Abstract
Objectives
Nerve-sparing radical hysterectomy has been implemented in order to reduce pelvic floor dysfunctions in women undergoing radical surgery for cervical cancer. Here, we aimed to investigate if the adoption of laparoscopic surgery impacts on patients' outcomes.
Methods
Data of consecutive patients affected by cervical cancer who had laparoscopic nerve-sparing radical hysterectomy were matched 1:1 with an historical cohort of patients undergoing open procedure. A propensity-score matched algorithm was applied.
Results
Thirty-five patients' pairs (70 patients: 35 undergoing laparoscopic vs. 35 undergoing open abdominal nerve-sparing radical hysterectomy) were included. Demographic and baseline oncologic characteristics were balanced between groups. Patients undergoing laparoscopic surgery had similar operative time than patients undergoing open abdominal procedures (249 [±91.5] vs. 223 [±65.0] minutes; p=0.066). Laparoscopic approach correlated with lower blood loss (30.5 [±11.0] vs. 190 [90.4] mL; p<0.001) and shorter hospital stay (3.2 [±1.2] vs. 5.4 [2.0] days; p=0.023). Patients undergoing laparoscopy experienced a lower 30-day pelvic floor dysfunction rate than patients having open surgery. Moreover, they experienced shorter recovery of bladder function than patients having open procedures (median, 7 vs. 9 days; p=0.004, log-rank test).
Conclusion
Laparoscopic approach resulted in a faster recovery of bladder function in comparison to open surgery for patients undergoing nerve-sparing radical hysterectomy.
Keywords: Uterine Cervical Neoplasms, Hysterectomy, Urination Disorders, Laparoscopy
INTRODUCTION
Although the massive implementation of primary and secondary prevention, cervical cancer (CC) still remains one of the most common cancer-related death among young women, even in the Western Countries. In the United States, more than 12,800 and 4,200 new diagnoses and deaths are estimated for the year 2017. CC represents the second most common cause of cancer-related death among women aged between 20 and 39 years [1].
Surgery or radiotherapy are useful in women affected by early stage disease; while chemo-radiation is the mainstay of treatment for women affected by locally-advanced cervical cancer (LACC) [2,3,4,5,6]. Growing evidences support that neoadjuvant chemotherapy followed by radical surgery might be considered a suitable treatment modality for patients affected by LACC, thus reducing long-term morbidity related to radiation therapy, especially in young women [2,3,4,5,6]. However, radical removal of the uterus is not without consequences, even in absence of surgery-related morbidity. In fact, the resection of the nervous fibers running into the tissue surrounding the uterus might related to the occurrence of pelvic floor dysfunctions impacting patients' quality of life. The introduction of nerve-sparing radical hysterectomy improved postoperative patients' outcomes, reducing voiding, sexual and rectal issues [7,8,9,10,11].
Moreover, in the recent years minimally invasive surgery has emerged for the treatment of several benign and malignant conditions, including CC [10,11,12,13]. Accumulating data from well conducted retrospective and prospective study underlined that minimally invasive surgery upholds long-term outcomes of open abdominal procedures, minimizing postoperative morbidity [14,15,16,17,18], but mature data on long-term safety of minimally invasive radical hysterectomy are lacking.
Unfortunately, only few investigations reported outcomes of minimally invasive nerve-sparing radical hysterectomy [14,15]. In fact, in most clinical practices this kind of challenging procedures are performed via traditional open surgery. However, the magnified view of the laparoscope provides a better visualization of the fibers running in the pelvic tissues, thus theoretically allowing a more precise preservation of the nerves. However, no studies evaluated this issue. Here, we sought to evaluate how the introduction of minimally invasive surgery impact on pelvic floor dysfunction of women undergoing nerve-sparing radical hysterectomy. Additionally, we sought to compare surgery-related results and long-term outcomes of minimally invasive surgery and open abdominal nerve-sparing radical hysterectomy.
MATERIALS AND METHODS
This is a retrospective comparison of prospective collected data of a series of consecutive CC patients undergoing MIS between August 2015 and February 2018. Institutional Review Board (IRB) was obtained. Preoperatively, all the patients give written informed consent for data collection for research purpose.
