Abstract
IMPORTANCE
Differences in childhood obesity by demographics and urbanization have been reported.
OBJECTIVE
To present data on obesity and severe obesity among US youth by demographics and urbanization and to investigate trends by urbanization.
DESIGN, SETTING, AND PARTICIPANTS
Measured weight and height among youth aged 2 to 19 years in the 2001–2016 National Health and Nutrition Examination Surveys, which are serial, cross-sectional, nationally representative surveys of the civilian, noninstitutionalized population.
EXPOSURES
Sex, age, race and Hispanic origin, education of household head, and urbanization, as assessed by metropolitan statistical areas (MSAs; large: ≥ 1 million population).
MAIN OUTCOMES AND MEASURES
Prevalence of obesity (body mass index [BMI] ≥95th percentile of US Centers for Disease Control and Prevention [CDC] growth charts) and severe obesity (BMI ≥120% of 95th percentile) by subgroups in 2013–2016 and trends by urbanization between 2001–2004 and 2013–2016.
RESULTS
Complete data on weight, height, and urbanization were available for 6863 children and adolescents (mean age, 11 years; female, 49%). In 2013–2016, the prevalence among youth aged 2 to 19 years was 17.8% (95% CI, 16.1%−19.6%) for obesity and 5.8% (95% CI, 4.8%−6.9%) for severe obesity. Prevalence of obesity in large MSAs (171% [95% CI, 14.9%−19.5%]), medium or small MSAs (17.2% [95% CI, 14.5%−20.2%]) and non-MSAs (21.7% [95% CI, 16.1%−28.1%]) were not significantly different from each other (range of pairwise comparisons P = .09–.96). Severe obesity was significantly higher in non-MSAs (9.4% [95% CI, 5.7%−14.4%]) compared with large MSAs (5.1% [95% CI, 4.1%−6.2%]; P = .02). In adjusted analyses, obesity and severe obesity significantly increased with greater age and lower education of household head, and severe obesity increased with lower level of urbanization. Compared with non-Hispanic white youth, obesity and severe obesity prevalence were significantly higher among non-Hispanic black and Hispanic youth. Severe obesity, but not obesity, was significantly lower among non-Hispanic Asian youth than among non-Hispanic white youth. There were no significant linear or quadratic trends in obesity or severe obesity prevalence from 2001–2004 to 2013–2016 for any urbanization category (P range = .07–.83).
CONCLUSIONS AND RELEVANCE
In 2013–2016, there were differences in the prevalence of obesity and severe obesity by age, race and Hispanic origin, and household education, and severe obesity was inversely associated with urbanization. Demographics were not related to the urbanization findings.
Differences in childhood obesity prevalence by demographics have been reported in the United States,1,2 and Healthy People 2020 objectives include reducing disparities.3 In 2015–2016, obesity prevalence was higher in non-Hispanic black (22%) and Hispanic (26%) youth compared with non-Hispanic white (14%) and non-Hispanic Asian (11%) youth.2 Although not nationally representative, in 2015, the prevalence of obesity among American Indian and Alaska Native youth was 30% (Indian Health Service National Data Warehouse).4 Differences have also been reported by education and income.5 Youth living in households headed by college graduates have a lower prevalence of obesity compared with youth living in households headed by individuals with less education. Similarly, youth in higher- income households have a lower prevalence of obesity than youth living in households with less income. These differences, however, vary by sex, and race and Hispanic origin and may be changing over time.5
Differences in obesity prevalence have also been reported by level of urbanization.6–10 In 2011–2012, based on self-reported weight and height, the prevalence of overweight or obesity among US youth aged 10 to 17 years living in small rural areas was 38% compared with 30% among urban youth.11 Measured weight and height from 1999–2006 showed that rural children aged 2 to 19 years had consistently higher odds of overweight and obesity even after adjustment for sociodemographics, health, diet, and exercise.12
This analysis presents national measured weight and height for 2013–2016 on obesity and severe obesity prevalence among US youth by demographic subgroup and by level of urbanization. Trends over time in obesity prevalence among US youth by age, race and Hispanic origin, income, and education of household head have been published,1,5,13 but trends in obesity and severe obesity prevalence by urbanization level have not been well studied. Thus an objective of this analysis was to investigate trends by urbanization level from 2001 through 2016.
Methods
A nationally representative survey of the civilian, noninstitutionalized population, the National Health and Nutrition Examination Survey (NHANES) contains both interviews and examinations.14 NHANES includes oversampling in its complex probability sample design. In 2013–2016, non-Hispanic black, non-Hispanic Asian, and Hispanic individuals were oversampled. NHANES began collecting data continuously in 1999 with public data releases every 2 years. Because of small sample sizes for some subgroups or due to low prevalence of some health conditions, multiple 2-year data cycles are often combined. Youth aged 7 to 17 years of age provided documented assent and, for youth 17 years and younger, parents or guardians provided permission. Participants 18 years and older provided consent. The National Center for Health Statistics (NCHS) research ethics review board approved NHANES. For youth aged 1 to 19 years, the response rate for the examination component was 76% in 2013–2014 and 64.6% in 2015–2016; response rates for youth from 2001–2002 to 2011–2012 ranged from 87% to 77%.15
Standardized measurements of weight and height were obtained during the NHANES examination. Obesity among youth aged 2 to 19 years was defined as body mass index (BMI [calculated as weight in kilograms divided by height in meters squared]) at or above the sex-specific 95th percentile of the US Centers for Disease Control and Prevention (CDC) BMI-for-age growth charts.16 Severe obesity was defined as BMI at or above 120% of the 95th percentile of the CDC BMI-for-age growth charts.17,18
Demographic variables included sex, age, race and Hispanic origin, and education of household head because previous analyses have found differences by these factors.1,19 Age groups were 2 to 5, 6 to 11, and 12 to 19 years at time of examination and were the age groups used in the sample design. Race and Hispanic origin was reported by participants or proxy respondents (such as parents) and was categorized as non-Hispanic white, non-Hispanic black, non-Hispanic Asian, Hispanic, and other (including multiple races). Results for the “other” category were included in analyses of the entire population but were not shown separately. The term “race and Hispanic origin” is used in the text to reflect the specific designation in NHANES. Education of household head was categorized as high school diploma or less, some college, and college graduate.
