, et al. Efficacy and safety of abatacept, a T-cell modulator, in a randomised, double-blind, placebo-controlled, phase III study in psoriatic arthritis. Ann Rheum Dis. 2017;76:1550–1558. doi: 10.1136/annrheumdis-2016-210724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kavanaugh A, Mease PJ, Gomez-Reino JJ, Adebajo AO, Wollenhaupt J, Gladman DD, et al. Treatment of psoriatic arthritis in a phase 3 randomised, placebo-controlled trial with apremilast, an oral phosphodiesterase 4 inhibitor. Ann Rheum Dis. 2014;73:1020–1026. doi: 10.1136/annrheumdis-2013-205056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cutolo M, Myerson GE, Fleischmann RM, Liote F, Diaz-Gonzalez F, Van den Bosch F, et al. A phase III, randomized, controlled trial of apremilast in patients with psoriatic arthritis: results of the PALACE 2 trial. J Rheumatol. 2016;43:1724–1734. doi: 10.3899/jrheum.151376. [DOI] [PubMed] [Google Scholar]
- 19.Edwards CJ, Blanco FJ, Crowley J, Birbara CA, Jaworski J, Aelion J, et al. Apremilast, an oral phosphodiesterase 4 inhibitor, in patients with psoriatic arthritis and current skin involvement: a phase III, randomised, controlled trial (PALACE 3) Ann Rheum Dis. 2016;75:1065–1073. doi: 10.1136/annrheumdis-2015-207963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gladman D, Rigby W, Azevedo VF, Behrens F, Blanco R, Kaszuba A, et al. Tofacitinib for psoriatic arthritis in patients with an inadequate response to TNF inhibitors. N Engl J Med. 2017;377:1525–1536. doi: 10.1056/NEJMoa1615977. [DOI] [PubMed] [Google Scholar]
- 21.Mease P, Hall S, FitzGerald O, van der Heijde D, Merola JF, Avila-Zapata F, et al. Tofacitinib or adalimumab versus placebo for psoriatic arthritis. N Engl J Med. 2017;377:1537–1550. doi: 10.1056/NEJMoa1615975. [DOI] [PubMed] [Google Scholar]
- 22.ISPE Guidelines for good pharmacoepidemiology practices (GPP) Pharmacoepidemiol Drug Saf. 2008;17:200–208. doi: 10.1002/pds.1471. [DOI] [PubMed] [Google Scholar]
- 23.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 24.Mease P, van der Heijde D, Landewé R, Mpofu S, Rahman P, Tahir H, et al. Secukinumab improves active psoriatic arthritis symptoms and inhibits radiographic progression: primary results from the randomised, double-blind, phase III FUTURE 5 study. Ann Rheum Dis. 2018;77:890–897. doi: 10.1136/annrheumdis-2017-212687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lebwohl MG, Kavanaugh A, Armstrong AW, Van Voorhees AS. US perspectives in the management of psoriasis and psoriatic arthritis: patient and physician results from the population-based multinational assessment of psoriasis and psoriatic arthritis (MAPP) survey. Am J Clin Dermatol. 2016;17:87–97. doi: 10.1007/s40257-015-0169-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van de Kerkhof PC, Reich K, Kavanaugh A, Bachelez H, Barker J, Girolomoni G, et al. Physician perspectives in the management of psoriasis and psoriatic arthritis: results from the population-based multinational assessment of psoriasis and psoriatic arthritis survey. J Eur Acad Dermatol Venereol. 2015;29:2002–2010. doi: 10.1111/jdv.13150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strand V, Mease P, Gossec L, Elkayam O, van den Bosch F, Zuazo J, et al. Secukinumab improves patient-reported outcomes in subjects with active psoriatic arthritis: results from a randomised phase III trial (FUTURE 1) Ann Rheum Dis. 2017;76:203–207. doi: 10.1136/annrheumdis-2015-209055. [DOI] [PubMed] [Google Scholar]
- 28.Mumtaz A, Gallagher P, Kirby B, Waxman R, Coates LC, Veale JD, et al. Development of a preliminary composite disease activity index in psoriatic arthritis. Ann Rheum Dis. 2011;70:272–277. doi: 10.1136/ard.2010.129379. [DOI] [PubMed] [Google Scholar]
- 29.Schoels M, Aletaha D, Funovits J, Kavanaugh A, Baker D, Smolen JS. Application of the DAREA/DAPSA score for assessment of disease activity in psoriatic arthritis. Ann Rheum Dis. 2010;69:1441–1447. doi: 10.1136/ard.2009.122259. [DOI] [PubMed] [Google Scholar]
- 30.Coates LC, Fransen J, Helliwell PS. Defining minimal disease activity in psoriatic arthritis: a proposed objective target for treatment. Ann Rheum Dis. 2010;69:48–53. doi: 10.1136/ard.2008.102053. [DOI] [PubMed] [Google Scholar]
- 31.McKenna SP, Doward LC, Whalley D, Tennant A, Emery P, Veale DJ. Development of the PsAQoL: a quality of life instrument specific to psoriatic arthritis. Ann Rheum Dis. 2004;63:162–169. doi: 10.1136/ard.2003.006296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gossec L, de Wit M, Kiltz U, Braun J, Kalyoncu U, Scrivo R, et al. A patient-derived and patient-reported outcome measure for assessing psoriatic arthritis: elaboration and preliminary validation of the psoriatic arthritis impact of disease (PsAID) questionnaire, a 13-country EULAR initiative. Ann Rheum Dis. 2014;73:1012–1019. doi: 10.1136/annrheumdis-2014-205207. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.