Inclusion criteria were: 1) age ≥18 years; 2) execution of type C1 (nerve-sparing) radical hysterectomy; and 3) at least 30 days of follow-up. Exclusion criteria were: 1) consent withdraw; 2) synchronous malignancies (<5 years). Staging system and architectural grade were reported in accord to the International Federation of Obstetrics and Gynecologists (FIGO) statements. The World Health Organization (WHO) taxonomy was used in order to classify histologic subtypes [6].
Patients affected by LACC were informed that neoadjuvant platinum-based chemotherapy followed by surgery represents an experimental option and those standard treatments for locally advanced CC consists in radiation plus platinum-based chemotherapy [3,4]. Preoperative workup included physical and gynecological examinations, chest and abdominal computed tomography (CT) scan and pelvic nuclear magnetic resonance imaging (MRI).
Selected patients with LACC were counseled about the role of neoadjuvant chemotherapy and surgery. Patients were thoroughly counseled about the different possible choices of treatment. In particular, in case of stage IB2-III disease, they were informed about concomitant chemo-radiation was indicated as standard treatment for LACC, and that neoadjuvant chemotherapy + surgery represented an experimental option. Neoadjuvant chemotherapy consisted in three cycles of platinum-based chemotherapy.
In our department, until the recent years, type C1 radical hysterectomies were performed via open surgery; while, from August 2015, after the acquisition of 3-dimensional (3D) laparoscopic technology, all type C1 radical hysterectomy were performed laparoscopically. In fact, in August 2015, we started a systematic implementation of laparoscopic radical hysterectomy and open abdominal procedures were performed only in selected cases. A detailed description of surgical technique and treatment's algorithm is presented elsewhere [15]. Briefly, radical hysterectomy refers to the excision of the uterus en bloc with the parametria (i.e., round, broad, cardinal, and uterosacral ligaments) and the upper one-third of the vagina. During type C1 radical hysterectomy the uterine artery was transected at its origin. Autonomic nerves were identified and the hypogastric plexus remains preserved. A 3D laparoscopic column (Karl Storz Endoskope, Tuttlingen, Germany) was used for all the procedures. The procedure was performed using a 4 ports technique (a 10-mm optical port was placed in the umbilicus and three 5-mm ancillary trocars were placed in the lower abdominal quadrants). A Clermont-Ferrant (Karl Storz, Tuttlingen, Germany) uterine manipulator was used. The utilization of 3D laparoscopic column allows more accurate identification of the anatomical structures and a more precise dissection in comparison to conventional laparoscopy [15].
During the study period, there were no significant differences in the facilities available for patient care. Other aspects of patient management unrelated to surgical approach remained consistent over time. Patients were catheterized with indwelling Foley catheter for 3 days. Moderate or severe de novo urinary incontinence and urinary retention (requiring re-catheterization) were defined as voiding dysfunctions. Operative times were recorded from the first skin incision to the last skin suture. Estimated blood loss was estimated from the contents of suction devices. Hospital stay was counted from the first postoperative day. Surgery-related complications were classified in intra and postoperative complications. Intra-operative complication included any event that affects patients during surgery. Postoperative complications were graded per the Accordion severity system [19]. For the purpose of this study, only severe (grade 3 or worse) complications occurring within 30 days were analyzed. Complications were recorded prospectively in a dedicated database. Additionally, in-hospital and follow-up medical records were reviewed. Historical controls were selected from an intuitional database containing data of all CC patients having type C1 radical hysterectomy. The database included patients treated from January 2000 to July 2015 and only patients treated between 2010 and 2015 were included in the current study.
Pelvic dysfunctions were classified in changes in voiding, and anorectal function that were not recovered at 30 days of follow-up. Regarding the evaluation of pelvic dysfunction we recorded all the occurrence of self-reported issue impacting on own patients' quality of life. Voiding dysfunctions included the occurrence of de novo urinary incontinence or urinary retention. Rectal dysfunctions included the occurrence of self-reported outlet constipation or dyschezia. Sexual dysfunctions included the self-reported occurrence of de novo dyspareunia. Criteria regarding adjuvant therapy administration and detailed description of follow-up protocols are reported elsewhere [15]
After the execution of neoadjuvant chemotherapy and radical hysterectomy, adjuvant treatments were on the basis of pathological results [15]. Follow-up evaluations were scheduled every 4 months for the first 2 years after surgery, every 6 months between 2- and 5-year after surgery and annually thereafter. Survival data were abstracted from a dedicated database prospectively up-dated on a regular basis. Rigorous efforts, including telephonic interviews, were done to improve quality of follow-up data.