Level of urbanization was assigned to each NHANES participant based on participant’s county of residence (NHANES 2001–2014) or county location of examination (NHANES 2015–2016). Unweighted agreement between urbanization level categories based on county of residence and county location of examination was 99.9% for NHANES 2007–2014 participants. County of residence and county location of examination were not included in the public use NHANES data files due to disclosure risk, but can be obtained through the NCHS Research Data Center.20 Level of urbanization was categorized based on 1990 (for NHANES 2001–2004), 2006 (for NHANES 2005–2012), and 2013 (for NHANES 2013–2016) NCHS classification schemes for counties.21,22 The NCHS scheme is based on 4 metropolitan and 2 nonmetropolitan categories. The metropolitan categories included (1) large central metropolitan or counties in metropolitan statistical areas (MSAs) with a population of 1 million or more that contain all or part of the area’s principal city; (2) large fringe metropolitan or counties in MSAs with a population of 1 million or more that surrounded the large central metropolitan counties; (3) medium metropolitan or counties in MSAs with a population of 250 000 to 999 999; and (4) small metropolitan or counties in MSAs with population of less than 250 000. Nonmetropolitan, or the most rural areas, included (1) micropolitan or counties with urban cluster populations from 10 000 to 49 999 and (2) noncore or metropolitan counties that did not qualify as micropolitan. For these analyses, urbanization was categorized as large MSA (combined large central and fringe metropolitan); medium or small MSA (combined medium and small metropolitan); and non-MSA (combined micropolitan and noncore). The NCHS metropolitan categories were collapsed for this analysis to increase sample size for subgroups and produce stable estimates based on the NCHS data presentation standards for proportions.23
Prevalence of obesity and severe obesity with 95% CIs were presented for each demographic subgroup and urbanization category. Estimates by urbanization category could not be presented by demographic subgroup due to small sample size and low degrees of freedom. Differences by urbanization category were tested using pairwise t tests and, adjustedfor demographic characteristics, in logistic regression models. Adjusted prevalence ratios24 and differences in the adjusted prevalence were presented. Ninety five percent CIs for the differences were constructed by the Wald method25 using a t statistic with degrees of freedom equal to the minimum degrees of freedom of the standard errors of the 2 risk ratios. Urbanization category, age, and education were also included as continuous variables in the logistic models to test for adjusted linear trends in obesity and severe obesity by these variables. The Satterthwaite-adjusted F test26 was used to assess statistical significance and the associated P values were reported.
To further investigate the association between urbanization category and obesity, smoothed, age-specific 50th and 95th percentiles of BMI were presented for each urbanization category. The percentiles were smoothed using weighted quantile regression with restricted cubic spline of age in months with 4 knots at the 5th, 35th, 65th, and 95th age percentiles.
Analysis of trends in obesity and severe obesity prevalence from 2001–2002 to 2015–2016 were conducted, stratified by urbanization category. Tabular and graphical presentation of obesity and severe obesity prevalence over this period included point estimates and CIs with combined 4-year NHANES data for 2001–2004, 2005–2008, 2009–2012, and 2013–2016 because these estimates were more stable than the estimates based on 2 years of data. Linear and quadratic trends in obesity prevalence by urbanization category were tested using orthogonal contrasts with 8 two-year survey cycles treated as a continuous variable. No significant interactions were found between urbanization category and survey period.
The NHANES complex sample design was incorporated in standard error estimates and all statistical testing. Taylor series linearization27 was used to estimate standard errors. Examination sample weights were used in all analyses and adjusted for the differential probabilities of selection, noncoverage, and nonresponse. These adjustments accounted for loss between the screener and interview and between interview and examination. The approach described in Korn and Graubard was used to calculate CIs.28 A 2-sided P value of .05 was used to assess statistical significance. No adjustments were made for multiple comparisons. Statistical reliability was assessed using the NCHS data presentation standards for proportions.23 Analyses were conducted in SAS (SAS Institute), version 9.4; SUDAAN (RTI International), version 11.0; R (R Foundation), version 3.4.1; and Stata (StataCorp), version 13.
Results
In 2013–2016, 152 youth aged 2 to 19 years were missing weight, height, or both and 9 were pregnant and were excluded from the analysis (unweighted percentage, 161 of 7024 participants [2.3%]) leaving a total sample size of 6863. An additional 229 youth were missing data on education of household head and were excluded from analyses that included this variable. No data on urbanization were missing. Non-Hispanic Asian subgroups had the lowest unweighted sample sizes (eg, 52 for females aged 2 to 5 years), whereas Hispanic subgroups had the largest (eg, 260 for females aged 2 to 5 years). Sample sizes for all subgroups are included in Table 1. Unweighted numbers of children and adolescents with obesity or severe obesity are in eTable 1 and eTable 2 in the Supplement.
Table 1.
Unweighted Sample Sizes for US Youth Aged 2 to 19 Years With BMI Data by Sex, Age Group, Education of Household Head, and Race and Hispanic Origin in the National Health and Nutrition Examination Survey, 2013–2016`.
| Race and Hispanic Origin, No. of Participants |
|||||
|---|---|---|---|---|---|
| Non-Hispanic |
|||||
| All Groupsa | White | Black | Asian | Hispanic | |
| All | 6863 | 1844 | 1669 | 612 | 2269 |
| Age, y | |||||
| 2–5 | 1657 | 468 | 414 | 129 | 510 |
| 6–11 | 2562 | 687 | 627 | 200 | 866 |
| 12–19 | 2644 | 689 | 628 | 283 | 893 |
| Sex | |||||
| Male | |||||
| Age, y | |||||
| 2–19 (Overall) | 3490 | 981 | 857 | 326 | 1094 |
| 2–5 | 846 | 242 | 205 | 77 | 250 |
| 6–11 | 1292 | 367 | 320 | 108 | 413 |
| 12–19 | 1352 | 372 | 332 | 141 | 431 |
| Female | |||||
| Age, y | |||||
| 2–19 (Overall) | 3373 | 863 | 812 | 286 | 1175 |
| 2–5 | 811 | 226 | 209 | 52 | 260 |
| 6–11 | 1270 | 320 | 307 | 92 | 453 |
| 12–19 | 1292 | 317 | 296 | 142 | 462 |
| Education of household headb | |||||
| ≤High school diploma | 3108 | 592 | 730 | 180 | 1450 |
| Some college | 2065 | 649 | 648 | 105 | 506 |
| College graduate | 1461 | 557 | 256 | 282 | 224 |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Includes race and Hispanic origin groups not shown separately.