1. Statistical methods
This is a retrospective comparison between two groups, thus possible allocation biases might impair the quality of the results reporting. Therefore, we performed a propensity-matched analysis. Propensity-matched comparison attempts to estimate the effect of a treatment by accounting for possible factors (e.g., constitutional variables) that predicts receiving the treatment, thus reducing possible selection biases. Propensity-matched comparison aims to reduce biases rising from different covariates. Propensity score was developed through multivariable logistic regression model. Age, body mass index, parity, histology, and stage of disease were included in the model. Patients undergoing laparoscopic type C1 radical hysterectomy were matched 1:1 to patients selected to a cohort of women undergoing open abdominal type C1 radical hysterectomy, using a caliper width ≤0.1 standard deviations (SDs) of the logit odds of the estimated propensity score. Detailed description of propensity matching is described elsewhere [20,21]. Basic descriptive statistics were used to describe the two populations (laparoscopic and open abdominal surgeries). Differences in categorical variables were analyzed using the Fisher exact test. Odds ratio (OR) and 95% confidence intervals (CIs) were calculated for each comparison. T-test and Mann-Whitney test were used to compare continuous variables as appropriate. Survival outcomes (disease-free and overall survivals) were estimated using Kaplan-Meier model. The log-rank test was used to compare the risk of developing recurrence and the risk of death between the two groups over the time. The p values <0.05 were considered statistically significant. Statistical analysis was performed with GraphPad Prism version 6.0 (GraphPad Software, San Diego, CA, USA) and IBM-Microsoft SPSS version 20.0 (SPSS Statistics; International Business Machines Corporation IBM, Armonk, NY, USA) for Mac.
RESULTS
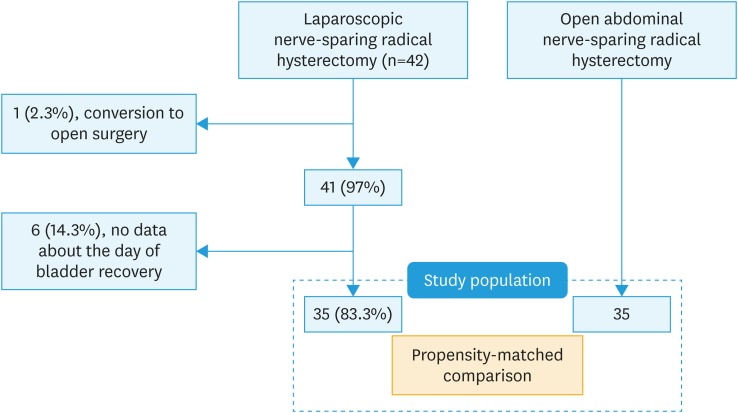
Over the study period, 42 patients had laparoscopic type C1 radical hysterectomy. One patient was excluded since she had conversion to open surgery. After the exclusion of six patients who had no data regarding 30-day pelvic floor dysfunction rates, 35 patients were included in the present analysis. Patients included in the study group was propensity-matched 1:1 with a control group of patients having open abdominal type C1 radical hysterectomy before the introduction of laparoscopic approach in our service. Fig. 1 shows the flow of patients through the study design.
Fig. 1. Study design.
Baseline characteristics of the study groups are presented in Table 1. According to the application of a propensity-matching algorithm, baseline characteristics were similar between groups.
Table 1. Baseline characteristics of patients undergoing nerve-sparing radical hysterectomy via laparoscopic and open abdominal surgery.