Sample sizes for education categories do not sum to 6863 due to missing values.
Analyses that included data from 2001–2002 to 2015–2016 included 29 292 youth (29 292 of 30102 participants [97.3%] who were nonpregnant and examined). From 2001–2002 to 2015–2016, 810 youth were missing data on weight, height, or both or urbanization.
The prevalence of obesity among US youth aged 2 to 19 years was 17.8% (95% CI, 16.1% to 19.6%) and the prevalence of severe obesity was 5.8% (95% CI, 4.8% to 6.9%) in 2013–2016 (Table 2). Differences in adjusted prevalence and adjusted prevalence ratios (aPR) by sex, age, race and Hispanic origin, education of household head, and urbanization in 2013–2016 also are shown in Table 2. In adjusted analyses of obesity, there was a significant linear trend by age (P < .001). Obesity prevalence among youth aged 6 to 11 years (17.9%) and 12 to 19 years (20.6%) was significantly higher compared with youth aged 2 to 5 years (11.6%) (adjusted difference for youth aged 6–11 years vs 2–5 years, 6.9 percentage points [95% CI, 3.8 to 10.1]; aPR, 1.62 (95% CI, 1.30 to 2.01); adjusted difference for youth aged 12–19 years vs 2–5 years, 9.6 percentage points [95% CI, 5.6 to 13.5]; aPR, 1.85 [95% CI, 1.45 to 2.37]).
Table 2.
Prevalence, Difference in Adjusted Prevalence, and Adjusted Prevalence Ratio for Obesity and Severe Obesity Among US Youth Aged 2 to 19 Years, 2013–2016a
| Characteristic | Prevalence, % (95% CI) | Difference in Adjusted Prevalence, % (95% CI)b | Adjusted Prevalence Ratio (95% CI)b | Linear Trend Across Characteristic, P Valueb’c |
|---|---|---|---|---|
|
Obesityd | ||||
| Overall | 17.8 (16.1 to 19.6) | |||
| Sex | ||||
| Male | 18.1 (16.0 to 20.4) | [Reference] | [Reference] | NA |
| Female | 17.5 (15.4 to 19.6) | 0.7 (−1.9 to 3.2) | 1.04 (0.90 to 1.20) | |
| Age, y | ||||
| 2–5 | 11.6 (9.8 to 13.6) | [Reference] | [Reference] | |
| 6–11 | 17.9 (15.5 to 20.5) | 6.9 (3.8 to 10.1) | 1.62 (1.30 to 2.01) | <.001 |
| 12–19 | 20.6 (17.6 to 23.8) | 9.6 (5.6 to 13.5) | 1.85 (1.45 to 2.37) | |
| Race and Hispanic origine | ||||
| Non-Hispanic white | 14.7 (12.7 to 16.9) | [Reference] | [Reference] | |
| Non-Hispanic black | 20.4 (17.1 to 24.1) | 5.0 (1.0 to 9.0) | 1.33 (1.07 to 1.66) | NA |
| Non-HispanicAsian | 9.8 (7.4 to 12.6) | −3.5 (−6.9 to 0) | 0.77 (0.58 to 1.02) | |
| Hispanic | 23.6 (21.2 to 26.1) | 7.4 (4.4 to 10.4) | 1.49 (1.27 to 1.75) | |
| Education of household head | ||||
| ≤High school diploma | 22.3 (20.3 to 24.4) | 7.5 (4.3 to 10.8) | 1.58 (1.25 to 1.98) | |
| Some college | 18.1 (15.1 to 21.3) | 5.2 (1.0 to 9.4) | 1.40 (1.06 to 1.85) | <.001 |
| College graduate | 11.6 (9.1 to 14.5) | [Reference] | [Reference] | |
| Urbanization | ||||
| Large MSA | 17.1 (14.9 to 19.5) | [Reference] | [Reference] | |
| Medium or small MSA | 17.2 (14.5 to 20.2)f | 1.0 (−2.2 to 4.3) | 1.06 (0.91 to 1.24) | .11 |
| Non-MSA | 21.7 (16.1 to 28.1)f | 3.7 (−2.4 to 9.8) | 1.22 (0.94 to 1.58) | |
|
Severe Obesityg | ||||
| Overall | 5.8 (4.8 to 6.9) | |||
| Sex | ||||
| Male | 6.0 (4.9 to 7.3) | [Reference] | [Reference] | NA |
| Female | 5.6 (4.4 to 7.1) | 0.3 (−1.2 to 1.8) | 1.05 (0.81 to 1.36) | |
| Age, y | ||||
| 2–5 | 1.8 (1.1 to 2.7) | [Reference] | [Reference] | |
| 6–11 | 4.8 (3.8 to 6.0) | 3.1 (1.6 to 4.5) | 2.70 (1.59 to 4.59) | <.001 |
| 12–19 | 8.4 (6.7 to 10.3) | 6.8 (4.9 to 8.7) | 4.78 (2.98 to 7.66) | |
| Race/Hispanic origin | ||||
| Non-Hispanic white | 4.4 (3.4 to 5.7) | [Reference] | [Reference] | |
| Non-Hispanic black | 7.9 (5.9 to 10.2) | 3.4 (1.6 to 5.2) | 1.76 (1.33 to 2.32) | NA |
| Non-HispanicAsian | 1.3 (0.5 to 3.0) | −3.1 (−4.6 to −1.5) | 0.31 (0.13 to 0.73) | |
| Hispanic | 8.4 (7.0 to 9.9) | 3.8 (1.9 to 5.6) | 1.84 (1.37 to 2.49) | |
| Education of household head | ||||
| ≤High school diploma | 7.7 (6.4 to 9.2) | 2.4 (0.8 to 4.0) | 1.57 (1.11 to 2.22) | |
| Some college | 6.0 (4.5 to 7.8) | 1.8 (−0.2 to 3.9) | 1.44 (0.95 to 2.18) | .01 |
| College graduate | 3.3 (2.2 to 4.7) | [Reference] | [Reference] | |
| Urbanization | ||||
| Large MSA | 5.1 (4.1 to 6.2) | [Reference] | [Reference] | |
| Medium or small MSA | 5.3 (4.3 to 6.5)f | 0.9 (−0.6 to 2.4) | 1.18 (0.93 to 1.50) | .003 |
| Non-MSA | 9.4 (5.7 to 14.4)f | 4.1 (0.4 to 7.9) | 1.83 (1.26 to 2.66) | |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); MSA, metropolitan statistical area; NA, not applicable.
Data from the National Health and Nutrition Examination Survey; estimates are weighted. See Table 1 for unweighted sample sizes and eTables 1 and 2 in the Supplement for unweighted No. of persons with obesity or severe obesity by age, sex, education of household head, race and Hispanic origin, and urbanization.
Multivariate logistic regression model included all 5 characteristics.
For linear trend.
Obesity was defined as at or above the sex-specific95th percentile of US Centers for Disease Control and Prevention (CDC) BMI-for-age growth charts.
Includes race and Hispanic origin groups not shown separately.
Standard error degrees of freedom <8.
Severe obesity was defined as ≥120% of the sex-specific 95th percentile of CDCBMI-for-age growth charts.
Obesity prevalence was also significantly higher among non-Hispanic black youth (20.4%) and Hispanic youth (23.6%) compared with non-Hispanic white youth (14.7%) (adjusted difference for non-Hispanic black youth vs non-Hispanic white youth, 4.97percentage points [95% CI, 0.95 to 8.99]; aPR, 1.33 [95% CI, 1.07 to 1.66]; adjusted difference for Hispanic youth vs non-Hispanic white youth, 7.37 percentage points [95% CI, 4.36 to 10.38]; aPR, 1.49 [95% CI, 1.27 to 1.75]). There was no significant difference between non-Hispanic Asian youth (9.8%) and non-Hispanic white youth (adjusted difference, −3.5 percentage points [95% CI, 0 to −6.9]; aPR, 0.77 [95% CI, 0.58 to 1.02]).
There was a significant linear trend in obesity by education of household head (P < .001). The prevalence of obesity among youth living in households headed by individuals with a high school diploma or less (22.3%) or in households headed by individuals with some college education (18.1%) was significantly higher compared with youth living in households headed by college graduates (11.6%) (adjusted difference for youth living in households headed by individuals with ≤high school diploma vs youth living in households headed by college graduates, 7.5 percentage points [95% CI, 4.3 to 10.8]; aPR, 1.58 [95% CI, 1.25 to 1.98]; adjusted difference for youth living in households headed by individuals with some college education vs youth living in households headed by college graduates, 5.2 percentage points [95% CI, 1.0 to 9.4]; aPR, 1.40 [95% CI, 1.06 to 1.85]).
A linear trend in obesity across urbanization categories was not significant (P = .11). The prevalence of obesity in non-MSAs (21.7%) and medium or small MSAs (17.2%) was not significantly different compared with large MSAs (17.1%) (adjusted difference for large MSAs vs non-MSAs, 3.7 percentage points [95% CI, −2.4 to 9.8]; aPR, 1.22 [95% CI, 0.94 to 1.58]; adjusted difference for large MSAs vs medium or small MSAs, 1.0 percentage points [95% CI, −2.2 to 4.3]; aPR, 1.06 [95% CI, 0.91 to 1.24]).
Results from the adjusted analysis of severe obesity were similar to results for obesity (Table 2), although the estimated aPRs were farther from 1.0 for age and race and Hispanic origin, and severe obesity was significantly lower for non-Hispanic Asian youth (1.3%) compared with non-Hispanic white youth (4.4%) (adjusted difference, −3.1 percentage points [95% CI, −1.5 to −4.6]; aPR, 0.31 [95% CI, 0.13 to 0.73]). The linear trend across urbanization categories for severe obesity was significant (P = .003). Prevalence of severe obesity in non-MSAs (9.4%) was significantly higher than in large MSAs (5.1%) (adjusted difference, 4.1 percentage points [95% CI, 0.4 to 7.9]; aPR, 1.83 [95% CI, 1.26 to 2.66]). The prevalence of severe obesity in medium or small MSAs (5.3%) was not significantly different compared with large MSAs (adjusted difference, 0.9 percentage points [95% CI, −0.6 to 2.4]; aPR, 1.18 [95% CI, 0.93 to 1.50]).
Detailed estimates of obesity and severe obesity prevalence by sex, age, education of household head, and race and Hispanic origin are presented in Table 3.
Table 3.