| Characteristics | Laparoscopy (n=35) | Open surgery (n=35) | p-value | |
|---|---|---|---|---|
| Age (yr) | 41.1 (±6.9) | 44.1 (±12.7) | 0.792 | |
| BMI (kg/m2) | 22.9 (±4.0) | 20.1 (±9.3) | 0.616 | |
| Charlson Comorbidity Index ≥1 (%) | 3 | 4 | 1.00 | |
| Parity | 1.3 (±1.2) | 1.3 (±0.8) | 0.739 | |
| Previous abdominal surgery | 7 (40) | 9 (35) | 0.776 | |
| Histotype | 1.00 | |||
| Squamous cell | 29 (82.9) | 29 (82.9) | ||
| Other | 6 (17.1) | 6 (17.1) | ||
| Stage of disease | 0.961 | |||
| IB1 | 3 (8.6) | 3 (8.6) | ||
| IB2 | 11 (31.4) | 10 (28.6) | ||
| IIA | 9 (25.7) | 11 (31.4) | ||
| IIB-III | 12 (34.3) | 11 (31.4) | ||
| Neoadjuvant chemotherapy | 1.000 | |||
| No | 5 (14.3) | 6 (17.1) | ||
| Yes | 30 (85.7) | 29 (82.9) | ||
| Adjuvant therapy | 1.000 | |||
| No | 25 (71.4) | 24 (68.6) | ||
| Yes | 10 (28.6) | 11 (31.4) | ||
| Follow-up (mon) | 11 (1, 32) | 49.5 (1, 91) | <0.001 | |
Data are presented as number (%), mean (±SD) or median (range).
BMI, body mass index; FIGO, International Federation of Obstetrics and Gynecologists; NACT, neoadjuvant chemotherapy; SD, standard deviation.
Looking at peri-operative results, we observed that patients undergoing laparoscopic surgery had similar operative time than patients undergoing open abdominal procedures (249 [±91.5] vs. 223 [±65.0] minutes; p=0.066). Laparoscopic approach correlated with lower blood loss (30.5 [±11.0] vs. 190 [±90.4] mL; p<0.001) and shorter hospital stay (3.2 [±1.2] vs. 5.4 [±2.0] days; p=0.023). Although patients in the study group had a lower transfusion rate than patients having open surgery, difference in transfusion rate did not reach statistical significance (0% vs. 14.2%; p=0.053). Intra-operative complication included: one vascular injury occurred and managed intraoperatively during open abdominal nerve-sparing radical hysterectomy. Severe postoperative complication rates were similar between cases and control (p=0.492). Two postoperative events occurred in the open abdominal group; they included: one ureteral fistula and haemoperitoneum requiring reoperation. No severe postoperative event was recorded in the study group. Table 2 reported details regarding operative outcomes. Considering pelvic floor dysfunctions rate, we observed that patients undergoing laparoscopy experienced a lower 30-day pelvic floor dysfunction rate than patients having open surgery (Table 3). Patients having laparoscopy had a trend toward lower 30-day voiding dysfunction rate in comparison to patients having open procedures (0% vs. 14.2%; p=0.053).
Table 2. Operative results of patients undergoing nerve-sparing radical hysterectomy via laparoscopic and open abdominal surgery.
| Characteristics | Laparoscopy (n=35) | Open surgery (n=35) | p-value |
|---|---|---|---|
| Operative time (min) | 249.4 (± 91.5) | 223.0 (± 65.0) | 0.066 |
| Estimated blood loss (mL) | 30.5 (± 11.0) | 190.0 (± 90.4) | <0.001 |
| Blood transfusions | 0 | 5 (14.2) | 0.053 |
| Hospital stay (days) | 3.2 (± 1.2) | 5.4 (± 2.0) | 0.023 |
| Intraoperative complications | 0 | 1 (3.3) | 1.000 |
| 30-day severe postoperative complications, grade 3 or worse | 0 | 2 (5.7) | 0.492 |
Data are presented as number (%) or mean (±SD).
SD, standard deviation.
Table 3. Pelvic dysfunctions rate for patients undergoing nerve-sparing radical hysterectomy via laparoscopic and open abdominal surgery.
| Characteristics | Laparoscopy (n=35) | Open surgery (n=35) | p-value |
|---|---|---|---|
| Pelvic dysfunctions (not yet recovered at 30-day) | 0 | 6 (17.1) | 0.024 |
| Bladder dysfunctions at 30 days | 0 | 5 (14.2) | 0.053 |
| Anorectal dysfunctions at 30 days | 0 | 1 (3.3) | 1.000 |
Data are presented as number (%).
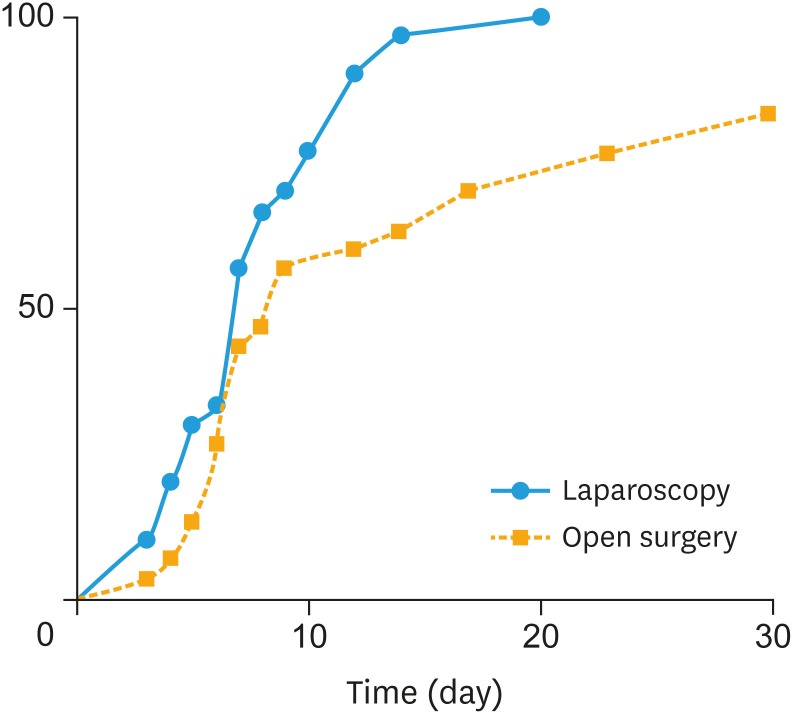
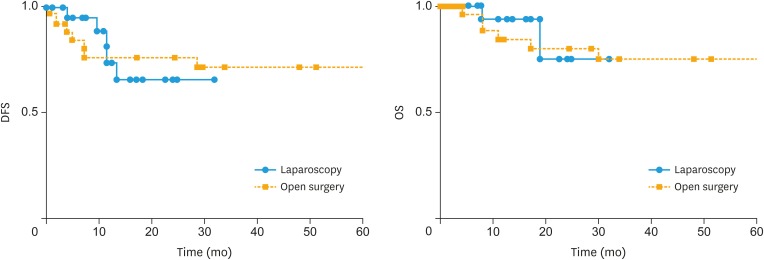
Patients undergoing laparoscopic surgery experienced shorter recovery of bladder function than patients having open procedures (median, 7 vs. 9 days). Fig. 2 shows time of bladder recovery according to surgical approach. As we observed in the curves, laparoscopic approach correlated in a faster recovery time (p=0.004, log-rank test). No voiding dysfunctions were recorded at 60-day in both groups. Survival rates were similar between the two techniques. After a median follow-up of 51.7 and 14.7 months for open abdominal and minimally invasive procedures, disease-free (p=0.617, log-rank test) and overall (p=0.814, log-rank test) survivals were similar between groups. They are reported in Fig. 3.
Fig. 2. Recovery of bladder function.
Fig. 3. Survival outcomes.
DISCUSSION
The present paper investigated peri-operative outcomes related to the execution of nerve-sparing radical hysterectomy executed via laparoscopic and open abdominal approach. We observed a number of noteworthy findings. First, patients undergoing laparoscopic approach experienced a lower pelvic floor dysfunction rate in comparison with open abdominal one. Second, in agreement with other studies we observed that patients having laparoscopic surgery had shorter hospital stay and blood loss than patients having open surgery. Interestingly however, we observed that laparoscopic approach did not increase operative time. Third, laparoscopic approach guaranteed similar oncologic results in comparison with conventional approach.
To date no other investigation focusing on pelvic floor dysfunction underlined that minimally invasive approach might improve patients' outcomes in comparison with conventional surgery. Although growing data support that minimally invasive surgery is safe and effective in CC patients, no other studies evaluated this issue. Moreover, we have to underline that researches on minimally invasive nerve-sparing radical hysterectomy are still scant. A recent systematic review and meta-analysis conducted by our study group (Prospero_CRD#57655) identified data of 325 patients treated with nerve-sparing minimally invasive radical hysterectomy [14]. Looking to single researches we observed that data about nerve-sparing minimally invasive radical hysterectomy are very limited. For instance, a recently published multi-institutional experience (involving 4 centers in Italy, including our unit) reported data of 47 procedures [6].