Prevalence of Obesity and Severe Obesity Among US Youth Aged 2 to 19 Years, by Sex, Age, Education of Household Head, and Race and Hispanic Origin, 2013–2016a,b
| Prevalence by Race and Hispanic Origin, % (95% CI) |
|||||
|---|---|---|---|---|---|
| Non-Hispanic |
|||||
| All Groupsc | White | Black | Asian | Hispanic | |
|
Obesityd | |||||
| Age, y | |||||
| 2–5 | 11.6 (9.8–13.6) | 9.9 (6.7–13.8) | 11.6 (7.4–17.1) | 7.0 (3.1–13.3)e | 16.5 (13.4–20.0) |
| 6–11 | 17.9 (15.5–20.5) | 14.0 (11.3–17.1) | 19.8 (16.6–23.3) | 12.9 (7.5–20.2) | 25.3 (22.2–28.7) |
| 12–19 | 20.6 (17.6–23.8) | 17.2 (12.6–22.6) | 25.0 (19.8–30.8) | 8.8 (5.7–12.7) | 25.9 (22.9–29.0) |
| Sex | |||||
| Male | |||||
| Age, y | |||||
| 2–19 (Overall) | 18.1 (16.0–20.4) | 15.3 (12.7–18.2) | 17.9 (14.4–21.8) | 11.9 (8.3–16.3) | 24.3 (20.6–28.3) |
| 2–5 | 11.5 (9.1–14.3) | 9.3 (5.6–14.4) | 12.4 (7.1–19.5) | 9.1 (3.4–18.8)e | 16.7 (11.7–22.8) |
| 6–11 | 19.6 (16.4–23.2) | 17.3 (13.3–21.9) | 15.5 (11.7–19.9) | 17.7 (8.0–31.8)e | 26.1 (19.9–33.1) |
| 12–19 | 20.0 (16.6–23.8) | 16.3 (11.4–22.2) | 22.0 (16.6–28.3) | 9.1 (4.9–15.1) | 26.7 (22.6–31.1) |
| Female | |||||
| Age, y | |||||
| 2–19 (Overall) | 17.5 (15.4–19.6) | 14.1 (11.1–17.5) | 23.0 (18.4–28.1) | 7.4 (4.7–11.1) | 22.9 (20.1–25.8) |
| 2–5 | 11.7 (9.6–14.2) | 10.4 (6.3–15.9) | 11.0 (6.8–16.4) | 4.3 (0.6–14.3)e,f | 16.3 (11.7–21.8) |
| 6–11 | 16.1 (13.5–19.0) | 10.4 (6.8–15.0) | 24.1 (19.4–29.4) | 7.8 (3.2–15.3)e | 24.5 (20.5–28.9) |
| 12–19 | 21.2 (17.4–25.4) | 18.1 (11.9–25.9) | 28.2 (20.8–36.5) | 8.4 (4.2–14.5) | 25.0 (20.4–30.1) |
| Education of household head | |||||
| ≤High school diploma | 22.3 (20.3–24.4) | 18.1 (14.3–22.6) | 20.1 (14.8–26.2) | 11.6 (7.0–17.7) | 27.2 (24.3–30.3) |
| Some college | 18.1 (15.1–21.3) | 15.2 (10.8–20.7) | 21.6 (18.0–25.5) | 18.6 (9.6–30.9) | 21.4 (17.9–25.2) |
| College graduate | 11.6 (9.1–14.5) | 11.5 (8.3–15.3) | 19.0 (12.7–26.7) | 6.4 (3.9–9.9) | 9.1 (4.5–16.0) |
|
Severe Obesityg | |||||
| Age, y | |||||
| 2–5 | 1.8 (1.1–2.7) | 1.1 (0.3–3.1) | 2.1 (0.7–5.0) | 0 (h)−2.8 | 2.7 (1.4–4.7) |
| 6–11 | 4.8 (3.8–6.0) | 3.1 (1.7–5.0) | 6.5 (4.7–8.8) | 2.4 (0.7–5.6) | 8.0 (6.3–10.0) |
| 12–19 | 8.4 (6.7–10.3) | 6.7 (4.9–9.0) | 11.5 (7.5–16.6) | 1.1 (0.2–3.3) | 11.6 (9.5–14.0) |
| Sex | |||||
| Male | |||||
| Age, y | |||||
| 2–19(Overall) | 6.0 (4.9–7.3) | 4.1 (3.0–5.5) | 7.2 (5.1–9.9) | 1.8 (0.6–4.0) | 9.8 (7.6–12.3) |
| 2–5 | 1.4 (0.7–2.4) | 0.4 (0.0–2.2) | 3.0 (0.9–7.5)e | 0 (h-4.7) | 2.8 (1.1–5.7) |
| 6–11 | 4.8 (3.4–6.5) | 3.2 (1.6–5.8) | 4.2 (2.3–7.1) | 2.4 (0.4–7.4)e | 9.1 (6.1–13.0) |
| 12–19 | 8.9 (6.9–11.4) | 6.3 (4.1–9.3) | 11.1 (6.5–17.4) | 2.2 (0.4–6.7)e | 13.7 (10.6–17.3) |
| Female | |||||
| Age, y | |||||
| 2–19(Overall) | 5.6 (4.4–7.1) | 4.7 (3.1–6.9) | 8.5 (5.9–11.9) | 0.8 (0.1–3.3) | 6.9 (5.2–8.9) |
| 2–5 | 2.1 (1.0–3.9) | 1.9 (0.3–5.9)e | 1.3 (0.1–5.2)e | 0 (h-6.8)f | 2.6 (1.0–5.4) |
| 6–11 | 4.8 (3.5–6.4) | 2.9 (1.4–5.4) | 8.9 (5.4–13.6) | 2.4 (0.2–9.5)e | 6.8 (4.7–9.6) |
| 12–19 | 7.8 (5.6–10.5) | 7.2 (3.9–11.9) | 11.9 (7.3–18.0) | 0 (h-2.6) | 9.3 (6.4–13.0) |
| Education of household head | |||||
| ≤High school diploma | 7.7 (6.4–9.2) | 5.3 (3.5–7.6) | 9.1 (5.8–13.4) | 1.6 (0.3–4.9) | 9.7 (8.0–11.6) |
| Some college | 6.0 (4.5–7.8) | 5.1 (3.3–7.4) | 7.8 (5.3–11.1) | 1.7 (0.1–7.5)e | 8.4 (5.6–11.9) |
| College graduate | 3.3 (2.2–4.7) | 3.4 (2.0–5.3) | 5.2 (2.3–9.8)e | 0.7 (0.1–2.5) | 1.8 (0.4–5.4) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Data from the National Health and Nutrition Examination Survey estimates are weighted.
See Table 1 for unweighted sample sizes and eTable 1 in the Supplement for unweighted No. of persons with obesity or severe obesity by age, sex, education of household head, and race and Hispanic origin.
Includes other race and Hispanic origin groups not shown separately.
Obesity was defined as at or above the sex-specific 95th percentile of US Centers for Disease Control and Prevention (CDC) BMI-for-age growth charts.
Estimate potentially unreliable, CI >5 percentage points and relative CI width >130%.
Standard error degrees of freedom <8.
Severe obesity was defined as ≥120% of the sex-specific 95th percentile of CDC BMI-for-age growth charts.
Lower limit of CI could not be calculated.
There were no significant linear or quadratic trends in obesity or severe obesity prevalence from 2001–2004 to 2013–2016 for any urbanization category (range of P = .07 to .83) (Table 4 and eFigures 1–2 in the Supplement). The same pattern was seen over time where the prevalence of obesity and severe obesity were higher in non-MSAs compared with large MSAs at each of the 4 periods. There was a significant linear trend across urbanization categories in prevalence of obesity (P = .006) and severe obesity (P < .001) when combining 16 years of data (2001–2016).
Table 4.
Trends in Prevalence of Obesity and Severe Obesity in US Youth Aged 2 to 19 Years by Urbanization, 2001–2004 to 2013–2016a
| Large MSA |
Medium or Small MSA |
Non-MSA |
||||
|---|---|---|---|---|---|---|
| Survey Years | No. of Participants | % (95% CI) | No. of Participants | % (95% CI) | No. of Participants | % (95% CI) |
|
Obesityb,c | ||||||
| 2001–2004 | 4201 | 15.3 (14.0–16.7) | 2806 | 15.7 (12.6–19.1) | 1211 | 20.0 (15.7–24.9) |
| 2005–2008 | 4658 | 15.8 (13.6–18.3) | 1759 | 14.9 (10.6–20.1)d | 1033 | 19.1 (14.8–24.1) |
| 2009–2012 | 4073 | 15.3 (13.5–17.2) | 1521 | 20.2 (15.7–25.4)d | 1167 | 17.1 (13.3–21.4) |
| 2013–2016 | 3886 | 17.1 (14.9–19.5) | 2047 | 17.2 (14.5–20.2)d | 930 | 21.7 (16.1–28.1)d |
| P value for trend over time | ||||||
| Linear | .14 | 00 | .46 | |||
| Quadratic | .28 | .19 | .07 | |||
|
Severe Obesitye,f | ||||||
| 2001–2004 | 4201 | 4.3 (3.5–5.2) | 2806 | 5.0 (3.7–6.6) | 1211 | 7.3 (4.6–10.8) |
| 2005–2008 | 4658 | 4.8 (3.9–5.8) | 1759 | 3.7 (2.3–5.6)d | 1033 | 6.8 (3.5–11.6) |
| 2009–2012 | 4073 | 4.6 (3.5–5.9) | 1521 | 7.3 (4.1–11.8)d | 1167 | 6.1 (4.5–8.0) |
| 2013–2016 | 3886 | 5.1 (4.1–6.2) | 2047 | 5.3 (4.3–6.5)d | 930 | 9.4 (5.7–14.4)d |
| P value for trend over time | ||||||
| Linear | .29 | .21 | .19 | |||
| Quadratic | .83 | .39 | .07 | |||
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); MSA, metropolitan statistical area.
Data from the National Health and Nutrition Examination Survey, all estimates except sample sizes are weighted; see eTable 2 in the Supplement for unweighted No. of persons with obesity and severe obesity by urbanization and survey period.
Obesity was defined as at or above the sex-specific 95th percentile of US Centers for Disease Control and Prevention (CDC) BMI-for-age growth charts.
Trend across urbanization all16ycombined (2001–2016), P = .006.
Standard error degrees of freedom <8.
Severe obesity was defined as ≥120% of the sex-specific95th percentile of CDC BMI-for-age growth charts.
Trend across urbanization all 16 y combined (2001–2016), P < .001.
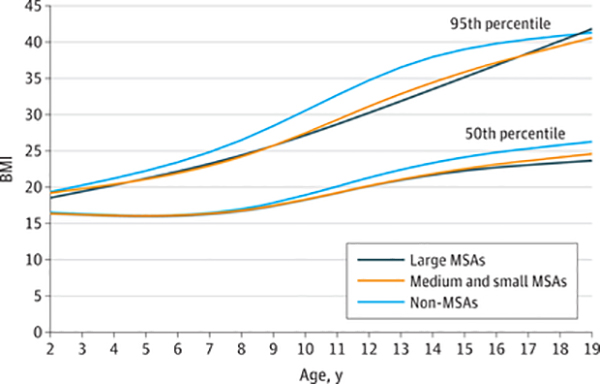
Smoothed estimates of the 50th and 95th percentiles of BMI by age for large MSAs, medium or small MSAs, and non- MSAs are shown in the Figure. The smoothed 95th percentile of BMI among adolescents aged 14 years living in non- MSAs was 38 (ie, 5% of adolescents aged 14 years had a BMI >38), whereas the 95th percentile among adolescents aged 14 years living in large MSAs was 33.5. These smoothed estimates describe the age patterns and differences between urbanization categories; statistical tests were not performed. Although the 50th percentiles overlapped between urbanization categories until about 10 years, the 95th percentile for non-MSAs was higher than in large MSAs and medium or small MSAs until age 18 years. This Figure shows different patterns in BMI distribution by urbanization category suggesting the distribution in non-MSAs is more skewed to the right than in other areas and that, starting around age 10 years, the distribution in non-MSAs is also shifted to the right compared with other urbanization categories.
Figure. Smoothed 50th and 95th BMI Percentiles Among US Youth Aged 2 to 19 Years by Urbanization Category and Age, 2013–2016.
BMI indicates body mass index (calculated as weight in kilograms divided by height in meters squared); MSA, metropolitan statistical area. Estimates are weighted. Data source: National Health and Nutrition Examination Survey.