Accumulating evidence suggested that nerve-sparing approach improves outcomes of patients undergoing type C radical hysterectomy in the setting of both open abdominal and minimally invasive surgery. In comparison to standard radical hysterectomy, the introduction of nerve-sparing approach reduces the occurrence of voiding dysfunction, and rectal as well as sexual issues, without determining detrimental effects on oncologic outcomes [14,21]. However, no studies had investigated how laparoscopic approach improves the beneficial effects of nerve-sparing procedures.
The main strength of our investigation is that this is the first paper focusing on the impact of laparoscopic approach in influencing the occurrence of pelvic floor dysfunction rates. The inherent biases related to the retrospective study design are the main limitation of the paper. Then, we have to stress that our results should be considered preliminary. Moreover, owing to the absence of other data and the relative small sample size of our population, further investigations are needed. We speculate that the magnified view of the laparoscope guarantees a better visualization of the nerves thus allowing a more accurate dissection in respect to open surgery. Additionally, other researches underlined that laparoscopic approach resulted in lower intra peritoneal adhesions and tissue damages in comparison with open procedures [22]. Four points of our study deserve to be addressed: 1) Patients in the control group had longer follow-up than patients undergoing laparoscopic surgery. Although we observed that there was no difference between the 2 approaches, our study had not aimed to compare oncologic effectiveness of these two approaches, but just to evaluate pelvic floor dysfunction rates. 2) The uses of a propensity-matching algorithm improve the value of our results. Although propensity matching does not correct for non-measurable variables (that are commonly corrected with the process of randomization) it aims to mimic a randomized study, reducing possible allocation biases between groups. 3) Our study compared 3D laparoscopic procedures with open abdominal procedures showing that 3D laparoscopy is associated with better outcomes than open surgery. Then our data are not fully applicable for conventional laparoscopic approach. To date no study focusing on this issue compared 3D and conventional laparoscopy. Further attention on this issue is needed. 4) All procedures are performed by skilled surgeons with a great experience in gynecologic oncology, thus our results are not projectable in a setting without experience for advanced gynecologic procedures.
It is important to underline that recent data questioned the safety of minimally invasive surgery for patients affected by CC [23,24]. The data from the Laparoscopic Approach to Carcinoma of the Cervix study presented by Ramirez et al. [23] at the Society of Gynecologic Oncology Annual Meeting underlined a detrimental effect related to the adoption of minimally invasive surgery in early stage CC. This phase III randomized controlled study compared minimally invasive vs. open abdominal radical hysterectomy. Minimally invasive radical hysterectomy was associated with higher recurrence rates in comparison to open abdominal operations. The number of disease recurrences after minimally invasive radical hysterectomy was four times higher than the number of recurrences after open surgery [23]. Similarly, results from more than 2,200 CC patients included in the Surveillance, Epidemiology & End Result (SEER) database reported similar the same finding [24]. The analysis of SEER database showed that 4-year mortality risks were 5.8% and 8.4% for open and minimally invasive surgery, respectively. The use of intrauterine manipulator, type of intra-abdominal colpotomy and the flow of gas into the abdominal cavity as well as the non-standardized learning curves among surgeons might be the reason of these findings. Further evidence is needed to better understand the association between type of surgical outcomes and survival outcomes.
In conclusion, the present paper investigated the role of laparoscopic surgery for the execution of nerve-sparing radical hysterectomy in patients affected by CC. Using a propensity-matched comparison (allowing to control for possible selection/allocation biases) we observed that laparoscopy guarantees better peri-operative results than open surgery. Laparoscopic approach is associated with a decrease in pelvic floor dysfunction rates in comparison of open surgery. The execution of laparoscopy correlates with a lower blood loss and shorter hospital stay in comparison to open surgery. Operative time and surgery-related morbidity as well as oncologic outcomes are comparable between groups. Further randomized controlled trials are warranted in order to explore the pros and cons of the adoption of minimally invasive techniques during nerve-sparing radical hysterectomy.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: B.G., R.D., D.A., C.V., L.C., L.R.M.U., L.D., R.F.
- Data curation: B.G., R.D., D.A., M.F., L.C., L.D., R.F.
- Formal analysis: B.G., M.F.
- Funding acquisition: B.G.
- Investigation: C.V.
- Methodology: B.G., R.F.
- Project administration: R.D.
- Resources: L.R.M.U., R.F.
- Software: L.R.M.U., R.F.
- Supervision: B.G., R.D., L.R.M.U.
- Validation: B.G., L.D.
- Visualization: B.G., L.C., R.F.
- Writing - original draft: B.G., R.D., M.F., C.V., L.C., L.R.M.U., L.D.
- Writing - review & editing: B.G., R.D., D.A., C.V., L.C., L.R.M.U., R.F.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 2.Rendón GJ, Echeverri L, Echeverri F, Sanz-Lomana CM, Ramirez PT, Pareja R. Outpatient laparoscopic nerve-sparing radical hysterectomy: a feasibility study and analysis of perioperative outcomes. Gynecol Oncol. 2016;143:352–356. doi: 10.1016/j.ygyno.2016.08.233. [DOI] [PubMed] [Google Scholar]
- 3.Gupta S, Maheshwari A, Parab P, Mahantshetty U, Hawaldar R, Sastri Chopra S, et al. Neoadjuvant chemotherapy followed by radical surgery versus concomitant chemotherapy and radiotherapy in patients with stage IB2, IIA, or IIB squamous cervical cancer: a randomized controlled trial. J Clin Oncol. 2018;36:1548–1555. doi: 10.1200/JCO.2017.75.9985. [DOI] [PubMed] [Google Scholar]
- 4.Kokka F, Bryant A, Brockbank E, Powell M, Oram D. Hysterectomy with radiotherapy or chemotherapy or both for women with locally advanced cervical cancer. Cochrane Database Syst Rev. 2015;(4):CD010260. doi: 10.1002/14651858.CD010260.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Lucidi A, Windemut S, Petrillo M, Dessole M, Sozzi G, Vercellino GF, et al. Self-reported long-term autonomic function after laparoscopic total mesometrial resection for early-stage cervical cancer: a multicentric study. Int J Gynecol Cancer. 2017;27:1501–1507. doi: 10.1097/IGC.0000000000001045. [DOI] [PubMed] [Google Scholar]
- 6.Raspagliesi F, Bogani G, Spinillo A, Ditto A, Bogliolo S, Casarin J, et al. Introducing nerve-sparing approach during minimally invasive radical hysterectomy for locally-advanced cervical cancer: a multi-institutional experience. Eur J Surg Oncol. 2017;43:2150–2156. doi: 10.1016/j.ejso.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 7.Bogani G, Serati M, Nappi R, Cromi A, di Naro E, Ghezzi F. Nerve-sparing approach reduces sexual dysfunction in patients undergoing laparoscopic radical hysterectomy. J Sex Med. 2014;11:3012–3020. doi: 10.1111/jsm.12702. [DOI] [PubMed] [Google Scholar]
- 8.Ercoli A, Delmas V, Gadonneix P, Fanfani F, Villet R, Paparella P, et al. Classical and nerve-sparing radical hysterectomy: an evaluation of the risk of injury to the autonomous pelvic nerves. Surg Radiol Anat. 2003;25:200–206. doi: 10.1007/s00276-003-0137-7. [DOI] [PubMed] [Google Scholar]
- 9.van Gent MD, Romijn LM, van Santen KE, Trimbos JB, de Kroon CD. Nerve-sparing radical hysterectomy versus conventional radical hysterectomy in early-stage cervical cancer. A systematic review and meta-analysis of survival and quality of life. Maturitas. 2016;94:30–38. doi: 10.1016/j.maturitas.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Díaz-Feijoo B, Bradbury M, Pérez-Benavente A, Franco-Camps S, Gil-Moreno A. Nerve-sparing technique during laparoscopic radical hysterectomy: critical steps. J Minim Invasive Gynecol. 2018;25:1144–1145. doi: 10.1016/j.jmig.2018.01.034. [DOI] [PubMed] [Google Scholar]