Discussion
In 2013–2016, obesity and severe obesity among US youth was associated with age, race and Hispanic origin, and education of household head. Severe obesity was also inversely associated with urbanization. The association between urbanization and obesity was in the same direction as severe obesity but was not significant. Demographics were not related to the difference by urbanization. In addition, differences in the distribution of BMI among children and adolescents in non- MSAs compared with large and medium or small MSAs suggest that youth in non-MSAs are heavier than those in other areas. Variation by age, race and Hispanic origin, and education of household head is comparable with previous reports.1
Recent analyses of health disparities, including obesity, in youth have included analyses based on urbanization.10 A review of the literature, including 2 studies using NHANES data from 1999–2006 and 2003–2006, reported that obesity prevalence was higher among rural children than among children living in urban areas, and this difference was larger among older children compared with younger children.6 The current results did not show an interaction between age and urbanization level. In an analysis of 2001–2010 NHANES data, racial differences in weight among US youth were explained entirely by social determinants including neighborhood factors.7 State-level studies have also found differences by urbanization. A study using school-based BMI from elementary schools in Pennsylvania found differences in obesity prevalence by urbanization.8 Different studies, however, use different categories of urbanization in part because of available sample sizes.
Research in low-income and middle-income countries has also shown differences by urbanization, but in the opposite direction compared with high-income countries. In low- income and middle-income countries, urban areas have had higher levels of BMI but the differences have been attenuated after adjusting for socioeconomic status.29 These results are in contrast with the current results in which adjustment for socioeconomic status did not change the association between urbanization and obesity. In the current analysis, however, no adjustments were made for measures of socioeconomic status beyond education and the analyses focused on prevalence, not mean BMI.
Trends from 2001–2002 to 2015–2016 were not significant for any urbanization category. The current study investigated trends over a 16-year period beginning in 2001–2002 because 4 years of data were needed to provide estimates by urbanization and 16 years allowed 4 estimates over time. Analysis of overall trends in obesity among youth beginning in 1999–2000 show an increase in prevalence,2 suggesting changes from 1999–2000 to 2015–2016 have been driven by changes very early in this period. Trends may also vary within subgroups not analyzed in the current study.
The prevalence of severe obesity among US youth was more than 10% in some adolescent subgroups. Research has suggested that youth with severe obesity have a worse cardiovascular disease risk profile than youth with lesser obesity.18 In one study,30 severe obesity was associated with higher risk for hypertension compared with lesser obesity. In addition, there was strong tracking over the study period of 2 to 3 years with 72% remaining severely obese at follow-up.
This study has strengths. NHANES is representative of the US civilian, noninstitutionalized population and contains measured weight and height, which result in more accurate estimates of BMI than do self-report or parental report of weight and height.31,32
Limitations
This study has several limitations. First, BMI is not a direct measure of adiposity and health risk. Although children with high BMIs are likely to have high levels of adiposity,33 there are variations by race and Hispanic origin.34 Adiposity among non-Hispanic black youth is lower than among non-Hispanic white and Mexican American youth at the same BMI level.34 However, among Asian adults, health risk begins at a lower BMI than in white adults.35 Differences among youth are not as well described, however. One study found that South Asian youth had higher BMI-adjusted blood pressure than white youth in the United States.36 The lower prevalence estimates of obesity seen among Asians compared with other race and Hispanic origin groups may not reflect lower disease risk.37 Second, NHANES is limited by small sample sizes for some subgroups, which restricts the ability to provide estimates by urbanization category for subgroups of the population. Third, NHANES was not designed to provide estimates representative of different urbanization categories or counties, so some cells have low degrees of freedom, which can result in inflated standard errors and reduced statistical power.
Conclusions
In 2013–2016, there were differences in the prevalence of obesity and severe obesity by age, race and Hispanic origin, and household education, and severe obesity was inversely associated with urbanization. Demographics were not related to the urbanization findings.
Supplementary Material
Key Points.
Question
In 2013–2016, were there differences in obesity and severe obesity prevalence by demographics and urbanization level among US children and adolescents?
Findings
In this cross-sectional analysis that included 6863 children and adolescents aged 2 to 19 years, differences in obesity and severe obesity prevalence by age, race and Hispanic origin, and household education were found. Differences in obesity by urbanization levels were not significant, but the prevalence of severe obesity was significantly higher in non-metropolitan statistical areas (MSAs) (9.4%) than in large MSAs (5.1%).
Meaning
Differences in age, race and Hispanic origin, or education of household head were not related to the difference in severe obesity by urbanization.
Acknowledgments
Role of the Funder/Sponsor: The National Center for Health Statistics (NCHS) and the US Centers for Disease Control and Prevention (CDC) had a role in the design and conduct of the National Health and Nutrition Examination Surveys and in the collection and management of the data and the clearance of the manuscript; however, the NCHS and the CDC had no role in the preparation of the manuscript; or in the decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Disclaimer: The findings and conclusions in this report are those of the authors and not necessarily the official position of the CDC.
Contributor Information
Cynthia L. Ogden, National Center for Health Statistics, US Centers for Disease Control and Prevention, Hyattsville, Maryland.
Cheryl D. Fryar, National Center for Health Statistics, US Centers for Disease Control and Prevention, Hyattsville, Maryland.
Craig M. Hales, National Center for Health Statistics, US Centers for Disease Control and Prevention, Hyattsville, Maryland; US Public Health Service, Rockville, Maryland.
Margaret D. Carroll, National Center for Health Statistics, US Centers for Disease Control and Prevention, Hyattsville, Maryland.
Yutaka Aoki, National Center for Health Statistics, US Centers for Disease Control and Prevention, Hyattsville, Maryland.
David S. Freedman, National Center for Chronic Disease Prevention and Health Promotion, US Centers for Disease Control and Prevention, Atlanta, Georgia.
REFERENCES
- 1.Ogden CL, Carroll MD, Lawman HG, Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315(21):2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief. 2017; (288):1–8. [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services. Healthy People 2020: nutrition and weight status. https://www.healthypeople.gov/2020/topics-objectives/topic/nutrition-and-weight-status. [Google Scholar]
- 4.Bullock A, Sheff K, Moore K, Manson S. Obesity and overweight in American Indian and Alaska native children, 2006–2015. Am J Public Health. 2017;107(9):1502–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Fakhouri TH, et al. Prevalence of obesity among youths by household income and education level of head of household—United States 2011–2014. MMWRMorb Mortal Wkly Rep. 2018;67(6):186–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson JA III, Johnson AM. Urban-rural differences in childhood and adolescent obesity in the United States: a systematic review and meta-analysis. ChildObes. 2015;11(3):233–241. [DOI] [PubMed] [Google Scholar]
- 7.Rossen LM, Talih M. Social determinants of disparities in weight among US children and adolescents. Ann Epidemiol. 2014;24(10):705–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bailey-Davis L, Horst M, Hillemeier MM, Lauter A. Obesity disparities among elementary-aged children: data from school-based BMI surveillance. Pediatrics. 2012;130(6):1102–1109. [DOI] [PubMed] [Google Scholar]
- 9.Tarasenko YN, Chen C, Smalley KB, Warren J. Rural-urban differences in perceptions of child overweight among children and adolescents, their guardians and health care professionals in the United States. J Rural Health. 2016;32(1):63–71. [DOI] [PubMed] [Google Scholar]
- 10.Probst JC, Barker JC, Enders A, Gardiner P Current state of child health in rural America: how context shapes children’s health. J Rural Health. 2018;34 (suppl 1):s3–s12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Department of Health and Human Services Health Resources and Services Administration Maternal and Child Health Bureau. The Health and Well-Being of Children in Rural Areas: A Portrait of the Nation, 2011–2012.2015:17 https://mchb.hrsa.gov/nsch/2011-12/rural-health/pdf/rh_2015_book.pdf.
- 12.Liu JH, Jones SJ, Sun H, Probst JC, Merchant AT, Cavicchia P. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: an urban and rural comparison. Child Obes. 2012;8(5): 440–448. [DOI] [PubMed] [Google Scholar]
- 13.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20): 2401–2405. [DOI] [PubMed] [Google Scholar]
- 14.CDC National Center for Health Statistics. National Health and Nutrition Examination Survey: questionnaires, datasets, and related documentation. https://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. [Google Scholar]
- 15.CDC National Center for Health Statistics. NHANES: response rates and population totals. https://wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx. [Google Scholar]
- 16.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health StatReport. 2010;(25):1–5. [PubMed] [Google Scholar]
- 17.Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. AmJClinNutr.2009;90(5):1314–1320. [DOI] [PubMed] [Google Scholar]
- 18.Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689–1712. [DOI] [PubMed] [Google Scholar]
- 19.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA. 2016;315 (21):2284–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.CDC National Center for Health Statistics. NCHS Research Data Center (RDC). https://www.cdc.gov/rdc/.
- 21.Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat 2 2014;(166):1–73. [PubMed] [Google Scholar]
- 22.Ingram DD, Franco SJ. NCH Surban-rural classification scheme for counties. Vital Health Stat 2 2012;(154):1–65. [PubMed] [Google Scholar]
- 23.Parker JD, Talih M, Malec DJ, et al. National Center for Health Statistics data presentation standards for proportions. Vital Health Stat. 2017;2 (175). https://www.cdc.gov/nchs/data/series/sr_02Zsr02_175.pdf. [PubMed] [Google Scholar]
- 24.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171(5):618–623. [DOI] [PubMed] [Google Scholar]
- 25.Cochran WG. Sampling techniques. 3rd ed New York, NY: John Wiley & Sons; 1977. [Google Scholar]
- 26.Skinner CJ, Holt D, Smith TMF. Analysis of Complex Surveys. Chichester, UK: John Wiley & Sons; 1989. [Google Scholar]
- 27.Wolters KM. Introduction to Variance Estimation. New York, NY: Springer-Verlag; 1982. [Google Scholar]
- 28.Korn EL, Graubard BI. Confidence intervals for proportions with small expected number of positive counts estimated from survey data. Surv Methodol. 1998;24(2). http://www5.statcan.gc.ca/olc-cel/olc.action?objId=12-001-X19980024356&objType=47&lang=en&limit=0. [Google Scholar]
- 29.Neuman M, Kawachi I, Gortmaker S, Subramanian SV. Urban-rural differences in BMI in low- and middle-income countries: the role of socioeconomic status. Am J Clin Nutr. 2013;97(2): 428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lo JC, Chandra M, Sinaiko A, et al. Severe obesity in children: prevalence, persistence and relation to hypertension. Int J Pediatr Endocrinol. 2014;2014(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sherry B, Jefferds ME, Grummer-Strawn LM. Accuracy of adolescent self-report of height and weight in assessing overweight status: a literature review. Arch Pediatr Adolesc Med. 2007;161(12): 1154–1161. [DOI] [PubMed] [Google Scholar]
- 32.Akinbami LJ, Ogden CL. Childhood overweight prevalence in the United States: the impact of parent-reported height and weight. Obesity (Silver Spring). 2009;17(8):1574–1580. [DOI] [PubMed] [Google Scholar]
- 33.Freedman DS, Wang J, Maynard LM, et al. Relation of BMI to fat and fat-free mass among children and adolescents. Int J Obes (Lond). 2005; 29(1):1–8. [DOI] [PubMed] [Google Scholar]
- 34.Flegal KM, Ogden CL, Yanovski JA, et al. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. Am J Clin Nutr. 2010;91(4):1020–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zheng W, McLerran DF, Rolland B, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364(8):719–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jafar TH, Islam M, Poulter N, et al. Children in South Asia have higher body mass-adjusted blood pressure levels than white children in the United States: a comparative study. Circulation. 2005;111 (10):1291–1297. [DOI] [PubMed] [Google Scholar]
- 37.Asian and Pacific Islander American Health Forum. Obesity and overweight among Asian American children and adolescents. 2016. https://www.apiahf.org/resource/obesity-and-overweight-among-asian-american-children-and-adolescents/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.