- 11.Bogani G, Raspagliesi F. Minimally invasive nerve-sparing radical hysterectomy: a win-win scenario. J Invest Surg. 2018 doi: 10.1080/08941939.2017.1413149. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 12.Bishop EA, Java JJ, Moore KN, Spirtos NM, Pearl ML, Zivanovic O, et al. Surgical outcomes among elderly women with endometrial cancer treated by laparoscopic hysterectomy: a NRG/Gynecologic Oncology Group study. Am J Obstet Gynecol. 2018;218:109.e1–109.11. doi: 10.1016/j.ajog.2017.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopez Labrousse MI, Frumovitz M, Guadalupe Patrono M, Ramirez PT. Sentinel lymph node mapping in minimally invasive surgery: role of imaging with color-segmented fluorescence (CSF) Gynecol Oncol. 2017;146:676–677. doi: 10.1016/j.ygyno.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 14.Bogani G, Rossetti DO, Ditto A, Signorelli M, Martinelli F, Mosca L, et al. Nerve-sparing approach improves outcomes of patients undergoing minimally invasive radical hysterectomy: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2018;25:402–410. doi: 10.1016/j.jmig.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Raspagliesi F, Bogani G, Martinelli F, Signorelli M, Chiappa V, Scaffa C, et al. Incorporating 3D laparoscopy for the management of locally advanced cervical cancer: a comparison with open surgery. Tumori. 2016;102:393–397. doi: 10.5301/tj.5000527. [DOI] [PubMed] [Google Scholar]
- 16.Kim HS, Kim M, Luo Y, Lee M, Song YS FUSION Study Group. Favorable factors for preserving bladder function after nerve-sparing radical hysterectomy: a protocol-based validation study. J Surg Oncol. 2017;116:492–499. doi: 10.1002/jso.24696. [DOI] [PubMed] [Google Scholar]
- 17.van Gent MD, Rademaker M, van der Veer JC, van Poelgeest MI, Gaarenstroom KN, Putter H, et al. Long-term oncological outcome after conventional radical hysterectomy versus 2 nerve-sparing modalities for early stage cervical cancer. Int J Gynecol Cancer. 2017;27:1729–1736. doi: 10.1097/IGC.0000000000001067. [DOI] [PubMed] [Google Scholar]
- 18.Bogani G, Cromi A, Uccella S, Serati M, Casarin J, Pinelli C, et al. Nerve-sparing versus conventional laparoscopic radical hysterectomy: a minimum 12 months' follow-up study. Int J Gynecol Cancer. 2014;24:787–793. doi: 10.1097/IGC.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 19.Bogani G, Multinu F, Dowdy SC, Cliby WA, Wilson TO, Gostout BS, et al. Incorporating robotic-assisted surgery for endometrial cancer staging: analysis of morbidity and costs. Gynecol Oncol. 2016;141:218–224. doi: 10.1016/j.ygyno.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 20.Bogani G, Uccella S, Cromi A, Serati M, Casarin J, Sturla D, et al. Electric motorized morcellator versus transvaginal extraction for myoma retrieval after laparoscopic myomectomy: a propensity-matched analysis. J Minim Invasive Gynecol. 2014;21:928–934. doi: 10.1016/j.jmig.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 21.Laterza RM, Salvatore S, Ghezzi F, Serati M, Umek W, Koelbl H. Urinary and anal dysfunction after laparoscopic versus laparotomic radical hysterectomy. Eur J Obstet Gynecol Reprod Biol. 2015;194:11–16. doi: 10.1016/j.ejogrb.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Ghezzi F, Cromi A, Serati M, Uccella S, Formenti G, Bogani G, et al. Radiation-induced bowel complications: laparoscopic versus open staging of gynecologic malignancy. Ann Surg Oncol. 2011;18:782–791. doi: 10.1245/s10434-010-1382-8. [DOI] [PubMed] [Google Scholar]
- 23.Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018;379:1895–1904. doi: 10.1056/NEJMoa1806395. [DOI] [PubMed] [Google Scholar]
- 24.Melamed A, Margul DJ, Chen L, Keating NL, Del Carmen MG, Yang J, et al. Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med. 2018;379:1905–1914. doi: 10.1056/NEJMoa1804923. [DOI] [PMC free article] [PubMed] [Google Scholar]